Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
CVA - Compilation of All Books
Caricato da
Johnpeter Esporlas0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
74 visualizzazioni4 pagineCVA sem reviewer
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCVA sem reviewer
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
74 visualizzazioni4 pagineCVA - Compilation of All Books
Caricato da
Johnpeter EsporlasCVA sem reviewer
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 4
John Peter Lovingski R. Esporlas b.
Chronic Stable Atrial Fibrillation
- 5 times
CVA c. Rheumatic Heart Disease + Atrial Fibrillation
- 17 times for embolic
- Non-traumatic, vascular cause, sudden neurologic
3. Diabetes Mellitus
deficit. - 3-6 times
Most Common Sign - 2 times as independent risk factor
- 2 times (De Lisa)
- Focal Weakness; it can produce a wide range of 4. Cigarette Smoking
symptoms such as sensory loss, speech & a. Heavy
language, disturbance, visual loss. - >40 cigarettes per day
- 2 times
Epidemiology b. Light
- <10 cigarettes per day
- Old>Young c. 5 years cessation
- >3 years from childhood stroke - Risk equal to normal
- <45 y/o for young stroke 5. Hypercholesterolemia
- Male>Female - Indirect risk factor for stroke
- Female>Male; if >85 y/o - Total for LDL & HDL: <200mg/dL
- Race a. Low-Density Lipoprotein
a. Black>White - <100 mg/dL
b. Asian>US b. High-Density Lipoprotein
- >60 mg/dL
Pathophysiology
6. Obesity
Process 7. Sedentary Lifestyle
8. Lack of Exercise
1. Focal Infarction & Ischemic Penumbra 9. Diet
- If the brain does not achieve blood flow at a 10. Heavy Alcohol Consumption
specific type; it will result to INFARCTION 11. Oral Contraception + Estrogen
2. Cerebral Edema
- Swelling of the brain TIA (Transient Ischemic Attack)
- Middle Cerebral artery has the largest cerebral - Asymptomatic carotid bruit
edema because it has 2 branches. - Carotid Bruit (Carotid Stenosis); Narrowing or
3. Increase Intracranial Pressure constricting of the carotid arteries.
4. Herniation
- (MC: Middle Cerebral Artery & Internal Carotid Risk Factors
Artery)
1. Hematocrit (Hct)
Signs & Symptoms - Faster blood clotting time
2. Serum Fibrinogen
Altered Level of Consciousness (coma, decreased - Faster coagulation
arousal levels) 3. Elevated C-Reactive Protein:
Widened pulse pressure - inflammatory marker due to endothelial injury
Increased HR 4. Elevated Homocysteine
Cheyne-Stokes Respiration - Can result from inherited or acquire enzyme
Vomiting deficiencies such as folate, B6, B12 and may
Unreacting pupils increase viscosity
Papilloedema
Metabolic Syndrome
Risk Factors (Modifiable)
- It is a cluster of interrelated metabolic risk factors
Lifestyle
for atherosclerotic disease.
1. Hypertension - 5 times risk if the following 5 are present
- Most significant risk factors 1. High Waist Circumference
- >165/95 mmHg (Braddom) 2. Increased Blood Pressure
- Parallel risk for Systolic Blood Pressure & Mean 3. Low HDL level
Arterial Pressure 4. Elevated serum triglyceride
2. Heart Disease 5. Elevated fasting glucose
- 2-6 times Non- Modifiable
a. Coronary Artery Disease
- 2 times - Race
- Age Cause:
- Sex
- Previous Stroke; Adults: Atherosclerosis; Thrombosis is the usual cause
Classification: (Temporal) Younger Patient: t/c inherited disease that cause
thrombophilia; probable inherited defects; abnormal
1. TIA increase platelets coagulation disorder is inherited thats
- A brief episode of neurologic dysfunction caused why patient has thrombophilia
by focal brain or retinal ischemia with clinical
symptoms typically lasting less than an hour and Children: Various (cerebrovascular anomalies, congenital
without evidence of acute infarction as heart disease, carotid dissection, sickle cell disease,
determined by cranial imaging (Braddom) inherited disorders of coagulation, and previous infection
- Within 24 hours, full resolution may show small with varicella zoster; hemorrhagic causes include
acute infarction in MRI moyamoya disease & hemophilia)
- No longer defined by time
- <1hr without evidence of acute infarction Ischemic
- Infarction on imaging is considered a stroke
- mortality is higher in large lesions with edema and
- Complete resolution, affects watershed zone
brain shift, areas of reduced flow
- CBF (Cerebral Blood Flow): <20-30 ml per 100
- (gCBF in normal hemisphere d/t diachisis, if
g/mL
rCBF <28 increase infarction) & increased flow
Causes (luxury perfusion d/t arteriolar vasodilation)
- Diaschisis- sudden loss (or change) of function in
Hemodynamic a portion of the brain connected to a distant, but
damaged, brain area.
- Hypoperfusion
- Insufficient of blood in one area, shift of blood LOOKUP IMPLICATION of CBF Values
- Subclavian Steal Syndrome stenosis of the
proximal subclavian artery; one side may manifest 1. Normal Cerebral Autoregulation
hypoxia; it may return to normal when rest; (-) - 50 mL/100g cerebral tissue/min
infarct when seen on MRI 2. Cerebrovascular Compromise
- Retrograde from the Vertebral Artery - 20 mL/ 100 g cerebral tissue/min
3. Cellular Death
Embolic - <10 mL / 100 g cerebral tissue/min
4. Sodium Potassium Pump Failed
- This is where usual embolus is found - 10-20mL/ 100g cerebral tissue/min
- Most common cause; most common in anterior
circulation Classification
- Faster occlusion but faster recovery
- (+) Dislodge of thrombus; not related in HTN Thrombotic (40%) Atherosclerosis
- Hemiplegic+ increase BP= severe stroke
- Atherosclerotic plaque is most common in
Reversible Ischemic Neurologic Deficit Common Carotid Artery & Vertebrobasilar Artery
- Dependent on the length of time the vessel is
- TIA>24 hours, temporary impairments within 3 occluded, the rate of flow through the occluded
weeks site and the effectiveness of the collateral
- Initial Symptom: Sudden fall weakness, after circulation
few weeks faster recovery - Collateral Circulation can be less effective in
- Some symptoms may still return, if infarct related elderly, diffuse atherosclerotic disease and DM
for more than 3 weeks; the area was perfused so it
will be on faster recovery Signs & Symptoms
Stroke in Evolution - Subtle & Gradual Onset
- Unstable, progressive Embolic (20%)
- Thrombus is a serious problem; it is starting to
- Most common in Middle Cerebral Artery
occlude the arteries & multiple vessels
- Majority are thromboembolism
- 1 st Localized effect Increased symptoms per day
Sources:
Completed Stroke
Cardiogenic
- Stable
- Neurological deficit must persist at least 24 hours - (+) Atrial Fibrillation
- Aysmptomatic, only one blood area, generally via Hemorrhagic
gravity, there is decrease of pressure blood will
pull downward, it will not flush down properly - Manifestation: Headache
1. Intracerebral (10%)
that is why there is formation of blood clot in the
- Deep perforating arteries, but does not obey
area.
anatomic distribution of vessel as compared to
- Arrhythmias; Atrial Fibrillation & Atrial Thrombus
- Valvular heart disease lacunar stroke, but dissects through tissue
- Mechanical/prosthetic valve, esp. if planes/parenchyma increase ICP, disruption of
anticoagulation is insufficient neural tracts, ventricular compression, herniation
- Acute mortality is high, rapid recovery 2-3 months
VEGETATIONS after injury
- Areas: Putamen & White matter
- verrucae (small warty vegetations along the lines - Causes
of closure of valve leaflets) in RHD a. Hypertension
- septic emboli from infectious/infective (bacterial) - Most common cause
endocarditis - microvascular changes: lipohyalinosis, Charcot-
- Mural Thrombus: in recent MI, hypokinesis, Bouchard aneurysms (pseudoaneurysms
cardiomyopathy, cardiac surgery microscopic ruptures)
- Paradoxical Emboli: Through (L) & cardiac - bleeding usually lasts for 1-2 hours, late
shunt (e.g patent foramen ovale) neurologic decline can be attributed to
- Atrial Myxoma: Primary Tumors of the heart posthemorrhagic edema or rebleeding
- Cholesterol emboli: atherosclerotic debris - Most common: Putamen & thalamus
- Air Emboli: neck, thoracic surgery it will go b. Cerebral amyloid angiopathy
straight to the brain - Elderly, MC >65 y/o, usually lobar than deep, MRI
- Fat Emboli: evidence of hemosiderin deposition indicative Hx
of microhemorrhage
Signs & Symptoms
- >55 y/o, with Hx of mild dementia, lobar
- Abrupt onset hemorrhage near cortex, amyloid deposits on
- Some fragment may break to small pieces as they adventitia
travel through the cerebral circulation c. Others
- Multiple small infarcts affecting several distal - Trauma, vasculitis, coagulation d/o, anticoagulant
branches of the main vessel therapy, bleeding into tumor
- Lysis & Fragmentation 2. Intraventricular
- Full Resolution - Loss of consciousness
- Without previous or progressive symptoms
- Reperfusion can occur in response to endogenous Signs & Symptoms
fibrinolysis, but may lead to 2 cerebral - severe headache -> progressive neurologic
hemorrhage since the capillaries become deficits -> coma, brain shift/displacement d/t
incompetent due to ischemic damage hematoma and cerebral edema and lead to
Lacunar: (20%) transtentorial herniation death; hematomas may
continue to expand, large posterior fossa lesions
- Area of lacune corresponds to vascular territory (e.g. acute cerebellar hemorrhages) occlusion
supplied by one of the deep perforating branches of 4th ventricle acute hydrocephalus
(Braddom)
- At most 1.5 cm diameter (De Lisa)
- Less than 1.5 cm (Braddom)
- blood coagulum can block foramen of Sylvius or
- Lacune: Refers to the small vessels found at the
4th ventricle -> acute obstructive hydrocephalus
deeper part of the brain.
- Areas: basal ganglia, internal capsule, pons,
cerebellum (Braddom) Sub-arachnoid (5%)
- + thalamus, brainstem (De Lisa)
Causes
Signs & Symptoms
- Saccular Aneurysm: 5th to 6th decade, MC
- May result to major neurologic deficits, minor anterior portion of Circle of Willis, >10mm
symptoms or even asymptomatic greatest risk of bleeding, intervention is advised
- Arteriovenous Malformation: 2nd-3rd decade,
Others
MC in MCA, tangle of dilated vessels
- Cerebral Vasculitis or cerebral hypoperfusion - Mycotic Vessels: Vessel wall infection
Signs
In Aneurysm
- Localized CN lesion can develop from direct
pressure of expanding aneurysm, headache can
occur from small bleed prior to major rupture
- major rupture will result to severe headache ->
meningism
- worst headache in my life
- Focal neurologic signs does not occur initially but
may develop due to intracerebral bleeding or
infarction (d/t arterial vasospasm caused by blood
in subarachnoid space)
- coma, acute death and rebleeding is more
common in aneurysm than AVM
- acute LOC is due to sudden decrease cerebral
perfusion pressure
- Hydrocephalus: immediate after intraventricular
hemorrhage, or a later complication of
arachnoiditis (d/t blood in CSF)
- poor prognosis for proximate survival: coma,
stupor, severe hemiplegia
IN AVM
- Can grow large and displace neural structures
without disruption of function
- MC initial indication of lesion hemorrhage (most
patients survive a single hemorrhagic event)
- Seizure, migraine & hemorrhage
- Hypertensive: >170/90 mmHg
Others: vasculitis, hypoperfusion
Neuroanatomical:
ICA: manifestation ACA + MCA
Can manifest ACA if ACOM problem; if wala symps
niya is usually MCA
Tagal madevelop thrombus; extend ng collateral
circulation -> neurological symp
Some cases: Walang nangyayari sobrang tagal ->
gawa sariling circulation
-Pre existing stenosis + nabara sa kabila
BICORTICAL presentation
1st Branch: Opthalmic artery: supplies retina
(globe of eyes)
-monocular blindness
-field of vision loss; unilat
BRACHIOCEPHALIC TRUNK
-symptoms of ICA; extremity circulation affected
(cyanosis); hemiplegia of kabila LE
-very rare
HYPOTENSION: WATERSHED ZONE watershed
infarcts
-area kung saan ambon lang yung circulation
CARDIAC ARREST: bilat symmetric
Nagsisimula na watershed din, dec blood supply
CRESCENT SHAPED INFARCRTS bilat.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- SLE Made EasyDocumento482 pagineSLE Made EasySumayyia Qamar100% (1)
- Sickle Cell AnemiaDocumento63 pagineSickle Cell Anemiaoss-20502745100% (4)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Id No.: CVD/NCD Assessment Form For Adults 20 Years Old and AboveDocumento1 paginaId No.: CVD/NCD Assessment Form For Adults 20 Years Old and AboveNel Jerez67% (3)
- KneeDocumento14 pagineKneeJohnpeter Esporlas100% (1)
- Frequency DR Hulda Clark ZapperDocumento45 pagineFrequency DR Hulda Clark ZapperkwbutterfliesNessuna valutazione finora
- CVA Bleed vs. InfarctDocumento33 pagineCVA Bleed vs. InfarctPaul Henry RoxasNessuna valutazione finora
- Mes 3Documento4 pagineMes 3Johnpeter EsporlasNessuna valutazione finora
- MOSCO'S CLERKING GUIDEDocumento88 pagineMOSCO'S CLERKING GUIDEtemitopeNessuna valutazione finora
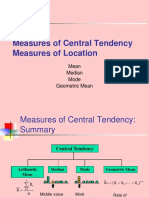
- Central TendencyDocumento25 pagineCentral TendencyJohnpeter EsporlasNessuna valutazione finora
- Amyotrophic Lateral SclerosisDocumento3 pagineAmyotrophic Lateral SclerosisJohnpeter EsporlasNessuna valutazione finora
- CBR Topic Outline 2017-2018Documento3 pagineCBR Topic Outline 2017-2018Johnpeter EsporlasNessuna valutazione finora
- Renr Practice Test 9 FinalDocumento12 pagineRenr Practice Test 9 FinalTk100% (2)
- Assistive Devices RealDocumento3 pagineAssistive Devices RealJohnpeter EsporlasNessuna valutazione finora
- B. The Contrecoup Injury Occurs Directly Opposite To The Point of ImpactDocumento4 pagineB. The Contrecoup Injury Occurs Directly Opposite To The Point of ImpactJohnpeter EsporlasNessuna valutazione finora
- Achalasia: Proximal Dysphagia Due To Neuromuscular Cause Distal Dysphagia Due To Mechanical ObstructionDocumento10 pagineAchalasia: Proximal Dysphagia Due To Neuromuscular Cause Distal Dysphagia Due To Mechanical ObstructionJohnpeter EsporlasNessuna valutazione finora
- Is There Anything Left to Trust? - 40-character for document on trusting the BibleDocumento28 pagineIs There Anything Left to Trust? - 40-character for document on trusting the BibleJohnpeter EsporlasNessuna valutazione finora
- Introduction To PharmacologyDocumento6 pagineIntroduction To PharmacologyJohnpeter EsporlasNessuna valutazione finora
- Bell's PalsyDocumento9 pagineBell's PalsyJohnpeter EsporlasNessuna valutazione finora
- Parables of Jesus ChristDocumento4 pagineParables of Jesus ChristJohnpeter EsporlasNessuna valutazione finora
- Pediatric Milestones Age Gross Motor Fine Motor Personal/Social Speech and LanguageDocumento3 paginePediatric Milestones Age Gross Motor Fine Motor Personal/Social Speech and LanguageJohnpeter EsporlasNessuna valutazione finora
- Postpolio SyndromeDocumento3 paginePostpolio SyndromeJohnpeter Esporlas100% (1)
- ReviewDocumento10 pagineReviewJohnpeter EsporlasNessuna valutazione finora
- Electrotherapy Parameters For Grand PraxDocumento3 pagineElectrotherapy Parameters For Grand PraxJohnpeter EsporlasNessuna valutazione finora
- TEP 2 Syllabus and Course Overviews for Physiotherapy ModulesDocumento2 pagineTEP 2 Syllabus and Course Overviews for Physiotherapy ModulesJohnpeter EsporlasNessuna valutazione finora
- Chapter 12Documento22 pagineChapter 12John EmmanuelNessuna valutazione finora
- Down SyndromeDocumento2 pagineDown SyndromeJohnpeter EsporlasNessuna valutazione finora
- Tep 11 Reflexes PrintoutDocumento2 pagineTep 11 Reflexes PrintoutJohnpeter EsporlasNessuna valutazione finora
- Effects of Prolonged Immobilization on the Musculoskeletal SystemDocumento14 pagineEffects of Prolonged Immobilization on the Musculoskeletal SystemJohnpeter EsporlasNessuna valutazione finora
- Patient Survey Results Guide Practice ImprovementsDocumento6 paginePatient Survey Results Guide Practice ImprovementsJohnpeter EsporlasNessuna valutazione finora
- Cardiovascular RehabilitationDocumento5 pagineCardiovascular RehabilitationJohnpeter EsporlasNessuna valutazione finora
- Normal Body TemperaturesDocumento5 pagineNormal Body TemperaturesJohnpeter EsporlasNessuna valutazione finora
- SHOULDER PAIN AND INJURY GUIDEDocumento7 pagineSHOULDER PAIN AND INJURY GUIDEJohnpeter EsporlasNessuna valutazione finora
- Neuroanatomy Pictures Part 2 - WaxmanDocumento6 pagineNeuroanatomy Pictures Part 2 - WaxmanJohnpeter EsporlasNessuna valutazione finora
- Atlas of Digestive SystemDocumento3 pagineAtlas of Digestive SystemJohnpeter EsporlasNessuna valutazione finora
- Anthropometric SDocumento3 pagineAnthropometric SJohnpeter EsporlasNessuna valutazione finora
- Etiology, Epidemiology & Differential Diagnosis For CADDocumento9 pagineEtiology, Epidemiology & Differential Diagnosis For CADJohnpeter EsporlasNessuna valutazione finora
- 40 - Advances in Motion and Electromyography Based Wearabletechnology For Upper Extremity Function Rehabilitation A ReviewDocumento7 pagine40 - Advances in Motion and Electromyography Based Wearabletechnology For Upper Extremity Function Rehabilitation A Reviewmihaela_986230018Nessuna valutazione finora
- Medical Questionnaire For PatientsDocumento1 paginaMedical Questionnaire For Patientsjrepko1Nessuna valutazione finora
- Prevalence and Impact of Pain Among Older Adults in The United StatesDocumento9 paginePrevalence and Impact of Pain Among Older Adults in The United StatesLucas TarquiNessuna valutazione finora
- Saxion Physiotherapy Curriculum OverviewDocumento22 pagineSaxion Physiotherapy Curriculum OverviewGretel EdelweissNessuna valutazione finora
- Healthmedicinet I 2017 5Documento630 pagineHealthmedicinet I 2017 5tuni santeNessuna valutazione finora
- Treatment of Upper Extremity Spasticity in Stroke Patients by Focal Neuronal or Neuromuscular Blockade: A Systematic Review of The LiteratureDocumento11 pagineTreatment of Upper Extremity Spasticity in Stroke Patients by Focal Neuronal or Neuromuscular Blockade: A Systematic Review of The LiteraturemitroisergiuNessuna valutazione finora
- Contoh Soal KMB Ujikom 1Documento34 pagineContoh Soal KMB Ujikom 1RobbyNessuna valutazione finora
- Overview of Primary Prevention of Coronary Heart Disease and Stroke - UpToDateDocumento15 pagineOverview of Primary Prevention of Coronary Heart Disease and Stroke - UpToDatethanh phung phamNessuna valutazione finora
- DynaMed Plus - Stroke (Acute Management)Documento126 pagineDynaMed Plus - Stroke (Acute Management)Sarah Shafa MarwadhaniNessuna valutazione finora
- Hubungan Gerd Dengan DepresiDocumento8 pagineHubungan Gerd Dengan DepresiDella Elvina RoeslandNessuna valutazione finora
- Padillo Vs Rural BankDocumento6 paginePadillo Vs Rural BankheymissrubyNessuna valutazione finora
- Stroke Incidence and Case Fatality in AustralasiaDocumento7 pagineStroke Incidence and Case Fatality in AustralasiaChintya Anugrah SuhendraNessuna valutazione finora
- European Stroke ScaleDocumento3 pagineEuropean Stroke ScaleAbdur RasyidNessuna valutazione finora
- 328 IndexDocumento29 pagine328 IndexDafi SanNessuna valutazione finora
- Comparison of CT and MR Imaging in Ischemic StrokeDocumento10 pagineComparison of CT and MR Imaging in Ischemic Strokeتغريد عبادةNessuna valutazione finora
- Neuromuscular Therapy Techniques for Stroke and MS RehabilitationDocumento11 pagineNeuromuscular Therapy Techniques for Stroke and MS RehabilitationWenzy Razzie cruzNessuna valutazione finora
- Shep TrialDocumento10 pagineShep TrialOlayemi OladiranNessuna valutazione finora
- Ezetimibe Added To Statin Therapy After Acute Coronary SyndromesDocumento11 pagineEzetimibe Added To Statin Therapy After Acute Coronary SyndromesAngela DelarmenteNessuna valutazione finora
- Ijms 13 11753 PDFDocumento20 pagineIjms 13 11753 PDFVandy IkraNessuna valutazione finora
- Advances in Intracranial HemorrhageDocumento15 pagineAdvances in Intracranial HemorrhageJorge GonzalesNessuna valutazione finora
- Impact of High Altitude On Cardiovascular Health: Current PerspectivesDocumento19 pagineImpact of High Altitude On Cardiovascular Health: Current PerspectivesveronicaNessuna valutazione finora
- 16 Vascular Diseases of Nervous System-QDocumento24 pagine16 Vascular Diseases of Nervous System-QAdi PomeranzNessuna valutazione finora
- Secure your family's future with this adjustable life insurance planDocumento25 pagineSecure your family's future with this adjustable life insurance planaaaNessuna valutazione finora