Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Safety Ra Pediatrics
Caricato da
DellDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Safety Ra Pediatrics
Caricato da
DellCopyright:
Formati disponibili
Pediatric Anesthesia ISSN 1155-5645
REVIEW ARTICLE
Safety in pediatric regional anesthesia
Claude Ecoffey
Service dAnesthesie-Reanimation 2, Hopital Pontchaillou, Universite Rennes 1, Rennes, France
Keywords Summary
morbidity; outcomes; regional; ultrasound;
local anesthetics; drugs; adverse events; The use of regional anesthesia is increasingly common in pediatric practice.
complications This review reports the complications and risks in pediatric regional
anesthesia. Few large studies reported incidence of complications. How-
Correspondence ever, the different studies have shown that regional anesthesia, when per-
Claude Ecoffey, Service dAnesthesie-
formed properly, carried a very low risk of morbidity in appropriately
Reanimation 2, Hopital Pontchaillou,
Universite Rennes 1, 35033-Rennes, France
selected infants and children. In addition, the use of ultrasound-guided
Email: cecoffey.rennes@invivo.edu peripheral nerve blockade has shown some promise toward increasing the
safety prole of these already safe techniques.
Accepted 17 August 2011
Section Editor: Per-Arne Lonnqvist
doi:10.1111/j.1460-9592.2011.03705.x
Introduction duration, reduction in volume of local anesthetic
agents required.
Pediatric regional anesthesia has attained wide use
Performing a regional block may result in different
internationally because of its efcacy and safety; its
complications, most of which could have been avoided
use is supported by the existence of extensive data
by learning the correct technique, using an appropriate
from the international literature (14). Safer drugs and
equipment, and applying the very basic safety rules.
dedicated pediatric tools are the keys to this success.
This is so despite the fact that general anesthesia is
necessary in most children for the regional block to be
General epidemiology of complications
performed easily, safely, and effectively. Indeed, place-
ment of regional blocks of all types under general Complications were rare and similar in both ADA-
anesthesia is considered the standard of care in pediat- RPEFs studies (1,4). As reported in the literature,
rics (5). A common logical argument is that there is they were more frequent (four times in the recent
less risk of injury when placing a needle in an immo- ADARPEF study) in children aged <6 months that
bile child than in one who is struggling or might move in children aged >6 months (Table 1). Central regio-
unpredictably. nal anesthesia has the highest incidence of complica-
The benet/risk ratio is excellent especially for tions (six times higher that peripheral). Moreover,
peripheral blocks, even when beginners perform them. their incidence remained low despite an increase in
All the regional blocks necessitate complete knowledge use in the last 12 years. Complications have not
of the anatomic landmarks, and specialists in pediatric reached extreme severity, despite results from a UK
anesthesia should supervise the training in their perfor- audit (5 years, 10 633 epidurals performed) reporting
mance in order to prevent repetitive errors. Despite its permanent residual neurologic decit in a child aged
well-known benets, clinical failures can occur during 3-month (1-year follow-up), two epidural abscesses,
the application of regional anesthetic techniques. one case of meningism, one postdural puncture head-
Ultrasound guidance has been shown to improve block ache requiring active blood patching, and one drug
characteristics, resulting in shorter block performance error resulting in cauda equina syndrome (2). The UK
time, higher success rates, shorter onset, longer block audit also reported ve cases of severe neuropathy/
Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd 25
Safety in pediatric regional anesthesia C. Ecoffey
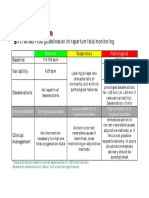
Table 1 Incidence of complications according to the age (n = 41) (4)
030 days 030 days 16 months 16 months 6 months
premature full term premature full term to 3 years 312 years >12 years
Complications n = 121 n = 475 n = 822 n = 2442 n = 10 499 n = 12 974 n = 3799
% of studied population 0.4 1.5 2.6 7.8 33.7 41.7 12.2
Relative % of complications 2.4 2.4 7.3 17.1 17.1 39 14.6
% of complications in the group 0.8 1 0.02 0.3 0.06 0.13 0.05
radiculopathy resolving over a period of 410 months cultured from the tips of the epidural catheters were
using pharmacological therapy in a Pain Clinic. The most frequently Staphylococcus aureus and coagulase-
recent ADARPEF study records a very low overall negative staphylococci (11).
morbidity for peripheral blocks, almost six times
lower than that in central regional anesthesia. Despite
Complications of central blocks
two colonic punctures, it should encourage anesthesi-
ologists to use peripheral rather than neuraxial Complications related to the technique
(including caudal) blocks as often as possible when The technique of nerve/space location may produce
appropriate. The use of catheters does not seem to complications. These include nerve damage, compres-
increase the occurrence of complications, even if car- sive hematoma, and denitive paraplegia, but also
diac toxicity following a secondary injection through a complications related to the medium used for the loss-
catheter was attributed to an inadvertent displacement of-resistance technique used to identify the epidural
of the catheter. Some complications (at least drug space, such as dilution and increase in the injected vol-
error, wrong side, lower limbs rising resulting in ume of local anesthetic if saline is used and headache,
extended spinal blockade) were avoidable. In the patchy anesthesia, lumbar compression, multiradicular
recent ADARPEF study, local anesthetic toxicity syndrome, subcutaneous cervical emphysema, or
resulted in one case of convulsions while the UK embolism if air is used.
audit reported only two respiratory arrests and one Epidural abscess, meningitis, arachnoiditis, radicul-
seizure following central regional anesthesia. They did opathies, discitis, and vertebral osteitis have been
not require treatment with Intralipid as reported in a reported following central blocks (2). Interposed bacte-
child (6). Some other complications (such as extended rial lters are effective in preventing contamination of
spinal anesthetics in two ex-premies, drug error and a the local anesthetic solution. Inadvertent dural punc-
part of cardiac toxicity) were probably also avoidable. ture with subsequent intrathecal injection of an epidu-
The Pediatric Regional Anesthetic Network (PRAN) ral dose of local anesthetic results in total spinal
database did not report any permanent nerve injuries anesthesia, the clinical expression of which is almost
from blocks of any type, and one only case of tran- immediate respiratory arrest requiring rapid control of
sient dysesthesia following a sciatic nerve block that ventilation and, in adolescents, cardiovascular collapse.
resolved within 6 months (3). Subdural injection results in a delayed (20 min) and
Large retrospective analyses of infections of epidural short-duration (60 min) block with an extensive distri-
catheters have been reported in two series of children bution of analgesia (involving sometimes cranial
(79). The main risk factor are long-term catheter nerves up to the fth pair) but with no or minimal
placement (3 days) (9), cancer, or acquired immuno- motor and sympathetic blockade. The injection of
deciency syndrome patients. Fortunately, the authors large volumes may result in excessive spread of the
conrmed that soft tissue infection manifesting as cel- local anesthetic, which can reach distant nerves, or in
lulitis and pus at epidural catheter exit is the main too high levels of epidural/spinal anesthesia with sub-
infectious complications with a good outcome. Several sequent respiratory failure because of intercostal mus-
routes might be possible for the introduction of micro- cle paralysis (above T4), or even in diaphragmatic
organisms into the epidural space. Infection might paralysis (C4).
originated from the skin ora particularly if several Finally, postdural puncture headache is a common
attempts have injured the skin (10), hematological complaint after spinal anesthesia in adults and has
spread of bacteria, contamination of the local anes- been reported to develop also in children under
thetic solution, or direct contamination of the catheter 10 years (12,13). Nonetheless, a much lower incidence
during its insertion. However, the microorganisms and severity of postdural puncture headache in
26 Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd
C. Ecoffey Safety in pediatric regional anesthesia
children have been reported during spinal anesthesia Local anesthetic toxicity
with a use of 2429-G needles (13). However, epidural
Systemic
blood puncture with 0.20.3 mlkg)1 of autologous
During the early phase of the introduction of regional
blood is an effective treatment for severe and persistent
anesthetic techniques into routine pediatric anesthetic
headache in young children (14).
practice, the safe doses of local anesthetics had not
been determined and, as a result, numerous case
Complications of the catheters reports of local anesthetic toxicity were published,
including both convulsions and cardiovascular compli-
Insertion of an epidural catheter can lead to several
cations. However, safe dosing guidelines for the use of
complications: misplacement, kinking, knotting, rup-
bupivacaine in newborns, infants, and children were
ture (especially if attempts are made to withdraw the
issued by Berde (18). With widespread adherence to
catheter through the epidural needle). Secondary
these recommendations, reports of systemic toxicity
migrations into the subarachnoid space, a blood ves-
from overdose of local anesthetic seem to have almost
sel, the subdural space, or the paravertebral space
disappeared, but no publication bias is possible. A
are very rare. Leakage around the puncture point
much debated issue is whether larger doses can be per-
occurs in approximately 10% of cases, more fre-
mitted when using the more modern and less toxic
quently with smaller catheter (15), and inadvertent
long-acting local anesthetics, ropivacaine and levobupi-
removal is not infrequent. Some pediatric cases of
vacaine. However, it should be remembered that the
catheter infection have been reported. Complications,
quality of a block is only very rarely improved by the
such as cutting and knotting, become apparent only
administration of more than the maximum recom-
on removal of the catheter; in most cases, they are
mended dose of local anesthetic. The use of ultrasound
directly related to the length of catheter introduced
guidance is associated with the need for lower volumes
into the epidural space, which should not exceed 2
of local anesthetic (Table 2), and may therefore
4 cm. The frequency of catheter-related complications
improve the safety margin for systemic toxicity by the
has been noted to be as high as 11% in a pediatric
use of lower total doses of local anesthetic.
series (15).
Local
Complications of peripheral blocks
Continuous peripheral nerve blocks have been pro-
Complications related to the technique
posed as an effective technique for postoperative pain
When block needles are used blindly, they may dam-
relief and chronic pain therapy, particularly in small
age a nerve trunk, especially when they are impru-
children. Only one clinical report has described myo-
dently inserted. In addition, the use of ultrasound
toxicity induced by bupivacaine in a child scheduled
does not always show the tip of the needle, espe-
for cataract surgery performed with peribulbar anes-
cially among beginners (16). Vascular lesions may
thesia (19), in contrast with a larger number of obser-
lead to compressive hematoma. Other tissue lesions
vations in adults. Bupivacaine-induced myotoxicity can
such as arterial wounds and pneumothorax can be
be explained by mitochondrial bioenergetics altera-
produced by attempted peripheral nerve blocks, the
tions; lower toxic effects of ropivacaine compared with
presenting symptoms of which can be delayed by
bupivacaine anesthetic-induced myotoxicity have been
several hours.
Interscalene brachial plexus, lumbar plexus, and
intercostal nerve blocks may lead to the same compli-
Table 2 Reduction in local anesthetic volume with ultrasound guid-
cations as with central blocks such as respiratory fail- ance
ure because of an epidural/spinal diffusion of local
anesthetic or a diaphragmatic paralysis following an Ultrasound Landmarks
interscalene block. guidance dosages
Technique dosages (mlkg)1) (mlkg)1)
Supraclavicular block (37) 0.3 0.5
Complications of the catheters
Infraclavicular block (32) 0.2 0.5
The indications of peripheral catheter insertion are Sciatic block (38) 0.2 0.3
fewer than those of epidural catheter. Most frequently Femoral block (38) 0.15 0.3
Rectus sheath block (39) 0.1 (each side) 0.3
reported complications with peripheral catheter
Ilio-inguinal block (40) 0.1 (each side) 0.4
involved mechanical problems as high as 20% (17).
Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd 27
Safety in pediatric regional anesthesia C. Ecoffey
reported in young rats (20). The clinical impact (22). In the PRAN database, positive test doses were
remains to be evaluated in practice, and the need for a detected in 0.6% of single injection and 0.7% of cathe-
clinical evaluation of local anesthetic myotoxicity in ter blocks (3).
young patients remains to be dened. The specicity of these changes has been questioned
recently as it seems that similar changes in heart rate
and blood pressure may be seen following a painful
Safety rules for performing regional anesthesia
stimulus (too light anesthesia during the performance
Patient monitoring of the block or intraneural injection). The temporal
Monitors should be applied and in use before any relationship is important and a secondary drop in
block is performed. In particular, the electrocardio- pulse rate detected after intravenous epinephrine dis-
gram should be adjusted so that the P wave, QRS tinguishes this from the response seen after a painful
complex, and upright T wave can be seen clearly. stimulus (23). Nonetheless, as no method of test dosing
Baseline systolic blood pressure and heart rates should is infallible, incremental injection is a critical safety
be noted. technique over a period of at least 60120 s, irrespec-
tive of the type of block, with repeated aspirations,
whenever large volumes of local anesthetics are
Skin preparation
injected (24). Direct visualization of the location of the
Bacterial colonization of epidural and caudal catheters needle tip and the injectate with ultrasound may pro-
in children occurs at a rate of 635%. Gram-positive vide additional or alternative conrmation of lack of
organisms are most common, though Gram-negative iv injection (25).
colonization may also occur, particularly with caudal
catheters. Children under 3 years of age are also most
Sympathetic tone
likely to have colonization of caudal catheters. Despite
high rates of colonization, serious epidural infections A clinically signicant decrease in blood pressure
are exceedingly rare (2,9). Disinfecting the skin with an related to sympathectomy from central neuraxial
alcoholic solution has proved to be effective in decon- blocks is rare in children younger than 8 years of age
taminating the transient skin ora (21), but not the (26), except in neonates following spinal block (27,28).
deeply placed resident ora, which remains colonized Volume loading before such blocks, commonly prac-
even after skin disinfection. In addition, insertion of ticed in adults, is unnecessary in this age group. In
an epidural catheter should be performed under strict older patients, the sympathetic block results in a slight
aseptic conditions with a daily observation of exit site (2025%) but consistent decrease in blood pressure.
while the catheter is in place and for 72 h after cathe- Even in adolescents, however, uids or vasopressors
ter removal. are rarely required to treat the hemodynamic effects of
central neuraxial blocks, excepted when clonidine is
added to local anesthetics.
Test dose
While placement of regional blocks under general
Contraindications
anesthesia is considered standard practice in children,
the search for the ideal test dose to reduce the risk of Contraindications are few and similar to those in
inadvertent intravascular injection continues. The ori- adults. These include coagulopathy, infection at the
ginal test dose described an increase in heart rate and needle insertion site, true local anesthetic allergy, and
blood pressure following intravenous administration abnormal supercial landmarks or lumbosacral myelo-
of epinephrine 0.5 lgkg)1. In children, these hemody- meningocele because of the risk of malposition of the
namic changes vary with the anesthetic agent used cord or dural sac. Progressive neurologic disease is a
(halothane, sevourane, isourane, or propofol) and relative contraindication primarily because of medico-
whether prior atropine has been administered. How- legal concerns. The safety of central neuraxial tech-
ever, an increase in heart rate of 10 bmin)1 above niques in the presence of a ventriculoperitoneal shunt
baseline occurring within 1 min of injection is a rea- is discussed: indeed, the major risk of performing a
sonable sign of intravascular injection for children caudal or epidural block in a child with a ventricular
anesthetized with sevourane. Monitoring the ECG shunt device is not infection but modications of intra-
changes, i.e., >25% change in T wave or ST segment cranial pressure (29). Risks and benets in these
changes irrespective of the ECG lead chosen, is consid- patients should be carefully considered on an individ-
ered by some to be more specic and more reliable ual basis.
28 Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd
C. Ecoffey Safety in pediatric regional anesthesia
Although it is rare to encounter opposition to the Importance of proper education and training
use of peripheral nerve blocks, certain conditions may
The use of ultrasound to locate nerves is increasingly
call for a judicious avoidance of them. Relative contra-
used in pediatric patients as it increases the speed of
indications include local infection, generalized sepsis,
onset, reliability, and safety of peripheral nerve blocks.
coagulopathy, risk of compartment syndrome, and
However, using this technique to identify the nerve is
parental or child dissent.
not a replacement for a good knowledge of the anat-
omy.
Impact of ultrasound on peripheral regional anesthesia New data have emerged suggesting that the novice
on safety ultrasonographer makes repeated errors, the two most
common being failure to visualize the needle tip during
A signicant problem in regional anesthesia is that a
its progression into the tissues and unintentional move-
large number of techniques still do not achieve a suc-
ment of the probe. For this reason, the American Soci-
cess rate close to 100%. Indeed, the key to successful
ety of Regional Anesthesia (ASRA) and the European
regional anesthesia has always depended on the accu-
Society of Regional Anesthesia (ESRA) created a Joint
racy of needle and local anesthetic placement in rela-
Committee; the result was a document to recommend
tion to the nerve structures to be blocked. In 1994,
to members and institutions the scope of practice, the
Kapral introduced ultrasound guidance into regional
teaching curriculum, the fellowship program and the
anesthesia (30). Few years later, Marhofer introduced
options for implementing the medical practice of ultra-
this technique into pediatric regional anesthesia prac-
sound guided regional anesthesia services (34,35).
tice (31,32). Real-time ultrasound guidance allows the
Indeed, training in the use of ultrasound-guided
demonstration of the target, whether it is a nerve, fas-
techniques is not easy. Dedicated efforts must be made
cial plane, or anatomical space, and the monitoring of
to allow the education of at least key individuals to
the distribution of the injected local anesthetic. Fur-
attend focused training, so that these people can start
thermore, ultrasound guidance allows the anesthesiolo-
to use and teach these techniques in their own institu-
gist to reposition the needle in the case of
tions.
maldistribution of the local anesthetic. There is some
In conclusion, regional blockade in infants and chil-
evidence to support ultrasound for improving outcome
dren appears to have a very high degree of safety (36).
in pediatric regional anesthesia (33).
The use of new technologies, such as ultrasound-
Despite the theoretical advantages of ultrasound
guided regional anesthesia, has shown some promise
imaging during the performance of nerve blocks, no
toward increasing the safety prole of these already
large prospective studies in pediatrics have so far been
safe techniques. Thus, very reassuring data support the
published in support of the notion that the use of
continued use of regional anesthesia in infants and
ultrasound in fact does reduce the incidence of compli-
children.
cations compared with alternative nerve blocking tech-
niques. Because serious complications luckily are very
rare following peripheral nerve blockade in infants and Acknowledgment
children (1,3), it is unlikely that even large-scale studies
This research was carried out without funding.
will prove ultrasound guidance to be superior to other
approaches with regards to the rate of complications.
However, it does not seem reasonable to expect that Conflicts of interest
the use of ultrasound would result in an increased rate
The author has declared no conicts of interest.
of complications.
References
1 Giaufre E, Dalens B, Gambert A. Epidemi- 3 Polaner DM, Bosenberg A, Cravero J et al. anesthesia in children: a follow-up one-year
ology and morbidity of regional anesthesia Preliminary Data from the Pediatric Regio- prospective survey of the French-Language
in children: a one year prospective survey of nal Anesthesia Network (PRAN): Demo- Society of Pediatric Anesthesiologists
the French-Language Society of Pediatric graphics, Practice Patterns and (ADARPEF). Pediatr Anesth 2010; 20:
Anesthesiologists. Anesth Analg 1996; 83: Complications [Abstract]. American Society 10611069.
904912. of Anesthesiologists Annual Meeting, New 5 Krane EJ, Dalens BJ, Murat I et al. The
2 Llewellyn N, Moriarty DA. The national Orleans, LA, 2009. safety of epidurals placed during general
pediatric epidural audit. Pediatr Anesth 4 Ecoffey C, Lacroix F, Giaufre E et al. anesthesia. Reg Anesth Pain Med 1998; 23:
2007; 17: 520533. Epidemiology and morbidity of regional 433438.
Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd 29
Safety in pediatric regional anesthesia C. Ecoffey
6 Ludot H, Tharin JY, Belouadah M et al. postoperative analgesia in children: feasibil- pressure! (letter). Pediatr Anesth 2007; 17:
Successful resuscitation after ropivacaine ity and side effects in a cohort study of 339 707709.
and lidocaine-induced ventricular arrhythmia catheters. Can J Anaesth 2009; 56: 843850. 30 Kapral S, Krafft P, Eibenberger K et al.
following posterior lumbar plexus block in a 18 Berde CB. Toxicity of local anesthetics in Ultrasound-guided supraclavicular approach
child. Anesth Analg 2008; 106: 15721574. infants and children. J Pediatr 1993; 122: for regional anesthesia of the brachial
7 Strafford MA, Wilder RT, Berde CB. The S14S20. plexus. Anesth Analg 1994; 78: 507513.
risk of infection from epidural analgesia in 19 Cadera W. Diplopia after peribulbar anes- 31 Marhofer P, Schrogendorfer K, Wallner T
children: a review of 1620 cases. Anesth thesia for cataract surgery. J Pediatr Oph- et al. Ultrasonographic guidance reduces the
Analg 1995; 80: 234238. thalmol Strabismus 1998; 35: 240241. amount of local anesthetic for 3-in-1 blocks.
8 Kost-Byerly S, Tobin JR, Greenberg RS 20 Nouette-Gaulain K, Dadure C, Morau D Reg Anesth Pain Med 1998; 23: 584588.
et al. Bacterial colonization and infection et al. Age-dependent bupivacaine-induced 32 Marhofer P, Sitzwohl C, Greher M et al.
rate of continuous epidural catheters in chil- muscle toxicity during continuous peripheral Ultrasound guidance for infraclavicular
dren. Anesth Analg 1998; 86: 712716. nerve block in rats. Anesthesiology 2009; brachial plexus anaesthesia in children.
9 Sethna NF, Clendenin D, Athiraman U 111: 11201127. Anaesthesia 2004; 59: 642646.
et al. Incidence of epidural catheter-associ- 21 Kinirons B, Mimoz O, Lafendi L et al. 33 Tsui BC, Pillay JJ. Evidence-based medicine:
ated infections after continuous epidural Chlorhexidine versus povidone iodine in assessment of ultrasound imaging for
analgesia in children. Anesthesiology 2010; preventing colonization of continuous epi- regional anesthesia in infants, children, and
113: 224232. dural catheters in children: a randomized, adolescents. Reg Anesth Pain Med 2010;
10 Meunier JF, Norwood P, Dartayet B et al. controlled trial. Anesthesiology 2001; 94: 35(Suppl): S47S54.
Skin abscess with lumbar epidural catheteri- 239244. 34 Sites BD, Chan VW, Neal JM et al. The
zation in infants: is it dangerous? Report of 22 Tanaka M, Nishikawa T. Evaluating American Society of Regional Anesthesia
two cases. Anesth Analg 1997; 84: 1248 T-wave amplitude as a guide for detecting and Pain Medicine and the European Soci-
1249. intravascular injection of a test dose in anes- ety of Regional Anaesthesia and Pain Ther-
11 Du Pen SL, Peterson DG, Williams A et al. thetized children. Anesth Analg 1999; 88: apy joint committee recommendations for
Infection during chronic epidural catheteri- 754758. education and training in ultrasound-guided
zation: diagnosis and treatment. Anesthesiol- 23 Wodey E, Senhadji L, Bansard JY et al. regional anesthesia. Reg Anesth Pain Med
ogy 1990; 73: 905909. Comparison of heart rate response to an 2010; 35(2 Suppl): S74S80.
12 Kokki H, Hendolin H, Turunen M. Post- epinephrine test dose and painful stimulus 35 Regional Anesthesiology and Acute Pain
dural puncture headache and transient neu- in children during sevourane anesthesia: Medicine Fellowship Directors Group.
rologic symptoms in children after spinal heart rate variability and beat-to-beat Guidelines for fellowship training in Regio-
anaesthesia using cutting and pencil point analysis. Reg Anesth Pain Med 2003; 28: nal Anesthesiology and Acute Pain Medi-
paediatric spinal needles. Acta Anaesthesiol 439444. cine: Second Edition, 2010. Reg Anesth Pain
Scand 1998; 42: 10761082. 24 Lerman J. Local anaesthetics belong in the Med 2011; 36: 282288.
13 Kokki H, Salonvaara M, Herrgard E et al. caudal/epidural space, not in the veins! Can 36 Polaner DM, Drescher J. Pediatric regional
Postdural puncture headache is not an age- J Anaesth 1997; 44: 582586. anesthesia: what is the current safety record?
related symptom in children: a prospective, 25 Rubin K, Sullivan D, Sadhasivam S. Are Pediatr Anesth 2011; 21: 737742.
open-randomized, parallel group study com- peripheral and neuraxial blocks with 37 De Jose Mar a B, Banus E, Navarro Egea
paring 22 G Quincke with a 22 G Whitacre ultrasound guidance more effective and safe M et al. Ultrasound-guided supraclavicular
needle. Paediatr Anaesth 1999; 9: 429434. in children? Pediatr Anesth 2009; 19: 9296. vs infraclavicular brachial plexus blocks in
14 Ylonen P, Kokki H. Management of post- 26 Dohi S, Naito H, Takahashi T. Age related children. Pediatr Anesth 2008; 18: 838844.
dural puncture headache with epidural changes in blood pressure and duration of 38 Oberndorfer U, Marhofer P, Bosenberg A
blood patch in children. Paediatr Anaesth motor block in spinal anesthesia. Anesthesi- et al. Ultrasonographic guidance for sciatic
2002; 12: 526529. ology 1979; 50: 319323. and femoral nerve blocks in children. Br J
15 Wood CE, Goresky GV, Klassen KA et al. 27 Mahe V, Ecoffey C. Spinal anesthesia with Anaesth 2007; 98: 797801.
Complications of continuous epidural infu- isobaric bupivacaine in infants. Anesthesiol- 39 de Jose Maria B, Gotzens V, Mabrok M.
sions for postoperative analgesia in children. ogy 1988; 68: 601603. Ultrasound-guided umbilical nerve block
Can J Anaesth 1994; 41: 613620. 28 Bonnet MP, Larousse E, Asehnoune K in children: a brief description of a
16 Sites BD, Spence BC, Gallagher JD et al. et al. Spinal anesthesia with bupivacaine new approach. Pediatr Anesth 2007; 17: 44
Characterizing novice behavior associated decreases cerebral blood ow in former pre- 50.
with learning ultrasound-guided peripheral term infants. Anesth Analg 2004; 98: 1280 40 Willschke H, Bosenberg A, Marhofer P
regional anesthesia. Reg Anesth Pain Med 1283. et al. Ultrasonographic-guided ilioinguinal/
2007; 32: 107115. 29 Veyckemans F, Scholtes JL. Caudal block iliohypogastric nerve block in pediatric
17 Dadure C, Bringuier S, Raux O et al. Con- and ventricular shunt devices: beware of the anesthesia: what is the optimal volume?
tinuous peripheral nerve blocks for consequences of increasing epidural Anesth Analg 2006; 102: 16801684.
30 Pediatric Anesthesia 22 (2012) 2530 2011 Blackwell Publishing Ltd
Potrebbero piacerti anche
- Multi OrgasmDocumento29 pagineMulti Orgasm4gen_7100% (2)
- Mil DTL 53072CDocumento43 pagineMil DTL 53072CMichael SkrableNessuna valutazione finora
- Emergency in Respiratory MedicineDocumento73 pagineEmergency in Respiratory MedicineIndra MahaputraNessuna valutazione finora
- Year 4 OSCEguideDocumento159 pagineYear 4 OSCEguideDrSajid BuzdarNessuna valutazione finora
- Year 4 OSCEguideDocumento159 pagineYear 4 OSCEguideDrSajid BuzdarNessuna valutazione finora
- Family Planning HandbookDocumento387 pagineFamily Planning HandbookvthiseasNessuna valutazione finora
- Technical Manual: For Installation, Operation and Maintenance ofDocumento129 pagineTechnical Manual: For Installation, Operation and Maintenance ofMegan Pierce100% (1)
- OsteosarcomaDocumento25 pagineOsteosarcomaChaitra Mahesh67% (3)
- Xinnong Cheng - Chinese Acupuncture and Moxibustion 1Documento282 pagineXinnong Cheng - Chinese Acupuncture and Moxibustion 1Abrar Abizar100% (1)
- Pediatric Regional AnesthesiaDocumento6 paginePediatric Regional Anesthesiatq9prx5s5qNessuna valutazione finora
- Pediatric Regional Anesthesia: What Is The Current Safety Record?Documento6 paginePediatric Regional Anesthesia: What Is The Current Safety Record?nurfitriaNessuna valutazione finora
- Paediatric Regional AnaesthesiaDocumento9 paginePaediatric Regional AnaesthesiaAlfredo HuamaniNessuna valutazione finora
- Fundamentals and Innovations in Regional Anaesthesia For Infants and ChildrenDocumento15 pagineFundamentals and Innovations in Regional Anaesthesia For Infants and ChildrenLuisArroboNessuna valutazione finora
- Regional AnesthesiaDocumento33 pagineRegional Anesthesiashaq545Nessuna valutazione finora
- Journal AnesthesiaDocumento9 pagineJournal AnesthesiaoliviafabitaNessuna valutazione finora
- Laringo y BroncoespasmoDocumento4 pagineLaringo y BroncoespasmoLUIS FERNANDO GOMEZ CANONessuna valutazione finora
- Management of Exposed Ventriculoperitoneal Shunt On The ScalpDocumento5 pagineManagement of Exposed Ventriculoperitoneal Shunt On The ScalpDian AdiNessuna valutazione finora
- Regional Anesthesia in Pediatric Orthopedics A CL 2022Documento9 pagineRegional Anesthesia in Pediatric Orthopedics A CL 2022Alejandra SanchezNessuna valutazione finora
- Outcome Analysis of Shunt Surgery in Hydrocephalus: Riginal RticleDocumento4 pagineOutcome Analysis of Shunt Surgery in Hydrocephalus: Riginal RticleiqbalNessuna valutazione finora
- 1 s2.0 S0165587617302975 Main PDFDocumento4 pagine1 s2.0 S0165587617302975 Main PDFAchmad YunusNessuna valutazione finora
- Polan Er 2012Documento12 paginePolan Er 2012nurfitriaNessuna valutazione finora
- Empijem SinusaDocumento4 pagineEmpijem SinusaIvan GalicNessuna valutazione finora
- Journal of Clinical Anesthesia: Original ContributionDocumento6 pagineJournal of Clinical Anesthesia: Original ContributionzaimmuhtarNessuna valutazione finora
- Articles: BackgroundDocumento14 pagineArticles: BackgroundinescubertaNessuna valutazione finora
- Contemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting PositionDocumento7 pagineContemporary Analysis of The Intraoperative and Perioperative Complications of Neurosurgical Procedures Performed in The Sitting PositionLloyd AllenNessuna valutazione finora
- AygunDocumento5 pagineAygunotheasNessuna valutazione finora
- Persistent Opioid Use in Cataract Surgery Pain.16Documento11 paginePersistent Opioid Use in Cataract Surgery Pain.16Danty IndriastutyNessuna valutazione finora
- Anaesthesia For Adenotonsillectomy An UpdateDocumento7 pagineAnaesthesia For Adenotonsillectomy An UpdateSrihari JanakiNessuna valutazione finora
- Brain-Sparing Radiotherapy For Neuroblastoma Skull MetastasesDocumento6 pagineBrain-Sparing Radiotherapy For Neuroblastoma Skull Metastasesasialoren74Nessuna valutazione finora
- Xia 2014Documento5 pagineXia 2014Akmal Niam FirdausiNessuna valutazione finora
- Peripheral Nerve Stimulation For Painful Mononeuropathy Secondary To Leprosy: A 12-Month Follow-Up StudyDocumento6 paginePeripheral Nerve Stimulation For Painful Mononeuropathy Secondary To Leprosy: A 12-Month Follow-Up StudySartika Ayu NingsihNessuna valutazione finora
- Ledderose2021 Article EndoscopicEndonasalRepairOfComDocumento7 pagineLedderose2021 Article EndoscopicEndonasalRepairOfComAlejandra Oliveros VargasNessuna valutazione finora
- Danger Points, Complications and Medico-Legal Aspects in Endoscopic Sinus SurgeryDocumento61 pagineDanger Points, Complications and Medico-Legal Aspects in Endoscopic Sinus SurgeryMyrellaAlexandraNessuna valutazione finora
- 102 FullDocumento5 pagine102 FullMohebNessuna valutazione finora
- Kokki2011 PDFDocumento9 pagineKokki2011 PDFnurfitriaNessuna valutazione finora
- SOS RegionalDocumento7 pagineSOS RegionalibunqumairaNessuna valutazione finora
- Journal of Clinical AnesthesiaDocumento7 pagineJournal of Clinical AnesthesiaNongnapat KettungmunNessuna valutazione finora
- Stolovitzky Et Al 2021 Effect of Radiofrequency Neurolysis On The Symptoms of Chronic Rhinitis A Randomized ControlledDocumento7 pagineStolovitzky Et Al 2021 Effect of Radiofrequency Neurolysis On The Symptoms of Chronic Rhinitis A Randomized ControlledfrischaNessuna valutazione finora
- General Principles of Regional Anaesthesia in ChildrenDocumento7 pagineGeneral Principles of Regional Anaesthesia in ChildrenAlfredo HuamaniNessuna valutazione finora
- Lauder 2019Documento12 pagineLauder 2019Julio AltamiranoNessuna valutazione finora
- Hadi2015 KetodexDocumento6 pagineHadi2015 KetodexRodrigodeAndradeNessuna valutazione finora
- ps03bp 2013 Guidelines For The Management of Major Regional Analgesia Background PaperDocumento5 pagineps03bp 2013 Guidelines For The Management of Major Regional Analgesia Background PaperJane KoNessuna valutazione finora
- 7 FullDocumento3 pagine7 FullcignalNessuna valutazione finora
- [19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedDocumento7 pagine[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedBruno MañonNessuna valutazione finora
- Complications of Local Anaesthesia. An Observational Study: International Journal of Dental Hygiene November 2009Documento4 pagineComplications of Local Anaesthesia. An Observational Study: International Journal of Dental Hygiene November 2009vbhdhuNessuna valutazione finora
- Cerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDocumento11 pagineCerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDaniel EllerNessuna valutazione finora
- Iranjradiol 14 03 21742Documento5 pagineIranjradiol 14 03 21742AisahNessuna valutazione finora
- Postoperative Care in Functional Endoscopic: Sinus Surgery?Documento4 paginePostoperative Care in Functional Endoscopic: Sinus Surgery?Ida KatarinaNessuna valutazione finora
- Extubation Readiness in Critically Ill Stroke PatientsDocumento8 pagineExtubation Readiness in Critically Ill Stroke PatientsMedicina InternaNessuna valutazione finora
- Multiples Resecciones EpilepsiaDocumento17 pagineMultiples Resecciones EpilepsiaAlejandra SaenzNessuna valutazione finora
- European Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1Documento11 pagineEuropean Multicenter Trial of The Prevention of Cystoid Macular Edema After Cataract Surgery in Nondiabetics: ESCRS PREMED Study Report 1salvadorNessuna valutazione finora
- Juvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyDocumento3 pagineJuvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyGiiszs AlvarezNessuna valutazione finora
- Advances in Regional Anaesthesia and Acute Pain Management: A Narrative ReviewDocumento10 pagineAdvances in Regional Anaesthesia and Acute Pain Management: A Narrative ReviewburhanNessuna valutazione finora
- Endarterectomia 2Documento12 pagineEndarterectomia 2Andrea RangelNessuna valutazione finora
- Failed Spinal AnaesthesiaDocumento10 pagineFailed Spinal AnaesthesiaYosua SiwabessyNessuna valutazione finora
- Bmjopen 2017 018148 PDFDocumento7 pagineBmjopen 2017 018148 PDFEva AstriaNessuna valutazione finora
- Garin 2015Documento9 pagineGarin 2015Thya84Nessuna valutazione finora
- Epi 412078Documento15 pagineEpi 412078Jucsy JuxyNessuna valutazione finora
- Acute Trauma PatientsDocumento24 pagineAcute Trauma PatientsCinthia Lee castroNessuna valutazione finora
- Advantage and Limitation of Endoscopic SeptoplastyDocumento10 pagineAdvantage and Limitation of Endoscopic SeptoplastyProf. Ashraful IslamNessuna valutazione finora
- 381 FullDocumento8 pagine381 Fullwaciy70505Nessuna valutazione finora
- An Overview of Emergency Ultrasound in The United StatesDocumento6 pagineAn Overview of Emergency Ultrasound in The United StatesNuriakhildaNessuna valutazione finora
- Ultrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentDocumento5 pagineUltrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentZarella Ramírez BorreroNessuna valutazione finora
- Rare and Fatal Complications of Tonsillectomy Sudden Pneumothorax and Extensive Subcutaneous EmphysemaDocumento8 pagineRare and Fatal Complications of Tonsillectomy Sudden Pneumothorax and Extensive Subcutaneous EmphysemaJoko NugrohoNessuna valutazione finora
- Development of A Modified Swallowing Screening TooDocumento7 pagineDevelopment of A Modified Swallowing Screening TooNADISH MANZOORNessuna valutazione finora
- 1gorgan BrainAbcessesDocumento8 pagine1gorgan BrainAbcessesHaryono HaryNessuna valutazione finora
- Adenoidectomy Anatomical Variables As Predic - 2021 - International Journal ofDocumento5 pagineAdenoidectomy Anatomical Variables As Predic - 2021 - International Journal ofHung Son TaNessuna valutazione finora
- Comparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourDocumento9 pagineComparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourtasyadelizaNessuna valutazione finora
- Echography and Doppler of the BrainDa EverandEchography and Doppler of the BrainChiara RobbaNessuna valutazione finora
- KADDocumento30 pagineKADDellNessuna valutazione finora
- B135 Work and EpilepsyDocumento33 pagineB135 Work and EpilepsyDrSajid BuzdarNessuna valutazione finora
- Disertasi Dr. TerawanDocumento8 pagineDisertasi Dr. TerawanNurhaidah AchmadNessuna valutazione finora
- Labour and Delivery Care Module - 4 Using The Partograph - View As Single PageDocumento21 pagineLabour and Delivery Care Module - 4 Using The Partograph - View As Single PageDellNessuna valutazione finora
- KADDocumento30 pagineKADDellNessuna valutazione finora
- Nature CardiologyDocumento7 pagineNature CardiologyDellNessuna valutazione finora
- Module 14 Pediatric TB ENGLISHDocumento85 pagineModule 14 Pediatric TB ENGLISHDellNessuna valutazione finora
- Clinical Diagnosis and Complications of Paratubal Cysts: Review of The Literature and Report of Uncommon PresentationsDocumento10 pagineClinical Diagnosis and Complications of Paratubal Cysts: Review of The Literature and Report of Uncommon PresentationsDellNessuna valutazione finora
- 5 Morisky Medication Adherence-Scale PDFDocumento1 pagina5 Morisky Medication Adherence-Scale PDFDellNessuna valutazione finora
- Sliwa Et Al-2017-European Journal of Heart FailureDocumento11 pagineSliwa Et Al-2017-European Journal of Heart FailureDellNessuna valutazione finora
- GLM0021 Postpartum HaemorrhageDocumento13 pagineGLM0021 Postpartum HaemorrhageDellNessuna valutazione finora
- SalerioDocumento28 pagineSalerioRizqaFebrilianyNessuna valutazione finora
- HTN Late PregnancyDocumento2 pagineHTN Late PregnancyDellNessuna valutazione finora
- Sliwa Et Al-2017-European Journal of Heart FailureDocumento11 pagineSliwa Et Al-2017-European Journal of Heart FailureDellNessuna valutazione finora
- Clinical Yeoh PDFDocumento5 pagineClinical Yeoh PDFAzizan HannyNessuna valutazione finora
- SPSS Crosstab PDFDocumento3 pagineSPSS Crosstab PDFDellNessuna valutazione finora
- CTG Classification PDFDocumento1 paginaCTG Classification PDFDellNessuna valutazione finora
- NICEguidelineonAEDsAugust2014 0Documento3 pagineNICEguidelineonAEDsAugust2014 0DellNessuna valutazione finora
- Jurnal Farmakologi Anti Konvulsi PDFDocumento13 pagineJurnal Farmakologi Anti Konvulsi PDFtherempongss100% (1)
- CE-Hypertension The Silent KillerDocumento8 pagineCE-Hypertension The Silent KillerD.E.P.HNessuna valutazione finora
- A Practical Classification of Septonasal Deviation.42Documento3 pagineA Practical Classification of Septonasal Deviation.42DellNessuna valutazione finora
- 144TD (C) 25 (E3) - Issue No 3 - Ear, Nose and Throat (ENT) Infections Antibiotic Guidelines PDFDocumento9 pagine144TD (C) 25 (E3) - Issue No 3 - Ear, Nose and Throat (ENT) Infections Antibiotic Guidelines PDFDellNessuna valutazione finora
- TB CutisDocumento16 pagineTB CutisDellNessuna valutazione finora
- Journal Pone 0158499Documento11 pagineJournal Pone 0158499DellNessuna valutazione finora
- Fitzpatrick's Dermatology in General Medicine, Eighth Edition, 2 Volume SetDocumento30 pagineFitzpatrick's Dermatology in General Medicine, Eighth Edition, 2 Volume SetDellNessuna valutazione finora
- Jnma00266 0071Documento4 pagineJnma00266 0071DellNessuna valutazione finora
- Functional Endoscopic Sinus Surgery - American Family PhysicianDocumento8 pagineFunctional Endoscopic Sinus Surgery - American Family PhysicianDellNessuna valutazione finora
- 3rd Care of The Critically Ill Surgical Patient PDFDocumento273 pagine3rd Care of The Critically Ill Surgical Patient PDFPavitra RamasamyNessuna valutazione finora
- Chap.30 Complications From Heart Disease WordDocumento6 pagineChap.30 Complications From Heart Disease WordcaisakiNessuna valutazione finora
- Hemo PathDocumento2 pagineHemo PathanadiguptaNessuna valutazione finora
- Owning Up The Mistakes: Narratives of An Ayurvedic PhysicianDocumento3 pagineOwning Up The Mistakes: Narratives of An Ayurvedic PhysicianVakamalla SubbareddyNessuna valutazione finora
- Trauma CounsellingDocumento2 pagineTrauma CounsellingSindujaa SelliahNessuna valutazione finora
- Dhulikhel Water Supply ProjectDocumento4 pagineDhulikhel Water Supply ProjectSujan Singh50% (2)
- Inborn Errors or MetabolismDocumento25 pagineInborn Errors or MetabolismSamdiSutantoNessuna valutazione finora
- Appendicitis and Peritonitis 1Documento21 pagineAppendicitis and Peritonitis 1chrisyenNessuna valutazione finora
- Advisor Vol 14Documento8 pagineAdvisor Vol 14ninh2dNessuna valutazione finora
- Document Dynasand Phosphorus Removal Case Study 1788Documento1 paginaDocument Dynasand Phosphorus Removal Case Study 1788taenker123Nessuna valutazione finora
- Case Study - La Roche-Posay Media Gathering 2006Documento3 pagineCase Study - La Roche-Posay Media Gathering 2006Lhcmkt LhcNessuna valutazione finora
- CKD CHCRTDocumento28 pagineCKD CHCRTNurhidayati KeriyunNessuna valutazione finora
- Case 29.07.09Documento51 pagineCase 29.07.09kanavgNessuna valutazione finora
- Part A. Reading Comprehension: Attitude Therapy Misleading Recognize Refuse EstablishmentDocumento2 paginePart A. Reading Comprehension: Attitude Therapy Misleading Recognize Refuse EstablishmentCarol80% (5)
- Patient and Family Guide To The CANMAT and ISBD Guidelines On The Management of Bipolar DisorderDocumento34 paginePatient and Family Guide To The CANMAT and ISBD Guidelines On The Management of Bipolar DisorderLucila VialeNessuna valutazione finora
- Diss 1 3 7 OCR Rev PDFDocumento5 pagineDiss 1 3 7 OCR Rev PDFKunotamashi KanakacheroNessuna valutazione finora
- Fasting Ramadan During PregnancyDocumento17 pagineFasting Ramadan During PregnancyHasiah Karim100% (1)
- Entrelazamiento (Amir Aczel)Documento8 pagineEntrelazamiento (Amir Aczel)Memento MoriNessuna valutazione finora
- Pyogenic MeningitisDocumento20 paginePyogenic MeningitisClever BarbieNessuna valutazione finora
- CPAP SlidesDocumento52 pagineCPAP SlidesAnusha Verghese100% (1)
- Biography of Dorothea OremDocumento6 pagineBiography of Dorothea OremGeorgeEchevarriaNessuna valutazione finora
- Catalogue v09Documento4 pagineCatalogue v09KRISHNA L BAISETTINessuna valutazione finora
- A Long-Term Study of 370 Autotransplanted Premolars. Part II. Tooth Survival and Pulp Healing Subsequent To TransplantationDocumento11 pagineA Long-Term Study of 370 Autotransplanted Premolars. Part II. Tooth Survival and Pulp Healing Subsequent To TransplantationRudnapon AmornlaksananonNessuna valutazione finora
- 2ton Steel 56.8gDocumento4 pagine2ton Steel 56.8gYasir AzmatNessuna valutazione finora










































![[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matched](https://imgv2-2-f.scribdassets.com/img/document/722525723/149x198/0c84be9862/1712965550?v=1)