Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Beta-Lactam Compound Mechanism of Action Effects Clinical Applications Pharmacokinetics Toxicities and Interaction Penicillin
Caricato da
Wynlor AbarcaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Beta-Lactam Compound Mechanism of Action Effects Clinical Applications Pharmacokinetics Toxicities and Interaction Penicillin
Caricato da
Wynlor AbarcaCopyright:
Formati disponibili
Beta-Lactam Mechanism of Effects Clinical Pharmacokinetics Toxicities and Interaction
Compound Action Applications
1. Penicillin Prevents bacterial Rapid Streptococcal IV administration | rapid renal Degraded by Beta-lactamases.
cell wall synthesis bactericidal infections, clearance with half-life of 30 Toxicities include immediate
(which occurs via activity against meningococcal minutes, 90% of which is via hypersensitivity, rash, seizures
transpeptidation susceptible infections, tubular secretion while the
rxn) by covalently bacteria. neurosyphilis remaining is through glomerular
binding to and filtration | Excreted into the
inhibiting cell wall sputum and breast milk to levels
transpeptidases 3-15% of those in serum | Poorly
penetrates eye, prostate, and CNS
2. Cephalospor Prevents bacterial Rapid Skin and soft IV administration | renal clearance Rash, drug fever
in cell wall synthesis bactericidal tissue | poorly penetrates CNS except
by covalently activity against infections, Ceftriaxone
binding to and susceptible urinary tract
inhibiting cell wall bacteria. infections,
transpeptidases surgical
prophylaxis
3. Carbapenem Prevents bacterial Rapid Serious IV administration | renal clearance Cilastatin added to prevent
cell wall synthesis bactericidal infections such hydrolysis by renal
by covalently activity against as pneumonia dehydropeptidase. Toxicities
binding to and susceptible and sepsis include seizures especially in
inhibiting cell wall bacteria. renal failure or with high doses
transpeptidases (>2 g/d)
4. Monobacta Prevents bacterial Rapid Infections IV administration | renal clearance No cross allergenicity with
m cell wall synthesis bactericidal caused by penicillin
by covalently activity against aerobic, gram-
binding to and susceptible negative
inhibiting cell wall bacteria. bacteria in
transpeptidases patients with
immediate
hypersensitivity
to penicillin
5. Glycopeptid Inhibits cell wall Bactericidal Infections Oral, IV administration | renal Red man syndrome,
e synthesis by activity against caused by gram- clearance nephrotoxicity
binding to the D- susceptible positive bacteria
ala D-Ala bacteria, including sepsis,
terminus of slower kill than endocarditis,
nascent beta-lactam and meningitis
peptidoglycan antibiotics
6. Lipopeptide Binds to cell Bactericidal Infections IV administration | renal clearance Inactivated by pulmonary
membrane, activity against caused by gram- surfactant so it cannot be used to
causing susceptible positive bacteria treat pneumonia. Toxicities
depolarization bacteria; more including sepsis include Myopathy whereas
and rapid cell rapidly and endocarditis monitoring of weekly creatinine
death bactericidal phosphokinase levels is
than recommended.
vancomycin
The Penicillin
Derivatives of 6-aminopenicillanic acid
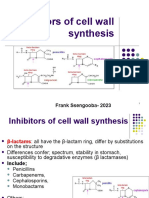
Contains beta-lactam ring, a four-membered cyclic amide which is the core component of several antibiotics,
and thiazolidine ring.
Blood levels of all penicillin can be raised by simultaneous administration of Probenecid, 0.5 g every 6 hours
orally, which impairs renal tubular secretion of weak acids such as -lactam compounds.
Penicillin inhibits bacterial growth by interfering transpeptidation reaction of bacterial cell wall synthesis
thereby halting peptidoglycan synthesis which is one of the components of the cell wall.
Transpeptidation cross links two polymer chains of peptidoglycans containing amino hexoses N-
acetylglucosamine and N-acetylmuramic acid whose peptide chain terminates in D-alanyl-D-alanine. When
cross-linking occurs the terminal alanine is removed by penicillin-binding protein and the exposed alanyl
links with a pentapeptide side chain of another N-acetylmuramic acid of the other polymer thereby giving
rigidity to the cell wall.
Generally, like any other -lactam antibiotics, they are hydrolyzed by -lactamases which are produced by
bacteria.
Mechanisms of Resistance:
i. Inactivation of antibiotic by -lactamase
ii. Modification of target PBPs
iii. Impaired penetration of drug to target PBPs
iv. Antibiotic efflux
Mechanism I is the most common mechanism of resistance.
Mechanism II is the basis of methicillin resistance in staphylococci and of penicillin resistance in
pneumococci and enterococci. These resistant organisms produce PBPs that have low affinity for binding
lactam antibiotics, and consequently they are not inhibited except at relatively high drug concentrations
which is often clinically unachievable.
Mechanism III occurs only in gram-negative species because of the impermeable outer membrane of the cell
wall which is absent in gram-positive bacteria. -lactam antibiotics cross the membrane via outer-membrane
protein channels called as porins. The absence of such channel or down-regulation of production greatly
impairs drug entry to the cell.
Mechanism IV occurs when gram-negative species produce efflux pump, which consists of cytoplasmic and
periplasmic protein components that efficiently transport some -lactam antibiotics from the periplasm back
across the cell wall outer membrane.
A. Normal Penicillin
1. Penicillin G
Less protein-bound penicillin
Intravenous route of administration
Used against streptococci, meningococci, susceptible pneumococci, non--lactamase producing
staphylococci bacteria
Used in Treponema pallidum and other spirochetes, Actinomyces and certain gram-positive rods, and in
some Clostridium species.
Also used in non--lactamase producing gram-negative anaerobic bacteria
2. Penicillin V
Oral form of penicillin
Poor bioavailability
Narrow antibacterial spectrum
Given 1-2 hours before or after meals
B. Long-Acting Penicillin formulated to delay absorption to prolong blood and tissue drug concentrations
however, yields lower drug levels compared to the normal penicillin drugs.
1. Benzathine Penicillin
2.4 million units of Benzathine Penicillin G administered Intramuscularly once a week for 1-3 weeks is
effective against syphilis
Intramuscular injection of 1.2 million units is effective against -hemolytic streptococcal pharyngitis
2. Procaine Penicillin G
was used for pneumococcal pneumonia and gonorrhea treatment
rarely used now against gonorrhea because many of gonococcal strains are penicillin-resistant
Rarely used now against pneumococcal pneumonia because many pneumococci require higher doses of
Penicillin G or more potent -lactams
C. Anti-staphylococcal Penicillin semisynthetic penicillin which are resistant to staphylococcal -lactamase
- Listeria monocytogenes, enterococci, and methicillin-resistant strains of staphylococci are resistant
1. Nafcillin
Intravenously administered
Highly protein-bound penicillin
Achieve lower free-drug concentration in serum
2. Methicillin
3. Oxacillin
4. Isoxazoyl Penicillin
a. Cloxacillin
b. Dicloxacillin
D. Extended-Spectrum Penicillin
1. Amoxicillin
2. Ampicillin
3. Carboxypenicillin
a. Carbenicillin
b. Ticarcillin
c. Ureidopenicillin
d. Pherpacillin
e. Mezlocillin
f. Azlocillin
The Cephalosporin
7-aminocephalosphoric acid as the nucleus wherein various R groups may attach
More stable against B-Lactamase compared to Penicillin
Can be hydrolyzed by extended-spectrum -lactamases expressed by strains of E. coli and Klebsiella sp
Inactive against L monocytogenes
Only Ceftaroline has some activity against enterococci
Lower toxicity
A. First Generation Cephalosporin
1. Orally Administered
a. Cephalexin
b. Cephradine
c. Cefadroxil
2. Parenteral Administration
a. Cefazolin (IV) only first-gen parenteral cephalosporin still in general use
b. Cephalothin (IV)
c. Cephapirin / Cefapirin (IV)
B. Second Generation Cephalosporin
1. Orally Administered
a. Cefaclor
b. Cefuroxime acetyl
c. Cefprozil
d. Loracarbef
2. Parental Administration
a. Cefoxitin (Cephamycin)
b. Cefmetazole (Cephamycin)
c. Cefotetan (Cephamycin)
d. Cefmandole
e. Cefonicid
f. Ceforanide
g. Cefuroxime
C. Third Generation Cephalosporin
1. Orally Administered
a.
2. Parenteral Administration
D. Fourth Generation Cephalosporin
Potrebbero piacerti anche
- CS1 AntibioticsDocumento4 pagineCS1 AntibioticsTaraKyleUyNessuna valutazione finora
- ANTIBIOTICSDocumento7 pagineANTIBIOTICSLutfi HakimNessuna valutazione finora
- PharmacologyDocumento8 paginePharmacologyfileacademicsNessuna valutazione finora
- NICU Drug StudyDocumento2 pagineNICU Drug StudyMay Chelle ErazoNessuna valutazione finora
- CeftriaxoneDocumento1 paginaCeftriaxonecen janber cabrillosNessuna valutazione finora
- CefuroximeDocumento1 paginaCefuroximePriscilla ChantalNessuna valutazione finora
- Drug Study of OxytocinDocumento4 pagineDrug Study of OxytocinNichole DancelNessuna valutazione finora
- Chapter 43 - Beta-Lactam Antibiotics & Amp Other Cell Wall - & Amp Membrane-Active AntibioticsDocumento9 pagineChapter 43 - Beta-Lactam Antibiotics & Amp Other Cell Wall - & Amp Membrane-Active AntibioticsSara OchoaNessuna valutazione finora
- Beta Lactams - PenicillinsDocumento74 pagineBeta Lactams - PenicillinsSunanda mohanNessuna valutazione finora
- Applied Pharmacotherapy: By: First GroupDocumento13 pagineApplied Pharmacotherapy: By: First GroupMUHAMMAD ISLAMINessuna valutazione finora
- CefuroximeDocumento1 paginaCefuroximekrz05Nessuna valutazione finora
- Cell Wall Synthesis Inhibitors: Jagir R. Patel Asst Prof. Anand Pharmacy CollegeDocumento30 pagineCell Wall Synthesis Inhibitors: Jagir R. Patel Asst Prof. Anand Pharmacy CollegeJagirNessuna valutazione finora
- Katzung Pharmacology Semester 5 TablesDocumento29 pagineKatzung Pharmacology Semester 5 TablesfatimaNessuna valutazione finora
- Drug Study in GentamicinDocumento2 pagineDrug Study in Gentamicinanthony_alviar100% (1)
- Pharmacology MidtermDocumento37 paginePharmacology Midtermnaomie manaliliNessuna valutazione finora
- Pharmacology MidtermDocumento27 paginePharmacology Midtermnaomie manaliliNessuna valutazione finora
- Cell Wall Inhibitors - Pharmacology 3 - Frank SsengoobaDocumento16 pagineCell Wall Inhibitors - Pharmacology 3 - Frank SsengoobaVhugala AudreyNessuna valutazione finora
- Cơ Chế Kháng Thuốc Gram (+) 2Documento9 pagineCơ Chế Kháng Thuốc Gram (+) 2Quỳnh Nguyễn Thị NhưNessuna valutazione finora
- Drug Study - CefoxitinDocumento5 pagineDrug Study - CefoxitinShaniah DawaNessuna valutazione finora
- Anti-Inffective AgentsDocumento2 pagineAnti-Inffective AgentsJamilah BanglanNessuna valutazione finora
- Antibiotics SummaryDocumento3 pagineAntibiotics SummaryMai GaberNessuna valutazione finora
- Phar - Cell Wall Inhibitor - Lec 7 - TheoDocumento20 paginePhar - Cell Wall Inhibitor - Lec 7 - Theoسلام شاكر حميد جميل 6506Nessuna valutazione finora
- Pharma-URO-CYCLIC LIPOEPETIDES (Vancomycin)Documento6 paginePharma-URO-CYCLIC LIPOEPETIDES (Vancomycin)Hussein AlhaddadNessuna valutazione finora
- Antimicrobial Agents: Beta - Lactam CompoundsDocumento6 pagineAntimicrobial Agents: Beta - Lactam CompoundsalejandraNessuna valutazione finora
- Antibacterial AgentsDocumento44 pagineAntibacterial Agentsbelindasithole965Nessuna valutazione finora
- Drug Index Generic Name MOA Clinical Uses Side Effects/ Contraindications DosageDocumento3 pagineDrug Index Generic Name MOA Clinical Uses Side Effects/ Contraindications Dosageyoke limuriaNessuna valutazione finora
- Group 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. JumuadDocumento25 pagineGroup 5 Subgroup 1: Jomarie Eve D. Enriquez Kurt Russel A. Jumuadrakish16Nessuna valutazione finora
- Penicillin's: Jagir R. Patel Asst Professor Dept. PharmacologyDocumento29 paginePenicillin's: Jagir R. Patel Asst Professor Dept. PharmacologyJagirNessuna valutazione finora
- Antmicrobial AgentDocumento93 pagineAntmicrobial Agentdrnuaman5Nessuna valutazione finora
- Drug Action Indications and Contraindications Nursing ResponsibilitesDocumento3 pagineDrug Action Indications and Contraindications Nursing ResponsibilitesGino B. BulanaNessuna valutazione finora
- DRUG TABULATION EditedDocumento7 pagineDRUG TABULATION EditedAlexa Nicole GayosoNessuna valutazione finora
- Drug Study MugnaDocumento7 pagineDrug Study Mugnakint manlangitNessuna valutazione finora
- Cell Wall Inhibitors: Zarqa University Pharmacy School Clinical Pharmacy and Therapeutics Department Pharmacology IIIDocumento45 pagineCell Wall Inhibitors: Zarqa University Pharmacy School Clinical Pharmacy and Therapeutics Department Pharmacology IIIAla'a AL AqrabawyNessuna valutazione finora
- Pedia Drug Study 5Documento2 paginePedia Drug Study 5Geddy SarigumbaNessuna valutazione finora
- Cell Wall Inhibitors: Beta-Lactams: PenicillinsDocumento12 pagineCell Wall Inhibitors: Beta-Lactams: Penicillinsمحمد بن صالحNessuna valutazione finora
- BCG Vaccine Drug StudyDocumento2 pagineBCG Vaccine Drug StudyLegendX83% (6)
- Beta-Lactam Antibiotics & Other Cell Wall Synthesis InhibitorsDocumento29 pagineBeta-Lactam Antibiotics & Other Cell Wall Synthesis InhibitorsRen PastelNessuna valutazione finora
- Pediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic DiscussionDocumento5 paginePediatric Hospital-Acquired and Ventilator-Associated Pneumonia Topic Discussionapi-602288180Nessuna valutazione finora
- Beta Lactam AntibioticsDocumento52 pagineBeta Lactam AntibioticsKaymie ReenNessuna valutazione finora
- Supervised By: Dr. Reem: Resistance of Penicillin and Its Allergy Resulted in HumanDocumento4 pagineSupervised By: Dr. Reem: Resistance of Penicillin and Its Allergy Resulted in HumanshahadNessuna valutazione finora
- PharmacyDocumento16 paginePharmacyJow RamosNessuna valutazione finora
- MeropenemDocumento1 paginaMeropenemMuhammad ArsalanNessuna valutazione finora
- Antimicrobials RevisionDocumento5 pagineAntimicrobials RevisionDanny LeeNessuna valutazione finora
- PenicillinDocumento21 paginePenicillinnadar shahNessuna valutazione finora
- ChemotherapyDocumento66 pagineChemotherapyElias HaimanotNessuna valutazione finora
- Antimicrobial DrugsDocumento89 pagineAntimicrobial DrugsShahane AlisosoNessuna valutazione finora
- RiteshDocumento4 pagineRiteshPharmacy On FingerTipsNessuna valutazione finora
- Drug StudyDocumento3 pagineDrug StudyDannielle EvangelistaNessuna valutazione finora
- Bacteria Gram:: Streptococcus PneumoniaeDocumento3 pagineBacteria Gram:: Streptococcus PneumoniaetrrrinsNessuna valutazione finora
- S1473309905700517 - 1 s2.0 S1473309905700517 MainDocumento10 pagineS1473309905700517 - 1 s2.0 S1473309905700517 MainwardaninurindahNessuna valutazione finora
- QUIMSON, JADEN Drug StudyDocumento3 pagineQUIMSON, JADEN Drug StudyJaden QuimsonNessuna valutazione finora
- BetaLactamAntibiotics StatPearls NCBIBookshelfDocumento8 pagineBetaLactamAntibiotics StatPearls NCBIBookshelfinkarkanat02Nessuna valutazione finora
- Antibacterial Drugs Cellwall and Protein Synthesis InhihibitorsDocumento41 pagineAntibacterial Drugs Cellwall and Protein Synthesis InhihibitorsWezzyNessuna valutazione finora
- Lecture 15 Presentation ENGDocumento37 pagineLecture 15 Presentation ENGjqpwzcg8xrNessuna valutazione finora
- Drug Classificati ON Indication Contraindica Tion Side Effects Nursing Responsibili TiesDocumento2 pagineDrug Classificati ON Indication Contraindica Tion Side Effects Nursing Responsibili TiesMelduard Godwin R. PulidoNessuna valutazione finora
- Antibiotic Classification and MechanismsDocumento43 pagineAntibiotic Classification and Mechanismsyoza_kidNessuna valutazione finora
- AntibioticDocumento84 pagineAntibioticDr. Kalavati PrajapatiNessuna valutazione finora
- Fluoroquinolones: QuinolonesDocumento7 pagineFluoroquinolones: QuinolonesGhubaya CopNessuna valutazione finora
- Ceftr Iaxon eDocumento1 paginaCeftr Iaxon eblazelex17Nessuna valutazione finora
- Adult Infectious Disease Bulletpoints HandbookDa EverandAdult Infectious Disease Bulletpoints HandbookValutazione: 4.5 su 5 stelle4.5/5 (9)
- A Review On Evaluation of TabletsDocumento5 pagineA Review On Evaluation of TabletsMukesh Tiwari50% (2)
- UroflowDocumento41 pagineUroflowSri HariNessuna valutazione finora
- The Sober Truth: Debunking The Bad Science Behind 12-Step Programs and The Rehab IndustryDocumento3 pagineThe Sober Truth: Debunking The Bad Science Behind 12-Step Programs and The Rehab IndustryEmma-Jean Weinstein100% (3)
- Family Genogram ArticleDocumento26 pagineFamily Genogram Articleaawulff100% (3)
- Daivonex Cream PI - LPS-11-045Documento5 pagineDaivonex Cream PI - LPS-11-045Hesam AhmadianNessuna valutazione finora
- Alzheimer's Disease Fact SheetDocumento6 pagineAlzheimer's Disease Fact SheetInternational Business Times100% (2)
- Ice TherapyDocumento5 pagineIce TherapyDiane CastillonNessuna valutazione finora
- Informative Speech OutlineDocumento3 pagineInformative Speech Outlineapi-27792479886% (14)
- Freedman Goldberg Reichmann The Radical Act of Inward LookingDocumento35 pagineFreedman Goldberg Reichmann The Radical Act of Inward LookingSantharaj KuppuswamyNessuna valutazione finora
- Motor Control TheoriesDocumento19 pagineMotor Control Theoriessridhar_physio50% (2)
- Discharge Plan 2.doc Imba - Doc123Documento4 pagineDischarge Plan 2.doc Imba - Doc123Hezron Ga33% (3)
- Herbal GuideDocumento42 pagineHerbal GuideladygreenNessuna valutazione finora
- Respiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoDocumento8 pagineRespiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoDopamina PsicoactivaNessuna valutazione finora
- What Is Medical DeontologyDocumento11 pagineWhat Is Medical DeontologyExorticNessuna valutazione finora
- Drugs That Affect The Digestive SystemDocumento17 pagineDrugs That Affect The Digestive SystemMusa MuhamadNessuna valutazione finora
- Hospital PlanningDocumento8 pagineHospital PlanningadithiNessuna valutazione finora
- The Case of Dora and Her DreamsDocumento5 pagineThe Case of Dora and Her DreamsHardik Motsara100% (1)
- Acute Calculous Cholecystitis Strasberg 2008 NEJMDocumento8 pagineAcute Calculous Cholecystitis Strasberg 2008 NEJMFrancisco Castro100% (1)
- Therapy ManualDocumento52 pagineTherapy ManualcrisNessuna valutazione finora
- Class XII Food, Nutrition & Dietrics Code - 834Documento120 pagineClass XII Food, Nutrition & Dietrics Code - 834Abhay GuptaNessuna valutazione finora
- Pelvic Inflammatory DiseaseDocumento34 paginePelvic Inflammatory DiseaseOhunakin AfolabiNessuna valutazione finora
- Therapeutic Effects of Phytochemicals and MedicinaDocumento11 pagineTherapeutic Effects of Phytochemicals and MedicinaMd. JubairNessuna valutazione finora
- Essentials of Orthognathic Surgery, 3eDocumento14 pagineEssentials of Orthognathic Surgery, 3epaolacsuarezaNessuna valutazione finora
- Management of Asthma in Adults (Second Edition) : November 2017 Moh/P/Pak/Xxx (Gu)Documento64 pagineManagement of Asthma in Adults (Second Edition) : November 2017 Moh/P/Pak/Xxx (Gu)Shamsyul IqramNessuna valutazione finora
- Equipos Monitoreo de CondicionesDocumento11 pagineEquipos Monitoreo de CondicionesJonathan Vasquez LlagunoNessuna valutazione finora
- List of Surgeries: AbdomenDocumento35 pagineList of Surgeries: AbdomenSaurav SaikiaNessuna valutazione finora
- Murtagh's Practice Tips, 6th EditionDocumento281 pagineMurtagh's Practice Tips, 6th EditionAishath MohamedNessuna valutazione finora
- RRL Anne)Documento27 pagineRRL Anne)api-3728522Nessuna valutazione finora
- AHA ACLS Megacode ScenariosDocumento6 pagineAHA ACLS Megacode ScenariosVitor Hugo G Correia86% (7)
- The Effectiveness of Treatment For Adult Sexual OffendersDocumento6 pagineThe Effectiveness of Treatment For Adult Sexual OffendersStephen LoiaconiNessuna valutazione finora