Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Journal Pone 0086797
Caricato da
Meirinda HidayantiTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Journal Pone 0086797
Caricato da
Meirinda HidayantiCopyright:
Formati disponibili
Prediction of Severe Neonatal Hyperbilirubinemia Using
Cord Blood Hydrogen Peroxide: A Prospective Study
Hung-Chieh Chou1,2, Chiang-Ting Chien3, Po-Nien Tsao2, Wu-Shiun Hsieh2, Chien-Yi Chen1,2, Mei-
Hwei Chang2*
1 National Taiwan University College of Medicine Graduate Institute of Clinical Medicine, Taipei, Taiwan, 2 Department of Pediatrics, National Taiwan University Hospital,
National Taiwan University, Medical College, Taipei, Taiwan, 3 Department of Life Science, National Taiwan Normal University, Taipei, Taiwan
Abstract
Background: We hypothesized that cord blood hydrogen peroxide (H2O2) could be utilized to predict the severity of
neonatal hyperbilirubinemia.
Methods: We prospectively enrolled term or near-term healthy neonates. Cord blood and capillary blood at three days of
age were measured for hydrogen peroxide and bilirubin concentrations. For newborns with hyperbilirubinemia, further
blood samples were obtained at five and seven days of age. Newborns were divided into severe or less severe
hyperbilirubinemic groups (peak bilirubin $17 mg/dL or not). The sensitivity, specificity, and negative predictive values
were determined.
Results: There were 158 neonates enrolled. The incidence of neonatal hyperbilirubinemia was 30.5% for a concentration
$15 mg/dl. The rising patterns were similar among bilirubin concentrations and hydrogen peroxide levels during the first
few days of life. There was a strong positive correlation between bilirubin concentrations and hydrogen peroxide levels after
correlation analysis. The rate of severe hyperbilirubinemia was 13.3%. It revealed that a cord blood hydrogen peroxide
signal level of 2500 counts/10 seconds was an appropriate cut-off for predicting severe hyperbilirubinemia. Sensitivity and
the negative predictive value were 76.2% and 93.3%, respectively.
Conclusions: Our findings confirm that hydrogen peroxide levels and bilirubin concentrations in cord and neonatal blood
are closely related. A cord blood hydrogen peroxide level above 2500 counts/10 seconds associated with a high predictive
value for severe hyperbilirubinemia. This method provides information about which neonate should be closely followed
after discharge from the nursery.
Citation: Chou H-C, Chien C-T, Tsao P-N, Hsieh W-S, Chen C-Y, et al. (2014) Prediction of Severe Neonatal Hyperbilirubinemia Using Cord Blood Hydrogen
Peroxide: A Prospective Study. PLoS ONE 9(1): e86797. doi:10.1371/journal.pone.0086797
Editor: Giovambattista Pani, Catholic University Medical School, Italy
Received August 28, 2013; Accepted December 14, 2013; Published January 23, 2014
Copyright: 2014 Chou et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The authors have no support or funding to report.
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: changmh@ntu.edu.tw
Introduction thereby increase the incidence of kernicterus [14]. Therefore,
researchers have been enthusiastic about identifying predictors of
The incidence of neonatal jaundice is around 60,70% in neonatal hyperbilirubinemia to assist in the early detection of
Western countries [1]. and even higher among newborns of Asian neonates at high risk of severe hyperbilirubinemia. The hour-
ethnicity. Neonatal jaundice is associated with increased uncon- specific bilirubin nomogram [15] is widely accepted by most
jugated bilirubin concentrations caused by the breakdown of red clinicians, but has a low sensitivity and may vary by ethnicity.
blood cells. Bilirubin can damage neurologic tissue and lead to Given the relationship between bilirubin and hydrogen
bilirubin-induced neurologic dysfunction [24]. Bilirubin in itself is peroxide, which is one of reactive oxygen species, we hypothesized
not completely detrimental and can exert a physiological that hydrogen peroxide levels in cord blood could be used to
protective effect [5] due to its antioxidant properties [6]. A predict neonatal hyperbilirubinemia.
number of previous studies have highlighted the relationship
between bilirubin and nitric oxide, reactive oxygen/nitrogen
Methods
species [711].
The American Academy of Pediatrics published guidelines for Subjects
the management of neonatal jaundice in 1994 [12]. Since then, All term or near-term healthy neonates (gestational age $34
several cases of kernicterus have been reported [13]. Another weeks) born at National Taiwan University Hospital during May
prominent concern is that neonates may be discharged from and June of 2005 were candidates for enrollment into this
hospital too early, before the onset of neonatal jaundice. This may prospective follow-up study. InfantsNewborns with early onset
delay the diagnosis of severe neonatal hyperbilirubinemia and hyperbilirubinemia (bilirubin $10 mg/dL before 24 hours of age),
PLOS ONE | www.plosone.org 1 January 2014 | Volume 9 | Issue 1 | e86797
H2O2 Predict Severe Hyperbilirubinemia
maternal ABO incompatibility, glucose-6-phosphate-dehydroge-
nase deficiency, cephalohematoma, multiple congenital anomalies,
maternal gestational diabetes mellitus, anemia, congenital hypo-
thyroidism, sepsis, cholestasis, and urinary tract infection were
excluded. All procedures were approved and supervised by the
Ethics Committee of Clinical Trials of National Taiwan University
Hospital (9361700383). Signed informed consent forms were
collected from parents before enrollment.
Peak bilirubin concentrations were determined in all infants-
newborns during the follow-up period. All infantsnewborns with
bilirubin concentrations $15 mg/dL were admitted for photo-
therapy; bilirubin concentrations were monitored until they fell
below 13 mg/dL.
Sample Collection
A total of 10 mL of cord blood was obtained from all enrolled
infantsnewborns at birth. Capillary blood was also collected in a
microtube using the heel-stick lancet method on the third day after
birth. For infantsnewborns admitted with hyperbilirubinemia, Figure 2. A scatter plot figure with bilirubin (on the X-axis) and
the corresponding hydrogen peroxide levels with Logarithmic
capillary blood was obtained at five and seven day of age. All transformation (on the Y-axis) was presented. There is a linear
samples were processed immediately. relationship between these 2 values. The regression equation is H2O2
signal = 3.371+0.108*Bilirubin. The P value is ,0.0001.
Bilirubin Measurement doi:10.1371/journal.pone.0086797.g002
All blood samples, including cord blood, were centrifuged at
1500 rpm for 5 minutes. Plasma bilirubin concentrations were Tohoku Electronic Industrial Co., Sendai, Japan). The blood
then measured using a bilirubin meter (BR-501, APEL, Japan). If samples were immediately wrapped in aluminum foil and kept on
the bilirubin concentration was found to be .15 mg/dL, the ice until CL measurement, usually done within 2 h. Immediately
sample was reanalyzed using a biochemical method in our central before CL measurement, 0.1 ml of phosphate-buffered saline
laboratory. Severe neonatal hyperbilirubinemia was indicated by a (pH 7.4) was added to 0.1 ml of blood sample as described
bilirubin concentration $17 mg/dL. At our institution, these previously [16]. The CL was measured in a completely dark
infantsnewborns receive intensive phototherapy. chamber of the Chemiluminescence Analyzing System. After 100-
s background level determination, 1.0 ml of 0.1 mM luminol in
Measurement of Specific Blood Hydrogen Peroxide phosphate-buffered saline (pH 7.4) was injected into the sample.
Activity The CL was monitored continuously for an additional 600 s. The
Cord and capillary blood hematocrit levels were determined total amount of CL was calculated by integrating of the area under
after centrifugation at 1500 rpm for 5 minutes. Chemilumines- the curve and subtracting it from the background level. The assay
cence (CL) signal emitting H2O2 and CL-emitting substances was performed in duplicate for each sample and was expressed as
(luminol, Sigma, St. Louis, MO) from whole blood (with CL (H2O2) counts/10 s for blood CL. The mean 6 SEM of the
phosphate buffered as a background control) were measured by CL level of each sample was calculated.
use of a Chemiluminescence Analyzing System (CLD-110,
Statistical Analysis
The relationship between bilirubin and H2O2 signal from
infant (up to five days of age) cord blood samples was determined
by assessing the Pearson Correlation. Correlation analysis was
performed and tested by regression analysis in each sample. We
divided the eligible population into the groups by the bilirubin
concentration (bilirubin $17 mg/dL or not). All parametric data
were compared by independent samples t-test, whereas categorical
data were compared by chi-square test. A receiver operating
characteristic (ROC) curve was generated to determine a cut-off
value for predicting severe neonatal hyperbilirubinemia. Sensitiv-
ity, specificity, and negative predictive values were calculated. A P
value ,0.05 was considered to indicate statistical significance.
Results
During the study period, 282 healthy newborns were born at
Figure 1. Bilirubin concentrations and hydrogen peroxide our institution. Of these newborns, 158 were enrolled in our study.
levels increased similarly during the first few days. The The incidence of neonatal hyperbilirubinemia during follow-up
correlation between these two variables was 0.454, P,0.001. The left was 48.7% for peak bilirubin $13 mg/dL and 30.5% for peak
y-axis is the bilirubin concentration, whereas the right y-axis is the H2O2 bilirubin $15 mg/dL. The incidence of severe hyperbilirubinemia
(luminol) signal. The y-axis scale is logarithmic because of the high (bilirubin $17 mg/dL) was 13.3%.
luminal signal values.
doi:10.1371/journal.pone.0086797.g001
PLOS ONE | www.plosone.org 2 January 2014 | Volume 9 | Issue 1 | e86797
H2O2 Predict Severe Hyperbilirubinemia
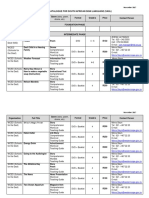
Table 1. Demographic and cord blood data for the severe and less severe hyperbilirubinemic groups.
Less Severe hyperbilirubinemic Group (n = 133)a Severe hyperbilirubinemic Group (n = 25)b P Value
GA (weeks) 38.561.6 38.861.5 0.503
BBW (g) 3106.56536.9 3246.66395.1 0.302
Apgar score (1) 9 (49) 9 (69) 0.209
Apgar score (5) 9 (89) 9 (99) 0.488
Cord blood bilirubin (mg/dL) 1.4060.67 1.5260.80 0.740
Cord hematocrit (%) 43.1065.77 44.6367.14 0.165
Abbreviations: GA, gestational age; BBW, birth body weight.
a
Newborns with peak bilirubin concentration ,17 mg/dL during the postnatal follow-up period.
b
Newborns with peak bilirubin concentration $17 mg/dL during the postnatal follow-up period.
doi:10.1371/journal.pone.0086797.t001
The Relationship between Bilirubin Concentration and less severe hyperbilirubinemic groups (Table 2). All three cut-off
H2O2 Levels values were found to be significant predictors of severe hyperbil-
Bilirubin concentrations were significantly increased in three irubinemia (P = 0.027, 0.017, and 0.030, respectively).
day-old newborns. The chemical illuminate H2O2 count was There were 75 newborns who had cord blood H2O2 signal
significantly increased in three and five day-old newborns (both levels that were below 2500 counts/10 seconds. Of these
P,0.0001). As postnatal age increased, there was a similar pattern newborns, only five newborns developed severe hyperbilirubin-
of increase in bilirubin concentrations and H2O2 (Figure 1). There emia during the follow-up period. Hence, the negative predictive
was a significant similar rising pattern (0.454, P,0.0001) between value was a maximum of 93.3%. To define if any other risk factors
bilirubin and H2O2 levels. of the 5 newborns who developed severe hyperbilirubinemia,
After the correlation analysis with scatter plot for each despite having low hydrogen peroxide levels, we compared the
individual sample, there was a strong positive correlation between demographic and clinical characteristics of these five newborns
bilirubin concentrations and hydrogen peroxide levels (Figure 2). and with those of the less severe hyperbilirubinemic group
The p value was ,0.0001. (Table 3). Three newborns (cases 1, 3, and 5) had high initial
bilirubin concentrations in cord blood. Three newborns (cases 2, 3,
The Most Suitable Cut-off Value for Predicting Severe and 4) had high initial hematocrit values. One infant (case 5)
exhibited the most pronounced loss in body weight during the first
Neonatal Hyperbilirubinemia
few days of life. All these five newborns possessed at least one
We compared demographic and clinical characteristics between
factor that was beyond the range of one standard deviation from
the severe hyperbilirubinemic group and the less severe hyperbi-
the mean value.
lirubinemic group. There were no between group differences in
gestational age, birth body weight, Apgar score (first and fifth
minutes), cord blood bilirubin concentration, or cord blood Discussion
hematocrit (Table 1). A comparison of the ROC curves for cord We have found that there is a strong correlation between cord
blood H2O2 signal levels between the severe and less severe blood hydrogen peroxide(H2O2) levels and bilirubin concentra-
hyperbilirubinemic groups (Figure 3) revealed that a cord blood tions in the immediate neonatal period. This is the first clinical
H2O2 signal level of 2500 counts/10 seconds was the most suitable study to examine the direct association between hydrogen
cut-off value for predicting severe neonatal hyperbilirubinemia. peroxide levels and bilirubin concentrations. Our results suggest
This cut-off was associated with 76.2% sensitivity and 54.8% that cord blood hydrogen peroxide levels can be used to predict
specificity. We used three different cut-off H2O2 signal levels neonatal severe hyperbilirubinemia. Being able to identify
(2400, 2500, 2650 counts/10 seconds) to compare the severe and
Table 2. The different cut-off values of H2O2 signal for predicting severe hyperbilirubinemia were compared between the severe
hyperbilirubinemic group and the less severe hyperbilirubinemic group.
Cord Blood Luminol Signal (Counts/10 seconds) Sensitivity Specificity P Value*
2000 76.2% 40.6% 0.567
2200 76.2% 43.6% 0.443
2400 76.2% 49.6% 0.027
2500 76.2% 51.9% 0.017
2600 71.4% 53.4% 0.030
2800 71.4% 56.4% 0.157
2900 66.7% 56.4% 0.307
*Comparison was performed by chi-square test.
doi:10.1371/journal.pone.0086797.t002
PLOS ONE | www.plosone.org 3 January 2014 | Volume 9 | Issue 1 | e86797
H2O2 Predict Severe Hyperbilirubinemia
the extra-fetal environment. Hydrogen peroxide may damage red
blood cell membranes, leading to the production of bilirubin [19].
The greater the reactive oxidative product, such as hydrogen
peroxide level after birth, the more bilirubin is produced. Hence,
we can measure hydrogen peroxide levels as an indicator of severe
hyperbilirubinemia.
As previously mentioned, bilirubin is an antioxidant of reactive
oxygen/nitrogen species or nitric oxide [18,20]. Bilirubin can be
re-used as a substrate. Ideally, there will be a balance between
oxidant and antioxidants levels. Therefore, if the reactive oxygen
species levels increase beyond the antioxidant capability of
bilirubin, bilirubin concentrations will increase further. This
suggests that the relationship between hydrogen peroxide levels
and bilirubin concentrations is not a direct proportion. That is
why we cannot use it to predict less severely hyperbilirubinemic
neonate.
As early nursery discharge is encouraged to facilitate bonding
between the mother and newborn infant, early prediction of severe
hyperbilirubinemia is of vital importance. The widely used hour-
Figure 3. Receiver operating characteristic (ROC) curve of cord specific nomogram, described by Bhutani et al., only 68 among
blood hydrogen peroxide (H2O2) signals at the peak bilirubin 172 newborns in high risk zone remained in the zone later, which
concentration ($17 mg/dL). means only 39.5% of sensitivity for predicting severe hyperbiliru-
doi:10.1371/journal.pone.0086797.g003 binemia [15]. Low sensitivity is a major challenge in clinical
research of prediction of neonatal hyperbilirubinemia. In the
newborns at birth who are likely to develop subsequent severe present study, the described means of predicting severe hyperbil-
hyperbilirubinemia would be of obvious clinical benefit. irubinemia was associated with 76.2% sensitivity, far higher than
The greatest change after birth is the rapid transition from a low that associated with the conventional nomogram. Further, we
oxygen environment (fetus) to a high oxygen environment found that a cord blood H2O2 signal level .2500 counts/10
(neonate). During this change in environment, the oxygen seconds was a good predictor of severe hyperbilirubinemia. This
concentration increases more than three-fold. Oxidation plays a cut-off has a high negative predictive value (93.3%), which suggests
role in the delivery process [17,18]. Antioxidants levels remain low that if the cord blood hydrogen peroxide level is ,2500 counts/10
at birth; however, this induces a series of RBC breakdown and seconds, the chance of developing a dangerous bilirubin concen-
heme metabolic processes. There is an association between tration ($17 mg/dL) in the following days will be very low.
bilirubin concentrations and reductive and oxidative reactions. There were five newborns that developed severe hyperbiliru-
The CL signals emitted by whole blood and CL-emitting binemia despite having low cord hydrogen peroxide levels.
substance (luminol), have been shown to be useful for detecting Therefore, there are clearly other factors involved in the
H2O2 [16]. A higher H2O2 signal indicates lower anti-oxidant development of severe hyperbilirubinemia; hence, there is
activity and/or a decreased capacity for reactive oxygen species currently no single factor with a high sensitivity for predicting
scavenging. We found that the level of hydrogen peroxide severe hyperbilirubinemia. It may be necessary to incorporate
increases rapidly during the first few days of life, parallel with other risk factors, such as cord blood bilirubin concentrations and
the increase in bilirubin concentrations. The significant correlation hematocrit levels or body weight loss in early life, to increase the
between hydrogen peroxide levels and bilirubin concentration sensitivity for detecting hyperbilirubinemia [21].
supports our hypothesis. The increase in hydrogen peroxide levels In conclusion, we have found that there is a strong correlation
is caused by increasing oxygen levels in the transition from fetal to between cord blood hydrogen peroxide levels and bilirubin
Table 3. Comparison of demographic and cord blood data between newborns in the less severe hyperbilirubinemic group and
the five newborns who developed severe hyperbilirubinemia despite having a low cord blood hydorgen peroxide level.
Case no. GA (weeks) BW loss (%) Cord Blood Bilirubin (mg/dL) Cord Blood Hematocrit (%)
1 40 7.0 1.8q* 43
2 39 6.0 1.5 52q
3 39 9.1 2.0q 49q
4 40 7.8 1.5 50q
5 38 11.1q 1.8q* 42
Less severe icteric group 38.561.6 7.862.7 1.4060.67 43.165.77
(n = 133)
Abbreviations: GA, gestational age; BW, body weight.
BW loss: physiological body weight loss = (birth weight2lowest body weight)/birth weight.
Q or q: beyond mean 61 standard deviation when compared with the less severe icteric group.
q*: bilirubin concentration beyond mean 60.5 standard deviation when compared with the less severe hyperbilirubinemic group.
doi:10.1371/journal.pone.0086797.t003
PLOS ONE | www.plosone.org 4 January 2014 | Volume 9 | Issue 1 | e86797
H2O2 Predict Severe Hyperbilirubinemia
concentrations. The rising patterns were similar among bilirubin Acknowledgments
concentrations and hydrogen peroxide levels in the immediate
The authors thank to Dr. Hsieh Jia-Jung who provided the consultation of
neonatal period, both of which increase in concert during the first
statistical analysis part of this article.
several days of life. A cord blood H2O2 signal level cut-off of 2500
counts/10 seconds can be used as a good predictor of severe
Author Contributions
hyperbilirubinemia with a high negative predictive value. This
method provides which neonate should be followed after discharge Conceived and designed the experiments: HCC CTC MHC. Performed
from the nursery. the experiments: HCC CTC. Analyzed the data: HCC PNT CYC.
Contributed reagents/materials/analysis tools: HCC CTC WSH. Wrote
the paper: HCC.
References
1. Maisels MJ, McDonagh AF. (2008) Phototherapy for neonatal jaundice. 12. American Academy of Pediatrics. Provisional Committee for Quality Improve-
N Engl J Med 358: 920928. ment and Subcommittee on Hyperbilirubinemia. (1994) Practice parameter:
2. Gazzin S, Tiribelli C. (2011) Bilirubin-induced neurological damage. J Matern management of hyperbilirubinemia in the healthy term newborn. Pediatrics 94:
Fetal Neonatal Med 24 Suppl 1: 154155. 558565.
3. Johnson L, Bhutani VK. (2011) The clinical syndrome of bilirubin-induced 13. From the Centers for Disease Control and Prevention. (2001) Kernicterus in full-
neurologic dysfunction. Semin Perinatol 35: 101113. term infantsUnited States, 19941998. JAMA 286: 299300.
4. Rodrigues CM., Sola S, Brites D. (2002) Bilirubin induces apoptosis via the 14. Johnson LH, Bhutani VK, Brown AK. (2002) System-based approach to
mitochondrial pathway in developing rat brain neurons. Hepatology 35: 1186 management of neonatal jaundice and prevention of kernicterus. J Pediatr 140:
1195. 396403.
5. Greenberg DA. (2002) The jaundice of the cell. Proc Natl Acad Sci U S A 99: 15. Bhutani VK, Johnson L, Sivieri EM. (1999) Predictive ability of a predischarge
1583715839. hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in
6. Yigit S, Yurdakok M, Kilin K, Oran O, Erdem G, et al. (1999) Serum healthy term and near-term newborns. Pediatrics 103: 614.
16. Chien CT, Lee PH, Chen CF, Ma MC, Lai MK, et al. (2001) De novo
malondialdehyde concentration in babies with hyperbilirubinaemia. Arch Dis
demonstration and co-localization of free-radical production and apoptosis
Child Fetal Neonatal Ed 80: F235237.
formation in rat kidney subjected to ischemia/reperfusion. J Am Soc Nephrol
7. Stocker R, Glazer AN, Ames BN. (1987) Antioxidant activity of albumin-bound
12: 973982.
bilirubin. Proc Natl Acad Sci U S A 84: 59185922.
17. Pearce WJ, Butler SM, Abrassart JM, Williams JM. (2011) Fetal cerebral
8. Stocker R, Yamamoto Y, McDonagh AF, Glazer AN, Ames BN. (1987) oxygenation: the homeostatic role of vascular adaptations to hypoxic stress. Adv
Bilirubin is an antioxidant of possible physiological importance. Science 235: Exp Med Biol 701: 225232.
10431046. 18. Schneider H. (2011) Oxygenation of the placental-fetal unit in humans. Respir
9. Brito MA, Silva RF, Brites D. (2002) Bilirubin induces loss of membrane lipids Physiol Neurobiol 178: 5158.
and exposure of phosphatidylserine in human erythrocytes. Cell Biol Toxicol 18: 19. Iuchi Y, Kibe N, Tsunoda S, Suzuki S, mikami T, et al. (2010) Implication of
181192. oxidative stress as a cause of autoimmune hemolytic anemia in NZB mice. Free
10. Rao W, Zhang L, Su N, Wang K, Hui H, et al. (2013) Blockade of SOCE Radic Biol Med 48: 935944.
portects HT22 cellsfrom hydrogen peroxide-induced apotosis. Biochem Biophys 20. Baranano DE, Rao M, Ferris CD, Snyder SH. (2002) Biliverdin reductase: a
Res Commun 291: 17261729. major physiologic cytoprotectant. Proc Natl Acad Sci U S A 99: 1609316098.
11. Barone E, Trombino S, Cassano R, Sqambato A, De Paola B, et al. (2009) 21. Huang HC, Yang HI, Chang YH, Chang RJ, Chen MH, et al. (2012) Model to
Characterization of the S-denitrosylating activity of bilirubin. J Cell Mol Med predict hyperbilirubinemia in healthy term and near-term newborns with
13: 23652375. exclusive breast feeding. Pediatr Neonatol 53: 354358.
PLOS ONE | www.plosone.org 5 January 2014 | Volume 9 | Issue 1 | e86797
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Follow UPDocumento4 pagineFollow UPMeirinda HidayantiNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Daftar PustakaDocumento1 paginaDaftar PustakaMeirinda HidayantiNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- YOR-PICU-011 SpO2 Monitoring June 2013Documento7 pagineYOR-PICU-011 SpO2 Monitoring June 2013Meirinda HidayantiNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Risk FactorDocumento7 pagineRisk FactorMeirinda HidayantiNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Daftar PustakaDocumento1 paginaDaftar PustakaMeirinda HidayantiNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Daftar PustakaDocumento1 paginaDaftar PustakaMeirinda HidayantiNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- YOR-PICU-001 Updated en Guidelines Dec 2013Documento16 pagineYOR-PICU-001 Updated en Guidelines Dec 2013Meirinda HidayantiNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hyperglicemic Control in Ped Intensive CareDocumento12 pagineHyperglicemic Control in Ped Intensive CareMeirinda HidayantiNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Peran Tenaga Kesehatan Sebagai Pelaksana Pelayanan Pelayanan Kesehatan PuskesmasDocumento9 paginePeran Tenaga Kesehatan Sebagai Pelaksana Pelayanan Pelayanan Kesehatan PuskesmasIntar TeaNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Length/height-For-Age BOYS: Birth To 5 Years (Z-Scores)Documento1 paginaLength/height-For-Age BOYS: Birth To 5 Years (Z-Scores)Malisa LukmanNessuna valutazione finora
- Candidiasis in PICUDocumento6 pagineCandidiasis in PICUMeirinda HidayantiNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Presentation Title: Subheading Goes HereDocumento4 paginePresentation Title: Subheading Goes HereMeirinda HidayantiNessuna valutazione finora
- NI in PICUDocumento8 pagineNI in PICUMeirinda HidayantiNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Modern Management of Anal Fistula: Elsa Limura, Pasquale GiordanoDocumento10 pagineModern Management of Anal Fistula: Elsa Limura, Pasquale GiordanoMeirinda HidayantiNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Measurement Tools For The Diagnosis of NasalDocumento9 pagineMeasurement Tools For The Diagnosis of NasalMeirinda HidayantiNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Migraine Patient Handout PDFDocumento14 pagineMigraine Patient Handout PDFMeirinda HidayantiNessuna valutazione finora
- Generic and Trade Names of Drugs For Treatment of TonsillitisDocumento5 pagineGeneric and Trade Names of Drugs For Treatment of TonsillitisMeirinda HidayantiNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Steroids As Adjuvant Therapy For Acute Pharyngitis in Ambulatory Patients: A Systematic ReviewDocumento6 pagineSteroids As Adjuvant Therapy For Acute Pharyngitis in Ambulatory Patients: A Systematic ReviewDita AnisaNessuna valutazione finora
- Jurnal Mata PDFDocumento8 pagineJurnal Mata PDFMeirinda HidayantiNessuna valutazione finora
- 11CPG-Management of Sore ThroatDocumento26 pagine11CPG-Management of Sore ThroatmakeitrealityNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Olfactory Dysfunction in Patients With Chronic RhinosinusitisDocumento5 pagineOlfactory Dysfunction in Patients With Chronic RhinosinusitisClodeyaRizolaNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Carcinoma of The LarynxDocumento3 pagineCarcinoma of The LarynxMeirinda HidayantiNessuna valutazione finora
- Nej M 200101183440308Documento7 pagineNej M 200101183440308Meirinda HidayantiNessuna valutazione finora
- 25-36 Safaa Wafi PDFDocumento12 pagine25-36 Safaa Wafi PDFMeirinda HidayantiNessuna valutazione finora
- Nej MCP 051888Documento8 pagineNej MCP 051888Meirinda HidayantiNessuna valutazione finora
- 694-701 Yoeruek LoDocumento8 pagine694-701 Yoeruek LoMeirinda HidayantiNessuna valutazione finora
- Ceh 48Documento16 pagineCeh 48Meirinda HidayantiNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- QA CataractDocumento22 pagineQA CataractMeirinda Hidayanti100% (1)
- Johnson's Baby OilDocumento10 pagineJohnson's Baby OilVictor SolipasNessuna valutazione finora
- DBE South African Sign Language National Catalogue 2018Documento7 pagineDBE South African Sign Language National Catalogue 2018Anonymous ozd4aLKhNessuna valutazione finora
- Sex For BeginnersDocumento106 pagineSex For Beginnersmathan_20100% (4)
- Lucrare de Disertatie Satisfactia SexualaDocumento100 pagineLucrare de Disertatie Satisfactia Sexualamklogistica106100% (1)
- HR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenDocumento2 pagineHR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenMiltonGreenNessuna valutazione finora
- PE and Health 11Documento67 paginePE and Health 11Janafaye Krisha100% (1)
- Soares - Como Escolher Um Anestesico Local - 2005 PDFDocumento9 pagineSoares - Como Escolher Um Anestesico Local - 2005 PDFjvb sobralNessuna valutazione finora
- New Patient Medical Form: in One SentenceDocumento1 paginaNew Patient Medical Form: in One SentenceAzra BarliNessuna valutazione finora
- Perdev Week 5Documento3 paginePerdev Week 5AdiraNessuna valutazione finora
- MAPEH NasDocumento7 pagineMAPEH Nasnoronisa talusobNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Mapping Bellvitge 2023Documento8 pagineMapping Bellvitge 2023Lluís Cavallé MorenoNessuna valutazione finora
- Match The ProverbsDocumento1 paginaMatch The ProverbsКристин ВалентиноваNessuna valutazione finora
- Safety Legislation, Regulation and PolicyDocumento110 pagineSafety Legislation, Regulation and PolicyNichoNessuna valutazione finora
- Revised MARPOL Annex VDocumento6 pagineRevised MARPOL Annex VDiana MoralesNessuna valutazione finora
- First - Aid Common Emergencies and Safety Practices in Outdoor ActivitiesDocumento14 pagineFirst - Aid Common Emergencies and Safety Practices in Outdoor ActivitiesJhon Keneth NamiasNessuna valutazione finora
- Pathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun MengDocumento20 paginePathogenic Fungal Infection in The Lung: Zhi Li, Gen Lu and Guangxun Mengbanteng wibisonoNessuna valutazione finora
- Ethics Module 3Documento10 pagineEthics Module 3Shean BucayNessuna valutazione finora
- Dosis Ranitidin cw1Documento5 pagineDosis Ranitidin cw1Cristine Indria Pieter IINessuna valutazione finora
- Listening ComprehensionDocumento5 pagineListening ComprehensionLaura michell Núñez SuarezNessuna valutazione finora
- FAQ Mid Day MealsDocumento7 pagineFAQ Mid Day Mealsvikramhegde87Nessuna valutazione finora
- Patomorfologia Prezentacja - KopiaDocumento14 paginePatomorfologia Prezentacja - KopiaOlgaNessuna valutazione finora
- MSDS Bleach PDFDocumento5 pagineMSDS Bleach PDFAlfonso Alejandro Loayza RodriguezNessuna valutazione finora
- Facilitated Positional Release FPRDocumento12 pagineFacilitated Positional Release FPRcoahuiltecoNessuna valutazione finora
- Gn-31 Qms Cad (Dec 2012) FinalDocumento19 pagineGn-31 Qms Cad (Dec 2012) FinalSeanNessuna valutazione finora
- Mandela 2017Documento48 pagineMandela 2017Kibrom HaftuNessuna valutazione finora
- Movie Review: Temple Grandin by Tabatha O.Documento6 pagineMovie Review: Temple Grandin by Tabatha O.Tabatha100% (1)
- Errors of Eye Refraction and HomoeopathyDocumento11 pagineErrors of Eye Refraction and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNessuna valutazione finora
- Division of Blood Transfusion Services: Ministry of Health and Family WelfareDocumento40 pagineDivision of Blood Transfusion Services: Ministry of Health and Family WelfareKirandragonNessuna valutazione finora
- LUS HSE FM4 455 005.01 Audit Gap Analysis ChecklistDocumento10 pagineLUS HSE FM4 455 005.01 Audit Gap Analysis ChecklistRichu PaliNessuna valutazione finora
- AK Vegan Animals Lifescape 2008 (May) 74-6Documento3 pagineAK Vegan Animals Lifescape 2008 (May) 74-6Pepa GarcíaNessuna valutazione finora
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionDa EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionValutazione: 3.5 su 5 stelle3.5/5 (11)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindDa EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindValutazione: 4.5 su 5 stelle4.5/5 (1)
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerDa EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerValutazione: 4 su 5 stelle4/5 (5)
- Relentless: From Good to Great to UnstoppableDa EverandRelentless: From Good to Great to UnstoppableValutazione: 5 su 5 stelle5/5 (784)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingDa EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingValutazione: 4.5 su 5 stelle4.5/5 (66)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayDa EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNessuna valutazione finora
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouDa EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouValutazione: 3.5 su 5 stelle3.5/5 (5)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsDa EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsValutazione: 5 su 5 stelle5/5 (96)