Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Acute Pain
Caricato da
Patrick DycocoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Acute Pain
Caricato da
Patrick DycocoCopyright:
Formati disponibili
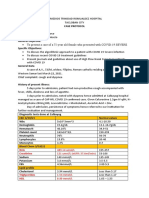
NURSING CARE PLAN
ASSESSMENT NURSING DIAGNOSIS RATIONALE OBJECTIVES NURSING INTERVENTIONS RATIONALE EVALUATION
3. Acute Pain related to Abdominal pain, cramping, Gen. Objective: Independent:
hyperperistalsis, prolonged diarrhea, and borborygmi may occur Relieve/ Reduce/ 1. Encourage patient/ child to May try to tolerate pain rather
skin/ tissue irritation, perirectal from gas released from Eliminate pain. report pain. than seek treatments.
excoriation, fissures as evidenced by undigested food, irritation 2. Assess reports of abdominal Changes in pain characteristics
reports of cramping or abdominal of bowel mucosa, distention cramping or pain, noting location may indicate spread of disease/
pain, guarding/ distraction behaviors of the intestines. Specific Objectives: duration, intensity,. Investigate and developing complications.
restlessness. After the nursing report changes in pain Child's primary way ofconveying
REF.: Medical & Surgical interventions have been characteristics. (Be very sensitive pain is maybe thru crying.
Nursing Textbook by employed, with the childs mov't or actions
Black & Hawks the child will be able to: e.g. crying as this suggests pain
pp. 809 - 810 Vol. I 1. Appear relax and be or something irritating to the child).
able to sleep or rest 3. Note nonverbal cues, e.g. Body language/ non verbal cues
appropriately. restlessness, reluctance to move, may be both physiological and
2. Report pain is relieved abdominal guarding. psychological and maybe used in
controlled. Investigate dispcrepancies between conjunction with verbal cues to
verbal and nonverbal cues. determine extent/ severity of the
problem.
4. Review factors that aggravate May pinpoint precipitating or
or alleviate pain. aggravating factors ( such as
stressful events, food
intolerance), or identify developing
complications.
5. Encourage patient to assume Reduces abdominal tension,
position of comfort, and promotes sense of control.
e.g. knees flexed as assisted by
the mother.
6. Provide comfort measures Promotes relaxation, refocuses
and diversional activities ( repositionattention, and may enhance coping
play with the child, offer toy) abilities. Promotes nurse - child
relationship.
7. Cleanse rectal area with mild soapProtecting skin from bowel acids,
and water/ wipes after each stool & preventing excoriation.
provide skin care. (Seek assistance from mother)
con.t
8. Observe/ record abdominal May indicate developing intestinal
distention, increased temperature, obstruction from inflammation,
. edema and scarring.
Collaborative:
1. Implement prescribed dietary Complete bowel rest can reduce
modification. pain, cramping.
2. Administer medications as
indicated:
Analgesics: For pain management,
Anticholinergics; relieve spasmsof Gi tract &
Antipyretics. lowers body temp. due to fever.
Patient is in NPO. 3. Imbalanced nutrition: less than Food and water intake is 3. Patient will be able to 1. Assess the over all nutritional To determine any deviation form
But could be given by body requirements realted to very essential since we can't demonstrate progress- status of the client by checking her previous data.
cotton water. inability to ingest/ digest food or survive without the two. ive weight gain toward daily weights, tissue integrity
absorb nutrients; N & V, NPO Gradual decrease of food goal with normalization & presence of adequate body fat
O: Patient is weak, status & nasogastric suctioning & intake would lead to body of laboratory values; and muscle mass.
restless, pallor, loss of appetite as evidenced by failure. Demonstrate behaviors, 2. Encourage client to choose To stimulate appetite.
showing expressions reported inadequate food intake lifestyle changes to foods that are appealing.
of difficulty with her less than RDA, lack of interest in regain and or maintain 3. Avoid foods that causes So as not to cause intestinal
situation. food "waray gana pagkaon,"/ appropriate weight. intolerances/ gastric motility problems.
aversion to eating & perceived (gas - forming foods, hot & spicy)
inability to digest food. 4. Limit fiber/ bulk. Since they can lead to early
satiety.
5. Promote pleasant, relaxing To stimulate proper appetite/
environment. enhance intake.
6. Limiting fluids hours prior to So as not to cause early
meal satiety.
7. Weigh weekly & prn. To monitor effectiveness of
care.
DISCHARGE PLANNING:
1. Emphasize importance of well
balance, nutritious intake.
2. Provide info regarding
individual needs & ways to meet
these needs within financial
constraints.
4. RISK for infection related to Body weakness would 4. Achieve timely 1. Demonstrate lifestyle changes For personal growth of the
inadequately primary defenses further lead to infections. healing. Be free of signs to promote safe environment. person.
(weak body), altered peristalsis, of infection 2. Cleanse insertion sites daily & To prevent sepsis.
change in pH secretions, Be afebrile. prn with solution.
nutritional deficiencies & stasis of 3. Encourage early ambulation, For mobilization of gastric
body fluids; chronic diseases, deep breathing, coughing, secretions.
position changes.
DISCHARGE PLANNING:
1. Explain the importance of proper
hygiene especially hand washing.
5. Ineffective breathing pattern Normal range of value for 5. The client will maintain 1. Maintain calm attitude, while To as to maintain and improve
O: RR 30 bpm. related to abdominal pain/ RR is 15 - 20 bpm. an effective breathing dealing with client to limit anxiety. rapport.
Patient having deep,tenderness as evidenced by RR 30 pattern as evidenced by 2. Assist client in use of relaxation So as to relax the client from
shallow, irregular bpm, anxiety/ decreased energy, RR within normal limits, techniques. the tension and anxiety she is
breathing. fatigue. relaxed respiratory effort suffering.
Demonstrate approp.
coping behaviors.
S: Patient uttered, 6. Anxiety related to change in Anxiety is a vague feeling 6. The client will express 1. Assess the client's level of To determine what interventions
"Tangala na ini na health status, change in of apprehension as to what and demonstrate anxiety by listening and observing. are suitable for the client.
adi tak may irong." environment, fear of pain returning will happen next. It is a normal decreasing 2. Reassure the client and To let the client feel secured,
& irritation brought about by the defense mechanism of the manifestations of acknowledge that the unknown is that she is not alone.
O: Fatigue, touchi NGT tube attached. body. anxiety as evidenced of frightening.
the NGT tube which displaying behavior 3. Allow significant others to
she wants to be associated with remain with the client.
removed. relaxation.
NAME: ROOM & BED #:
AGE/SEX: WARD:
CHIEF COMPLAINT: ATTENDING PHYSICIAN:
Prepared by: Submitted to:
DONN ED MARTIN A. ABRIL MR. ROBERT PONTIAN AGNER, R.N.
RTRMF - CN Student Nurse Clinical Instructor
EVRMC
15-Nov-05
Potrebbero piacerti anche
- Heavy Metal Intoxication and Chelators MCQ Answer SheetDocumento4 pagineHeavy Metal Intoxication and Chelators MCQ Answer SheetPatrick Dycoco75% (4)
- Case Protocol Covid SevereDocumento3 pagineCase Protocol Covid SeverePatrick DycocoNessuna valutazione finora
- Approach To Liver HH (Autosaved)Documento59 pagineApproach To Liver HH (Autosaved)Patrick Dycoco100% (1)
- EVRMC 1st EndorsementDocumento4 pagineEVRMC 1st EndorsementPatrick DycocoNessuna valutazione finora
- History Taking 3Documento4 pagineHistory Taking 3Patrick DycocoNessuna valutazione finora
- Cerebral PerfusionDocumento5 pagineCerebral PerfusionPatrick DycocoNessuna valutazione finora
- Case Study - BlenteDocumento10 pagineCase Study - BlentePatrick DycocoNessuna valutazione finora
- CHFDocumento7 pagineCHFPatrick DycocoNessuna valutazione finora
- Related Lit Additional (Mercado)Documento7 pagineRelated Lit Additional (Mercado)Patrick DycocoNessuna valutazione finora
- Spot Map Part 1Documento1 paginaSpot Map Part 1Patrick DycocoNessuna valutazione finora
- PCM Epidemiology of Yellow FeverDocumento7 paginePCM Epidemiology of Yellow FeverPatrick DycocoNessuna valutazione finora
- Spot Map Part 1Documento1 paginaSpot Map Part 1Patrick DycocoNessuna valutazione finora
- Dengue Pedia MMCDocumento26 pagineDengue Pedia MMCPatrick DycocoNessuna valutazione finora
- Dengue Pedia MMCDocumento26 pagineDengue Pedia MMCPatrick DycocoNessuna valutazione finora
- STDDocumento69 pagineSTDPatrick DycocoNessuna valutazione finora
- IntussusceptionDocumento10 pagineIntussusceptionPatrick DycocoNessuna valutazione finora
- AsthmaDocumento72 pagineAsthmaPatrick DycocoNessuna valutazione finora
- Gugon, Pcap DDocumento6 pagineGugon, Pcap DPatrick DycocoNessuna valutazione finora
- Acute GastroenteritisDocumento4 pagineAcute GastroenteritisPatrick DycocoNessuna valutazione finora
- Tetralogy of Fallot with Hypercyanotic SpellsDocumento11 pagineTetralogy of Fallot with Hypercyanotic SpellsPatrick DycocoNessuna valutazione finora
- Acute PancreatitisDocumento7 pagineAcute PancreatitisPatrick DycocoNessuna valutazione finora
- TofDocumento5 pagineTofPatrick DycocoNessuna valutazione finora
- Review of SystemsDocumento2 pagineReview of SystemsPatrick DycocoNessuna valutazione finora
- Difficulty Breathing Patient InterviewDocumento1 paginaDifficulty Breathing Patient InterviewPatrick DycocoNessuna valutazione finora
- PCM Epidemiology of Yellow FeverDocumento7 paginePCM Epidemiology of Yellow FeverPatrick DycocoNessuna valutazione finora
- Superficial MycosesDocumento6 pagineSuperficial MycosesPatrick DycocoNessuna valutazione finora
- SeizureDocumento7 pagineSeizurePatrick DycocoNessuna valutazione finora
- Blood Supply of Head and NeckDocumento44 pagineBlood Supply of Head and NeckPatrick DycocoNessuna valutazione finora
- Distance & Speed ProblemsDocumento2 pagineDistance & Speed ProblemsAnonymous GNWnQacNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Vangsness2009 GlucosamineDocumento9 pagineVangsness2009 GlucosaminebuddybbuddyNessuna valutazione finora
- Implementing Guidelines for Health Discounts and Privileges for PWDsDocumento11 pagineImplementing Guidelines for Health Discounts and Privileges for PWDsjeffrey arzagaNessuna valutazione finora
- Paper On Intergenerational TraumaDocumento13 paginePaper On Intergenerational TraumaEdith G.LebelNessuna valutazione finora
- DrugsDocumento17 pagineDrugsQais ShaikhNessuna valutazione finora
- Chocolate Milk Argument Essay SamplesDocumento3 pagineChocolate Milk Argument Essay Samplesapi-349881433100% (4)
- PenicillinDocumento75 paginePenicillinJean CabigaoNessuna valutazione finora
- Prepare Sponge and CakesDocumento30 paginePrepare Sponge and Cakesmarilyn rosilNessuna valutazione finora
- CrohnsDocumento19 pagineCrohnsLauren LevyNessuna valutazione finora
- Ohi Graphic OrganizerDocumento1 paginaOhi Graphic Organizerapi-278298083Nessuna valutazione finora
- Digestive Disorders April 2007 PDFDocumento8 pagineDigestive Disorders April 2007 PDFAnanta RanaNessuna valutazione finora
- Teaching Plan On Newborn ScreeningDocumento8 pagineTeaching Plan On Newborn ScreeningQueenie Sicco100% (1)
- Birštonas Toursim Manual 2022Documento64 pagineBirštonas Toursim Manual 2022Visit BirštonasNessuna valutazione finora
- IMPLANT OCCLUSION GUIDEDocumento57 pagineIMPLANT OCCLUSION GUIDEElango2548994% (16)
- Pain Management: Dr. Surya Bayu Prajayana, M.Biomed, Sp. OTDocumento22 paginePain Management: Dr. Surya Bayu Prajayana, M.Biomed, Sp. OTOgizWaraNessuna valutazione finora
- EVOLUTION OF CARD REPERTORYDocumento7 pagineEVOLUTION OF CARD REPERTORYRahul RamanNessuna valutazione finora
- Narcotics Anonymous Meeting 3Documento6 pagineNarcotics Anonymous Meeting 3api-401390929Nessuna valutazione finora
- CPT ChecklistDocumento1 paginaCPT ChecklistphilippepreanNessuna valutazione finora
- 1 - O - Anuruddha KumaraDocumento8 pagine1 - O - Anuruddha Kumaraumapati 1505Nessuna valutazione finora
- Anxiety DisorderDocumento9 pagineAnxiety DisorderSatish KujurNessuna valutazione finora
- RN review nuggets: Essential fundamentals of nursingDocumento32 pagineRN review nuggets: Essential fundamentals of nursingr.a.g.Nessuna valutazione finora
- Postpartum HaemorrhageDocumento19 paginePostpartum HaemorrhageJonas Marvin AnaqueNessuna valutazione finora
- COR PULMONALE - MahasiswaDocumento14 pagineCOR PULMONALE - MahasiswaGalih Maygananda PutraNessuna valutazione finora
- Psychology Presentation Chapter 10 - Life Span DevelopmentDocumento15 paginePsychology Presentation Chapter 10 - Life Span DevelopmentEduardo VillanuevaNessuna valutazione finora
- Classroom Lesson PlansDocumento34 pagineClassroom Lesson PlansZakia Aikaz100% (1)
- GDC Dental Team WorkingDocumento12 pagineGDC Dental Team WorkingRamona RochianNessuna valutazione finora
- DisolusiDocumento47 pagineDisolusiNoonaNuzha Lestary NuzhaAyuNessuna valutazione finora
- Reverse AlzheimersDocumento40 pagineReverse Alzheimersakajhon100% (9)
- Female Welfare ProgrammeDocumento6 pagineFemale Welfare ProgrammeAnnapurna DangetiNessuna valutazione finora
- Transcatheter EmbolizationDocumento9 pagineTranscatheter EmbolizationPatrick SalengaNessuna valutazione finora
- AmenorrheaDocumento41 pagineAmenorrheaDewi Felayati Gusni100% (2)