Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Antidepressant Therapy Algorithm
Caricato da
Zubair Mahmood KamalCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Antidepressant Therapy Algorithm
Caricato da
Zubair Mahmood KamalCopyright:
Formati disponibili
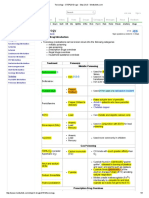
Algorithm for Initiating Antidepressant Therapy in Depression
Refer for
psychotherapy if
patient preference or
add cognitive
behavioural office
skills to antidepressant
medication
For mild depression specific psychological
treatments are preferable to antidepressants,
PHQ <15 unless history of previous
depressive episodes
Assess within 2 weeks.
Depressed
Mood
Moderate to Severe depression
(PHQ 15 or more)
Offer Antidepressant
Medication
Antidepressant
Treatment Appropriate
Under 18s: Fluoxetine
Choice of Antidepressant
Peripartum: See Family Practice
Guide section 7 or call Motherisk at
416-813-6780 www.motherisk.org
Consider:
Cost and acceptability to patient
Tolerability and adverse effects to a particular drug
Likely side effect profile/potential interactions
Risk of suicide/accidental overdose
Consider using previously effective drug
First Line : SSRI,SNRI or
Bupropion
See Family Practice Guide 3.31
Assess within 2 weeks and then every
2-4 weeks (6 weeks in elderly) for 3
months
If increased risk of suicide or younger
than 30 years, see after 1 week and
frequently thereafter.
Partial Response Choices
Family Practice Guide 3.30
postpone switch until 4-6 wks
-optimize dose
-augmentation with Lithium, T3,
or atypical antipsychotic
-switch to another class
-combine SSRI+ SNRI,
Mirtazapine, or Bupropion
Bipolar: Mood stabilizer +/antidepressant
Post MI/Acute Coronary Syndrome
Citalopram 20mg or Sertraline 50-100mg
daily
No response after 4-6weeks of
therapeutic dose:
-Switch to another first line
agent
-Consider switching classes
-Re-evaluate diagnosis
-Reassess compliance
-Reassess comorbidity
Not tolerated
Lower
dose.,
Switch to a
different
class
Ineffective
Second line agent:
Tricyclic
antidepressant
Adequate trials of 2
medications not
effective or not
tolerated
-Emergent situation
developing (psychosis,
suicidal intent)
-Diagnostic dilemma
-Significant comorbidity
Drug effective and
tolerated at any stage
Continue on same dose:
For min. 6 months after return to normal functioning/mood
if 1st episode (12 months in elderly) and then review need
for continued treatment considering number of previous
episodes, severity of initial illness, presence of residual
symptoms and concurrent psychosocial difficulties. If 2 or
more episodes treat for at least 2 years
Use gradual stepwise reduction of dose to discontinue
may not be necessary for Fluoxetine.
Refer :
Mental Health Services or
Emergency services if
patient in imminent danger
to self or other
May 2009
MAJOR DEPRESSIVE DISORDER
Not all medications listed are eligible for coverage under the No-Charge Psychiatric Medication Program (Plan G).
Coverage information is provided on the BC PharmaCare website at www.health.gov.bc.ca/pharme/outgoing/plangtable.html.
FA M I LY P H YS I C I A N G U I D E
PHARMACOLOGICAL INTERVENTION
3.31
APPENDIX 2: WOMENS MENTAL HEALTH ISSUES
Detailed information on the specific application of these treatment modalities in the
perinatal period is in the (1) Best Practices Guidelines relating to Reproductive
Mental Health, and (2) Self-Care Program for Women with postpartum depression &
anxiety (see Resources). See also the section on non-pharmacological therapies in
the Guide.
Pharmacotherapy in the Perinatal Period
Practice Issues: Antidepressants in Pregnancy and Postpartum
Sustaining maternal mental health throughout pregnancy is the key to ensuring
an optimum outcome for the baby.
As yet, there is little evidence for the efficacy of psychotherapy in the treatment
of moderate to severe depression in pregnant, depressed women.
Resolution of symptoms for women in this category is best achieved, at present,
with antidepressant medications.
Women with severe depression and with a prior history of depression can be
treated with a combination of antidepressant medication and psychotherapy.
To date, existing evidence suggests that the most commonly used antidepressant
medications, such as SSRIs (e.g., Prozac, Paxil, Zoloft, Luvox and Celexa) and
SNRIs (e.g., Effexor), have not been associated with major birth defects.
There is increasing concern regarding transient neonatal adaptation symptoms
following prenatal exposure.
This has led the Health Canada (see Health Canada Advisory below) and the US
Food and Drug Administration (FDA) to issue warnings regarding third-trimester
SSRI and SNRI use for treating depression during pregnancy.
The recent concern over the warnings by Health Canada and the US FDA
regarding infants exposed to antidepressants in the third trimester, has lead to a
clinical dilemma for treating physicians. The evidence for these warnings is:
based on case reports and retrospective data.
the number of cases studied tends to be small, particularly with newer
anti-depressants
In addition, the presence/absence of symptoms observed in neonates are
governed by a complex set of factors including:
prematurity
maternal mental and physical health
use of concomitant substances (e.g., alcohol, cigarettes)
polypharmacy
Characteristics of this Neonatal Poor Adaptation Syndrome include:
transient course in the infant
resolution within the first few days of life
no evidence of long-term consequences in the children.
the use of multiple psychotropic medications during pregnancy with an
SSRI appears to increase the risk of these symptoms
Neonatal Management Issues
An infant can be identified as being at risk for transient Neonatal Poor
Adaptation Syndrome if the mother is:
taking a high dose of any antidepressant medication
on more than one medication
if the woman is mentally ill and/or under-treated
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
7.13
APPENDIX 2: WOMENS MENTAL HEALTH ISSUES
7.14
The infants behaviour should be monitored closely :
by nursing and medical staff
if there are signs of abnormal Central Nervous System (CNS) behaviour, avoid
early discharge and consider a differential diagnosis
obtain infant drug levels if possible where a diagnosis remains unclear
Supportive neonatal care of symptomatic infants can be provided by using
the following approach:
provide low level stimulation
support breastfeeding
provide supportive measures where appropriate
follow symptoms closely
Ensure long-term follow-up for mother and infant.
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
Pharmacotherapy in the Perinatal Period: Specific Medications
7.16
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
Pharmacotherapy in the Perinatal Period: Specific Medications
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
7.17
Pharmacotherapy in the Perinatal Period: Specific Medications
7.18
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
Pharmacotherapy in the Perinatal Period: Specific Medications
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
7.19
Pharmacotherapy in the Perinatal Period: Specific Medications
7.20
FA M I LY P H YS I C I A N G U I D E
APPENDIX
2:
WOMEN S MENTAL HEALTH ISSUES
MAJOR DEPRESSIVE DISORDER
3.32
FA M I LY P H YS I C I A N G U I D E
PHARMACOLOGICAL INTERVENTION
FA M I LY P H YS I C I A N G U I D E
A D D R E S S I N G S U I C I DA L R I S K
page 2 of 6
3.73
MAJOR DEPRESSIVE DISORDER
Bipolar Disorder
Generally, initiate a mood stabilizer on admission with mania, hypomania,
or bipolar depression.
Discontinue antipsychotic typically six months after there has been a
good response.
Maintain on a mood stabilizer.
A combination of a mood stabilizer and a very low dose of an antipsychotic
is an option for treating refractory bipolar disorder.
FA M I LY P H YS I C I A N G U I D E
PHARMACOLOGICAL INTERVENTION
3.33
Potrebbero piacerti anche
- Second and Third Generation Antipsychotics: A Comprehensive HandbookDa EverandSecond and Third Generation Antipsychotics: A Comprehensive HandbookValutazione: 5 su 5 stelle5/5 (1)
- Biological Aspects of OCD SeminarDocumento60 pagineBiological Aspects of OCD Seminarneha mattikoppaNessuna valutazione finora
- INTRODUCTION TO NEUROPHARMACOLOGYyyDocumento27 pagineINTRODUCTION TO NEUROPHARMACOLOGYyyEbad RazviNessuna valutazione finora
- The Maudsley Prescribing Guidelines in PsychiatryDa EverandThe Maudsley Prescribing Guidelines in PsychiatryValutazione: 4 su 5 stelle4/5 (1)
- Neurobiology of Depression: Guide-Dr. Vijay Niranjan SirDocumento42 pagineNeurobiology of Depression: Guide-Dr. Vijay Niranjan SirPriyash JainNessuna valutazione finora
- Third Generation Antipsychotic DrugsDocumento45 pagineThird Generation Antipsychotic DrugsGabriela Drima100% (1)
- CEP BPSD Discussion Guide ENG RFCG Updated2019 PDFDocumento8 pagineCEP BPSD Discussion Guide ENG RFCG Updated2019 PDFM.DalaniNessuna valutazione finora
- Introduction To NeuropharmacologyDocumento6 pagineIntroduction To Neuropharmacologyammarhafez78100% (1)
- AripripazoleDocumento13 pagineAripripazoleOneng IfayaniNessuna valutazione finora
- Brain Imaging in PsychiatryDocumento7 pagineBrain Imaging in PsychiatryKaram Ali ShahNessuna valutazione finora
- JCP Optimizing Antipsychotics GuidelinesDocumento31 pagineJCP Optimizing Antipsychotics GuidelinesSusasti HasanahNessuna valutazione finora
- Pharmacotherapy in PschiatryDocumento8 paginePharmacotherapy in PschiatryygfhdgNessuna valutazione finora
- Treatment Resistant OCD .Documento55 pagineTreatment Resistant OCD .Dr viren SolankiNessuna valutazione finora
- First vs Second Generation Antipsychotics: CATIE & CUtLASS TrialsDocumento3 pagineFirst vs Second Generation Antipsychotics: CATIE & CUtLASS TrialsvinodksahuNessuna valutazione finora
- Polypharmacy in PsychiatryDocumento43 paginePolypharmacy in PsychiatryMike SionzonNessuna valutazione finora
- B /G C U I R: Anti-PsychoticsDocumento2 pagineB /G C U I R: Anti-PsychoticsErsy Sakti ilhamNessuna valutazione finora
- Neurobiology of SchizophreniaDocumento54 pagineNeurobiology of SchizophreniaPriyash JainNessuna valutazione finora
- Session 7 Psychiatric AssessmentDocumento54 pagineSession 7 Psychiatric AssessmentPetroNessuna valutazione finora
- Current Clinical Strategies: Handbook of Psychiatric DrugsDocumento72 pagineCurrent Clinical Strategies: Handbook of Psychiatric Drugsmike116Nessuna valutazione finora
- Psychiatry Notes - Defenses MechanismsDocumento2 paginePsychiatry Notes - Defenses MechanismsLiSenNessuna valutazione finora
- Neuroanatomy For The Psychiatrist: Textbook of PsychiatryDocumento37 pagineNeuroanatomy For The Psychiatrist: Textbook of Psychiatrykrysdana22Nessuna valutazione finora
- Antidepressant Side Effects 2006Documento9 pagineAntidepressant Side Effects 2006Renny AnggrainiNessuna valutazione finora
- Geriatric Giants - DR SeymourDocumento108 pagineGeriatric Giants - DR SeymourSharon Mallia100% (1)
- Types of DepressionDocumento12 pagineTypes of DepressionKADAMBARINessuna valutazione finora
- SchizophreniaDocumento22 pagineSchizophrenianabeelNessuna valutazione finora
- Terms in The Field of Psychiatry and NeurologyDocumento25 pagineTerms in The Field of Psychiatry and NeurologyMarlon SigfredNessuna valutazione finora
- Overview of Psychotropic DrugsDocumento7 pagineOverview of Psychotropic Drugsnad101Nessuna valutazione finora
- Geriatric Psychiatry LectureDocumento113 pagineGeriatric Psychiatry LectureabrihamNessuna valutazione finora
- Antidepressants Comparison Guide Most Commonly Prescribed: Recommend GenericsDocumento3 pagineAntidepressants Comparison Guide Most Commonly Prescribed: Recommend GenericsCarina ColtuneacNessuna valutazione finora
- Antipsychotic DrugsDocumento47 pagineAntipsychotic DrugsIkram UddinNessuna valutazione finora
- Psychiatry Capstone 43020 Agitation PsychopharmacologyDocumento20 paginePsychiatry Capstone 43020 Agitation Psychopharmacologyapi-552282470Nessuna valutazione finora
- Archives of Indian Psychiatry OctoberDocumento63 pagineArchives of Indian Psychiatry OctoberGanpat Vankar100% (1)
- Mobile Clinic Mobile PSE GuideDocumento18 pagineMobile Clinic Mobile PSE GuideFrancisco Javier Salazar Núñez100% (1)
- Intro To Clinical PsychiatryDocumento26 pagineIntro To Clinical PsychiatryNoelle Grace Ulep Baroman100% (1)
- Terms in The Field of PsychiatryDocumento18 pagineTerms in The Field of PsychiatryOchie YecyecanNessuna valutazione finora
- Glutamate & Gaba: NeurotransmittersDocumento33 pagineGlutamate & Gaba: NeurotransmittersPanchitaJuarezNessuna valutazione finora
- AntidepressantsDocumento4 pagineAntidepressantsSalman HabeebNessuna valutazione finora
- Pharmacology and Toxicology of Antidepressants and AntipsychoticsDocumento50 paginePharmacology and Toxicology of Antidepressants and AntipsychoticsPintu Bhushan MitraNessuna valutazione finora
- Second and Third Year Psychiatry Residency QuizDocumento5 pagineSecond and Third Year Psychiatry Residency QuizSpacetoon Days100% (1)
- Psychiatry ExamDocumento4 paginePsychiatry Examapi-3703352Nessuna valutazione finora
- Off-Label Trazodone Prescription-Evidence, Benefits and RisksDocumento9 pagineOff-Label Trazodone Prescription-Evidence, Benefits and RisksomarapesNessuna valutazione finora
- Varun Kumar, 2017 - Getting Started in PsychiatryDocumento148 pagineVarun Kumar, 2017 - Getting Started in PsychiatryBernard FZ100% (1)
- Shortened REM Latency and Increased REM: Previous AttemptDocumento19 pagineShortened REM Latency and Increased REM: Previous AttemptActeen MyoseenNessuna valutazione finora
- Why Psychiatry? Some Thoughts For Medical Students.Documento3 pagineWhy Psychiatry? Some Thoughts For Medical Students.Davin TanNessuna valutazione finora
- Treatment Modalities For Mood DisordersDocumento55 pagineTreatment Modalities For Mood DisordersGlory MimiNessuna valutazione finora
- Common Psychiatric TermsDocumento6 pagineCommon Psychiatric TermsKatrina Heart Rauto AvilaNessuna valutazione finora
- Understanding Schizoaffective DisorderDocumento2 pagineUnderstanding Schizoaffective DisorderRumana AliNessuna valutazione finora
- Alcohol Use Disorder MGMT Guideline - Final... EstDocumento83 pagineAlcohol Use Disorder MGMT Guideline - Final... EstMuluken TesfayeNessuna valutazione finora
- Psychiatry Beginners ManualDocumento132 paginePsychiatry Beginners ManualGabriel Viana SilveiraNessuna valutazione finora
- Psychiatry: ' ' Psychology 538 ' Pathology 540 ' Pharmacology 556Documento24 paginePsychiatry: ' ' Psychology 538 ' Pathology 540 ' Pharmacology 556Brush LowdryNessuna valutazione finora
- Psychiatry MD Paper IDocumento5 paginePsychiatry MD Paper Iprasad8384Nessuna valutazione finora
- Nuero-Psychiatry: Multiple Choice Questions: (Mcqs Model Paper 2007)Documento25 pagineNuero-Psychiatry: Multiple Choice Questions: (Mcqs Model Paper 2007)usamaNessuna valutazione finora
- Psychiatry Diagnosis PDFDocumento4 paginePsychiatry Diagnosis PDFEpstein HouseNessuna valutazione finora
- Mood DisordersDocumento1 paginaMood DisordersTeresa MartinsNessuna valutazione finora
- MC IIIA Topics: Midterm Material. Won't Be in The Final Exam, Only Antiparkinsonian IncludedDocumento138 pagineMC IIIA Topics: Midterm Material. Won't Be in The Final Exam, Only Antiparkinsonian IncludedToqa ElmansouryNessuna valutazione finora
- Anatomy and Physiology eBook CollectionDocumento1 paginaAnatomy and Physiology eBook CollectionLavinia BădiciNessuna valutazione finora
- UW Notes - 13 - PsychiatryDocumento21 pagineUW Notes - 13 - PsychiatryDor BenayounNessuna valutazione finora
- HPI GuidelinesDocumento5 pagineHPI GuidelinesHani NadiahNessuna valutazione finora
- Pharmacological Management of DepressionDocumento66 paginePharmacological Management of DepressionPriyash JainNessuna valutazione finora
- Social Psychology-1Documento23 pagineSocial Psychology-1Zubair Mahmood KamalNessuna valutazione finora
- PanjgurDocumento39 paginePanjgurKashani DrShoaibNessuna valutazione finora
- AHD 2013 Lafontaine - Psychogenic Movement Disorders2011no VideosDocumento33 pagineAHD 2013 Lafontaine - Psychogenic Movement Disorders2011no VideosZubair Mahmood KamalNessuna valutazione finora
- Psychological Impact of COVID-19 and Lockdown Among University Students in Malaysia: Implications and Policy RecommendationsDocumento13 paginePsychological Impact of COVID-19 and Lockdown Among University Students in Malaysia: Implications and Policy RecommendationsCindy MamalangkasNessuna valutazione finora
- Psychiatric Aspects of Somatic Disorder in Child andDocumento61 paginePsychiatric Aspects of Somatic Disorder in Child andZubair Mahmood KamalNessuna valutazione finora
- Update in Clinical Psychopharmacology: Peter A. Demaria, JR., M.D., FasamDocumento52 pagineUpdate in Clinical Psychopharmacology: Peter A. Demaria, JR., M.D., FasamZubair Mahmood KamalNessuna valutazione finora
- EnuresisDocumento31 pagineEnuresisZubair Mahmood KamalNessuna valutazione finora
- Legal Aspect of Child CareDocumento56 pagineLegal Aspect of Child CareZubair Mahmood KamalNessuna valutazione finora
- Icd 11 New Question For MrcpsychDocumento8 pagineIcd 11 New Question For MrcpsychZubair Mahmood KamalNessuna valutazione finora
- Somatic Symptom DisorderDocumento55 pagineSomatic Symptom DisorderZubair Mahmood KamalNessuna valutazione finora
- Psychosocial and Socio-Economic Crisis in Bangladesh Due To COVID-19 Pandemic: A Perception-Based AssessmentDocumento17 paginePsychosocial and Socio-Economic Crisis in Bangladesh Due To COVID-19 Pandemic: A Perception-Based AssessmentZubair Mahmood KamalNessuna valutazione finora
- Movement Disorders: K. ZárubováDocumento32 pagineMovement Disorders: K. ZárubováZubair Mahmood KamalNessuna valutazione finora
- PsychopharmacologyDocumento95 paginePsychopharmacologyTomChristianNessuna valutazione finora
- Contemporary Powerpoint School of Management WidescreenDocumento13 pagineContemporary Powerpoint School of Management WidescreenonemalaysiaNessuna valutazione finora
- Gut Metagenomics-Derived Genes As Potential Biomarkers of Parkinson's DiseaseDocumento16 pagineGut Metagenomics-Derived Genes As Potential Biomarkers of Parkinson's DiseaseZubair Mahmood KamalNessuna valutazione finora
- White Matter Abnormalities Across Different Epilepsy Syndromes in Adults: An ENIGMA-Epilepsy StudyDocumento20 pagineWhite Matter Abnormalities Across Different Epilepsy Syndromes in Adults: An ENIGMA-Epilepsy StudyZubair Mahmood KamalNessuna valutazione finora
- Covid Reference: Bernd Sebastian Kamps Christian HoffmannDocumento172 pagineCovid Reference: Bernd Sebastian Kamps Christian HoffmannZubair Mahmood KamalNessuna valutazione finora
- PsychopharmacologyDocumento116 paginePsychopharmacologyZubair Mahmood KamalNessuna valutazione finora
- Two Centuries of Neurology and Psychiatry Nejm DoczDocumento8 pagineTwo Centuries of Neurology and Psychiatry Nejm DoczZubair Mahmood KamalNessuna valutazione finora
- Notable Articles of 2019 PDFDocumento44 pagineNotable Articles of 2019 PDFjmin49Nessuna valutazione finora
- Management of Gout in AdultsDocumento3 pagineManagement of Gout in AdultsZubair Mahmood KamalNessuna valutazione finora
- Condensed ADULT DIABETIC KETOACIDOSIS (DKA) MANAGEMENT CHART Aug 2017Documento2 pagineCondensed ADULT DIABETIC KETOACIDOSIS (DKA) MANAGEMENT CHART Aug 2017Zubair Mahmood KamalNessuna valutazione finora
- SARS-CoV-2 Is Present in Peritoneal Fluid in COVID-19 PatientsDocumento5 pagineSARS-CoV-2 Is Present in Peritoneal Fluid in COVID-19 PatientsELizabeth OlmosNessuna valutazione finora
- CASC Cases MRCGP PDFDocumento48 pagineCASC Cases MRCGP PDFZubair Mahmood KamalNessuna valutazione finora
- PIIS0140673620310424Documento10 paginePIIS0140673620310424JohnStrowskyNessuna valutazione finora
- Recovery Dexamethasone Statement 160620 V2finalDocumento2 pagineRecovery Dexamethasone Statement 160620 V2finalZubair Mahmood KamalNessuna valutazione finora
- Jama Sanders 2020 RV 200005Documento13 pagineJama Sanders 2020 RV 200005Juan Carlos PabonNessuna valutazione finora
- Remdesivir For COVID19Documento12 pagineRemdesivir For COVID19Zubair Mahmood KamalNessuna valutazione finora
- INVEGA SUSTENNA-piDocumento18 pagineINVEGA SUSTENNA-piSponge BobNessuna valutazione finora
- Treatment and Prevention of Enteric (Typhoid and Paratyphoid) Fever - UpToDate 2020Documento17 pagineTreatment and Prevention of Enteric (Typhoid and Paratyphoid) Fever - UpToDate 2020Zubair Mahmood KamalNessuna valutazione finora
- Dispensing, Incompatibilities, ADR PDFDocumento19 pagineDispensing, Incompatibilities, ADR PDFKate Evangelista100% (1)
- Respiratory MedicationsDocumento18 pagineRespiratory Medicationsapi-338095748Nessuna valutazione finora
- BromazepamDocumento6 pagineBromazepamMariusNeicuNessuna valutazione finora
- Factors Influencing Bioavailability of Drugs PDFDocumento2 pagineFactors Influencing Bioavailability of Drugs PDFRoy50% (2)
- A Survey Exploring The Knowledge and Perceptions of Senior Medical Students in Nepal Toward Generic MedicinesDocumento6 pagineA Survey Exploring The Knowledge and Perceptions of Senior Medical Students in Nepal Toward Generic MedicinesDavids MarinNessuna valutazione finora
- DiureticsDocumento4 pagineDiureticsNazmul Islam AbirNessuna valutazione finora
- SEMINAR - 7 (Pharmacoepidemilogy)Documento69 pagineSEMINAR - 7 (Pharmacoepidemilogy)LathaVijendraNessuna valutazione finora
- OTC drug database with active ingredientsDocumento7.389 pagineOTC drug database with active ingredientsserifblackNessuna valutazione finora
- IV Solutions, Equipment, and CalculationsDocumento48 pagineIV Solutions, Equipment, and CalculationsEn RasNessuna valutazione finora
- Toxicology - MedbulletsDocumento5 pagineToxicology - MedbulletsindyaholicNessuna valutazione finora
- Acls Algorithms 2012Documento12 pagineAcls Algorithms 2012Prashanth KumarNessuna valutazione finora
- Life Cycle Management of Ageing Pharmaceutical - Sokol - MansoDocumento4 pagineLife Cycle Management of Ageing Pharmaceutical - Sokol - Mansonu_disaster0% (1)
- Causes, Symptoms and Treatments of VaginitisDocumento16 pagineCauses, Symptoms and Treatments of VaginitisMae Christelle Hamoy100% (2)
- The Tanzania Food, Drugs and Cosmetics Act, 2003Documento89 pagineThe Tanzania Food, Drugs and Cosmetics Act, 2003ananthNessuna valutazione finora
- Drugs and Their ClassificationDocumento23 pagineDrugs and Their Classificationkalkigarg0% (2)
- JDDR 139Documento11 pagineJDDR 139Earthjournal PublisherNessuna valutazione finora
- Management of Pain: Classification, Assessment, Treatment OptionsDocumento40 pagineManagement of Pain: Classification, Assessment, Treatment OptionsMaduka SanjeewaNessuna valutazione finora
- Controlled Release Oral Drug Delivery SystemsDocumento37 pagineControlled Release Oral Drug Delivery Systemsamitchauhan09Nessuna valutazione finora
- General AnesthesiaDocumento58 pagineGeneral AnesthesiaAli Mohamed100% (1)
- Insomnia QuestionnaireDocumento6 pagineInsomnia QuestionnaireNuradila Athirah LockmanNessuna valutazione finora
- 8 Sample Care Plans For ACDFDocumento11 pagine8 Sample Care Plans For ACDFacasulla98Nessuna valutazione finora
- Top analgesics, anti-inflammatories and antihistaminesDocumento3 pagineTop analgesics, anti-inflammatories and antihistaminesFrancineAntoinetteGonzalesNessuna valutazione finora
- Commonly Used Vet DrugsDocumento31 pagineCommonly Used Vet DrugsIfran ChowdhuryNessuna valutazione finora
- Indiana Article 2 Controlled SubstancesDocumento73 pagineIndiana Article 2 Controlled SubstancesJon EvanenkoNessuna valutazione finora
- Calculation of DosesDocumento10 pagineCalculation of DosesDavinWijaya100% (1)
- Famotidine (Pepcid)Documento1 paginaFamotidine (Pepcid)Adrianne BazoNessuna valutazione finora
- Daftar Obat FahrenheitDocumento15 pagineDaftar Obat FahrenheitRahmah Gadis Wartania Putri50% (2)
- Allergy Clinic Policy and ProceduresDocumento4 pagineAllergy Clinic Policy and ProceduresMiselonNessuna valutazione finora
- EUCAST Expert Rules for PneumococcusDocumento3 pagineEUCAST Expert Rules for PneumococcusJulyadharma Wangsa DharmaNessuna valutazione finora
- Drugs: G L David Krupadanam - D Vijaya Prasad K Varaprasad Rao - K L N Reddy C SudhakarDocumento4 pagineDrugs: G L David Krupadanam - D Vijaya Prasad K Varaprasad Rao - K L N Reddy C SudhakarANU CHOUDHARY0% (3)