Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Medical Record 1
Caricato da
Costel GoreCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Medical Record 1
Caricato da
Costel GoreCopyright:
Formati disponibili
MEDICAL RECORD
The medical interview is the process of gathering data that will lead to an understanding of the
disease and the underlying physiological process. To be effective, an interviewer must possess
good communication skills and be alert to nonverbal clues as well as to the verbal message.
Often, more information is conveyed by nonverbal actions and tone of voice than by words. The
objective is to obtain an accurate and comprehensive picture of the patients situation, including
the nature and timing of symptoms, emotional factors (including types of stress), and past
medical conditions that may place the patient at greater risk for certain diseases.
The accuracy and usefulness of the medical interview depend on the physicians ability to elicit
information pertinent to the problem at hand and on the patients accurate recall and articulation
of the sequence of symptoms. This may be difficult, because meaningful data may be forgotten if
the patient is experiencing pain or emotional distress. The skilled interviewer knows when to use
silence, open-ended questions, or specific closed-ended questions to explore avenues in which
the most useful information may be found. The real reason for the patients visit may not be
apparent until a rapport has been established and the person feels comfortable describing what is
most bothersome. Problems that are emotionally threatening may not be voiced until adequate
courage has been summonedsometimes not until the end of the appointment when the patients
hand is on the doorknob.
To begin the Examination
Wash your hands.
Introduce yourself to the patient (first name, surname, medical studentstatus)
Greet the patient (title and surname).called.
Explain what you would like to do and seek consent for the examination.
Explain what you are about to do at each stage without using jargon.
PThenosition the patient appropriately (45 degrees for cardiovascular and
respiratory, flat for abdominal).
Then expose the relevant part of the patient ensuring as much privacy as possible.
Perform a general inspection from the end of the bed. Dont forget to look at the
surroundings (for sputum pot, central line, walking stick, etc.).
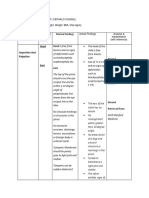
MEDICAL RECORD TEMPLATE
Patient Patient name
demographics Date of birth
Patient sex
Patient address
Admission details Admission method (How the patient was admitted to hospital. Eg:
elective,
emergency, maternity, transfer, etc.)
Source of admission (Where the patient was immediately prior to
admission, eg, usual place of residence, temporary place of
residence, penal establishment.)
Relevant clinical Relevant clinical riskf actors (Factors that have been shown to be
risk factors associated with the development of a medical condition being
considered as a diagnosis/differential diagnosis. Eg being
overweight, smoker, no use of sun screen, enzyme deficiency, poor
sight (can impact on falls), etc.)
Risk mitigation (Action taken to reduce the clinical risk, including
thromboembolic preventative action and date actioned.)
Reason for The health problems and issues experienced by the patient resulting
admission in their referral by a healthcare professional for hospital admission,
eg, chest pain, blackout, fall, a specific procedure, investigation or
treatment.
Presenting The list and description of the health problems and issues
complaints or issues experienced by the patient resulting in their attendance. These may
include disease state, medical condition, response and reactions to
therapies. Eg blackout, dizziness, chest pain, follow up from
admission, falls, a specific procedure, investigation or treatme
Medical history History of each presenting complaint or issue (Information directly
related to the development and characteristics of each presenting
complaint (eg, including travel history). Including if the information
is given by the patient or their carer
Relevant past medical, surgical and mintal health history (The
record of the patients significant medical, surgical and mental
health history. Including relevant previous diagnoses, problems and
issues, procedures, investigations, previous hospitalizations, etc
(will include dental and obstetric history)
Management to date (Referrals, management, investigations and
treatment that have already been undertaken, including patient
managing their symptoms. Including: Procedures conducted
procedures carried out (and the date) and procedure report.
Drug history (medication the patient is taking (prescribed and over
the counter; medication that the patient is known to be sensitive to)
Allergies and Causative agent (The agent such as food, drug or substances that has
adverse reaction caused or may cause an allergy, intolerance or adverse reaction in
this patient.)
Description of the A description of the manifestation of the allergic
or adverse reaction reaction experienced by the patient.)
Date first experienced
Personal Early development / Childhood / School / Adolescence
History/Development Occupation
Menstrual history / Sexual history /Marital history / Children
Social context Household composition (Eg: lives alone, lives with family, lives
with partner, etc. This may be plain text.)
Lifestyle (The record of lifestyle choices made by the patient which
are pertinent to his or her health and well-being, eg, the record of
the patients physical activity level, pets, hobbies, sexual habits and
the current and previous use of recreational drugs.)
Smoching (Latest or current smoking observation)
Alcohol intake (Latest or current alcohol consumption observation)
Occupational history (The current and/or previous relevant
occupation(s) of the patient/individual. The occupational history is
important because the workplace may be a source of toxins, such as
chemicals, asbestos fibres, or cigarette smoke, that place one at
higher risk of cancer or other diseases.
Family history Included in a family history are the age and state of health of each
immediate family member as well as the cause of death of any
parents, grandparents, and other close relatives. Of particular
importance are genetic or environmental diseases that have known
risks.
Any disease that arises in two or more members of a family suggests
a possible predisposing factor, and the patient should be considered
to be at increased risk for this condition.
Examination The record of findings from clinical examination
findings The record of a clinicians first impression assessment including
general clinical examination finding, eg,
obese/malnourished/cachectic, height, weight, symmetry, and
posture etc. confusion, delirium, coma
Vital signs The record of essential physiological measurements, eg, heart rate,
blood pressure, temperature, pulse, respiratory rate, level of
consciousness.
The record of The physical examination continues the diagnostic process, adding
findings from information obtained by inspection, palpation, percussion, and
examination auscultation.
Palpation is the act of feeling the surface of the body with the hands
to determine the characteristics of the organs beneath the surface. It
can be performed with one hand or two and can be light or deep.
Gentle palpation begins farthest away from the pain to localize the
point of maximum tenderness.
Percussion is a diagnostic procedure used to determine the density
of a part by tapping the surface with short, sharp blows and
evaluating the resulting sounds.
Auscultation is performed with a stethoscope to evaluate sounds
produced by the heart, the lungs, the blood vessels, or the bowels.
If the presenting complaint is pain (most types of pain e.g. chest,
abdominal etc) the main points to elicit can easily be remembered
using the mnemonic SOCRATES.
S -site
O -onset
C -character
R -radiation
A - associations
T -timing
E -exacerbating & relieving factors
S -severity
Remember to ask about use of medication for pain relief.
For details consult: A Practical Guide to Clinical Medicine
http://meded.ucsd.edu/clinicalmed/
Review of systems / organs:
o Integument
o Eyes
o Ears Nose Mouth Throat
o Head and neck
o Cardio-vascular
o Respiratory
o Gastrointestinal
o Genitourinary
o Musculoskeletal
o Lymphatic
o Neurological
o Mental state /Psychiatric
o Endocrine
Provisional diagnosis The diagnosis will require you to synthesise predisposing and
perpetuating factors and signs / symptoms in the case report to
identify core problems. You should explicate your reasoning for
drawing the links between signs and symptoms and diagnostic
decision-making. In other words, what important aspects in the
History, Mental State Examination and Physical Examination lead
you to making the provisional diagnosis? An accurate conclusion
depends on the timing and the sequence of the symptoms, past
medical history and risk factors for certain diseases, and a recent
exposure to disease.
Examination A procedure completed as part of the examination of the patient. Eg
procedure sygmoidoscopy, lumbar puncture, pleural tap, etc.
Problems and issues (Summary of problems that require
investigation or treatment. This would include significant
examination findings which are likely to have relevance, yet are not
a diagnosis. In mental health and psychiatry, this may be the place
for formulation.)
Investigations: Investigations requested (This includes a name or description of the
laboratory tests / investigation requested)
imaging Investigations results (this includes the result value, with unit of
instruments observation and reference interval where applicable and date), and
/procedures plans for acting upon investigation results.)
Investigatioons results discussion
Differential The determination of which one of several diseases may be
diagnosis producing the symptoms.
Take each differential diagnosis and write down the pros and cons
evident in the earlier parts of your report that serve to support or
discount the likelihood of the differential diagnosis.
Pick out the relevant pieces of these sections and make links with
the final diagnosis.
Final diagnosis The diagnostic process is the method by which health professionals
select one disease over another, identifying one as the most likely
cause of a persons symptoms.
In making a final diagnosis, also relies on various other clues such
as the results of selected laboratory and radiological and other
imaging tests.
You should explicate your reasoning for drawing the links between
signs and symptoms and investigations results and differential
diagnoses.
Include the stage of the disease where relevant.
Medications and Medication name (May be generic name or brand name (as
medical devices appropriate).
Medication form (Eg capsule, drops, tablet, lotion etc)
Route (Medication administration description (oral, IM
(intramuscular), IV intravenous), etc): may include method of
administration, (eg, by infusion, via nebuliser, via NG (nasogastric)
tube) and/or site of use (eg, to wound, to left eye, etc)
Dose (This is a record of the total amount of the active ingredient(s)
to be given at each administration. It should include, eg, units of
measurement, number of tablets, volume/concentration of liquid,
number of drops, etc.
Medication frequency (Frequency of taking or administration of the
therapeutic agent or medication.)
Reason for medication (Reason for medication being prescribed,
where known.)
Medication recommendations (Suggestions about duration and/or
review, ongoing monitoring requirements, advice on starting,
discontinuing or changing medication)
Reason for non-administration
Information and The oral or written information or advice given to the patient, carer,
advice given other authorised representative, care professional or other third
party. May include advice about actions related to
medicines or other ongoing care activities on an information
prescription. State here if there are concerns about the extent to which
the patient and/or carer understands the information provided about
diagnosis, prognosis and treatment.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Nursing ProcessDocumento17 pagineThe Nursing ProcessElla Lobenaria100% (1)
- Physical ExaminationDocumento117 paginePhysical Examinationsasmita nayakNessuna valutazione finora
- Physical ExaminationgiDocumento61 paginePhysical ExaminationgiHei LeeNessuna valutazione finora
- Vomiting in PregnancyDocumento13 pagineVomiting in PregnancyPriyanka John100% (4)
- Clinical Examination of Companion AnimalsDocumento6 pagineClinical Examination of Companion AnimalsLouise Alysson OrtegaNessuna valutazione finora
- Health Assesment LectureDocumento15 pagineHealth Assesment LecturemeowzartNessuna valutazione finora
- Purina Body Condition Score DiagramDocumento1 paginaPurina Body Condition Score DiagramRonnel Anthony CelerioNessuna valutazione finora
- Askling ProtocolDocumento8 pagineAskling Protocolchrisschapendonk123Nessuna valutazione finora
- Nursing Care: Musculoskeletal SystemDocumento13 pagineNursing Care: Musculoskeletal SystemSukmawati PassiNessuna valutazione finora
- Assessment Mouth and Oropharynx LipsDocumento8 pagineAssessment Mouth and Oropharynx LipsQuinmarc LimNessuna valutazione finora
- (Undefined Series For Scimag) - Libgen - LiDocumento7 pagine(Undefined Series For Scimag) - Libgen - LiNicholas LimNessuna valutazione finora
- HEAS 1000 Health Assessment: Reflection of PracticeDocumento4 pagineHEAS 1000 Health Assessment: Reflection of PracticePreet ChahalNessuna valutazione finora
- Cerebral Palsy Amdekar SirDocumento42 pagineCerebral Palsy Amdekar SirVishalSapateNessuna valutazione finora
- Clinical Examination of Varicose VeinsDocumento6 pagineClinical Examination of Varicose VeinsR.m. AndriyanNessuna valutazione finora
- Chinese Herbology Study GuideDocumento58 pagineChinese Herbology Study Guidegiovanna2004100% (1)
- Health Assessment JarvisDocumento14 pagineHealth Assessment JarvisLilly Daye81% (31)
- CVS Study Guide 2023Documento28 pagineCVS Study Guide 2023Muhammad SulamanNessuna valutazione finora
- Assessment of The Abdomen ChecklistDocumento4 pagineAssessment of The Abdomen ChecklistKyle Randolf CuevasNessuna valutazione finora
- Po1 Po2 Po3 Po4 Po5 Po6 Po7 Po8 Po9 Po10 Po11 Po12 Po13 Po14Documento16 paginePo1 Po2 Po3 Po4 Po5 Po6 Po7 Po8 Po9 Po10 Po11 Po12 Po13 Po14Jerry AbleNessuna valutazione finora
- Abdominal Exam GuideDocumento5 pagineAbdominal Exam GuideNesma AdelNessuna valutazione finora
- Here are the zones in hand reflexology:Zone 1:Zone 2: Zone 3:Zone 4: Zone 5:Zone 6:Zone 7:Zone 8: Zone 9:Zone 10:Zone 11:Zone 12Documento12 pagineHere are the zones in hand reflexology:Zone 1:Zone 2: Zone 3:Zone 4: Zone 5:Zone 6:Zone 7:Zone 8: Zone 9:Zone 10:Zone 11:Zone 12Kim Caguioa100% (2)
- AssessmenDocumento1.083 pagineAssessmenluizamgoNessuna valutazione finora
- Breast Examination: 1. Iintroduction and Consent 2. ExposureDocumento4 pagineBreast Examination: 1. Iintroduction and Consent 2. ExposureNoor Ul AinNessuna valutazione finora
- Breast Exam GuideDocumento2 pagineBreast Exam GuideAyman HajeerNessuna valutazione finora
- Fundamentals of Nursing 9th Edition by Taylor Lynn Bartlett Test BankDocumento8 pagineFundamentals of Nursing 9th Edition by Taylor Lynn Bartlett Test Bankkathleenbaileytcgsrikobx100% (28)
- Case StudyDocumento6 pagineCase StudyEndla SriniNessuna valutazione finora
- Assessment Method Used Normal Findings: Head Head Is Free FromDocumento6 pagineAssessment Method Used Normal Findings: Head Head Is Free FromGil PerezNessuna valutazione finora
- Shamsurin CWU AwerzDocumento10 pagineShamsurin CWU AwerzAiman ArifinNessuna valutazione finora
- Examination of The BreastDocumento2 pagineExamination of The BreastAufi FillaNessuna valutazione finora