Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Steroid-Induced Iatrogenic Glaucoma
Caricato da
Lenyi Iyo AlbertiCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Steroid-Induced Iatrogenic Glaucoma
Caricato da
Lenyi Iyo AlbertiCopyright:
Formati disponibili
Review
Ophthalmic Res 2012;47:6680 Received: September 1, 2010
Accepted after revision: April 4, 2011
DOI: 10.1159/000328630
Published online: July 13, 2011
Steroid-Induced Iatrogenic Glaucoma
M.RezaRazeghinejad a,b L.JayKatz b
a
Department of Ophthalmology, Shiraz University of Medical Sciences, Shiraz, Iran;
b
Wills Eye Institute, Philadelphia, Pa., USA
Key Words Introduction
Steroid-induced ocular hypertension Glaucoma
Intravitreal drug delivery The discovery of steroids was a major breakthrough in
the treatment of various autoimmune and inflammatory
diseases. Like other therapeutic agents, these medica-
Abstract tions have their own side effects, including ocular hyper-
Steroids in susceptible individuals can cause a clinical condi- tension and iatrogenic glaucoma. The issue of steroid-
tion similar to primary open-angle glaucoma. Five percent of induced iatrogenic glaucoma was first described in
the population are high steroid responders and develop an the 1950s with the observation of glaucoma in associa-
intraocular pressure (IOP) elevation of more than 15 mm Hg tion with administration of systemic adrenocorticotrop-
above baseline. IOP elevation may occur as early as 1 day to ic hormones or topical and systemic steroids [13]. Arma-
as late as 12 weeks after intravitreal triamcinolone in 2065% ly and Becker [4] and Becker [5] independently report-
of patients. On average, 75% of eyes with steroid implants ed that the normal population could be divided into 3
require IOP-lowering therapy at some point within 3 years of groups based on their response to the topical administra-
follow-up. The exact mechanism of steroid-induced glau- tion of dexamethasone and bethamethasone: (1) high re-
coma is not totally understood, but decreased trabecular sponders, 46% of the population, developed an intra-
meshwork outflow is regarded as the main cause of IOP el- ocular pressure (IOP) above 31 mm Hg or a rise of more
evation. High-risk patients who receive steroids should be than 15 mm Hg above baseline; (2) moderate responders,
monitored closely and if they develop elevated IOP, steroids approximately one third of the population, had IOPs be-
with lower potency or steroid-sparing agents should be tween 20 and 31 mm Hg, or a pressure rise of 615 mm
used. The IOP usually returns to normal within 24 weeks Hg; nonresponders, the remaining two thirds, had pres-
after stopping the steroid. About 15% of patients do not sure increases of less than 6 mm Hg and IOPs of less than
respond to medical therapy and need surgery. Trabeculec- 20 mm Hg.
tomy, trabeculotomy, shunt surgery, and cyclodestructive The most common routes of inducing iatrogenic hy-
procedures are among the methods employed. Removal of pertension or glaucoma are topical and intraocular or
residual sub-Tenon or intravitreal steroids may help hasten periocular administration. It can also occur after receiv-
the resolution of the steroid response. Early results with ing systemic steroids, application to the skin, intranasal-
anecortave acetate, an analog of cortisol acetate with anti- ly, or by inhalation [6].
angiogenic activity, in controlling IOP have been promising. With the advent of laser refractive surgery and post-
Copyright 2011 S. Karger AG, Basel operative steroid use, cases of severe IOP elevation have
179.7.82.148 - 2/7/2017 1:18:14 AM
2011 S. Karger AG, Basel L. Jay Katz, MD
00303747/12/04720066$38.00/0 Glaucoma Service at Wills Eye Institute
Fax +41 61 306 12 34 840 Walnut Street, Suite 1130
E-Mail karger@karger.ch Accessible online at: Philadelphia, PA 19107 (USA)
Downloaded by:
www.karger.com www.karger.com/ore Tel. +1 215 928 0166, E-Mail LJKwayne@aol.com
been reported [7, 8]. Corneal-induced errors in IOP mea- weeks) [37]. IOP elevation after IVTA usually occurs 12
surement, decreased corneal thickness and the accumu- months after injection [24, 38], but Smithen et al. [22] re-
lation of fluid beneath the Lasik flap may be possible ported the occurrence at a mean of 100.6 days. However,
reasons for the failure to recognize steroid-induced Singh et al. [39] reported 3 cases of early and rapid in-
iatrogenic glaucoma [9, 10]. The current popular use of creases in IOP within 1 week following an IVTA injec-
intravitreal triamcinolone acetonide (IVTA) for various tion. All patients were pseudophakic, which may have al-
vitroretinal diseases has led to an increased incidence of lowed the medication to move into the anterior segment,
corticosteroid-induced ocular hypertension or glaucoma causing physical obstruction of the trabecular meshwork.
from IVTA [1125]. As the list of indications and use of In 1 patient, a whitish deposit was observed in the infe-
IVTA increases, the incidence of IOP elevation secondary rior angle in gonioscopy. Vedantham [40] suggested that
to IVTA will be more common and more likely to be en- pseudophakic patients and those with prior vitrectomies
countered by ophthalmologists. This review will address should be followed closely. In addition, he suggested in-
the issue of steroid-induced iatrogenic hypertension or structing these patients to sleep on their backs to prevent
glaucoma with an emphasis on the glaucoma associated the migration of triamcinolone into the anterior cham-
with IVTA. ber.
Different formulations of the same drug may have dif-
ferent effects on IOP. For example, triamcinolone aceton-
Timing of Response ide sub-Tenon injection, a minimally water-soluble agent,
can induce IOP elevations for as long as 6 months, but the
The time frame when ocular hypertension begins de- diacetate form of the drug is moderately water soluble
pends on the specific drug, the dosage, the frequency and and thus tends to have a briefer effect on the IOP [4143].
route of administration, and the susceptibility of the in-
dividual patient. The incidence of steroid-induced iatro-
genic glaucoma or ocular hypertension following system- Risk Factors
ic therapies is much less common than following topical
administration. Although an acute response has been re- The possibility of high response is greater in the fol-
ported with intensive systemic steroid therapy, the IOP lowing cases: patients with primary open-angle glauco-
response often occurs over years [26]. Bernstein and ma (POAG) or glaucoma suspects, first-degree relatives
Schwartz [27] reported that patients who had been on sys- with POAG [44], old age or age less than 6 years, connec-
temic steroids for more than 4 years had significantly tive tissue disease, especially rheumatoid arthritis in men
higher IOPs than those who had received systemic ste- [45], high myopia [46, 47], type 1 diabetes mellitus [37,
roids for less than a year. 48], and angle recession glaucoma [49]. Patients with pre-
Although the majority of studies reported that IOP disposing risk factors should be monitored more dili-
rises 36 weeks after the beginning of topical steroid use, gently when receiving corticosteroids.
some elevation of pressure can be found in most patients
as early as the first or second week [2831]. Armaly [28, Primary Open-Angle Glaucoma
29] noted that normal patients developed the hyperten- Armaly [28, 29] reported that approximately one third
sive effect of steroid at the end of the first week, with a of glaucoma suspects and more than 90% of patients with
mean increase in pressure of 19%. It almost never occurs POAG experienced an IOP elevation greater than 6 mm
sooner than 5 days [32]. Failure of IOP to increase after 6 Hg after receiving topical 0.1% dexamethasone for 4
weeks of steroid treatment is no assurance that it will not weeks. Becker and Mills [50] also indicated that glauco-
increase if treatment is continued [33]. ma or glaucoma suspect patients who received topical
There may be a delay in the onset of the increase in IOP 0.1% betamethasone for 24 weeks demonstrated large,
of up to several months after corticosteroid injections [22, highly significant increases in IOP and exhibited de-
3436]. In Kalinas [36] study, 18 ocular hypertensions creased outflow facility during the treatment period. The
were seen after the subconjunctival injection of reposi- IOP returned to baseline or normal in approximately 1
tory corticosteroid at a mean of 7.1 weeks (range: 1.516 week after discontinuing the drops [50].
weeks) and lasted for a mean duration of 3 months. Ret- Whereas 1836% of the general population shows a
robulbar injection of triamcinolone acetonide resulted in moderate increase in IOP after the topical administration
an elevation of IOP at a mean of 5.2 weeks (range: 113 of corticosteroids, 56% of the general population versus
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 67
Downloaded by:
4692% of patients with POAG have a significant in- occurs more frequently, more severely, and more rapidly
crease in IOP [28, 29, 5052]. Studies of patients with sec- than that reported in adults. Although older patients are
ondary open-angle glaucoma generally do not find such at increased risk, the frequency of steroid responsiveness
a high response rate [53]. Other studies showed that sim- with age may occur in a bimodal distribution and chil-
ply having a first-degree relative with POAG could make dren should be monitored closely.
one susceptible to being a high steroid responder [50, 54].
However, having POAG or a first-degree relative with Diabetes Mellitus
POAG is not an absolute contraindication for steroid use Becker et al. [62] reported that the steroid IOP-increas-
because sometimes steroids are the most effective treat- ing effect was greater in diabetic patients . In a retrospec-
ment modality. Given that patients who have undergone tive study of 49 patients who received one trans-Tenon
filtering surgery have an alternate outflow pathway, it is retrobulbar injection of triamcinolone acetonide (20 mg),
plausible that their IOP should be minimally affected by Hirooka et al. [37] reported that the only preoperative
the administration of steroids. In a study by Oliver et al. predictive factor for steroid responders was the presence
[55] of 9 patients with prior glaucoma surgery who re- of diabetes mellitus (multiple logistic regression analysis,
ceived IVTA, the mean difference between pre-IVTA and odds ratio = 32.78, p = 0.006). In contrast, in a prospective
maximum post-IVTA IOP was 1 mm Hg. Only 2 patients study of 60 patients who received IVTA, Park et al. [21]
required additional medication to control their IOP. Fi- found that diabetes mellitus had no correlation with IOP
nally, some studies indicate that normal individuals clas- elevation.
sified as high steroid responders were more likely to de-
velop glaucoma [56]. Testing for steroid responsiveness by Genetic Susceptibility
topical agents to identify patients at risk of developing It has been suggested that a genetic difference exists
POAG has not become routine because of the variability between corticosteroid responders and nonresponders
in the extent of response and the potential risk to normal and that patients who show an increase in IOP have a dif-
individuals [5]. ferent or more sensitive corticosteroid receptor. Some re-
searchers tried to explain this genetic susceptibility by a
Age monozygotic autosomal mechanism. It was suggested
It has been demonstrated that the steroid IOP-increas- that medium responders were heterozygous while high
ing effect is greater in older compared with younger pa- responders were homozygous [5, 63, 64].
tients [28, 29, 38]. Infants and children under 10 years of Mueller et al. [65] retrospectively studied 63 eyes of 55
age may have a marked IOP response although not all patients who received posterior sub-Tenon corticosteroid
studies agree [57, 58]. A study by Lam et al. [59] on chil- injections (80 mg methylprednisolone acetate, or 40 mg
dren who had had strabismus surgery showed that 71.2 triamcinolone acetonide). All patients had been treated
and 59.2% of children receiving topical 0.1% dexametha- previously with topical or systemic corticosteroids and
sone (4 times per day and 2 times per day, respectively) did not experience an excessive increase in IOP. Some pa-
developed IOP elevations greater than 21 mm Hg. In chil- tients had received multiple injections, and in none of
dren who received dexamethasone 0.1% drops 4 times them was IOP elevation detected. The nonresponders
per day, the peak IOP was greater, the net increase in IOP seemed to be immune to high doses of steroids in the long
was greater, and the time required to reach the peak IOP run. However, Schwartz et al. [66] found no significant
was less. difference in the frequency of steroid-induced IOP eleva-
In an observational case series by Yamashita et al. [60] tion between monozygotic and dizygotic twin groups.
of 5 children with leukemia aged less than 6 years, the This may suggest that an environmental factor may influ-
patients received systemic steroids with their systemic ence the steroid response.
chemotherapy. An IOP rise greater than 21 mm Hg was Several genes have been shown to be upregulated in
observed in all patients. IOP increased to a mean maxi- dexamethasone-treated trabecular meshwork cells, and
mum of 39.6 8 7.2 mm Hg (range: 2847). All patients the most extensively studied represents the protein myo-
achieved controlled IOP with antiglaucoma medications. cilin [6769]. Mutations of the myocilin gene are one
One of the patients had glaucomatous optic neuropathy cause of autosomal dominant juvenile- and adult-onset
on the first exam. In their study on children below 10 POAG, but the mechanism by which mutant myocilins
years, Kwok et al. [61] concluded that the ocular hyper- cause disease is poorly understood [70]. In animal stud-
tensive response to topical dexamethasone in children ies, the investigators could not find statistically signifi-
179.7.82.148 - 2/7/2017 1:18:14 AM
68 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
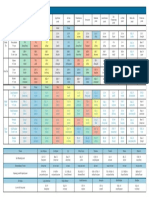
cant evidence of a link between myocilin gene mutations Table 1. Anti-inflammatory and IOP elevations for different top-
or myocilin overexpression and steroid-induced IOP el- ical steroid preparations
evation [7173]. Further studies are necessary to enhance Corticosteroid preparation Rise in IOP Anti-inflamma-
our understanding of the role of genetics in steroid-in- (mm Hg) tory potency
duced iatrogenic glaucoma.
Dexamathasone 0.1% 2282.9 24
Connective Tissue Disease and Sex Prednisolone 1.0% 1081.7 2.3
Fluorometholone 0.1% 6.181.4 21
In a study of 34 patients with connective tissue disease, Hydrocortisone 0.5% 3.281.0 1
mainly rheumatoid arthritis, who used 0.1% dexametha- Tetrahydrotriamcinolone 0.25% 1.881.3 1.4
sone drops in one eye for 6 weeks, Gaston et al. [45] re- Medrysone 1.0% 1.081.3 1.7
ported a higher incidence of positive steroid response
than would be expected in a normal population. Addi-
tionally, most of the male patients were responders. Five
patients (15% of the total) were high responders (a rise in
IOP to 32 mm Hg or more). They were all male. Seven no problem following a short course, the susceptible
patients (20%) were intermediate responders (IOP be- groups are at risk, especially if prescriptions for the drugs
tween 25 and 31 mm Hg); 4 (57%) were male and 3 were may be refilled.
female. Twenty-two patients (65%) were nonresponders There is evidence that topical steroids are absorbed
(IOP 24 mm Hg or less); 2 (9%) were male and 20 were systemically. When one eye is treated with topical ste-
female. roids, the contralateral untreated eye may be affected by
Mixed results have been obtained regarding the effect the systemically absorbed steroid [75, 76]. The amount of
of sex on IOP elevation after IVTA injection. In a study steroid reaching the eye is probably less with systemic
of 147 patients, male sex [11] and in another study of 82 therapy than with topical application and it may explain
patients, female sex [16] were risk factors for IOP eleva- the higher frequency of IOP elevation with topical ste-
tion in patients who received 4 mg IVTA. More studies roids compared to systemic forms [77]. Fluoromethalone
are necessary to determine if sex can be regarded as a risk and medrysone are less potent topical corticosteroids, but
factor. they have also been shown to produce an elevated IOP
with much less risk. The risk of producing an elevated
High Myopia IOP with the new corticosteroids rimexolone and lote-
Although it has been demonstrated that patients with prednol is comparable to fluorometholone (table1) [78].
high myopia have a greater risk of increased steroid re- Difluprednate, a difluorinated prednisolone derivative,
sponse [47, 49], in a prospective, noncomparative study of penetrates the corneal epithelium rapidly and effectively.
60 patients who received 4 mg IVTA, Park et al. [21] found Difluprednate does not use benzalkonium chloride as a
that high myopia had no correlation with IOP elevation. preservative, but is preserved with sorbic acid, which has
been shown to cause little irritation or damage to ocu-
lar tissue and is recommended for sensitive eyes [79].
Mode of Administration In a multicenter, randomized, double-masked, parallel-
group, placebo-controlled trial on 438 patients with uni-
Topical Steroids lateral ocular surgery, 111 received difluprednate 2 times
In most cases, corticosteroid glaucoma or ocular hy- a day, 107 received difluprednate 4 times a day, and 220
pertension are caused by drops or ointments instilled in received a placebo 2 or 4 times a day. A clinically signifi-
the eye. In a series with 34 cases of steroid-induced iatro- cant IOP rise (defined as 610 mm Hg from baseline and
genic glaucoma, topical steroid use was the most frequent 621 mm Hg overall) was observed in 3 patients (3%) in
(73.5%) mode of administration [74]. Tragically, many both difluprednate groups and 2 patients (1%) in the pla-
cases of steroid-induced glaucoma are produced by treat- cebo group [80]. Elevated IOP was effectively controlled
ment for trivial conditions such as contact lens discom- with topical medication. In another randomized trial on
fort or red eye. Because of the widespread availability and 182 patients, 3 subjects (3.7%) in the difluprednate group
effectiveness of combination steroid-antibiotic eyedrops, had a clinically significant IOP rise (610 mm Hg from
the general medical community routinely prescribes baseline and 621 mm Hg overall) compared to the pla-
these drops for red eye. Although the majority develops cebo group [81].
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 69
Downloaded by:
Table 2. Frequency of different IOP in individuals treated with systemic steroid
Authors Patients Mean Sex Mean steroid Mean duration Patients (%)
(number) age dosage of treatment
(years) (mg/kg) (years) IOP <20 IOP 2031 IOP >31
mm Hg mm Hg mm Hg
Lee [86] 13 57 7 female 18 4.4 (16) 54 46 0
6 male
Bernstein and Schwartz [27] 48 50 35 female 16 3.5 (0.211) 76 24 0
13 male
Hovland and Ellis [85] 26 26 10 female 24 1.252.5 69 29 2
16 male
Figures in parentheses are ranges.
Long-term steroid creams, lotions and ointments ap- mg/kg/day), was significantly higher than the pretreat-
plied to the face, eyelids, or at distant sites may raise the ment IOP at week 0 (average: 19.7 vs. 16.4 mm Hg, respec-
IOP, as so may systemically administered corticosteroids tively, p ! 0.0001), and when the infants were receiving
[27, 34, 46, 8284]. the minimum dose of dexamethasone (0.15 mg/kg/day)
at week 3 (19.7 vs. 15.8 mm Hg, p ! 0.0001), and also 5
Systemic Steroids weeks after discontinuance of dexamethasone (19.7 vs.
Although glaucoma is also observed in Cushings syn- 16.0 mm Hg, p ! 0.0001).
drome with the production of excess endogenous ste-
roids, the likelihood of IOP elevation with systemic ste- Steroid Inhalers
roids is less than the topical route. Generally, groups of A large cross-sectional, population-based study found
patients being treated with long-term systemic steroids that the use of inhaled steroids was associated with an
showed higher mean IOPs, as well as an increased num- increased risk of IOP elevation only in subjects reporting
ber of individuals with higher pressures than are present a first-degree relative with a family history of glaucoma
in the normal population (table2) [27, 85, 86]. This has [92]. In another study by Bui et al. [93], a significant re-
been confirmed by comparing steroid-treated patients to duction in IOP was observed after discontinuing nasal
the normal population with no steroid treatment or to a steroids in patients with glaucoma. Studies on the non-
group of patients with a similar disease but without ste- glaucomatous patients have not revealed IOP elevation
roid treatment [27, 87]. With systemic steroids, there was after using various forms of steroid inhalers [94, 95]. As
evidence for both an increase in flow, especially upon the administered dose of steroid is not high with inhalers,
short-term administration, and a decrease in the facility it is logical that we see an increase in the IOP only in sus-
of outflow [77, 88]. In patients who are steroid responders, ceptible patients.
pressure elevations with systemic steroid use average ap-
proximately 60% of those produced by topically applied Intravitreal Steroids
steroids [89]. One study found a 10% incidence of ocular Intravitreal corticosteroids are a recent therapeutic
hypertension in renal-transplant patients receiving ste- modality that are being used increasingly to treat various
roids [90]. Tripathi et al. [33] found a significant relation- edematous and neovascular intraocular conditions. Tri-
ship between IOP and the dose of corticosteroid (1.4 mm amcinolone acetonide is the most commonly used intra-
Hg increase in mean IOP for each 10 mg increase in the vitreal steroid. The usual dose is 4 or 20 mg (the latter is
average daily dose of prednisone) administered. more commonly used in Europe). Recently, Chuang et al.
Ng et al. [91] reported the use of a dose-tapering [96] reported that the incidence of secondary ocular hy-
regimen of dexamethasone was associated with a tran- pertension was not significantly different between 2 ver-
sient increase in IOP in preterm very low birth-weight sus 4 mg IVTA (38.9 vs. 50%, p = 0.36). However, patients
(!1,500 g) infants. The IOP at week 1, while the infants who received 4 mg had a higher proportion of long-term
were receiving the maximum dose of dexamethasone (0.6 antiglaucoma medication usage (5.6 vs. 40.6%, p ! 0.001).
179.7.82.148 - 2/7/2017 1:18:14 AM
70 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
Table 3. Studies on IOP elevation after IVTA injection
Authors Patients Definition of Average Prevalence of Risk factors Dose No response
and eyes IOP follow-up IOP elevation of to medical
(numbers) elevation (months) IVTA therapy and
underwent
surgery
Roth et al. [13] 929 eyes of >21 mm Hg 14 24% in 12 months, glaucoma 4 mg 1%
841 patients 28% in 24 months young age (10-year increase
in age was associated with a
16% reduction in risk)
IOP elevation after first
IVTA injection
Lau et al. [11] 147 eyes >6 mm Hg increase in 2.5 43.5% male sex 4 mg 6.8%
baseline IOP young age <55 years
Vasconcelos-Santos 150 eyes >21 mm Hg 7.7 32% glaucoma 4 mg
et al. [25] baseline IOP >16 mm Hg
Im et al. [15] 14 eyes >24 mm Hg 1 43% 4 mg none
Yamamato 82 eyes of >5 mm Hg increase in 6 34.1% female sex 4 mg 2.4%
et al. [16] 69 patients baseline IOP age <60 years
Baath et al. [17] 233 eyes of 9.5 31.3% needed medical 4 mg 1%
192 patients therapy
Kramar et al. [18] 85 eyes 4 59 mm Hg in 32% 4 mg none
10 mm Hg in 30%
Gregori et al. [19] 40 eyes 10 mm Hg 12 24% 5%
Konstantopoulos 114 eyes of >28 mm Hg 30% 4 mg 1%
et al. [20] 108 patients
Rhee et al. [12] 570 eyes of >30% increase in 12 50 and 65% that received baseline IOP >16 mm Hg 4 mg 1%
536 patients baseline IOP second injection second IVTA injection
Park et al. [21] 60 eyes >21 or 5 mm Hg 6.1 43.3% age <60 years 4 mg 1%
increase in baseline IOP
Smithen et al. [22] 89 eyes >24 mm Hg 100 days 40% baseline IOP >15 mm Hg 4 mg none
Bakri et al. [23] 43 eyes of >5 and >10 mm Hg 3 49 and 28% 4 mg none
38 patients increase in baseline IOP
Jonas et al. [24] 305 eyes of >21 mm Hg 41.2% younger age 20 mg 1%
272 patients
IVTA limits the impact of corticosteroids to ocular tis- treatment, the IVTA has been reported to be present in-
sues, thereby minimizing the side effects associated with traocularly in measurable concentrations up to 1.5 years
systemic steroid therapy. Additionally, the issues of drug after intravitreal injection [100].
penetration and bioavailability are eliminated. The re- In order to predict the possibility of a post-IVTA IOP
ported frequency of IOP elevation varies from 20 to 65% rise, Breusegem et al. [101] conducted a topical dexameth-
(table 3) [22]. This wide range of values might be ex- asone provocative test (4 drops a day for 4 weeks) before
plained by the IVTA dose, variation between definitions IVTA injection. A steroid response after the dexametha-
of IOP elevation, length of follow-up, sample size, and sone test or after IVTA was defined as an IOP increase of
whether patients have previously received IVTA injec- 66 mm Hg. In dexamethasone responders, the IOP eleva-
tions or not. Several reports have suggested the higher tion after IVTA was 17.0 8 7.8 versus 5.0 8 4.4 mm Hg
frequency of IOP elevation in younger patients, higher in dexamethasone nonresponders (p = 0.005). This test
baseline IOP, intravitreal injection compared to sub-Ten- had a low sensitivity, a high specificity, a high positive pre-
on injection and increased triamcinolone acetonide dos- dictive value and a moderate negative predictive value. In-
age [21, 9799]. Although IOP elevation commonly oc- terestingly, all test responders demonstrated high IOP in-
curs as early as 1 day to as late as 12 weeks after the initial creases after intraocular repository-steroid injection.
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 71
Downloaded by:
The highest IOP elevation within the first 24 h after In two identical, multicenter, masked, randomized,
IVTA injection occurs within 10 min, and to combat this 6-month, sham-controlled clinical trials on patients with
rise, some perform anterior chamber paracentesis [102, central or branch retinal-vein occlusion, a total of 1,267
103]. However, one anterior chamber paracentesis for patients received intravitreal dexamethasone implants
treating an IOP spike after IVTA precipitated an episode [105]. The percentage of dexamethasone implant-treated
of malignant glaucoma [104]. eyes with an IOP of 625 mm Hg peaked at 16% at month
In a meta-analysis, it was shown that there was a ten- 2 but was not different from sham by month 6. Studies
dency toward a higher increase in IOP in patients with with longer follow-up periods are necessary to determine
uveitis and patients with central retinal vein occlusion the effect of this implant on the IOP.
[24].
Intravitreal Sustained-Release Steroid Implants Mechanism
Intravitreal steroid implants are designed for control-
ling intraocular inflammation due to noninfectious pos- Trabecular meshwork accounts for nearly 90% of
terior-segment uveitis or macular edema due to vascular aqueous humor drainage from the eye. Although the pro-
accidents [105, 106]. Through three trials of the fluocino- posed mechanism of corticosteroid-induced IOP eleva-
lone acetonide implantation, a total of 584 eyes received tion is increased resistance to aqueous flow via this route,
a single implant at one of two dosages: 0.59 or 2.1 mg. At the precise mechanism is still unknown [110]. Krishnan
1 year, the IOP was elevated to above 30 mm Hg in 36.9 et al. [111] obtained complete success with viscocanalos-
and 40.7% of eyes treated with the 0.59-mg and 2.1-mg tomy in lowering IOP and because the stripping of the
implants, respectively. At 2 and 3 years, these values were juxtacanalicular tissue and the inner endothelial lining
46.4 and 55.2% and 51.2 and 59.0%, respectively [106 of Schlemms canal relieved the steroid-induced resis-
109]. The incidence of elevated IOP with the fluocinolone tance to aqueous outflow, the obstruction to aqueous out-
acetonide implant has been higher than that with IVTA flow in steroid-induced glaucoma seems to lie predomi-
injections [106]. One explanation for this may be expo- nantly in the juxtacanalicular tissue and the endothelium
sure to sustained corticosteroid levels throughout the im- of Schlemms canal. Based on the histopathologic study
plants 30-month lifespan, whereas the eyes treated with of 2 patients who had trabeculectomy because of uncon-
IVTA injections are exposed to fluctuating corticosteroid trolled IOP after IVTA, the ultrastructural changes in the
levels every 3 months. trabecular meshwork resembled those with glaucoma af-
Overall, 75% of eyes receiving the fluocinolone ace- ter topical corticosteroid treatment [112]. There are a
tonide implant required IOP-lowering therapy at some number of observations that can be summarized as fol-
point within the course of the 3-year study. More than lows.
one third of the eyes (36.6%) required IOP-lowering sur-
gery. The most common surgery employed was trabecu- Trabecular Meshwork Extracellular Matrix
lectomy (76.2%) and 20.6% received glaucoma drainage The effect of steroids on the trabecular meshwork ex-
devices as first-line treatment. Other employed surgical tracellular matrix may be due to altered rates of protein
therapies included cyclodestructive procedures and non- synthesis, or to protein degradation, or a combination of
penetrating glaucoma surgeries [107]. both. This results in increased deposition of glycosami-
A major complication of surgical intervention for high noglycan, elastin, fibronectin, laminin, and type IV col-
IOP in these patients was the high prevalence of hypoto- lagen as part of the extracellular matrix secondary to in-
ny (42.5%) that was defined as IOP ! 5. The prevalence of creased production and decreased destruction because of
hypotony in eyes that received the implant but did not inhibition of several trabecular meshwork matrix metal-
require IOP-lowering surgery was 35.4%. Therefore, it is loproteinases [8183]. Additionally, dexamethasone is
likely that eyes receiving the fluocinolone acetonide im- known to inhibit the phagocytic abilities of trabecular
plant were predisposed to low IOP independent of IOP- meshwork cells so that debris accumulates within the
lowering filtrating surgery [107]. In the study by Callanan drainage channels [113].
et al. [106], the frequency of IOP-lowering surgery began
to increase by postimplantation week 12 for implanted Gene Expression
eyes and month 27 for fellow eyes. Myocilin was the first glaucoma gene (GLC1A) to be
mapped and identified and was a glaucoma candidate
179.7.82.148 - 2/7/2017 1:18:14 AM
72 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
gene because of its expression in the trabecular mesh- tivities may lead to the decreased proliferation, migration
work and its induction by steroids [114116]. The myo- and phagocytosis of the trabecular meshwork cells [76,
cilin gene product, known as myocilin or trabecular 80]. All these cause the diminished cellularity of the tra-
meshwork-inducible glucocorticoid response (TIGR) becular meshwork seen in patients with steroid-induced
protein, is distributed intracellularly as well as in the ex- glaucoma and the progressive accumulation of extracel-
tracellular matrix of the normal and glaucomatous tra- lular debris and increased aqueous outflow resistance.
becular meshwork [117]. Myocilin gene mutations are re-
sponsible for juvenile open-angle glaucoma and 35% of
cases of POAG [118, 119]. Mutations of this gene appear Clinical Picture and Differential Diagnosis
to produce a dysfunctional secretion of the translated
protein in trabecular meshwork cells, leading to de- Steroid-induced glaucoma can occur with any form of
creased aqueous outflow [120]. A more than 100-fold in- steroid administration. Patients with steroid-induced
crease in myocilin gene expression has been reported af- glaucoma have relatively few symptoms. These patients
ter exposure to dexamethasone [121]. However, a recent do not complain until they notice visual disturbances:
study of human trabecular meshwork cells that were cul- blurred vision or signs of visual-field defect. Glaucoma
tured in the presence of ophthalmic steroids did not may be discovered by chance during an ophthalmological
show that myocilin gene overexpression is associated checkup. If the IOP is not measured at the initial stages
with an increase in IOP [122]. More studies are needed when there are no glaucomatous optic nerve head find-
to explain the variations in the myocilin gene and their ings, misdiagnosis is not unusual. The blurred vision is
role in steroid-induced glaucoma. caused by corneal edema if the IOP has risen to the point
of compromising corneal function and may be associated
Trabecular Meshwork Cells with halo. It may even be due to a posterior subcapsular
Trabecular meshwork cells have glucocorticoid recep- cataract. The IOP rise is generally gradual and painless,
tors, and the activation of these receptors by steroids al- but a few patients may experience ocular or brow ache
ters the structure and protein expression of trabecular [26, 128].
meshwork cells [79]. Steroids have been shown to alter The typical manifestation of steroid induced-glauco-
trabecular meshwork cell morphology by causing an in- ma in adults is similar to POAG. Even in patients with
crease in nuclear size and DNA content [113, 123]. high IOP, the eyes are remarkably white. However, some
In a study of the effects of steroids on junctional pro- patients may present with a pale disk, often not typically
tein expression and cytoskeleton organization in primary excavated at the onset, and the uncharacteristically dete-
human trabecular meshwork cultures, it was shown that riorated visual field resembling the findings after an
dexamethasone increased the protein levels of zonula oc- acute angle-closure attack. This picture develops when
cludens-1 and connexin 43 in trabecular meshwork cells, the IOP reaches high values rapidly. Elderly patients who
which are thought to be closely related to fluid flow resis- received corticosteroid treatment in the past may present
tance. Dexamethasone also altered the F-actin architec- as cases of normal-tension glaucoma. They have experi-
ture and promoted cross-linked actin network formation enced IOP elevation and glaucomatous optic-nerve dam-
[124]. F-actin interacts with zonula occludens-1 to help age while being on steroids and, years later, present off
intercellular tight junction assembly, in which the tight- steroid with normal IOP and glaucomatous optic neu-
ness and distribution of the tight junctions influence the ropathy. Because these eyes are generally asymptomatic,
outflow rate of aqueous humor. F-actin is also organized diagnosis relies on appropriate recognition and monitor-
to respond to cell contraction and to participate in gener- ing of patients at risk [129].
ating forces responsible for the continued development Of the reported complications of steroids that may ac-
and maintenance of tension. It has been shown that dexa- company steroid-induced glaucoma are mydriasis and
methasone induces F-actin expression and enhances the ptosis. In cases with unilateral steroid-induced glaucoma,
mediated contraction of trabecular meshwork cells [125, mydriasis and ptosis may be striking; otherwise, as they
126]. Contraction of the trabecular meshwork reduces are not severe, they may not be evident [130].
the intercellular spaces and thus reduces the outflow of In a pediatric series reported by Yamashita et al. [60],
aqueous humor [127]. no patient had symptoms, even the one who had an IOP
Changes in the microstructure of the trabecular mesh- of 47 mm Hg. The clinical picture in infants with steroid-
work (cross-linked actin network formation) and cell ac- induced glaucoma resembles congenital glaucoma [57].
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 73
Downloaded by:
Management If the drug should be continued, it must be used in a
lower concentration or replaced by weaker corticoste-
The most effective treatment for corticosteroid-in- roids, or antiglaucoma agents should be commenced to
duced glaucoma is its prevention through judicious use control the high IOP. In the case of topical steroids,
of steroids. In this regard, education of the patient and loteprednol can be a suitable alternative since it undergoes
physician about the potential ocular complications of ste- hydrolysis in the cornea and aqueous humor to become an
roids is necessary. Failure of IOP elevation after 6 weeks inactive derivative and thus may not have a marked effect
of therapy is no assurance that an individual will not de- on the IOP [133]. Rimexolone 1% is a topical steroid de-
velop an increase in IOP if steroid administration is con- signed so as not to elevate IOP, but IOP increase has been
tinued. For this reason, patients who are on steroids, reported, even though it is rare [32]. Systemic steroids can
specially the topical form, should have regular follow-up be replaced by steroid-sparing agents such as systemic
examinations to prevent iatrogenic glaucomatous optic- nonsteroidal anti-inflammatory agents [134].
nerve damage [33].
Medical Management
IOP Monitoring It may not be possible to discontinue the steroid, and
Recognition of the condition is the most important the elevated IOP should be managed medically or surgi-
step in its management. When patients are put on ste- cally. The medical management of these cases is essen-
roids, particularly with potent topical steroids and peri- tially the same as for POAG. Nearly all patients who de-
ocular injections, the physicians should monitor them velop steroid-induced iatrogenic glaucoma can be con-
thoroughly. This includes baseline IOP measurement, trolled with topical antiglaucoma therapy [18, 31]. Sihota
mostly to rule out preexisting glaucoma. IOP monitoring et al. [74] reported that in 25 of 34 patients (73.5%), IOP
should initially occur at 2 weeks and then every 46 could be controlled by topical medications alone. At 6, 12,
weeks for 23 months, and then every 6 months after an and 18 months follow-up, 22 (64.7%), 33 (97.1%), and all
initial response has been ruled out. In the case of IVTA 34 (100%) patients were off treatment, respectively. In a
injection, in addition to the above-mentioned measure- study by Gillies et al. [95], of 75 patients who received
ments, IOP should be checked on the injection day and 4 mg IVTA, it was shown that with the criterion of treat-
first week [129]. ing any IOP above 25 mm Hg, 21 (28.0%) required treat-
ment with topical glaucoma therapy. A single medication
Discontinuance of Steroids was sufficient in 18 (85.7%) patients, whereas the other 3
The steroid-induced IOP increase is usually short-lived (14.3%) required 2 medications to control IOP. Topical
and reversible by discontinuance of therapy if the drug glaucoma treatment was discontinued in 52.4% at the
has not been used for more than a year. It is likely to result 6-month follow-up and in 71.4% after a mean period of 8
in permanent IOP elevation if steroid therapy has been months (range: 1.532 months). Eight percent of eyes that
continued for 18 months or more [32]. The IOP usually did not receive glaucoma medication before IVTA con-
returns to normal within 24 weeks after discontinuing tinued to require glaucoma medication at the last study
the steroid [131]. In cases with repository-steroid injection visit (3-year study duration).
and high IOP, the residual subconjuctival or intraocular Another study revealed that the patient who was man-
steroid may be removed [28, 8688]. In the two cases with aged with topical glaucoma medications for elevated IOP
very high IOP described by Agrawal et al. [132], the re- after IVTA injection no longer needed antiglaucoma
moval of the intravitreal corticosteroid by vitrectomy re- agents about 6 months after the injection [135]. Overall, as
versed the elevated IOP. However, the potential surgical the ocular hypertensive effect of repository steroids de-
complications of vitrectomy, including rhegmatogenous creases, the majority of patients need to receive antiglau-
retinal detachment, proliferative vitreoretinopathy, and coma medications for just 6 months after steroid injection.
induction of cataract, have to be considered against the All available antiglaucoma medications can be used in
risk-benefit profile of other treatment modalities, such as these patients, beginning with aqueous humor suppres-
laser trabeculoplasty and trabeculectomy or shunt sur- sants. These include -blockers, followed by either 2 ag-
gery. However, some reports document continued IOP el- onists or topical carbonic anhydrase inhibitors.
evation, even long after withdrawal of the steroid [21, 89]. Topical -blockers are a popular first-line agent for
Additionally, the removal of the repository steroid will treating this type of glaucoma and are categorized as
also result in a reduction in the drugs desired effect. well-tolerated drugs in patients with uveitis [136].
179.7.82.148 - 2/7/2017 1:18:14 AM
74 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
The 2 agonist brimobidine is an often effective drug after laser trabeculoplasty in patients who have intraocu-
for treating steroid-induced iatrogenic glaucoma and can lar steroids could also be due to the waning of the steroid
be used in patients with intraocular inflammation [129]. effect, this procedure can reduce IOP until the steroid-
Carbonic anhydrase inhibitors are also regarded as ef- induced hypertensive effect disappears [141, 143]. Laser
fective agents in this condition. Acetazolamide is fre- trabeculoplasty may be considered as a primary option
quently used for the short-term control of high IOP, and for steroid-induced ocular hypertension when consider-
the topical forms can be used for a more prolonged peri- ing the ocular and systemic adverse effects of antiglau-
od. They are also regarded as potent and effective agents coma agents.
in controlling IOP in patients with uveitis [136].
Prostaglandin analogues have been reported to induce Surgical Management
uveitis and are relatively contraindicated in patients who If the patients IOP is very high or remains elevated for
have developed high IOP after using steroids to control a significant period of time, surgical intervention should
ocular inflammation [137]. However, this agent, as well be considered. Although most patients with steroid-in-
as miotics, may be effective, particularly as an additive duced elevated IOP can be treated systemically or topi-
agent. Although prostaglandin analogues may not be the cally, about 15% with intractable glaucoma must still
first choice, they can be helpful in some situations in undergo surgery to normalize their IOP [15, 97]. Also, if
which further IOP lowering is required. the patient is expected to have repeated exposure to ste-
roids, surgery may be the best solution so steroids can
Laser Trabeculoplasty then be used more freely. However, Muecke and Brian
Rubin et al. [138] reported 7 patients who underwent [144] reported a case with several episodes of steroid-in-
selective laser trabeculoplasty (SLT) for increased IOP af- duced ocular hypertension (above 50 mm Hg) when
ter IVTA. The mean preoperative IOP of 38.4 8 7.3 with challenged with topical steroid on two occasions despite
4 medications decreased postoperatively to 23.9 at 3 having a functional Molteno shunt and having received
months (p ! 0.006) with 3.9 medications, and 15.7 at 6 maximal hypotensive medication after each steroid chal-
months (p ! 0.001) with 2.4 medications. Four patients lenge. Moreover, in a prospective study of 87 eyes of 52
had a second SLT procedure. Two patients failed after the patients with POAG, a significant steroid-induced rise in
third-month visit: one had pars plana vitrectomy and IOP in the 4 weeks after trabeculectomy was observed in
lensectomy and the other underwent Ahmed valve im- 23% of eyes [145]. The patients who need to receive ste-
plantation. roids in any form after glaucoma surgery for steroid-in-
In another study, SLT was performed on 4 patients un- duced iatrogenic glaucoma need to be monitored regu-
der 47 years with elevated IOP after a sub-Tenon injection larly.
of triamcinolone acetonide which could not be main- In a series, 9 out of 34 patients with steroid-induced
tained within normal limits by antiglaucoma medica- iatrogenic glaucoma (26.5%) required surgery. The mean
tions. In 3 eyes, the mean IOP before the SLT was 28.7 baseline IOP in the eyes requiring surgery was 49.67 8
mm Hg and the postoperative mean IOP was 15.3 mm Hg 13.28 mm Hg, and in the eyes managed medically 30.36
at 6 months without antiglaucoma medications. In 1 pa- 8 7.51 mm Hg (p = 0.002). In addition, patients ^20
tient, the IOP increased to 40 mm Hg at 4 weeks after SLT, years old with greater glaucomatous optic neuropathy
and the patient underwent trabeculotomy [139]. were more likely to need surgery [74].
Five patients who received argon laser trabeculoplasty The most commonly employed surgery in patients
for increased IOP after IVTA achieved normal IOP with- with virgin conjunctiva is trabeculectomy; otherwise,
in the first postoperative month [140, 141]. The advan- shunt implantation or cyclodestructive procedures may
tages of laser trabeculoplasty are numerous when consid- be preferred. Repository-steroid removal (excision in the
ering the possible hazards of trabeculectomy, including case of sub-Tenon deposits and vitrectomy in the IVTA)
anesthesia, hypotony, cataract, and endophthalmitis. It is and a glaucoma procedure can be performed in one ses-
also a time-efficient and cost-effective procedure when sion when the IOP drop does not seem to be controlled by
compared with filtering surgery [141, 142]. Another ad- steroid removal [146].
vantage of this procedure, in contrast to filtering proce-
dures that increase the turnover and wean off the effect Vitrectomy
of steroids, is keeping the intraocular steroid so that its Agrawal et al. [132] reported the successful outcome
therapeutic effect does not cease. Although the IOP drop of vitrectomy in 2 patients that had an IOP of 70 after
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 75
Downloaded by:
IVTA. The IOP returned to below 21 within the first Future Therapies
postoperative week with no antiglaucoma medications.
However, pars plana vitrectomy is a more invasive inter- Anecortave acetate is an analog of cortisol acetate that
vention than trabeculectomy or shunt surgery, and the lacks the typical anti-inflammatory and immunosup-
therapeutic effect of steroids stops. In addition, up to 3% pressive properties of glucocorticoids. Anecortave ace-
of steroid responders may have irreversible elevations of tate functions as an antiangiogenic agent, inhibiting
IOP [26]. blood vessel growth by decreasing extracellular protease
expression and inhibiting endothelial cell migration. Its
Filtering Procedures angiostatic activity does not seem to be mediated through
In a case series of 3 eyes of 3 patients with elevated IOP any of the commonly known pharmacological receptors
after IVTA, trabeculectomy augmented with 5-fluouracil [150152]. In a case series, a total of 8 eyes of 7 subjects
controlled the IOP to less than 18 mm Hg without anti- with medically uncontrolled IOP following intravitreal
glaucoma medications, with a median follow-up of 9.5 or sub-Tenon injections of triamcinolone acetonide re-
months [147]. Krishnan et al. [111] reported a series of 3 ceived an anterior juxtascleral depot of 3% anecortave ac-
patients who developed refractory glaucoma secondary etate solution. To administer the drug in the juxtascleral
to IVTA and were successfully treated with viscocanalos- area after instilling topical anesthesia and inserting a lid
tomy. speculum, the patients were advised to look upward.
Then, using a 33-gauge needle on a tuberculin syringe,
Trabeculotomy 0.81.0 ml of a 30 mg/ml suspension (2430 mg) of ane-
Contrary to other types of adult glaucoma, trabecu- cortave was injected into the anterior sub-Tenon space in
lotomy has been reported to be effective in adult patients the inferior fornix approximately 4 mm from the limbus
with steroid-induced iatrogenic glaucoma [139, 148]. with the needle parallel to the limbus slowly over 12
Honjo et al. [148] studied 14 eyes in 7 patients with a his- min. The mean baseline IOP had reduced from 39.9 mm
tory of topical or systemic corticosteroid treatment before Hg by 34.5% (14.1 mm Hg, p = 0.003) at the 1-month fol-
the rise of IOP and underwent trabeculotomy as the first low-up. Four eyes required surgical intervention despite
surgical procedure. After an average follow-up of 60.6 8 a decrease in IOP because of a markedly elevated initial
33.5 months, the IOP in all of the 14 eyes was well con- IOP and the degree of preexisting glaucomatous optic
trolled below or equal to 21 mm Hg at the final examina- neuropathy. No adverse effects were observed [92].
tions. In a prospective interventional case series of 28 uncon-
trolled glaucoma (mainly uveitic/steroid-induced glauco-
Shunt Implantation ma), Prata et al. [153] showed that a single juxtascleral
Seven eyes of 5 patients underwent fluocinolone ace- depot injection of anecortave acetate (2430 mg) resulted
tonide implantation and Ahmed valve placement in a sin- in a significant IOP reduction for at least 3 months in 11
gle surgical session. The average IOP decreased from 27.3 patients (39.2%). This series also sustained no complica-
mm Hg at baseline to 14.6 mm Hg 12 months after the tion. The mechanism underlying this anecortave effect is
combined surgery (p = 0.01). One eye did not maintain unclear [9294], but these studies provide a basis and
target IOP and underwent the placement of a second model not only for studying the mechanism of steroid-
glaucoma tube shunt 4.4 months after the initial surgery, induced glaucoma but also of POAG and evaluating po-
with subsequent appropriate IOP control [149]. tential therapies.
Eyes with active inflammation or conjunctival scar-
ring from previous surgery will benefit particularly from
the use of a shunt implantation. Another consideration Conclusion
for implant selection is plate size. In eyes with fluocino-
lone acetonide implants, larger plate size may result in a The exact mechanism of steroid-induced glaucoma is
higher risk of hypotony. An implant with a smaller plate not yet known. The genetics are not fully understood.
size, such as the Ahmed implant, is probably less likely to Contrary to the postulation of simple Mendelian inheri-
cause chronic hypotony in patients with uveitis and ste- tance, steroid-induced glaucoma seems to be induced by
roid implants [106]. In patients with IVTA and high IOP, a number of gene locus interactions and environmental
Ahmed valve implantation has proven to be effective [39, factors. The responses of normal, suspect or glaucoma-
138]. tous patients to steroids differ. The lowest pressure eleva-
179.7.82.148 - 2/7/2017 1:18:14 AM
76 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
tion after steroid use has been observed in normal pa- surgery to normalize their IOP. Trabeculectomy, trabec-
tients, while the highest has been observed in patients ulotomy, shunt surgery, and cyclodestructive procedures
with glaucoma. Data from several studies indicate that are among the surgeries employed and can be combined
the response of IOP to steroids appears to be dependent with vitrectomy in patients who have IVTA to remove the
upon mean initial pressure. Susceptible patients should remainder of the steroid. Early results of anecortave ac-
be identified early enough and monitored closely to pre- etate, an angiostatic steroid, in controlling IOP have been
vent irreversible optic nerve damage. Discontinuance of promising. Further studies on the mechanism of steroid-
the steroid or resection of the remainder of the repository induced glaucoma, genetics, and the potential role of an-
steroid may be of benefit to the patient. The majority of ecortave acetate can improve our understanding of this
cases with steroid-induced iatrogenic glaucoma can be sight-threatening complication of steroids to advance
controlled successfully by topical glaucoma medications. their medical and surgical management.
The high incidence of elevated IOP is a significant
complication with intravitreal fluocinolone acetonide
implants but can be managed in most patients with IOP- Disclosure Statement
lowering eye drops or surgery. However, surgery is associ-
Neither author has any conflicts of interest associated with the
ated with a high frequency of postoperative hypotony.
work presented in this article.
About 15% of patients with steroid-induced iatrogen-
ic glaucoma do not respond to medical therapy and need
References
1 Woods AC: Clinical and experimental ob- 12 Rhee DJ, Peck RE, Belmont J, Martidis A, Liu 19 Gregori NZ, Rosenfeld PJ, Puliafito CA,
servation on the use of ACTH and cortisone M, Chang J, Fontanarosa J, Moster MR: In- Flynn HW Jr, Lee JE, Mavrofrides EC, Smid-
in ocular inflammatory disease. Trans Am traocular pressure alterations following in- dy WE, Murray TG, Berrocal AM, Scott IU,
Ophthalmol Soc 1950;48:259296. travitreal triamcinolone acetonide. Br J Gregori G: One-year safety and efficacy of
2 Covell LL: Glaucoma induced by systemic Ophthalmol 2006;90:9991003. intravitreal triamcinolone acetonide for the
steroid therapy. Am J Ophthalmol 1958; 45: 13 Roth DB, Verma V, Realini T, Prenner JL, management of macular edema secondary to
108109. Feuer WJ, Fechtner RD: Long-term inci- central retinal vein occlusion. Retina 2006;
3 Goldmann H: Cortisone glaucoma. Arch dence and timing of intraocular hyperten- 26:889895.
Ophthalmol 1962;68:621626. sion after intravitreal triamcinolone aceton- 20 Konstantopoulos A, Williams CP, Newsom
4 Armaly MF, Becker B: Intraocular pressure ide injection. Ophthalmology 2009;116:455 RS, Luff AJ: Ocular morbidity associated
response to topical corticosteroids. Fed Proc 460. with intravitreal triamcinolone acetonide.
1965;24:12741278. 14 Vasconcellos JP, Melo MB, Costa VP, Tsuku- Eye (Lond) 2007;21:317320.
5 Becker B: Intraocular pressure response to mo DM, Basseres DS, Bordin S, Saad ST, Cos- 21 Park HY, Yi K, Kim HK: Intraocular pres-
topical corticosteroids. Invest Ophthalmol ta FF: Novel mutation in the MYOC gene in sure elevation after intravitreal triamcino-
1965;4:198205. primary open glaucoma patients. J Med Gen- lone acetonide injection. Korean J Ophthal-
6 Urban RC Jr, Dreyer EB: Corticosteroid-in- et 2000;37:301303. mol 2005; 19:122127.
duced glaucoma. Int Ophthalmol Clin 1993; 15 Im L, Allingham RR, Singh I, Stinnett S, 22 Smithen LM, Ober MD, Maranan L, Spaide
33:135139. Fekrat S: A prospective study of early intra- RF: Intravitreal triamcinolone acetonide
7 Shaikh NM, Shaikh S, Singh K, Manche E: ocular pressure changes after a single intra- and intraocular pressure. Am J Ophthalmol
Progression to end-stage glaucoma after la- vitreal triamcinolone injection. J Glaucoma 2004;138:740743.
ser in situ keratomileusis. J Cataract Refract 2008;17:128132. 23 Bakri SJ, Beer PM: The effect of intravitre-
Surg 2002;28:356359. 16 Yamamoto Y, Komatsu T, Koura Y, Nishino al triamcinolone acetonide on intraocular
8 Morales J, Good D: Permanent glaucoma- K, Fukushima A, Ueno H: Intraocular pres- pressure. Ophthalmic Surg Lasers Imaging
tous visual loss after photorefractive keratec- sure elevation after intravitreal or posterior 2003;34:386390.
tomy. J Cataract Refract Surg 1998; 24: 715 sub-Tenon triamcinolone acetonide injec- 24 Jonas JB, Degenring RF, Kreissig I, Akkoyun
718. tion. Can J Ophthalmol 2008;43:4247. I, Kamppeter BA: Intraocular pressure eleva-
9 Samuelson TW: Refractive surgery in glau- 17 Baath J, Ells AL, Crichton A, Kherani A, Wil- tion after intravitreal triamcinolone aceton-
coma. Curr Opin Ophthalmol 2004; 15:112 liams RG: Safety profile of intravitreal triam- ide injection. Ophthalmology 2005;112:593
118. cinolone acetonide. J Ocul Pharmacol Ther 598.
10 Hamilton DR, Manche EE, Rich LF, Maloney 2007;23:304310. 25 Vasconcelos-Santos DV, Nehemy PG,
RK: Steroid-induced glaucoma after laser in 18 Kramar M, Vu L, Whitson JT, He YG: The Schachat AP, Nehemy MB: Secondary ocu-
situ keratomileusis associated with interface effect of intravitreal triamcinolone on intra- lar hypertension after intravitreal injec-
fluid. Ophthalmology 2002;109:659665. ocular pressure. Curr Med Res Opin 2007; tion of 4 mg of triamcinolone acetonide: in-
11 Lau LI, Chen KC, Lee FL, Chen SJ, Ko YC, Liu 23:12531258. cidence and risk factors. Retina 2008; 28:
CJ, Hsu WM: Intraocular pressure elevation 573580.
after intravitreal triamcinolone acetonide 26 Francois J: Corticosteroid glaucoma. Ann
injection in a Chinese population. Am J Ophthalmol 1977;9:10751080.
Ophthalmol 2008;146:573578.
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 77
Downloaded by:
27 Bernstein HN, Schwartz B: Effects of long- 43 Goldstein DA, Fiscella RG, Tessler HH: Bio- 60 Yamashita T, Kodama Y, Tanaka M, Yama-
term systemic steroids on ocular pressure chemical quantification of triamcinolone in kiri K, Kawano Y, Sakamoto T: Steroid-in-
and tonographic values. Arch Ophthalmol subconjunctival depots. Arch Ophthalmol duced glaucoma in children with acute lym-
1962;68:742753. 1996;114:363364. phoblastic leukemia: a possible complica-
28 Armaly MF: Effect of corticosteroids on in- 44 Davies TG: Tonographic survey of the close tion. J Glaucoma 2010;19:188190.
traocular pressure and fluid dynamics. I. relatives of patients with chronic simple 61 Kwok AK, Lam DS, Ng JS, Fan DS, Chew SJ,
The effect of dexamethasone in the normal glaucoma. Br J Ophthalmol 1968;52:3239. Tso MO: Ocular-hypertensive response to
eye. Arch Ophthalmol 1963;70:482491. 45 Gaston H, Absolon MJ, Thurtle OA, Sattar topical steroids in children. Ophthalmology
29 Armaly MF: Effect of corticosteroids on in- MA: Steroid responsiveness in connective 1997;104:21122116.
traocular pressure and fluid dynamics. Il. tissue diseases. Br J Ophthalmol 1983; 67: 62 Becker B, Bresnick G, Chevrette L, Kolker AE,
The effect of dexamethasone in the glauco- 487490. Oaks MC, Cibis A: Intraocular pressure and
matous eye. Arch Ophthalmol 1963;70:492 46 Spaeth GL, Rodrigues MM, Weinreb S: Ste- its response to topical corticosteroids in dia-
499. roid-induced glaucoma: A. Persistent eleva- betes. Arch Ophthalmol 1966;76:477483.
30 Becker B, Mills DW: Corticosteroids and in- tion of intraocular pressure. B. Histopatho- 63 Armaly MF: Statistical attributes of steroid
traocular pressure. Arch Ophthalmol 1963; logical aspects. Trans Am Ophthalmol Soc hypertensive response in the clinically nor-
70:500507. 1977;75:353381. mal eye. I. The demonstration of three levels
31 Carnahan MC, Goldstein DA: Ocular com- 47 Podos SM, Becker B, Morton WR: High my- of response. Invest Ophthalmol 1965; 4: 187
plications of topical, peri-ocular, and sys- opia and primary open-angle glaucoma. Am 197.
temic corticosteroids. Curr Opin Ophthal- J Ophthalmol 1966;62:10381043. 64 Becker B, Hahn KA: Topical corticosteroids
mol 2000; 11:478483. 48 Becker B: Diabetes mellitus and primary and heredity in primary open-angle glauco-
32 American Academy of Ophthalmology: Ba- open-angle glaucoma. The XXVII Edward ma. Am J Ophthalmol 1964;57:543551.
sic and Clinical Science Course, Section 2: Jackson Memorial Lecture. Am J Ophthal- 65 Mueller AJ, Jian G, Banker AS, Rahhal FM,
Fundamentals and Principles of Ophthal- mol 1971; 71:116. Capparelli E, Freeman WR: The effect of
mology. San Francisco, American Academy 49 Spaeth GL: Traumatic hyphema, angle re- deep posterior subTenon injection of corti-
of Ophthalmology, 2008, p 419. cession, dexamethasone hypertension, and costeroids on intraocular pressure. Am J
33 Tripathi RC, Kirschner BS, Kipp M, Tripathi glaucoma. Arch Ophthalmol 1967; 78: 714 Ophthalmol 1998;125:158163.
BJ, Slotwiner D, Borisuth NS, Karrison T, Er- 721. 66 Schwartz JT, Reuling FH, Feinleib M, Gar-
nest JT: Corticosteroid treatment for inflam- 50 Becker B, Mills DW: Corticosteroid and in- rison RJ, Collie DJ: Twin study on ocular
matory bowel disease in pediatric patients traocular pressure. Arch Ophthalmol 1963; pressure following topically applied dexa-
increases intraocular pressure. Gastroenter- 70:500507. methasone. Il. Inheritance of variation in
ology 1992;102:19571961. 51 Becker B, Mills DW: Elevated intraocular pressure response. Arch Ophthalmol 1973;
34 Herschler J: Intractable intraocular hyper- pressure following corticosteroid eye drops. 90:281286.
tension induced by repository triamcinolone JAMA 1963;185:884886. 67 Alward WL: The genetics of open-angle
acetonide. Am J Ophthalmol 1972; 74: 501 52 Franois J, Heintz-De Bree C, Tripathi RC: glaucoma: The story of GLC1A and myo-
504. The cortisone test and heredity of early cilin. Eye (Lond) 2000;14:429436.
35 Helm CJ, Holland GN: The effects of poste- open-angle glaucoma (in French). Bull Soc 68 Polansky JR, Nguyen TD: The TIGR gene,
rior subTenon injection of triamcinolone Belge Ophtalmol 1965; 141:576581. pathogenic mechanisms, and other recent
acetonide in patients with intermediate uve- 53 Becker B: The effect of topical corticoste- advances in glaucoma genetics. Curr Opin
itis. Am J Ophthalmol 1995;120:5564. roids in secondary glaucoma. Arch Ophthal- Ophthalmol 1998;9:1523.
36 Kalina RE: Increased intraocular pressure mol 1964; 72: 769771. 69 Lo WR, Rowlette LL, Caballero M, Yang P,
following subconjunctival corticosteroid ad- 54 Reichle ML: Complications of intravitreal Hernandez MR, Borras T: Tissue differential
ministration. Arch Ophthalmol 1969; 81: steroid injections. Optometry 2005; 76: 450 microarray analysis of dexamethasone in-
788790. 460. duction reveals potential mechanisms of ste-
37 Hirooka K, Shiraga F, Tanaka S, Baba T, 55 Oliver A, Gao H, WuDunn D, Peracha MO, roid glaucoma. Invest Ophthalmol Vis Sci
Mandai H: Risk factors for elevated intraoc- Cantor LB: Intravitreal triamcinolone in- 2003;44:473485.
ular pressure after trans-Tenon retrobulbar jection in patients with surgically control- 70 Liu Y, Vollrath D: Reversal of mutant myo-
injections of triamcinolone. Jpn J Ophthal- led glaucoma. Arch Ophthalmol 2006; 124: cilin non-secretion and cell killing: implica-
mol 2006; 50:235238. 17881790. tions for glaucoma. Hum Mol Genet 2004;13:
38 Jones R, 3rd, Rhee DJ: Corticosteroid-in- 56 Kitazawa Y, Horie T: The prognosis of corti- 11931204.
duced ocular hypertension and glaucoma: a costeroid-responsive individuals. Arch Oph- 71 Zillig M, Wurm A, Grehn FJ, Russell P,
brief review and update of the literature. thalmol 1981; 99:819823. Tamm ER: Overexpression and properties of
Curr Opin Ophthalmol 2006; 17:163167. 57 Kass MA, Kolker AE, Becker B: Chronic top- wild-type and Tyr437His mutated myocilin
39 Singh IP, Ahmad SI, Yeh D, Challa P, Hern- ical corticosteroid use simulating congenital in the eyes of transgenic mice. Invest Oph-
don LW, Allingham RR, Lee PP: Early rapid glaucoma. J Pediatr 1972;81:11751177. thalmol Vis Sci 2005; 46:223234.
rise in intraocular pressure after intravitreal 58 Ohji M, Kinoshita S, Ohmi E, Kuwayama Y: 72 Gould DB, Miceli-Libby L, Savinova OV,
triamcinolone acetonide injection. Am J Marked intraocular pressure response to in- Torrado M, Tomarev SI, Smith RS, John SW:
Ophthalmol 2004;138:286287. stillation of corticosteroids in children. Am Genetically increasing Myoc expression sup-
40 Vedantham V: Intraocular pressure rise after J Ophthalmol 1991;112:450454. ports a necessary pathologic role of abnor-
intravitreal triamcinolone. Am J Ophthal- 59 Lam DS, Fan DS, Ng JS, Yu CB, Wong CY, mal proteins in glaucoma. Mol Cell Biol
mol 2005; 139:575; author reply 576. Cheung AY: Ocular hypertensive and anti- 2004;24:90199025.
41 Herschler J: Increased intraocular pressure inflammatory responses to different dosages 73 Fingert JH, Clark AF, Craig JE, Alward WL,
induced by repository corticosteroids. Am J of topical dexamethasone in children: a ran- Snibson GR, McLaughlin M, Tuttle L, Mack-
Ophthalmol 1976;82: 9093. domized trial. Clin Experiment Ophthalmol ey DA, Sheffield VC, Stone EM: Evaluation
42 Kalina PH, Erie JC, Rosenbaum L: Biochem- 2005;33:252258. of the myocilin (MYOC) glaucoma gene in
ical quantification of triamcinolone in sub- monkey and human steroid-induced ocular
conjunctival depots. Arch Ophthalmol 1995; hypertension. Invest Ophthalmol Vis Sci
113:867869. 2001;42:145152.
179.7.82.148 - 2/7/2017 1:18:14 AM
78 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
74 Sihota R, Konkal VL, Dada T, Agarwal HC, 91 Ng PC, Lee CH, Tam BS, Wong SP, Lam HS, 103 Dwinger MC, Pieper-Bodeewes I, Eter N,
Singh R: Prospective, long-term evaluation Kwok AK, Fok TF: Transient increase in in- Holz FG: Variations in intraocular pressure
of steroid-induced glaucoma. Eye (Lond) traocular pressure during a dose-tapering (IOP) and necessity for paracentesis follow-
2008;22:2630. regime of systemic dexamethasone in pre- ing intravitreal triamcinolone injection.
75 Levene R, Wigdor A, Edelstein A, Baum J: term infants. Ophthalmology 2008;115:e7 Klin Monbl Augenheilkd 2005; 222: 638
Topical corticosteroid in normal patients e14. 642.
and glaucoma suspects. Arch Ophthalmol 92 Mitchell P, Cumming RG, Mackey DA: In- 104 Heatley CJ, Lim KS, Siriwardena D, Barton
1967;77:593597. haled corticosteroids, family history, and K: Malignant glaucoma as a complication
76 Spiers F: Topical steroids and intraocular risk of glaucoma. Ophthalmology 1999; of intravitreal triamcinolone acetonide.
pressure. I. Clinical investigation on the re- 106:23012306. Acta Ophthalmol Scand 2006; 84: 712
actions of 93 outpatients to monocular ste- 93 Bui CM, Chen H, Shyr Y, Joos KM: Discon- 713.
roid provocation and to subsequent water- tinuing nasal steroids might lower intraoc- 105 Haller JA, Bandello F, Belfort R Jr, Blumen-
drinking test. Acta Ophthalmol (Copenh) ular pressure in glaucoma. J Allergy Clin kranz MS, Gillies M, Heier J, Loewenstein
1965;43:735745. Immunol 2005;116:10421047. A, Yoon YH, Jacques ML, Jiao J, Li XY,
77 Schwartz B: The response of ocular pressure 94 Behbehani AH, Owayed AF, Hijazi ZM, Whitcup SM: Randomized, sham-con-
to corticosteroids. Int Ophthalmol Clin Eslah EA, Al-Jazzaf AM: Cataract and ocu- trolled trial of dexamethasone intravitreal
1966;6:929989. lar hypertension in children on inhaled implant in patients with macular edema
78 Stewart RH, Kimbrough RL: Intraocular corticosteroid therapy. J Pediatr Ophthal- due to retinal vein occlusion. Ophthalmol-
pressure response to topically administered mol Strabismus 2005; 42:2327. ogy 2010;117:11341146, e1133.
fluorometholone. Arch Ophthalmol 1979; 95 Gillies MC, Simpson JM, Billson FA, Luo 106 Callanan DG, Jaffe GJ, Martin DF, Pearson
97:21392140. W, Penfold P, Chua W, Mitchell P, Zhu M, PA, Comstock TL: Treatment of posterior
79 Jamal KN, Callanan DG: The role of diflu- Hunyor AB: Safety of an intravitreal injec- uveitis with a fluocinolone acetonide im-
prednate ophthalmic emulsion in clinical tion of triamcinolone: results from a ran- plant: three-year clinical trial results. Arch
practice. Clin Ophthalmol 2009;3:381390. domized clinical trial. Arch Ophthalmol Ophthalmol 2008;126:11911201.
80 Korenfeld MS, Silverstein SM, Cooke DL, 2004;122:336340. 107 Bollinger KE, Smith SD: Prevalence and
Vogel R, Crockett RS: Difluprednate oph- 96 Chuang LH, Yeung L, Wang NK, Shen-Lih management of elevated intraocular pres-
thalmic emulsion 0.05% for postoperative Chen H, Ku WC, Lai CC: Secondary ocu- sure after placement of an intravitreal sus-
inflammation and pain. J Cataract Refract lar hypertension after intravitreal injection tained-release steroid implant. Curr Opin
Surg 2009;35:2634. with 2 mg or 4 mg of triamcinolone in reti- Ophthalmol 2009;20:99103.
81 Smith S, Lorenz D, Peace J, McLeod K, nal vein occlusion. J Ocul Pharmacol Ther 108 Goldstein DA, Godfrey DG, Hall A, Calla-
Crockett R, Vogel R: Difluprednate ophthal- 2010;26:325328. nan DG, Jaffe GJ, Pearson PA, Usner DW,
mic emulsion 0.05% (durezol) administered 97 Inatani M, Iwao K, Kawaji T, Hirano Y, Comstock TL: Intraocular pressure in
two times daily for managing ocular inflam- Ogura Y, Hirooka K, Shiraga F, Nakanishi patients with uveitis treated with fluocino-
mation and pain following cataract surgery. Y, Yamamoto H, Negi A, Shimonagano Y, lone acetonide implants. Arch Ophthalmol
Clin Ophthalmol 2010;4:983991. Sakamoto T, Shima C, Matsumura M, 2007;125:14781485.
82 Cubey RB: Glaucoma following the applica- Tanihara H: Intraocular pressure elevation 109 Jaffe GJ, Martin D, Callanan D, Pearson
tion of corticosteroid to the skin of the eye- after injection of triamcinolone acetonide: PA, Levy B, Comstock T: Fluocinolone
lids. Br J Dermatol 1976;95:207208. a multicenter retrospective case-control acetonide implant (Retisert) for noninfec-
83 Zugerman C, Saunders D, Levit F: Glaucoma study. Am J Ophthalmol 2008; 145: 676 tious posterior uveitis: thirty-four-week
from topically applied steroids. Arch Derma- 681. results of a multicenter randomized clini-
tol 1976;112:1326. 98 Jonas JB, Kreissig I, Degenring R: Intraocu- cal study. Ophthalmology 2006; 113: 1020
84 Alfano JE: Changes in the intraocular pres- lar pressure after intravitreal injection of 1027.
sure associated with systemic steroid thera- triamcinolone acetonide. Br J Ophthalmol 110 Clark AF, Wordinger RJ: The role of ste-
py. Am J Ophthalmol 1963;56:245247. 2003;87:2427. roids in outflow resistance. Exp Eye Res
85 Hovland KR, Ellis PP: Ocular changes in re- 99 Iwao K, Inatani M, Kawaji T, Koga T, Mawa- 2009;88:752759.
nal transplant patients. Am J Ophthalmol tari Y, Tanihara H: Frequency and risk fac- 111 Krishnan R, Kumar N, Wishart PK: Visco-
1967;63:283289. tors for intraocular pressure elevation after canalostomy for refractory glaucoma sec-
86 Lee PF: The influence of systemic steroid posterior sub-Tenon capsule triamcinolone ondary to intravitreal triamcinolone ace-
therapy on the intraocular pressure. Am J acetonide injection. J Glaucoma 2007; 16: tonide injection. Arch Ophthalmol 2007;
Ophthalmol 1958;46:328331. 251256. 125:12841286.
87 Lindholm B, Linner E, Tengroth B: Effects of 100 Jonas JB: Intraocular availability of triam- 112 Kubota T, Okabe H, Hisatomi T, Yamakiri
long-term systemic steroids on cataract for- cinolone acetonide after intravitreal injec- K, Sakamoto T, Tawara A: Ultrastructure of
mation and on aqueous humour dynamics. tion. Am J Ophthalmol 2004;137:560562. the trabecular meshwork in secondary
Acta Ophthalmol 1965;43:120127. 101 Breusegem C, Vandewalle E, Van Calster J, glaucoma eyes after intravitreal triamcino-
88 Diotallevi M, Bocci N: Effect of systemically Stalmans I, Zeyen T: Predictive value of a lone acetonide. J Glaucoma 2006; 15: 117
administered corticosteroids on intraocular topical dexamethasone provocative test be- 119.
pressure and fluid dynamics. Acta Ophthal- fore intravitreal triamcinolone acetonide 113 Wordinger RJ, Clark AF: Effects of gluco-
mol (Copenh) 1965; 43:524527. injection. Invest Ophthalmol Vis Sci 2009; corticoids on the trabecular meshwork: to-
89 Feiler-Ofry V, Godel V, Stein R: Systemic ste- 50:573576. wards a better understanding of glaucoma.
roids and ocular fluid dynamics. 3. The ge- 102 Bakri SJ, Pulido JS, McCannel CA, Hodge Prog Retin Eye Res 1999;18:629667.
netic nature of the ocular response and its DO, Diehl N, Hillemeier J: Immediate in- 114 Sheffield VC, Stone EM, Alward WL, Drack
different levels. Acta Ophthalmol (Copenh) traocular pressure changes following intra- AV, Johnson AT, Streb LM, Nichols BE: Ge-
1972;50:699706. vitreal injections of triamcinolone, pegap- netic linkage of familial open angle glau-
90 Adhikary HP, Sells RA, Basu PK: Ocular tanib, and bevacizumab. Eye (Lond) 2009; coma to chromosome 1q21-q31. Nat Genet
complications of systemic steroid after renal 23:181185. 1993;4:4750.
transplantation and their association with
HLA. Br J Ophthalmol 1982; 66:290291.
179.7.82.148 - 2/7/2017 1:18:14 AM
Steroid-Induced Iatrogenic Glaucoma Ophthalmic Res 2012;47:6680 79
Downloaded by:
115 Stone EM, Fingert JH, Alward WL, Nguyen 125 Fanning AS, Jameson BJ, Jesaitis LA, An- 140 Ricci F, Missiroli F, Parravano M: Argon la-
TD, Polansky JR, Sunden SL, Nishimura D, derson JM: The tight junction protein ZO-1 ser trabeculoplasty in triamcinolone ace-
Clark AF, Nystuen A, Nichols BE, Mackey establishes a link between the transmem- tonide induced ocular hypertension refrac-
DA, Ritch R, Kalenak JW, Craven ER, Shef- brane protein occludin and the actin cyto- tory to maximal medical treatment. Eur J
field VC: Identification of a gene that causes skeleton. J Biol Chem 1998; 273: 29745 Ophthalmol 2006;16:756757.
primary open angle glaucoma. Science 29753. 141 Viola F, Morescalchi F, Staurenghi G: Ar-
1997;275:668670. 126 Clark AF, Wilson K, McCartney MD, gon laser trabeculoplasty for intractable
116 Polansky JR, Fauss DJ, Chen P, Chen H, Miggans ST, Kunkle M, Howe W: Glu- glaucoma following intravitreal triamcino-
Lutjen-Drecoll E, Johnson D, Kurtz RM, cocorticoid-induced formation of cross- lone. Arch Ophthalmol 2006;124:133134.
Ma ZD, Bloom E, Nguyen TD: Cellular linked actin networks in cultured human 142 Drake M: Complications of glaucoma fil-
pharmacology and molecular biology of the trabecular meshwork cells. Invest Ophthal- tration surgery. Int Ophthalmol Clin 1992;
trabecular meshwork inducible glucocorti- mol Vis Sci 1994; 35:281294. 32:115130.
coid response gene product. Ophthalmo- 127 Wiederholt M: Direct involvement of tra- 143 Chen WL, Tsai YY, Chiang CC, Lin JM: Ar-
logica 1997;211:126139. becular meshwork in the regulation of gon laser trabeculoplasty for late glaucoma
117 Tawara A, Okada Y, Kubota T, Suzuki Y, aqueous humor outflow. Curr Opin Oph- after intravitreal triamcinolone. Acta Oph-
Taniguchi F, Shirato S, Nguyen TD, Ohni- thalmol 1998; 9:4649. thalmol 2009; 87:238239.
shi Y: Immunohistochemical localization 128 Weinreb RN, Polansky JR, Kramer SG, 144 Muecke J, Brian G: Steroid-induced ocular
of MYOC/TIGR protein in the trabecular Baxter JD: Acute effects of dexamethasone hypertension in the presence of a function-
tissue of normal and glaucomatous eyes. on intraocular pressure in glaucoma. Invest ing Molteno seton. Aust N Z J Ophthalmol
Curr Eye Res 2000;21:934943. Ophthalmol Vis Sci 1985;26:170175. 1995;23:6768.
118 Alward WL, Fingert JH, Coote MA, John- 129 Kersey JP, Broadway DC: Corticosteroid- 145 Thomas R, Jay JL: Raised intraocular pres-
son AT, Lerner SF, Junqua D, Durcan FJ, induced glaucoma: a review of the litera- sure with topical steroids after trabeculec-
McCartney PJ, Mackey DA, Sheffield VC, ture. Eye (Lond) 2006;20:407416. tomy. Graefes Arch Clin Exp Ophthalmol
Stone EM: Clinical features associated with 130 Goldmann H: Cortisone glaucoma. Int 1988;226:337340.
mutations in the chromosome 1 open-angle Ophthalmol Clin 1966;6:9911003. 146 Kaushik S, Gupta V, Gupta A, Dogra MR,
glaucoma gene (GLC1A). N Engl J Med 131 Tripathi RC, Parapuram SK, Tripathi BJ, Singh R: Intractable glaucoma following in-
1998;338:10221027. Zhong Y, Chalam KV: Corticosteroids and travitreal triamcinolone in central retinal
119 Fingert JH, Heon E, Liebmann JM, Yama- glaucoma risk. Drugs Aging 1999; 15: 439 vein occlusion. Am J Ophthalmol 2004;137:
moto T, Craig JE, Rait J, Kawase K, Hoh ST, 450. 758760.
Buys YM, Dickinson J, Hockey RR, Wil- 132 Agrawal S, Agrawal J, Agrawal TP: Vitrec- 147 Jonas JB, Degenring RF, Kamppeter BA:
liams-Lyn D, Trope G, Kitazawa Y, Ritch R, tomy as a treatment for elevated intraocular Outcome of eyes undergoing trabeculecto-
Mackey DA, Alward WL, Sheffield VC, pressure following intravitreal injection of my after intravitreal injections of triamcin-
Stone EM: Analysis of myocilin mutations triamcinolone acetonide. Am J Ophthal- olone acetonide. J Glaucoma 2004;13:261.
in 1703 glaucoma patients from five differ- mol 2004; 138:679680. 148 Honjo M, Tanihara H, Inatani M, Honda Y:
ent populations. Hum Mol Genet 1999; 8: 133 Novack GD, Howes J, Crockett RS, Sher- External trabeculotomy for the treatment
899905. wood MB: Change in intraocular pressure of steroid-induced glaucoma. J Glaucoma
120 Clark AF, Steely HT, Dickerson JE Jr, Eng- during long-term use of loteprednol eta- 2000;9:483485.
lish-Wright S, Stropki K, McCartney MD, bonate. J Glaucoma 1998;7:266269. 149 Malone PE, Herndon LW, Muir KW, Jaffe
Jacobson N, Shepard AR, Clark JI, Matsu- 134 Brennan KM, Brown RM, Roberts CW: A GJ: Combined fluocinolone acetonide in-
shima H, Peskind ER, Leverenz JB, Wilkin- comparison of topical non-steroidal an- travitreal insertion and glaucoma drainage
son CW, Swiderski RE, Fingert JH, Shef- ti-inflammatory drugs to steroids for con- device placement for chronic uveitis and
field VC, Stone EM: Glucocorticoid induc- trol of post cataract inflammation. Insight glaucoma. Am J Ophthalmol 2010; 149:
tion of the glaucoma gene MYOC in human 1993;18:89, 11. 800806, e801.
and monkey trabecular meshwork cells and 135 Jonas JB, Kreissig I, Degenring R: Second- 150 DAmico DJ, Goldberg MF, Hudson H, Jer-
tissues. Invest Ophthalmol Vis Sci 2001;42: ary chronic open-angle glaucoma after in- dan JA, Krueger DS, Luna SP, Robertson
17691780. travitreal triamcinolone acetonide. Arch SM, Russell S, Singerman L, Slakter JS, Yan-
121 Rozsa FW, Reed DM, Scott KM, Pawar H, Ophthalmol 2003;121:729730. nuzzi L, Zilliox P: Anecortave acetate as
Moroi SE, Kijek TG, Krafchak CM, Oth- 136 Moorthy RS, Mermoud A, Baerveldt G, monotherapy for treatment of subfoveal
man MI, Vollrath D, Elner VM, Richards Minckler DS, Lee PP, Rao NA: Glaucoma neovascularization in age-related macular
JE: Gene expression profile of human tra- associated with uveitis. Surv Ophthalmol degeneration: twelve-month clinical out-
becular meshwork cells in response to long- 1997;41:361394. comes. Ophthalmology 2003; 110: 2372
term dexamethasone exposure. Mol Vis 137 Smith SL, Pruitt CA, Sine CS, Hudgins AC, 2383; discussion 23842375.
2006;12:125141. Stewart WC: Latanoprost 0.005% and ante- 151 Schmidt-Erfurth U, Michels S, Michels R,
122 Sohn S, Hur W, Choi YR, Chung YS, Ki CS, rior segment uveitis. Acta Ophthalmol Aue A: Anecortave acetate for the treat-
Kee C: Little evidence for association of the Scand 1999;77:668672. ment of subfoveal choroidal neovascular-
glaucoma gene MYOC with open-angle glau- 138 Rubin B, Taglienti A, Rothman RF, Marcus ization secondary to age-related macular
coma. Br J Ophthalmol 2010;94:639642. CH, Serle JB: The effect of selective laser degeneration. Eur J Ophthalmol 2005; 15:
123 Weinreb RN, Mitchell MD, Polansky JR: trabeculoplasty on intraocular pressure in 482485.
Prostaglandin production by human tra- patients with intravitreal steroid-induced 152 Clarke MS: Anecortave acetate. Ophthal-
becular cells: in vitro inhibition by dexa- elevated intraocular pressure. J Glaucoma mology 2004; 111: 2316; author reply 2316
methasone. Invest Ophthalmol Vis Sci 2008;17:287292. 2317.
1983;24:15411545. 139 Yuki K, Inoue M, Shiba D, Kawamura R, 153 Prata TS, Tavares IM, Mello PA, Tamura C,
124 Zhuo YH, He Y, Leung KW, Hou F, Li YQ, Ishida S, Ohtake Y: Selective laser trabecu- Lima VC, Belfort R Jr: Hypotensive effect of
Chai F, Ge J: Dexamethasone disrupts in- loplasty for elevated intraocular pressure juxtascleral administration of anecortave
tercellular junction formation and cyto- following subtenon injection of triamcino- acetate in different types of glaucoma. J
skeleton organization in human trabecular lone acetonide. Clin Ophthalmol 2010; 4: Glaucoma 2010;19:488492.
meshwork cells. Mol Vis 2010;16:6171. 247249.
179.7.82.148 - 2/7/2017 1:18:14 AM
80 Ophthalmic Res 2012;47:6680 Razeghinejad /Katz
Downloaded by:
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Perbedaan Kadar Hbsag Sampel Serum Dan Plasma Metode Clia Pada PendonorDocumento7 paginePerbedaan Kadar Hbsag Sampel Serum Dan Plasma Metode Clia Pada PendonorAAK DHGRiski MaulanaNessuna valutazione finora
- Hemophilia: Factor IX (Hemophilia B)Documento38 pagineHemophilia: Factor IX (Hemophilia B)Jhvhjgj JhhgtyNessuna valutazione finora
- Ast (Sgot) ColorDocumento2 pagineAst (Sgot) ColorShribagla MukhiNessuna valutazione finora
- S/N Description UnitDocumento16 pagineS/N Description UnitPeccamb SurgicalNessuna valutazione finora
- tmpD1AB TMPDocumento9 paginetmpD1AB TMPFrontiersNessuna valutazione finora
- Abeba Final Thesis After DefenceDocumento112 pagineAbeba Final Thesis After DefenceYayew MaruNessuna valutazione finora
- Inborn Error of MetabolismDocumento33 pagineInborn Error of MetabolismAlmiraNessuna valutazione finora
- Intake and OutputDocumento3 pagineIntake and Outputtina100% (1)
- Bowen Family TheoryDocumento320 pagineBowen Family Theorytonifieraru100% (14)
- Menstrual DisordersDocumento45 pagineMenstrual DisordersMegat Mohd Azman Adzmi100% (1)
- Points From Accupuncture AtlasDocumento1 paginaPoints From Accupuncture AtlasdishkuNessuna valutazione finora
- Global Developmental DelayDocumento2 pagineGlobal Developmental DelayAtlerNessuna valutazione finora
- Nausea and Vomiting in Adolescents and AdultsDocumento30 pagineNausea and Vomiting in Adolescents and AdultsPramita Ines ParmawatiNessuna valutazione finora
- Ezhilan MBADocumento48 pagineEzhilan MBAVigneshMuchiNessuna valutazione finora
- CHF CSDocumento4 pagineCHF CSLaren CyrNessuna valutazione finora
- Supraspinatus Tendon Pathomechanics: A Current Concepts ReviewDocumento12 pagineSupraspinatus Tendon Pathomechanics: A Current Concepts Reviewgia purnamaNessuna valutazione finora
- Daftar ObatDocumento1 paginaDaftar ObatPramukadua DepokNessuna valutazione finora
- DSWD Guidelines For Residential FacilitiesDocumento12 pagineDSWD Guidelines For Residential FacilitiesCharlene Ordoñez Dela CruzNessuna valutazione finora
- Brain DeathDocumento24 pagineBrain DeathKawaljit KaurNessuna valutazione finora
- Module IIIDocumento128 pagineModule IIIJoan Clarice CorlaNessuna valutazione finora
- Migraine Patient HandoutDocumento14 pagineMigraine Patient HandoutthiautamiNessuna valutazione finora
- Mayur - 01Documento2 pagineMayur - 01mukesh jambukiyaNessuna valutazione finora
- Advanced Cardiovascular Life Support (ACLS)Documento27 pagineAdvanced Cardiovascular Life Support (ACLS)Sara Ali100% (3)
- Drugs Used in The Management of COPDDocumento6 pagineDrugs Used in The Management of COPDASWINI GNessuna valutazione finora
- Grand Halad Sa Kapamilya: List of ServicesDocumento2 pagineGrand Halad Sa Kapamilya: List of ServicesLeo LastimosaNessuna valutazione finora
- CDK Edisi CME-2 TH 2020 5 SKP PDFDocumento24 pagineCDK Edisi CME-2 TH 2020 5 SKP PDFnarinaaviNessuna valutazione finora
- Serenity: Violence, Inequality, and Recovery On The Edge of Mexico CityDocumento18 pagineSerenity: Violence, Inequality, and Recovery On The Edge of Mexico CityE Panchi NuñezNessuna valutazione finora
- H3C Abstract Final 11262014Documento204 pagineH3C Abstract Final 11262014AAPI ConventionNessuna valutazione finora
- The Tragedy of Schizophrenia Without PsychotherapyDocumento30 pagineThe Tragedy of Schizophrenia Without PsychotherapyRachel AHNessuna valutazione finora
- Food Safety HandoutsDocumento8 pagineFood Safety HandoutsNurul MaisyaraNessuna valutazione finora