Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Unusual Causes and Presentations of
Caricato da
dnazaryTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Unusual Causes and Presentations of
Caricato da
dnazaryCopyright:
Formati disponibili
CLINICAL STUDIES
UNUSUAL CAUSES AND PRESENTATIONS OF
HEMIFACIAL SPASM
In-Bo Han, M.D. OBJECTIVE: To evaluate unusual possible causes and clinical presentations of hemifa-
Department of Neurosurgery, cial spasm (HFS).
Pochon CHA University
College of Medicine, METHODS: The authors reviewed 1642 cases of HFS. Assessments were based on clin-
Sungnam, Korea ical features, 3-dimensional time-of-flight magnetic resonance angiography, and sur-
gical findings. Causes other than neurovascular compression at the root exit zone of
Jong Hee Chang, M.D. the facial nerve were investigated and unusual clinical presentations were noted.
Department of Neurosurgery,
RESULTS: Nine (0.5%) patients had a secondary causative structural lesion, 7 patients
Yonsei University
College of Medicine, had a tumor, and the remaining 2 had a vascular malformation. Direct compression by
Seoul, Korea dolichoectatic vertebrobasilar artery was noted in 12 (0.7%) patients. In 7 (0.4%)
patients, only the distal portion of the facial nerve was compressed, and five (0.3%)
Jin Woo Chang, M.D. had only venous compression. Bilateral HFS and tic convulsif were encountered in 7
Department of Neurosurgery, (0.4%) and 6 (0.37%) patients, respectively. Fifty-six (3.4%) patients were younger than
Yonsei University
College of Medicine, 30 years old at the time of microvascular decompression.
Seoul, Korea CONCLUSION: HFS can result from tumor, vascular malformation, and dolichoectatic
artery. Therefore, appropriate preoperative radiological investigations are crucial to
Ryoong Huh, M.D. achieve a correct diagnosis. The authors emphasize that distal compression or only
Department of Neurosurgery,
venous compression can be responsible for persistent or recurrent symptoms postop-
Pochon CHA University
College of Medicine, eratively. In cases of bilateral HFS, a definite differential diagnosis is necessary for appro-
Sungnam, Korea priate therapy. MVD is recommended as the treatment of choice in patients younger
than 30 years old or patients with painful tic convulsif.
Sang Sup Chung, M.D.
KEY WORDS: Bilateral, Dolichoectasia, Facial nerve, Hemifacial spasm, Neurovascular compression, Tic
Department of Neurosurgery,
convulsif
Pochon CHA University
College of Medicine,
Sungnam, Korea Neurosurgery 65:130137, 2009 DOI: 10.1227/01.NEU.0000348548.62440.42 www.neurosurgery-online.com
Reprint requests:
Ryoong Huh, M.D.,
H
or Sang Sup Chung, M.D., emifacial spasm (HFS) is characterized artery enlargement and tortuosity, is also a rare
Department of Neurosurgery, by involuntary contractions of the cause of HFS (13). Vascular compression usu-
Pochon CHA University, facial muscles and is generally caused ally occurs at the REZ of the facial nerve by
Bundang CHA Hospital, by vascular compression of the root exit zone arterial vessels. However, Ryu et al. (14)
351 Yatap-dong, Bundang-gu,
Sungnam, 463-712, Korea.
(REZ) of the ipsilateral facial nerve (1, 4). reported that only the distal portion of the
Email: haninbo@naver.com However, a number of rare causes of HFS have facial nerve was compressed in 2.1% of pa-
also been identified, which include tumors, tients, and Barker et al. (1) reported that the
Received, September 1, 2008. aneurysms, and arteriovenous malformations. facial nerve is compressed only by a vein in
Accepted, March 12, 2009. Furthermore, a number of large series have 2.9% of patients.
reported that symptomatic HFS resulting from Bilateral involvement in HFS is extremely
Copyright 2009 by the
Congress of Neurological Surgeons
mass lesions occurs infrequently in 0.4% to rare and occurs in only an estimated 0.6% to
2.2% of cases (1, 810, 15, 19). In addition, 5% of patients (7, 17, 18). The coexistence of
direct compression by dolichoectatic verte- HFS and ipsilateral trigeminal neuralgia (TN),
brobasilar arteries (VBAs), characterized by also known as tic convulsif, is an additional
possible clinical manifestation. Barker et al. (1)
ABBREVIATIONS: HFS, hemifacial spasm; MVD, reported that 4.1% of HFS patients had tic con-
microvascular decompression; REZ, root exit vulsif. HFS usually occurs in middle-aged and
zone; TN, trigeminal neuralgia; VBA, verte- older patients, but HFS has been reported in
brobasilar artery
patients younger than 30 years old (3).
130 | VOLUME 65 | NUMBER 1 | JULY 2009 www.neurosurgery-online.com
UNUSUAL CAUSES AND PRESENTATIONS OF HEMIFACIAL SPASM
In the present study, we investigated unusual causes of HFS
(i.e., other than vascular compression at the REZ of the facial TABLE 1. Type of offenders
nerve) and its unusual clinical manifestations. In addition, the Type No. of patients (%)
literature on the subject was reviewed and possible mecha-
nisms are discussed. Vessels 1633 (99.4 %)
Artery 1628 (99.1%)
PATIENTS AND METHODS Only vein 5 (0.3 %)
Mass 9 (0.5 %)
Patient Population Epidermoid 3
We analyzed 1642 HFS patients who were treated at Yonsei Vestibular schwannoma 1
University, Severance Hospital (September 1978February 2003) and at
Lipoma 2
Pochon CHA University, Bundang CHA Hospital (March 2003March
2007). A total of 1658 operations were performed by the senior author Arachnoid Cyst 1
(SSC). Decisions to perform surgery were based on clinical assessments Arterivenous malformation 1
and preoperative imaging findings.
Developmental venous anomaly 1
Pre- and Intraoperative Evaluation Total 1642 (100%)
Preoperative 3-dimensional time-of-flight magnetic resonance
angiography (Sonata; Siemens, Erlangen, Germany) was first utilized in
1992 and preoperative 3-dimensional-constructive interference in (1.6%). Multiple offenders were found in 15.5% of cases.
steady state magnetic resonance imaging in 2003. As compared with However, 7 patients (0.4%) had HFS secondary to a cerebello-
3-dimensional time-of-flight images, more vascular contact at the root
pontine angle tumor (3 epidermoids, 1 vestibular schwannoma,
entry zone can be detected by constructive interference in steady state
magnetic resonance imaging. Brainstem auditory evoked potentials
1 arachnoid cyst, and 2 lipomas), and 2 patients (0.1%) had HFS
were monitored during operations, but facial electromyography was resulting from vascular malformations (1 from an arteriovenous
not performed intraoperatively. malformation and 1 due to a developmental venous anomaly).
Types of offenders are summarized in Table 1. In 3 cases (2 epi-
Clinical Assessments dermoids and 1 arachnoid cyst), the facial nerve was com-
Clinical results were assessed by personal interview or by telephone, pressed by the tumor and vascular compression was observed
and were classified as excellent, good, fair, or poor, where excellent at the REZ after tumor resection. Therefore, in these cases,
meant no residual spasm following microvascular decompression Teflon felt (Bard, Tempe, AZ) was also placed to decompress the
(MVD), good meant spasm relief of more than 90%, fair indicated facial nerve (Fig. 1). In the remaining 3 cases (1 epidermoid, 1
50% to 90% spasm relief, and poor described spasm relief of less vestibular schwannoma, and 1 lipoma), surgical findings
than 50%. Recurrence was defined as reappearance of facial spasm showed an incorporated and distorted facial nerve within the
after complete symptom resolution at more than 6 months after MVD.
tumor without any obvious vascular compression; thus, only
tumor removal was performed (Fig. 2). Postoperatively, HFS
RESULTS completely disappeared in all 6 patients. In 1 case with worsen-
ing HFS, we excised the lipoma; the subsequent HFS completely
Clinical Features and Surgical Outcomes resolved. However, the patient developed transient facial weak-
The mean patient age was 49.5 years (age range, 15 78 ness and a severe permanent hearing loss after resection.
years). The male-to-female ratio was 1:3.4, and no significant Another lipoma patient was managed conservatively due to a
laterality differences were observed. The mean symptom dura- perceived high surgical risk (Fig. 3). In a case with a cerebellar
tion was 7.0 years (range, 6 months40 years), and the mean arteriovenous malformation, an engorged draining vein com-
follow-up duration was 31.7 months (range, 6.4196.8 months). pressed the superior aspect of the REZ of the facial nerve (Fig.
Excellent and good results were achieved by 87.7% and 4). This patient was treated effectively by gamma knife surgery.
5.9% of patients, respectively, resulting in an overall success One patient (patient 25) with a developmental venous anomaly
rate of 93.7%. The rate of HFS recurrence was 0.8% (n 13). presented with a 5-year history of left trigeminal neuralgia and
Postoperative complications included infarction or hemorrhage an 18-month history of left HFS. In this case, the HFS was
(n 18, 1.1%), permanent facial palsy (n 21, 1.3%), permanent caused by a draining vein which compressed the REZ of the
hearing deficit (n 36, 2.2%), wound infection (n 64, 3.9%), facial nerve, and the TN probably resulted from the involve-
lower cranial nerve palsy (n 4, 0.2%), and a cerebrospinal ment of the spinal trigeminal nucleus of the trigeminal nerve by
fluid leak (n 21, 1.3%). There was no operative death. the developmental venous anomaly (Fig. 5). This patient was
treated conservatively due to the high risk of surgery.
Secondary HFS
In patients with neurovascular compression, the main cul- Vertebrobasilar Dolichoectasia
prits were the anterior inferior cerebellar artery (42.3%), the pos- Direct compression by dolichoectatic VBA was noted in 12
terior inferior cerebellar artery (39.9%), and the vertebral artery patients (0.7%) who underwent MVD. The mean patient age
NEUROSURGERY VOLUME 65 | NUMBER 1 | JULY 2009 | 131
HAN ET AL.
A B A B
C D
FIGURE 1. Preoperative magnetic C
resonance imaging (MRI) series in
a 75-year-old woman with a 5-year
history of right hemifacial spasm.
A, axial T2-weighted MRI scan
showing a hyperintense lesion in
the right cerebellopontine angle cis-
tern. B, axial 3-dimensional time-
of-flight (3D-TOF) magnetic reso-
nance angiogram (MRA) showing
the artery (arrow) compressing the
FIGURE 3. Axial MRI series in a 37-year-old woman with a 2-year his-
root exit zone. C, diffusion weighted
tory of left hemifacial spasm. T2-weighted (A), T1-weighted (B), and
image revealing the hyperintensity
fluid-attenuated inversion recovery (C) images demonstrating a hyperin-
of the lesion (arrow), consistent
tense lesion. D, the lesion appears hypointense on fat suppression
with an epidermoid tumor.
sequences, consistent with a lipoma.
A B 26%, respectively, and 8.3% had a permanent hearing deficit. Of
these 12 patients, one (patient 17) had bilateral HFS and 2
patients (patients 20 and 24) had tic convulsif. The patient with
bilateral symptoms underwent 2-stage MVD and achieved
complete recovery, and the 2 patients with tic convulsif
achieved satisfactory results after MVD.
Only Venous Compression of the Facial Nerve
Venous compression alone was identified in 5 patients (0.3%).
FIGURE 2. Preoperative MRI series in a 34-year-old woman with a 2-year Table 2 shows the clinical features of these patients. Two patients
history of left hemifacial spasm. A, T1-weighted scan showing a (patients 1 and 4) exhibited a prominent large vein crossing over
hypointense lesion in the left cerebellopontine angle cistern. B, T2-
the REZ of the facial nerve. Teflon felt was placed to separate this
weighted scan revealing a hyperintense lesion, consistent with an epider-
moid tumor.
from the facial nerve and to elevate coagulated venous branches
off the facial nerve following coagulation. The remaining 2
patients (patients 2 and 3) had a smaller vein, which had coagu-
was 58.9 years (age range, 4271 years) with a male-to-female lated and divided, compressing the facial nerve REZ. As
ratio of 7:5. Ten patients had symptoms on the left side, and the described in our previous report (11), 1 patient (Patient 5) had no
mean symptom duration was 7.0 years (range, 122 years). improvement after the first MVD at another hospital and under-
Dolichoectatic VBA proved difficult to mobilize and a Teflon went a second operation. During the second MVD procedure, a
ball (Bard, Tempe, AZ) was introduced step-by-step from the large vein compressing the facial nerve in the distal region only
proximal part of the dolichoectatic VBA to separate the facial was located under Teflon felt. The patient achieved complete
nerve from the offender. After performing this maneuver, all relief from HFS after the second MVD procedure.
the patients achieved satisfactory symptom relief. However,
the postoperative complication rate among these 12 patients Distal Compression of the Facial Nerve
was greater than the overall complication rate. Transient facial The authors treated 7 patients (0.4%) who exhibited com-
palsy and transient hearing impairment were noted in 25% and pression only at the distal portion of the facial nerve. Table 3
132 | VOLUME 65 | NUMBER 1 | JULY 2009 www.neurosurgery-online.com
UNUSUAL CAUSES AND PRESENTATIONS OF HEMIFACIAL SPASM
symptom duration was 8.6 years (range, 120 years). HFS
A B started on the left side in 5 of the 7, and the mean latency to
contralateral facial nerve involvement was 6.1 year (range,
0.510 years). The sides affected initially usually remained
more severely involved. The upper face was the site of onset in
all patients. All but 1 of the 7 patients underwent unilateral
MVD for the initial more severe spasm, because contralateral
HFS was mild and satisfactory results were achieved post uni-
lateral MVD. However, 1 patient (patient 17) with dolicho-
ectatic VBA compressing the facial nerve had sufficiently severe
contralateral symptoms to require bilateral MVD (Fig. 6). This
patient developed left eyelid twitching followed by lower facial
FIGURE 4. 3D-TOF MRA in a 40-year-old man with a 5-year history of muscles. Operative findings on the side of initial onset showed
left hemifacial spasm, revealing a nidus (arrow) in the left cerebellum (A)
REZ compression of the facial nerve by dolichoectatic VBA and
and dilated vein (arrow) compressing superior aspect of root exit zone of
posterior inferior cerebellar artery. Approximately 6 years after
facial nerve (B). The patients hemifacial spasm improved significantly
after gamma knife radiosurgery. HFS abolition by initial MVD, the patient developed twitching
of right facial muscles. A second operation revealed neurovas-
cular compression at the right REZ by the anterior inferior cere-
A B bellar artery (Fig. 6). This patient was successfully treated by 2-
stage bilateral MVD.
Tic Convulsif (Concurrent HFS and Ipsilateral TN)
Six patients (0.4%) were found to have tic convulsif. Table 5
shows the clinical features of these 6 patients. Two patients
(patients 20 and 24) noted facial muscle contraction and ipsilat-
eral severe TN. These patients were successfully treated by
simultaneous decompression of Cranial Nerves V and VII. One
patient (patient 24) had a single dolichoectatic VBA compressing
both the trigeminal and facial nerve. In 3 patients (patients 20,
FIGURE 5. Two-dimensional fast C 21, and 22), multiple vessels were responsible for tic convulsif.
spin echo image (A) and T1-
Because complete remission from TN occurred after botulinum
weighted image after the adminis-
toxin injections, 2 patients (patients 21 and 22) underwent MVD
tration of gadolinium (B) showing
dilated draining vein (arrow) com- for HFS alone. Another patient (patient 23) exhibited no visible
pressing the facial nerve (arrow- vessels compressing the REZ of the trigeminal nerve and MVD
head). C, T1-weighted image with was performed for only HFS. Patient 25 had a developmental
contrast demonstrating an involve- venous anomaly, namely, an engorged draining vein compress-
ment of the spinal trigeminal ing the REZ of the facial nerve and the spinal trigeminal nucleus
nucleus (arrow) of the trigeminal of the trigeminal nerve (Fig. 5). This patient was managed con-
nerve by the developmental venous servatively due to the high risk of surgery.
anomaly.
HFS in Youth
shows the clinical features of these patients. All patients expe- Fifty-six (3.4%) patients were younger than the age of 30
rienced typical HFS, and no vascular compression was found at years at the time of MVD. Thirty-three (58.9%) were women,
the REZ in these 7 patients. All but 2 patients (patients 5 and 6) and 31 (55.4%) had right side symptoms. The mean symptom
had an excellent result after MVD. In 1 patient (patient 5) with duration was 5.7 0.5 years. The patients age at HFS onset
persistent spasm after the first MVD procedure, the facial nerve ranged from 11 to 27 years (mean, 22.6 0.7 years) and the age
was found to be distally compressed by a vein. This patient at time of MVD ranged from 21 to 30 years (mean, 26.3 0.3
achieved complete recovery after repeat MVD. years). All patients had definite offending vessels as follows:
anterior inferior cerebellar artery in 48.2% (27 of 56), posterior
Bilateral HFS inferior cerebellar artery in 42.9% (24 of 56), or multiple vessels
The prevalence of bilateral HFS in our series was 0.4% (7 in 8.9% (5 of 56). No anatomic variations were found of vessels
patients), and its main clinical features are summarized in Table at the REZ. The overall success rate (excellent or good) was
4. All patients had unilateral HFS followed by bilateral and 92.9% (n 52) and 1 (1.8%) recurred. No significant difference
asymmetric facial contractions. The mean age of these 7 was found between young patients and older patients in terms
patients was 50.3 years (age range, 3569 years), and the mean of symptom duration and surgical outcome.
NEUROSURGERY VOLUME 65 | NUMBER 1 | JULY 2009 | 133
HAN ET AL.
TABLE 2. Summary of five cases of hemifacial spasm resulting from only venous compressiona
Symptom Side of
Patient no. Age (y)/sex Treatment Result
duration (y) symptom
1 38/F 8 Left MVD Excellent
2 61/F 7 Right Coagulation Poor
3 63/F 10 Right Coagulation Excellent
4 35/F 7 Right MVD Excellent
5 49/F 5 Right First operation: MVD of artery at REZ No relief
Second operation: 5 years later Excellent
No NVC at REZ
Vein
a
MVD, microvasular decompression; REZ, root entry zone; NVC, neurovascular compression.
TABLE 3. Summary of seven cases of hemifacial spasm resulting from compression of the distal portion of the facial nervea
Age Symptom Surgical
Patient no. Side Offenders
(y)/sex duration (y) outcome
6 45/F 3 Left No NVC at REZ Poor
MVD of PICA at distal portion of the nerve
7 60/M 8 Left No NVC at REZ Good
MVD of AICA at midportion of the nerve
8 42/F 6 Left No NVC at REZ Excellent
MVD of PICA at distal portion of the nerve
9 46/M 2 Left No NVC at REZ Good
MVD of AICA at distal portion of the nerve
5 49/F 5 Right First operation: MVD of artery at REZ No relief
Second operation: 5 years later Excellent
No NVC at REZ
Vein at distal portion of the nerve
11 62/F 1 Left No NVC at REZ Good
MVD of AICA at distal portion of the nerve
12 56/M 5 Right No NVC at REZ Excellent
MVD of PICA at distal portion of the nerve
a
NVC, neurovascular compression; REZ, root entry zone; MVD, microvasular decompression; PICA, posterior inferior cerebellar artery; AICA, anterior inferior cerebellar artery.
DISCUSSION sion if a vessel loop is noted in close proximity to the nerve and
is compressing its REZ (6). In cases of cerebellopontine angle
HFS is characterized by a painless, involuntary twitching of lipoma, which is a slow-growing tumor with infiltrative
one side of the face. Vascular compression at the REZ of the growth, conservative treatment is usually recommended due to
facial nerve has been suggested to be responsible for HFS (1, 4), the high risk of surgery. However, in cases with intractable
although other less common etiologies and presentations have clinical symptoms, partial resection is usually advocated to
been described (2, 6, 810, 12, 15, 16, 19). minimize postoperative deficits (2). In our series, 1 lipoma
patient with worsening HFS achieved complete relief from
Secondary HFS spasm after surgical resection, but at the expense of transient
HFS may result from direct neural compression by a second- facial weakness and permanent severe hearing loss.
ary mass lesion causing neural dysfunction or irritation of the
facial nerve pathway. Coexistent vascular compression of the Vertebrobasilar Dolichoectasia
facial nerve is a possible cause in secondary HFS. Therefore, HFS resulting from dolichoectatic VBA has been reported to
MVD of the facial nerve should be performed after tumor exci- be treatable by MVD. However, manipulation of ectactic arter-
134 | VOLUME 65 | NUMBER 1 | JULY 2009 www.neurosurgery-online.com
UNUSUAL CAUSES AND PRESENTATIONS OF HEMIFACIAL SPASM
TABLE 4. Clinical features of patients with bilateral hemifacial spasma
Age at onset Symptom Side Symptom Side of
Patient no. Latency (y) Severity Imaging
(y)/sex duration (y) onset type MVD
13 39/F 7 L Typical 6 LR Left PICA compression L
Right AICA contact
14 60/F 20 L Typical 10 LR Left AICA compression L
Right AICA contact
15 35/F 3 R Typical 7 RL Right PICA compression R
Left: normal
16 54/F 6 R Typical 7 RL Right AICA compression R
Left AICA contact
17 51/F 1 L Typical 4 LR Dolichoectatic VBA L, R
18 44/F 8 L Typical 8 LR Left AICA compression L
Right: normal
19 69/F 15 L Typical 0.5 LR Left AICA compression L
Right PICA contact
a
MVD, microvasular decompression; L, left; R, right; PICA, posterior inferior cerebellar artery; AICA, anterior inferior cerebellar artery; VBA, vertebrobasilar artery.
(4, 13). In our series, the postoperative complication rate was
A B greater than the overall complication rate, although satisfactory
symptom relief was achieved. To reduce complications and
decompress the REZ successfully, we recommend a stepwise
decompression method, that is, incremental decompression
from the proximal part of the dolichoectatic VBA using a Teflon
ball. Furthermore, an effort should be made to leave enough
working space to decompress offenders related to dolichoecta-
sia and to reduce vascular manipulation to a minimum.
Only Venous Compression of the Facial Nerve
C D Venous compression alone can cause persistent symptoms or
recurrence after the first MVD procedure (11, 14). In our series,
1 patient (patient 5) with persistent spasm had a large vein in
the distal portion that was overlooked during the first MVD
procedure. This serves as a reminder that every effort should be
made to identify veins that compress the facial nerve during
operation. Furthermore, recurrence of HFS attributable to veins
can be caused by venous recollateralization. Therefore, Teflon
felt should be placed to elevate coagulated venous branches,
especially if a large vein compressing the facial nerve is coag-
ulated and cut.
FIGURE 6. Preoperative 3D-TOF MRA showing left vertebral artery
Distal Compression of the Facial Nerve
compressing the facial nerve at the root exit zone (A) and tortuosity of the
vertebral artery (B). C and D, MRA source images after first operation Neurosurgeons can easily overlook vascular compression of
revealing loop of right anterior inferior cerebellar artery (arrow) causing the distal portion of the facial nerve, and as a result, spasms
neurovascular compression. may persist after MVD. Although Schwann cells of peripheral
axons are more resistant to demyelination, distal compression
of the facial nerve may play an important role, especially in
ies and traction of small perforators during MVD have been cases with no offender at the REZ (14). Therefore, it should be
reported to present serious risks, which included permanent borne in mind that compression of the distal portion of the
facial weakness, deafness, stroke, or death. Furthermore, fre- nerve may be responsible for HFS in cases with no vascular
quent recurrence may occur due to poor mobility of the artery, compression at the REZ during operation, and in patients with
which makes it difficult to achieve sufficient decompression a persistent spasm after first MVD at the REZ.
NEUROSURGERY VOLUME 65 | NUMBER 1 | JULY 2009 | 135
HAN ET AL.
TABLE 5. Summary of five cases with tic convulsifa
Offender
Age Trigeminal Facial Follow-up Surgical
Patient no. Side Surgery
(y)/sex nerve nerve duration (y) outcome
20 59/M Vein, SCA Dolichoectactic L 5 MVD for TN, No pain,
VA, AICA HFS HFS: good
21 40/F SCA AICA R 2 MVD for No pain, HFS:
HFS excellent
22 44/F SCA PICA R 2 MVD for No pain, HFS:
HFS excellent
23 52/F No AICA R 1 MVD for Mild pain, HFS:
offender HFS excellent
24 75/F Dolichoec- Dolichoec- L 2 MVD for TN, Mild pain,
tactic VA, SCA tactic VA, PICA HFS HFS: good
25 41/F Developmental Draining vein L 3 Conservative
venous anomaly of developmental treatment
venous anomaly
a
SCA, superior cerebellar artery; VA, vertebral artery; AICA, anterior inferior cerebellar artery; L, left; MVD, microvasular decompression; TN, trigeminal neuralgia; HFS, hemifacial
spasm; R, right; PICA, posterior inferior cerebellar artery.
Bilateral HFS Furthermore, they also suggest that HFS may be caused by eti-
In our series, no significant clinical difference was found ologies other than congenital anomalies of offenders or the ves-
between unilateral and bilateral HFS. All bilateral patients had sel aging process. Moreover, although the pathogenesis of early
typical HFS, and the side affected initially usually remained the onset HFS remains unclear, the causes and progress of HFS
more severely involved. Bilateral HFS may sometimes be difficult appear to be identical in young and elderly HFS patients.
to distinguish from other facial dyskinesias, such as ble-
pharospasm, facial tics, and facial myokymia, but a misdiagnosis CONCLUSIONS
can lead to inadequate therapy a progressive symptom worsen-
HFS can result from tumor, vascular malformation, or
ing. Thus, differential diagnosis should be undertaken promptly
dolichoectatic artery. Therefore, appropriate preoperative radi-
to ensure appropriate treatment. The protracted latency of con-
ological investigations are mandatory to reach a correct diagno-
tralateral involvement and asymmetrical contractions may help
sis. Distal compression can be responsible for HFS, especially if
to differentiate bilateral HFS from other facial dyskinesias (7).
vascular compression at the REZ is not identified during oper-
Tic Convulsif ation and if MVD at the REZ does not result in cure. Further-
more, it should be borne in mind that only venous compression
Previous reports have described various causes of tic convul-
can be responsible for persistent symptoms or recurrence after
sif. These include dolichoectatic vertebral artery, vascular mal-
first MVD. In cases of bilateral HFS, a definite differential diag-
formations, and tumors (5, 6). In our series, multiple vessels
nosis is necessary to facilitate appropriate therapy. Moreover, in
compressed the REZ of the trigeminal and facial nerve in most
young patients under 30 and painful tic convulsif patients,
cases, but only 1 patient had a single dolichoectatic VBA com-
MVD is recommended as the treatment of choice.
pressing both facial and trigeminal nerves. When neurovascu-
lar compressions are found at the REZs of trigeminal and facial Disclosure
nerves, MVD of the 2 cranial nerves is recommended. The authors have no personal financial or institutional interest in any of the
drugs, materials, or devices described in this article.
HFS in Youth
HFS is generally a disease of the elderly, and vascular com- REFERENCES
pression is believed to result from atherosclerotic vessel
changes. As described in our previous report (3), in young 1. Barker FG 2nd, Jannetta PJ, Bissonette DJ, Shields PT, Larkins MV, Jho HD:
patients (30 years) undergoing MVD, we rarely observed a Microvascular decompression for hemifacial spasm. J Neurosurg 82:201210,
tortuous vertebral artery compressing the facial nerve and 1995.
2. Brodsky JR, Smith TW, Litofsky S, Lee DJ: Lipoma of the cerebellopontine
found no anatomic variations of vessels or any arachnoid thick- angle. Am J Otolaryngol 27:271274, 2006.
ening. The findings of the present study show that satisfactory 3. Chang JW, Chang JH, Park YG, Chung SS: Microvascular decompression of the
surgical results are achieved in both younger and older patients. facial nerve for hemifacial spasm in youth. Childs Nerve Syst 17:309312, 2001.
136 | VOLUME 65 | NUMBER 1 | JULY 2009 www.neurosurgery-online.com
UNUSUAL CAUSES AND PRESENTATIONS OF HEMIFACIAL SPASM
4. Chung SS, Chang JH, Choi JY, Chang JW, Park YG: Microvascular decompres- Although rare, the presence of other structural abnormalities causing
sion for hemifacial spasm: A long-term follow-up of 1,169 consecutive cases. HFS underscores the importance of preoperative high-resolution imag-
Stereotact Funct Neurosurg 77:190193, 2001. ing. This is important not only for planning surgical intervention but
5. Cook BR, Jannetta PJ: Tic convulsif: Results in 11 cases treated with microvas- also for avoiding surgical intervention in unusual circumstances in
cular decompression of the fifth and seventh cranial nerves. J Neurosurg
which the pathology may not be readily amenable to surgical therapy.
61:949951, 1984.
This is the situation for patients with lipomas and developmental
6. Desai K, Nadkarni T, Bhayani R, Goel A: Cerebellopontine angle epidermoid
tumor presenting with tic convulsif and tinnitusCase report. Neurol Med venous anomalies.
Chir (Tokyo) 42:162165, 2002. The authors also reviewed patients with unusual manifestations of
7. Felcio AC, Godeiro-Junior Cde O, Borges V, Silva SM, Ferraz HB: Bilateral HFS, including 7 patients with a compression of the distal portion of the
hemifacial spasm: A series of 10 patients with literature review. Parkinsonism facial nerve, 5 with venous compression alone, 7 with bilateral HFS, and
Relat Disord 14:154156, 2008. 6 with tic convulsif. Three of the patients underwent microvascular
8. Kim Y, Tanaka A, Kimura M, Yoshinaga S, Tomonaga M: Arteriovenous mal- decompression when they were under 20 years of age. This large experi-
formation in the cerebellopontine angle presenting as hemifacial spasm ence has been analyzed in detail to provide further insight into the
Case report. Neurol Med Chir (Tokyo) 31:109112, 1991. unusual manifestations and unusual etiologies for HFS. These anomalies
9. Kobata H, Kondo A, Iwasaki K: Cerebellopontine angle epidermoids pre-
and variants should be kept in mind when evaluating patients with HFS.
senting with cranial nerve hyperactive dysfunction: Pathogenesis and long-
term surgical results in 30 patients. Neurosurgery 50:276286, 2002. Daniel L. Barrow
10. Nagata S, Matsushima T, Fujii K, Fukui M, Kuromatsu C: Hemifacial spasm Atlanta, Georgia
due to tumor, aneurysm, or arteriovenous malformation. Surg Neurol
38(3):204209, 1992.
11. Park YS, Chang JH, Cho J, Park YG, Chung SS, Chang JW: Reoperation for
persistent or recurrent hemifacial spasm after microvascular decompression.
I n this report, Han et al. describe their collective experience with a very
large series of patients operated on for HFS during a 30-year period. A
total of 1642 patients over this time period were analyzed, and the
Neurosurgery 58:11621167, 2006.
12. Peker S, Ozduman K, Kili T, Pamir MN: Relief of hemifacial spasm after authors culled out those patients who had unusual clinical or surgical
radiosurgery for intracanalicular vestibular schwannoma. Minim Invasive findings to obtain a guess on the incidence of these findings as well as
Neurosurg 47:235237, 2004. the results of surgery in these unusual circumstances. Specifically, the
13. Rahman EA, Trobe JD, Gebarski SS: Hemifacial spasm caused by vertebral authors examined patients with secondary HFS, bilateral HFS, HFS
artery dolichoectasia. Am J Ophthalmol 133:854856, 2002. attributable to venous compression, HFS attributable to distal nerve com-
14. Ryu H, Yamamoto S, Sugiyama K, Uemura K, Miyamoto T: Hemifacial spasm pression, and HFS in the pediatric population. These scenarios are admit-
caused by vascular compression of the distal portion of the facial nerve. tedly uncommon. In fact, the small numbers of patients in each of these
Report of seven cases. J Neurosurg 88:605609, 1998.
categories in this large series underscores just how uncommon they are.
15. Sato K, Ezura M, Takahashi A, Yoshimoto T: Fusiform aneurysm of the ver-
tebral artery presenting hemifacial spasm treated by intravascular emboliza-
The first message, therefore, is that whenever a practitioner encounters
tion: Case report. Surg Neurol 56:5255, 2001. a patient with, say, bilateral HFS, another cause for these symptoms
16. Takano S, Maruno T, Shirai S, Nose T: Facial spasm and paroxysmal tinnitus should be thoroughly sought. The same can be said of patients thought
associated with an arachnoid cyst of the cerebellopontine angleCase report. to have venous compression as a cause of HFS; these patients are far
Neurol Med Chir (Tokyo) 38:100103, 1998. more likely to have an occult arterial compression.
17. Tan EK, Chan LL: Clinico-radiologic correlation in unilateral and bilateral The overall results reported in this large series largely reflect those
hemifacial spasm. J Neurol Sci 222:5964, 2004. of other previously published studies. The complications outlined by
18. Tan EK, Jankovic J: Bilateral hemifacial spasm: A report of five cases and a lit- the authors also reflect the usual array of complications seen elsewhere.
erature review. Mov Disord 14:345349, 1999. Therefore, with the usual caveats of a historical, uncontrolled series,
19. Uchino M, Nomoto J, Ohtsuka T, Kuramitsu T: Fusiform aneurysm of the ver-
this series confirms earlier reports. There is not enough information in
tebral artery presenting with hemifacial spasm treated by microvascular
decompression. Acta Neurochir (Wien) 147:901903, 2005.
this type of report on the results of surgery in the setting of any of the
unusual causes the authors examined; there are simply too few patients
in each of these groups. Nevertheless, specific attention to the unusual
Acknowledgment
causes of HFS in such a large series allows the reader to glean insight
Ryoong Huh, M.D., and Sang Sup Chung, M.D., contributed equally to the into their true incidence.
preparation of this manuscript.
Oren Sagher
Ann Arbor, Michigan
COMMENTS
H emifacial spasm (HFS) is a very specific clinical entity that is asso-
ciated with vascular compression at the root exit zone of the facial
T he surgical treatment of choice for HFS is microvascular decompres-
sion. However, the diverse anatomic variants and causes of compres-
sion of the facial nerve do not always make it easy. The authors present a
nerve, with very rare exceptions. This article elegantly outlines those
series of 1642 patients with HFS treated during a period of more than 29
rare exceptions and provides some insight into the incidence and clini-
years. Through their distinct experiences, they describe the unusual cases,
cal management of other structural anomalies that may account for HFS.
including HFS attributable to venous compression, compression of the
Han et al. have reviewed the extensive experience of the senior author
distal portion of the facial nerve, bilateral HFS, and tic convulsif.
(SSC) in managing 1642 patients with HFS who were evaluated by clin-
Although this article is rather descriptive for the paucity of unusual
ical examination, 3-dimensional magnetic resonance angiography, and
causes, it may give the reader information on the incidence and operative
intraoperative findings in the majority of patients. Nine patients har-
results of these entities. I wish that the overall results, including compli-
bored structural abnormalities, including 7 neoplasms and 2 vascular
cations, of their vast experience were presented so that one could compare
malformations causing the HFS. Direct compression by dolichoectatic
and understand the surgical outcomes of these unusual cases.
vertebrobasilar arteries was identified in 12 patients, for an incidence of
1.2% of patients having structural compression of the facial nerve attrib- Dong Gyu Kim
utable to an anomaly other than microvascular compression. Seoul, Korea
NEUROSURGERY VOLUME 65 | NUMBER 1 | JULY 2009 | 137
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Smart Science 6Documento16 pagineSmart Science 6april light67% (3)
- Crochet Pattern For A Human Heart: Valérie Prieur-Côté May 3, 2018Documento7 pagineCrochet Pattern For A Human Heart: Valérie Prieur-Côté May 3, 2018Ale ReséndizNessuna valutazione finora
- Life Processes Class 10 Notes Biolog1Documento8 pagineLife Processes Class 10 Notes Biolog1Eashurock KnigamNessuna valutazione finora
- CH 19 Transport in HumanDocumento49 pagineCH 19 Transport in HumanRay PeramathevanNessuna valutazione finora
- USABO 18 Open Exam - Final Wo AnsDocumento17 pagineUSABO 18 Open Exam - Final Wo AnsJ.Chang ChangNessuna valutazione finora
- Open Heart SurgeriesDocumento48 pagineOpen Heart SurgeriesHoney PrasadNessuna valutazione finora
- 2 Phlebotomy Notes Taken From The Lecture of Sir Antonio Pascua JR RMTDocumento5 pagine2 Phlebotomy Notes Taken From The Lecture of Sir Antonio Pascua JR RMTRhoda Mae CubillaNessuna valutazione finora
- American Academy of Aesthetic Medicine Level 1Documento11 pagineAmerican Academy of Aesthetic Medicine Level 1Lydia KirbyNessuna valutazione finora
- Dermatology MCQ 1700Documento45 pagineDermatology MCQ 1700Dr-Jahanzaib Gondal100% (1)
- Principles of Patient PositioningDocumento62 paginePrinciples of Patient PositioningMelody JusticeNessuna valutazione finora
- ULAM, CHIN V. - NCM 118 PrelimDocumento8 pagineULAM, CHIN V. - NCM 118 PrelimChin Villanueva Ulam100% (1)
- Cover LetterDocumento1 paginaCover LetterdnazaryNessuna valutazione finora
- Galley ProofDocumento4 pagineGalley ProofdnazaryNessuna valutazione finora
- ReferensiDocumento3 pagineReferensidnazaryNessuna valutazione finora
- Oi2011 PDFDocumento8 pagineOi2011 PDFdnazaryNessuna valutazione finora
- Title PageDocumento1 paginaTitle PagednazaryNessuna valutazione finora
- Nocun2015 PDFDocumento5 pagineNocun2015 PDFdnazaryNessuna valutazione finora
- Endoscopic Ventriculostomy Versus Shunt Operation in Normal Pressure Hydrocephalus: Diagnostics and IndicationDocumento4 pagineEndoscopic Ventriculostomy Versus Shunt Operation in Normal Pressure Hydrocephalus: Diagnostics and IndicationdnazaryNessuna valutazione finora
- Effects of Information Provision Activities in Streets On Driving SpeedsDocumento8 pagineEffects of Information Provision Activities in Streets On Driving SpeedsdnazaryNessuna valutazione finora
- Cornell A 2003Documento13 pagineCornell A 2003dnazaryNessuna valutazione finora
- T S M P H: HE Urgical Anagement of Ediatric YdrocephalusDocumento10 pagineT S M P H: HE Urgical Anagement of Ediatric YdrocephalusdnazaryNessuna valutazione finora
- Berg Sneider 2008Documento18 pagineBerg Sneider 2008dnazaryNessuna valutazione finora
- Diagnosis and Management of Idiopathic Normal-Pressure HydrocephalusDocumento11 pagineDiagnosis and Management of Idiopathic Normal-Pressure HydrocephalusdnazaryNessuna valutazione finora
- Hemifacial Spasm A NeurosurgicalDocumento8 pagineHemifacial Spasm A NeurosurgicaldnazaryNessuna valutazione finora
- Treatment of Hydrocephalus: Mere Survival Is Not EnoughDocumento7 pagineTreatment of Hydrocephalus: Mere Survival Is Not EnoughdnazaryNessuna valutazione finora
- Tests General 08Documento32 pagineTests General 08melvingeorge200950% (2)
- Joukal (2017) Anatomy of The Human Visual PathwayDocumento16 pagineJoukal (2017) Anatomy of The Human Visual PathwaysektemujibNessuna valutazione finora
- Learning Resource Workbook Science 6-Analyn Gaballo PagsabanganDocumento6 pagineLearning Resource Workbook Science 6-Analyn Gaballo PagsabanganJohana BALASNessuna valutazione finora
- Abbreviations 2011Documento27 pagineAbbreviations 2011Takahito KamimuraNessuna valutazione finora
- Hemodynamic DisordersDocumento6 pagineHemodynamic DisordersPradeep100% (1)
- 2012-03 - Resection of Tumors of The Neck of The Pancreas With Venous Invasion - The "Whipple at The Splenic Artery (WATSA) " Procedure PDFDocumento7 pagine2012-03 - Resection of Tumors of The Neck of The Pancreas With Venous Invasion - The "Whipple at The Splenic Artery (WATSA) " Procedure PDFNawzad SulayvaniNessuna valutazione finora
- Deep Vein Thrombosis FlyerDocumento2 pagineDeep Vein Thrombosis FlyerMuhammad Reza Syahli PiliangNessuna valutazione finora
- Dog Heart (Plastinated)Documento3 pagineDog Heart (Plastinated)Roger CallNessuna valutazione finora
- Pelvic ThrombophlebitisDocumento12 paginePelvic ThrombophlebitisMicah Magallano100% (1)
- AVBS2001Documento81 pagineAVBS2001Celine Berjot100% (1)
- The Hazards: OF Blood TransfusionDocumento7 pagineThe Hazards: OF Blood TransfusionPranjal Kr SahariaNessuna valutazione finora
- Guia Esvs Manejo Evc 2015Documento60 pagineGuia Esvs Manejo Evc 2015Steeven Ruilova Valle100% (1)
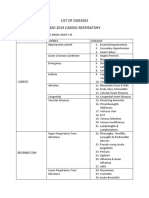
- List of Diseases Imo 2019 Cardio-RespiratoryDocumento2 pagineList of Diseases Imo 2019 Cardio-RespiratoryDimas Adjie Yuda MahendraNessuna valutazione finora
- CVS MonitoringDocumento33 pagineCVS MonitoringMicheal NorrisNessuna valutazione finora
- Med Term Study GuideDocumento706 pagineMed Term Study GuideJesse LeonardNessuna valutazione finora
- Anesthesia For Maxillofacial ProcedureDocumento90 pagineAnesthesia For Maxillofacial ProcedureShalini Thakur Dubey0% (2)
- Systemic CirculationDocumento3 pagineSystemic CirculationWira SentanuNessuna valutazione finora
- TV MCQ Pertanyaan TokDocumento5 pagineTV MCQ Pertanyaan TokdhinahafizNessuna valutazione finora
- Science - G9 - Week 2 (Lessons-4-6)Documento46 pagineScience - G9 - Week 2 (Lessons-4-6)Rhyan Zero-four BaluyutNessuna valutazione finora