Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pakya ECG Basics
Caricato da
Frederick CokroCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pakya ECG Basics
Caricato da
Frederick CokroCopyright:
Formati disponibili
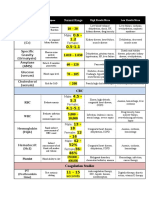
ECG BASICS
-criteriae for normal sinus rhythm (benda nie beza2, so myb different
bw different sources)
1. heart rate of 60-100 bpm
2. regular rhythm
3. P wave must present for every QRS complex in ratio of 1:1
4. PR interval is bw 0.12 sec to 0.2 sec (3-5 small sq)
5. QRS should be less than 0.12 sec (3 small sq)
-lead v1/v2 look at RV, lead v3/v4 look at IV septum, lead v5/v6 look at
LV
-description of ECG step by step
1. rhythm & rate
4. cardiac axis
2. PR interval
5. T waves, ST segments, etc
3. QRS complex duration
origin of
-P waves - atrial contraction
-QRS - ventricular depolarization
-T - ventricular repolarization
-U - repolarization of papillary ms
first degree heart block
-signs of CAD, acute rheumatic carditis, digoxin toxicity, or electrolyte
disturbances
-PR interval prolonged (normal 3-5 small sq)
-1 small square 0.04 sec (40 millisec)
-1 large sq 0.2 sec (200 ms)
-5 large sq 1 sec
-to calculate heart rate - 300 divide by how many large boxes bw R-R
-normal PR interval - 3-5 small squares
-normal QRS complex - less than 3 small squares
-normal QT interval - less than 2.5 large sq (<450 millisec). if >450 may
leads to VT
-right leg - earth lead
-cardiac rhythm - identify from whichever lead shows P wave most
clearly, usually lead 2
-to determine cardiac axis, look at lead 1 and 2, in which one the S
wave taller than R wave? [1R 2L]
1. if in lead 1 then it is right axis deviation (+90 to -90) - means RV
hypertrophy
2. if in lead 2 then it is left axis deviation (-30 to -90) - means LV
hypertrophy
3. if both lead 1 and lead 2 S is shorter than R, then normal cardiac axis
(N cardiac axis -30 to +90)
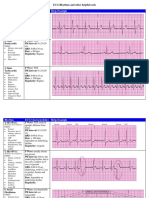
second degree heart block
-there are 3 variations
1. wenckebach or mobitz type 1
-one nonconducted P wave followed by progressively longer
conducted waves
-in mobitz type 1 next conducted beat has longer PR interval than
preceeding conducted beats
2. mobitz type 2
-one P wave not followed by QRS complex
-PR interval of conducted beats is constant
right axis deviation
left axis deviation
ECG axis
3. 2:1, 3:1 or 4:1 conduction AV block
-2:1 means 2 P waves per QRS complex. same for 3:1 and 4:1
-the jarak bw P is constant regardless ada QRS or not
-the cause of 1st degree heart block is delay somewhere along the
conduction pathway
-for 2nd degree heart block the excitation completely fails to pass
through AV node or bundle of His. the underlying causes are still the
same as 1st degree heart block
-wenckebach is usually benign but mobitz type 2, 2:1, 3:1, and 4:1 may
precedes complete or 3rd degree heart block
third degree heart block / complete heart block
-occur when atrial contraction normal but no beats conducted to the
ventricles
-may occur as acute phenomenon in pt with MI (usually transient), or it
myb chronic, usually dt fibrosis around bundle of His. may also be
caused by block of both bundle branches
-possible patterns
1. PR interval at all leads no consistency
3. abN shaped QRS
2. no relationship bw P & QRS
pathways of depolarization
-conduction problems in :1. AV/BoH 2. LBB/RBB - results in bundle branch block
with its large muscle mass
6. if RBBB + LAH - ECG shows RBBB + left axis deviation - also called as
bifascicular block
-bifascicular block indicates widespread damage to the conducting
system!
complete heart block
-RBBB can be further divided into 2, complete and incomplete RBBB.
incomplete RBBB are those with QRS <120 millisec whereas complete
RBBB are those with QRS >120 millisec
-causes of RBBB - normal heart, ASD & other congenital heart dz, PE
bundle branch blocks
-wide QRS complex - indicates bundle branch block
-RBBB - often indicates problems in right side of heart. but RBBB
patterns with QRS complex of normal duration (incomplete RBBB) are
quite common in healthy people
-LBBB however, always an indication of heart dz, usually of LV
-RBBB pattern 1. 2nd R wave (RSR') in lead v1
2. wide & deep S wave, and consequently a wide QRS complex in lead
v6
-LBBB pattern 1. M pattern, best seen in lead v6
2. W pattern in lead v1, often not fully developed
3. associated with T inversion in lateral leads (1, aVL, v5-v6), though
not necessarily in all these
ECG BASICS (PAGE 2)
practical issues
1-first degree block
-often seen in normal people. but always think of AMI & ARF
-no specific action needed
2- second degree block
-usually indicates heart dz. often seen in AMI
-mobitz type 2 & wenckebach block do not need specific tx
-2:1, 3:1, or 4:1 block may indicate need for temporary of permanent
pacing, esp if ventricular rate is slow
4) accelerated idioventricular rhythm
-often ass with AMI
-although appearance of ECG similar to VT, AIR is benign & should not
be treated
-VT should not be diagnosed unless HR > 120/min
-pattern - ventricle escape, wide QRS, abN T
3- third degree block / complete heart block
-always indicates conducting tissue dz - more often fibrosis than
ischemic
-consider temporary or permanent pacemaker
4- RBBB
-think about ASD. no specific tx
5- LBBB
-think about aortic stenosis & ischemic dz
-if pt asx no action needed
-if pt recently had severe chest pain, LBBB may indicate an AMI, and
intervention should be considered
6- left axis deviation
-think about LV hypertrophy and its causes. no action needed
7- bifascicular block
-indicates severe conducting tissue d/o. no specific tx needed
-pacemaker required if pt has sx suggestive of intermittent complete
heartblock
*extrasystole - a premature cardiac contraction that is independent of
the normal rhythm and arises in response to an impulse outside the
SAN
5)supraventricular extrasystole. 2 forms
a- atrial extrasystole - appears as early and abN P wave, followed by
normal QRS complex
b- junctional extrasystole - no P wave, normal QRS
atrial
extrasystole
---here begins the little bit more complex part of ECG--1)atrial escape
-atrium takes over as focus of depolarization
-abN P with normal QRS
-if widespread called as ectopic atrial rhythm
junctional extrasystole
2) junctional escape
-AV node takes over as focus of depolarization
-no P, normal QRS
3) ventricular escape
-no P, abN QRS (& wide), abN T
6) ventricular extrasystole
-common, but usually of no importance. but when they occur early in T
wave of preceding beat they may induce VF
-early beat, wide QRS, abN T
ventricular extrasystole occur at peak of T waves of preceeding sinus
beats
-R on T phenomenon
torsades de pointes VT
-broad complex tachycardia in which QRS initially upright but then
changed to become downward pointing
-its either self-limiting or progress to VF
7) atrial flutter
-atrial rate of >250/min & no flat baseline bw P waves (sawtooth
appearance)
-atrial flutter usually with AV block eg atrial flutter with 2:1 block, atrial
flutter with 3:1 block
8) supraventricular tachycardia
a- atrial tachycardia -P waves superimposed on T waves of preceding
beats. normal QRS
b- junctional tachycardia - no P waves, QRS complexes completely
regular, narrow QRS, normal T waves
10) atrial fibrillation
-irregularly irregular rhythm
-no P waves, irregular baseline, QRS complexes mb irregular or normal
shaped
-some waves may resembles atrial flutter (common in AF)
11) ventricular fibrillation
-ECG totally disorganized, no QRS complex can be identified, pt loss of
consciousness
atrial tachycardia
12) Wolff-Parkinson-White (WPW) syndrome
-short PR interval, QRS complex shows early slurred upstroke called
delta wave
junctional tachycardia
9) ventricular tachycardia
-also called broad complex tachycardia. theres wide QRS, T waves
difficult to identify, no P wave
13) Lown-Ganong-Levine (LGL) syndrome
-short PR with normal QRS
WPW syndrome
LGL syndrome
ECG BASICS (PAGE 3)
abN of P wave
1)RA hypertrophy - causes - tricuspid valve stenosis, pulmonary HPT
-P wave peaked
-only significant if features of RVH present
2)LA hypertrophy -causes - usually dt mitral stenosis
-broad & bifid P wave
digoxin
subendocardial ischemia (exercise induced or during angina atk)
RA hypertrophy
LA hypertrophy
abN of QRS complex
-normal QRS 1. duration <3 small sq
2. V1, S>R
3. in V5-V6, height of R <25 mm
4. V5-V6 may show Q waves dt septal depolarization, but less than
2 mm deep & <1 small sq
1)abN of the width
-abN wide in BBB, or when ventricular ms takes over as focus of
depolarization, or in WPW syndrome
2)height of QRS compex
a-RV hypertrophy
-in V1, R>S
-deep S waves in V6 (clockwise rotation)
-rt axis deviation, peaked P waves,
-in severe cases, inversion of T in V1 & V2, sometimes in V3 & V4
b-pulmonary embolism
-ECG may shows features of RV hypertrophy
-when PE suspected, look for any of following :
-peaked P waves -inverted T in V1 spreading across V2-V3
-rt axis deviation -clockwise rotation
-tall R in V1
-Q wave in lead III resembling inf infarction
-RBBB
c-LV hypertrophy
-tall R in V5-V6, deep S in V1-V2 (but in practical are unhelpful to dx
LV enlargement)
-with significant hypertrophy inverted T in I, aVL, V5, V6,
sometimes V4, there mb left axis deviation
-diffcult to dx minor degrees of LVH
d-MI (tgk nota ACS)
abN of ST segment
-normal - isoelectric - same lvl as part bw T & next P
-elevation - indication of acute myocardial injury, usually dt either to
recent infarction or pericarditis
-horizontal depression ass with upright T wave usualy sn of ischemia as
opposed to infarction eg exercise induced angina
-digoxin downward sloping ST (reversed tick)
abN of T wave
-T wave inversion is seen in the following :
1. normal - leads aVR, V1, sometimes leads III & V2
2. MI/ischemia
4. BBB
3. ventricular hypertrophy 5. digoxin
-biphasic T waves seen in leads adjacent to those
showing inverted T waves
electrolyte abN
-hypoK - T wave flattening + appearance of a hump on end of T wave
called as U wave
-hyperK -peaked T waves with disappearance of ST segment
-QRS complex mb widened
2+
-effects of abN Mg lvl are similar
-hypoCa - prolongation of QT interval
-hyperCa - shortens QT interval
-hypo/hyperNa - no effect on ECG
prolonged QT (>450 ms or 11 small sq)
-causes - Romano-Ward syndrome
-antiarrhythmic drugs (mc) eg amiodarone, procainamide,
disopyramide, sotalol
-other drugs - TCA, erythromycin
-low K, low Mg, low Ca
-sick sinus syndrome - sinus bradycardia + junctional escape (or could
be others eg atrial extrasystole etc)
-pt often asx, but may complain dizziness,
syncope, or sx suggesting paroxysmal tachycardia
Potrebbero piacerti anche
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsDa EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNessuna valutazione finora
- ECGDocumento6 pagineECGMatthew MackeyNessuna valutazione finora
- EKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Da EverandEKG and ECG Interpretation: Learn EKG Interpretation, Rhythms, and Arrhythmia Fast!Nessuna valutazione finora
- ECG ReadingDocumento11 pagineECG ReadingSuresh Shrestha100% (1)
- ECG and ArrhythmiasDocumento25 pagineECG and ArrhythmiasRashed ShatnawiNessuna valutazione finora
- Wolff-Parkinson- White-Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandWolff-Parkinson- White-Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- EKG Pocket GuideDocumento2 pagineEKG Pocket GuideFabian Ramirez HincapiéNessuna valutazione finora
- EKG InterpretationDocumento65 pagineEKG Interpretationpaskariatne probo dewi100% (1)
- ECG InterpretationDocumento40 pagineECG InterpretationMuhammad BadrushshalihNessuna valutazione finora
- Cardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandCardiac Tamponade, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- A Simplified ECG GuideDocumento4 pagineA Simplified ECG Guidejalan_z96% (27)
- Cardiac Arrhythmia Recognition: an easy learning guideDa EverandCardiac Arrhythmia Recognition: an easy learning guideNessuna valutazione finora
- EKG Flash CardsDocumento5 pagineEKG Flash CardsRyann Sampino FreitasNessuna valutazione finora
- Reading A EKGDocumento10 pagineReading A EKGMayer Rosenberg100% (15)
- May/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12Documento3 pagineMay/No P: Inverted/B/ A Qrs P (Befor e QRS) - 0.12is_aradanas0% (1)
- Basic Arrhythmia RulesDocumento3 pagineBasic Arrhythmia Rulesgreenflames0997% (30)
- EKG Rhythms2 PDFDocumento7 pagineEKG Rhythms2 PDFAya KamajayaNessuna valutazione finora
- Mini Test QUIZDocumento9 pagineMini Test QUIZAbdul RohimNessuna valutazione finora
- ECG Interpretation - Axis and Conduction AbnormalitiesDocumento9 pagineECG Interpretation - Axis and Conduction Abnormalitiesradha1000100% (1)
- EKG Practice TestDocumento16 pagineEKG Practice TestAbdul Rohim100% (1)
- Cardiac Rhythms and DysrhythmiasDocumento14 pagineCardiac Rhythms and DysrhythmiasShawn Gaurav Jha100% (1)
- Ekg Guidelines PDFDocumento7 pagineEkg Guidelines PDFd.ramadhan100% (1)
- Cardiac DysrhythmiasDocumento3 pagineCardiac DysrhythmiasKatherine Santiago92% (62)
- Ecg Cheat Sheet 35Documento2 pagineEcg Cheat Sheet 35jessjaylee80% (5)
- Advanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineDocumento88 pagineAdvanced Ekg Interpretation: Micelle J. Haydel, M.D. LSU New Orleans Emergency MedicineRoroNessuna valutazione finora
- Dysrhythmias ChartDocumento6 pagineDysrhythmias Chartjkrix100% (1)
- Ecg Reading NotesDocumento17 pagineEcg Reading NotesMarian FloresNessuna valutazione finora
- Basic EKG For DummiesDocumento133 pagineBasic EKG For Dummieseduardocmoura86% (7)
- Spotlight On Cardiac DrugsDocumento2 pagineSpotlight On Cardiac Drugspauerish100% (2)
- Cardiac Dysrhythmia Chart Med-Surg NUR4Documento3 pagineCardiac Dysrhythmia Chart Med-Surg NUR4ktfosterfd2096% (97)
- Cardiac PacingDocumento89 pagineCardiac Pacingsandwhale056Nessuna valutazione finora
- EKG Flash Cards PDFDocumento9 pagineEKG Flash Cards PDFdiani arisandhi100% (1)
- BASIC ECG READING For Nle NOVEMBER 2018Documento63 pagineBASIC ECG READING For Nle NOVEMBER 2018Sharmaine KimmayongNessuna valutazione finora
- Basic EKG Interpretation Exam AnswersDocumento3 pagineBasic EKG Interpretation Exam AnswerstwdroppointNessuna valutazione finora
- Name That EKG: D:/My Documents/Documents/AIME/Handouts/EKG PracticeDocumento5 pagineName That EKG: D:/My Documents/Documents/AIME/Handouts/EKG PracticelcascolanNessuna valutazione finora
- ECG StripsDocumento5 pagineECG Stripssurviving nursing school100% (1)
- Dubin ECG Reference SheetsDocumento13 pagineDubin ECG Reference SheetsEllie100% (1)
- ArrhythmiaDocumento2 pagineArrhythmiaChris Pritchard93% (30)
- Cardiac Study GuideDocumento11 pagineCardiac Study Guidejenwiley318096% (73)
- EKG Practice PowerpointDocumento25 pagineEKG Practice PowerpointDave Amarasinghe100% (2)
- Critical Care - Hemodynamic Monitoring TableDocumento7 pagineCritical Care - Hemodynamic Monitoring TableVictoria Romero100% (2)
- Heart Sounds & MurmursDocumento32 pagineHeart Sounds & MurmursVisruth M Kumar100% (1)
- ECG StripsDocumento5 pagineECG StripsNursingSchoolNotes100% (1)
- EKG Cheat SheetDocumento9 pagineEKG Cheat SheetAlert Twitter100% (5)
- Lab ValuesDocumento3 pagineLab Valuessurviving nursing school100% (1)
- Cardiac Study Guide PDFDocumento11 pagineCardiac Study Guide PDF281175100% (1)
- Dysrhytmia NotesDocumento11 pagineDysrhytmia NoteshannahhwolfNessuna valutazione finora
- EcgDocumento57 pagineEcgenii_ta100% (9)
- Ekg Strip NotesDocumento13 pagineEkg Strip NotesNick Loizzo100% (2)
- Ecg CookbookDocumento2 pagineEcg CookbookCalin Popa100% (1)
- EKG RhythmsDocumento10 pagineEKG RhythmsQueenNessuna valutazione finora
- Rhythm ECG Characteristics Strip Example: ECG Rhythms and Other Helpful ToolsDocumento6 pagineRhythm ECG Characteristics Strip Example: ECG Rhythms and Other Helpful ToolsJohnildy MatiasNessuna valutazione finora
- Paramedic Pediatric Scenario 2017Documento3 pagineParamedic Pediatric Scenario 2017Chad StreetNessuna valutazione finora
- Acid-Base WorksheetDocumento2 pagineAcid-Base WorksheetMayer Rosenberg100% (18)
- Practice StripsDocumento9 paginePractice StripsErica Yamamoto50% (4)
- ACLS EKG Rhythms and InterpretationDocumento10 pagineACLS EKG Rhythms and Interpretationdonheyzz_02Nessuna valutazione finora
- Ecg StripsDocumento39 pagineEcg StripsNursyNurse100% (3)
- Child With HematuriaDocumento42 pagineChild With HematuriaalaaNessuna valutazione finora
- Lampiran Berita Acara Pemusnahan Reagen Dan Bahan Medis Habis Pakai Tanggal 28 Januari 2019Documento2 pagineLampiran Berita Acara Pemusnahan Reagen Dan Bahan Medis Habis Pakai Tanggal 28 Januari 2019HendroNessuna valutazione finora
- Based Isometric Handgrip Exercise Terhadap PenurunanDocumento13 pagineBased Isometric Handgrip Exercise Terhadap Penurunanemanuelin petriNessuna valutazione finora
- Abstract MCVU 2019Documento1 paginaAbstract MCVU 2019Afdhalia Khairunnisa SyammarhanNessuna valutazione finora
- Heart Disease in Pregnancy: Mohana PreeshaDocumento50 pagineHeart Disease in Pregnancy: Mohana PreeshaChuks LeviNessuna valutazione finora
- CRF LvadDocumento5 pagineCRF LvadAnonymous oQtve4oNessuna valutazione finora
- Acls AlgorithmDocumento6 pagineAcls AlgorithmDet LaurenteNessuna valutazione finora
- Physician Assistant Certification and Recertification Exam Review - PANRE - PANCEDocumento14 paginePhysician Assistant Certification and Recertification Exam Review - PANRE - PANCEThe Physician Assistant Life100% (3)
- ACGME-Accredited Specialties and SubspecialtiesDocumento4 pagineACGME-Accredited Specialties and SubspecialtiesWan Nurul AmieraNessuna valutazione finora
- Case 1 Recruitment at Windsor Hospital Student Copy 1629976167334Documento8 pagineCase 1 Recruitment at Windsor Hospital Student Copy 1629976167334Baladaru Krishna PrasadNessuna valutazione finora
- Poster HCS EventDocumento1 paginaPoster HCS EventChris LlewellynNessuna valutazione finora
- NCLEX Practice Exam 21 (60 Questions)Documento36 pagineNCLEX Practice Exam 21 (60 Questions)Melodia Turqueza GandezaNessuna valutazione finora
- Evaluacion Valvula MitralDocumento9 pagineEvaluacion Valvula MitralRafaelDavidVillalbaRodriguezNessuna valutazione finora
- Coronary Steal SyndromeDocumento3 pagineCoronary Steal SyndromeEdward XiamNessuna valutazione finora
- AbbVie Corporate PresentationDocumento22 pagineAbbVie Corporate PresentationVarun ZotaNessuna valutazione finora
- Human Physiology 14Th Edition Fox Solutions Manual Full Chapter PDFDocumento37 pagineHuman Physiology 14Th Edition Fox Solutions Manual Full Chapter PDFletitiaestheru3hnxz100% (9)
- BSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemDocumento36 pagineBSC Nursing: Medical Surgical Nursing - I Unit V - Disorders of The Cardio Vascular SystemPoova RagavanNessuna valutazione finora
- Clasificacion Cardioaptias Ductus DependientesDocumento7 pagineClasificacion Cardioaptias Ductus DependientesdavidNessuna valutazione finora
- 4 Cardiovascular Alterations Diagnostic ProceduresDocumento3 pagine4 Cardiovascular Alterations Diagnostic ProceduresChristian Joseph OpianaNessuna valutazione finora
- Nclex ExamDocumento18 pagineNclex Examwaqas_xsNessuna valutazione finora
- 10.08.07 Cardiac Tamponade HaagDocumento16 pagine10.08.07 Cardiac Tamponade HaagFairuz Az ZabiedahNessuna valutazione finora
- Inventaris IGD 2022 TerbaruDocumento5 pagineInventaris IGD 2022 TerbaruEryNessuna valutazione finora
- CardiacArrhythmiasPathophysiology PDFDocumento1 paginaCardiacArrhythmiasPathophysiology PDFNeelam Raj ThakurNessuna valutazione finora
- Bifascicular Block Revealing Steinerts Myotonic DystrophyDocumento8 pagineBifascicular Block Revealing Steinerts Myotonic DystrophyIJAR JOURNALNessuna valutazione finora
- Econdary ABCD (Airway, Breathing, Circulation, Differential Diagnosis)Documento20 pagineEcondary ABCD (Airway, Breathing, Circulation, Differential Diagnosis)Nikol NataliaNessuna valutazione finora
- Anatomy Heart Homework (Due Mon. 3-9 1 or Tues. 3-10 2 /4) Vocabulary - Define The FollowingDocumento2 pagineAnatomy Heart Homework (Due Mon. 3-9 1 or Tues. 3-10 2 /4) Vocabulary - Define The FollowingKameron WardNessuna valutazione finora
- Rainer Kozlik-Feldmann, Georg Hansmann, Damien Bonnet, Dietmar Schranz, Christian Apitz, Ina Michel-BehnkeDocumento7 pagineRainer Kozlik-Feldmann, Georg Hansmann, Damien Bonnet, Dietmar Schranz, Christian Apitz, Ina Michel-BehnkeHerdinadNessuna valutazione finora
- Heart Dysrhythmias Cheat Sheet PDFDocumento5 pagineHeart Dysrhythmias Cheat Sheet PDFpcmundotNessuna valutazione finora
- Telemetry Recognition WorkbookDocumento29 pagineTelemetry Recognition WorkbookQueenNessuna valutazione finora
- Pathophysiology of Tetralogy of FallotDocumento2 paginePathophysiology of Tetralogy of Fallotsubham kumar100% (3)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (30)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (4)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (5)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainDa EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainValutazione: 4 su 5 stelle4/5 (95)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedValutazione: 4 su 5 stelle4/5 (61)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (59)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (45)