Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Outcome of End-Stage Renal Disease Patients
Caricato da
Muneeb SikanderCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Outcome of End-Stage Renal Disease Patients
Caricato da
Muneeb SikanderCopyright:
Formati disponibili
ORIGINAL ARTICLE
Outcome of End-Stage Renal Disease Patients
with Advanced Uremia and Acidemia
ABSTRACT
Iqbal Ur Rehman, Muhammad Khalid Idrees and Shoukat
Objective: To determine the outcome of End-Stage Renal Disease (ESRD) patients presenting with advanced uremia and
acidemia requiring hemodialysis and adverse events seen within 72 hours of admission.
Study Design: Cross-sectional study.
Place and Duration of Study: Sindh Institute of Urology and Transplantation, Karachi, Pakistan, from October 2010 to
March 2011.
Methodology: ESRD patients with advanced uremia and acidemia were included in the study. History, physical
examination, complete blood count, serum urea, creatinine, electrolytes, arterial blood gases analysis, and ultrasound of
kidneys were done in each patient. Adverse events and outcome were recorded for the next 72 hours. Data was analyzed
by SPSS version (10). Mean value and standard deviation of quantitative measurements were calculated and statistical
significance computed by t-test. A p-value 0.05 was taken as significant. Statistical significance of categorical variables
was determined by chi-square test.
Results: Out of the 194 ESRD patients (mean age 46.54 14.07 years), 28 (14%) expired and 166 (86%) survived within
72 hours of admission. Hypotension requiring inotropic support was the commonest adverse event observed in 40 (20.6%)
cases followed by fits in 31 (16%); and 25 (12.9%) patients required ventilatory support. Mortality was high in patients
above 50 years of age. There was no statistically significant difference between two genders regarding adverse events
and mortality.
Conclusion: The morbidity and mortality of patients with ESRD are serious concerns. Early referral of patients with ESRD,
before they develop severe acidosis, can prevent significant morbidity and mortality.
Key Words: Uremia. Acidosis. Dialysis. Inotropic. Mortality. Renal failure.
INTRODUCTION
The global burden of End-Stage Renal Disease (ESRD)
is rapidly rising and increasing number of patients is
entering in the pool of those on renal replacement
therapy (dialysis or transplant). Approximately 1.9 million
ESRD patients are undergoing hemodialysis worldwide.
Access to the facility of Renal Replacement Therapy
(RRT) correlates directly with socioeconomic development and regional income.1 The initiation of RRT in
developing world is restricted to fewer than a quarter of
ESRD patients.1 In 2010, only 58.9% of ESRD patients
received dialysis or had kidney transplantation. There
was disparity among different parts of the world
regarding access to renal replacement therapy, ranging
from less than 2% in most of sub-Saharan Africa to over
70% in high-income North America, high-income Asia
Pacific, and East Asia.2 The annual incidence of EndStage Renal Disease (ESRD) in Pakistan is estimated at
about 100 per million populations,3 and it is increasing
Department of Nephrology, Sindh Institute of Urology and
Transplantation (SIUT), Karachi.
Correspondence: Dr. Iqbal Ur Rehman, Department of
Nephrology, SIUT, Dewan Farooq Medical Complex,
Off M.A. Jinnah Road, Karachi.
E-mail: siutpakistan@gmail.com
Received: July 18, 2014; Accepted: October 16, 2015.
with each passing year. Only 10% of renal failure patients
receive renal replacement therapy.4
ESRD patients have a high mortality rate during the first
year of initiation of dialysis and at least 6% patients die
within first 90 days.5 Late nephrology referral has been
associated with adverse outcomes among ESRD
patients. In Pakistan, till few years ago, almost 100%
patients presented in emergency department with
uremia and required urgent dialysis.6 A recent survey
from Karachi (the largest metropolis of Pakistan) found
that 41% of family physicians did not know when to refer
a renal failure patient to nephrologist.7
In late referral patients with ESRD, metabolic acidosis is
present which is in most cases mild and partially or fully
compensated with pH > 7.2 and may not be life
threatening. However, more severe acidosis i.e. pH
< 7.2 can cause hemodynamic instability (hypotension,
cardiac arrhythmias),8 especially in patients with
advanced uremia. Metabolic acidosis, however, is not
the sole culprit for early mortality and morbidity whereas
other factors may also contribute.9 During the first year
of dialysis, mortality is lowest during the first month and
at peak during the second and third month.10 Analysis of
patients record from the authors institution revealed that
patients were received with advanced uremia and
metabolic acidosis requiring urgent hemodialysis via
temporary vascular access and frequently need
Journal of the College of Physicians and Surgeons Pakistan 2016, Vol. 26 (1): 31-35
31
Iqbal Ur Rehman, Muhammad Khalid Idrees and Shoukat
ventilatory and inotropic support with high (very early,
within 72 hours) mortality. As this type of presentation is
now rare in developed and Western countries, this
phenomenon is not reported in the literature and its
prognostic factors are not well studied.
There is lack of data regarding the outcome of patients
with advanced uremia and acidemia in our population.
This study was conducted to study the patients
demographics, occurrence of adverse events (fits,
hypotension requiring inotropic support and requirement
of ventilatory support) and their impact on outcome
(survival/expiry) of the patients who presented with
advanced uremia and acidemia.
METHODOLOGY
This cross-sectional study was conducted at Sindh
Institute of Urology and Transplantation (SIUT), Karachi,
Pakistan, from October 2010 to March 2011. Patients
between 15 - 60 years of age, presenting first time to
emergency department of SIUT having advanced
uremia (arbitrarily defined as serum urea level 250
mg/dl at first presentation at SIUT) and diagnosed ESRD
on the basis of clinical features, serum biochemistry and
ultrasound kidneys, were included in the study by
convenience sampling technique. Patients with acute or
chronic renal failure and those already on dialysis were
excluded from the study. The study was approved by the
Ethical Review Committee (ERC) of the institution.
Informed consent was obtained.
History was taken and physical examination done. Blood
samples for Complete Blood Count (CBC) and serum
biochemistry (serum urea, creatinine, electrolytes) sent
along with a separate heparinized sample of arterial
blood for pH, PO2, PCO2, O2 saturation and bicarbonate
measurement. Ultrasound of kidneys was done to see
the size of the kidneys and exclude obstruction.
Outcome of patients (whether the patient expired or
survived) was observed for the next 72 hours after
admission. Additionally, adverse events (fits, need of
mechanical ventilation and hypotension) were observed.
During this period, hemodialysis was done in supervision
of trained physician. The dialysis was of short duration
(90 - 120 minutes), with low flux hollow fibre
(polysulphone) dialyzer, without any anticoagulation
(saline flushes to prevent clotting of dialyzer),
bicarbonate dialysate, blood flow of 250 ml/minute and
dialysate flow of 500 ml/minute. Ultrafiltration was done
in patients having fluid overload. All the relevant
information (survival, death and adverse outcome) were
recorded on the proforma.
Data was entered and analyzed in statistical software
(SPSS version 10). Frequency and percentage were
computed for categorical (qualitative) variables like age
group, gender, outcome of end stage of renal disease
patients and adverse event. Mean and standard
deviation were computed for quantitative measurement
like age, temperature, hemoglobin, TLC, platelet,
32
potassium, sodium and pH. Statistical significance of
these variables was determined by t-test and value of p
equal or less than 0.05 was taken as statistically
significant. Similarly, the statistical significance of
categorical data was determined by chi-square test.
Stratification was done with regard to age, gender and
number of dialysis to observe the effect on outcomes.
RESULTS
This study included 194 ESRD patients (130 males and
64 females) having advanced uremia and acidemia. The
average age of the patients was 46.54 14.07 years and
most of the patients were above 50 years of age.
Patients who expired were older as compared to those
who survived (52.29 12.77 vs. 45.57 14.09 years) and
this difference was statistically significant (p= 0.019). All
the patients had fairly advanced uremia with a mean
serum urea of 349.04 77.6 mg/dl and mean serum
creatinine of 14.44 4.41 mg/dl respectively. About 40%
patients had hyperkalemia. The patients who expired
had lower pH (7.01 0.11) as compared to those who
survived (7.14 0.09) and this difference was statistically
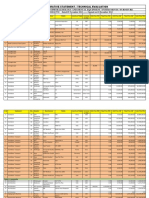
significant (p=0.0005). Table I shows the descriptive
statistics of study variables.
Table I: Descriptive statistics of study variables (n=194).
Variables
Mean SD
Max - Min
98.59 0.96
103 - 98
88.06 20.51
122 - 47
Platelet
246.78 139.95
716 - 5
Sodium
134.66 8.48
168 - 107
H.ion (nmol/L)
79.15 21.94
Creatinine mg/dL
14.44 4.41
Age (years)
Temperature*
Hemoglobin
Mean arterial pressure
TLC
Potassium**
pH
Urea mg/dl
46.54 14.07
7.87 1.82
15.48 8.23
5.41 1.35
65 - 15
11 - 3
56 - 1
9-2
7.12 0.13
7.29 - 6.84
349.04 77.6
594 - 251
*Out of 194 patients, 66 (34%) had temperature more than 100F
** Out of 194 patients, 78 (40.2%) had hyperkalemia
144 - 52
36.9 - 8.0
Hypotension requiring inotropic (vasopressor) support
was the commonest adverse event that was observed in
40 (20.6%) patients followed by fits (seizures) in 31
(16%) patients while 25 (12.9%) patients required
ventilatory support. Fits and ventilatory support were
more common in patients below 30 years of age while
hypotension was observed in patients above 50 years of
age. Frequency of fits and ventilatory support was nearly
same in male and female (p=0.46 and p=0.90,
respectively) while hypotension was more common in
females than males (28.1% vs. 16.9%); but this
difference did not reach statistical significance (p=0.07).
Frequency of hypotension and ventilatory support was
high in those cases who had only one session of dialysis
as compared to those who required 2 and 3 dialysis
sessions during the period of 72 hours (p=0.001 and
0.0001 respectively) while there was no statistically
Journal of the College of Physicians and Surgeons Pakistan 2016, Vol. 26 (1): 31-35
Outcome of ESRD with advanced uremia and acidemia
significant difference in case of fits (p=0.172). These
patients had more severe metabolic acidosis and
consequent highest mortality as shown in Table II.
Dialysis prescription varied very little from patient to
patient as all the patients had short duration dialysis and
dialysate flow (500 ml/minute) whereas dialysate
compositions (prepared in the institution in bulk) were
fixed and dialyzer used was of the same size (1.4 m2) for
all the patients.
Fourteen percent (28/194) patients expired and 86%
(166/194) survived within 72 hours after admission.
Mortality/expiry rate was highest (20.8%) among those
above 50 years of age while it was about 8% (8 out of
98) in those below 50 years of age. Mortality was
statistically significantly higher in those above 50 years
of age as compared to those below 50 years (p=0.029).
There was no difference in both genders regarding
mortality (p=0.918). Similarly, mortality/expiry rate was
100% in those cases who had only one dialysis session.
Frequencies of adverse events and mortality are
summarized in Table III.
Table II: Comparison of characteristics between survived and expired
patients.
Variables
Survive group
Expired group
p-value
111 (66.9%)
19 (67.9%)
0.918
45.57 14.09
52.29 12.77
99.16 1.60
0.001*
(mmHg)
91.62 18.25
66.94 20.71
0.0005*
TLC (1000/mm3)
14.63 7.39
20.46 11
0.0005*
376.64 92.67
0.042
5.89 2.03
0.002*
Gender
Male
Female
Age (years)
Temperature (F)
Mean arterial pressure
Hemoglobin (gm/dl)
Platelets (100,000/mm3)
Urea (mg/dl)
Creatinine (mg/dl)
Bicarbonate (mmol/L)
PCO2
(n=166)
55 (33.1%)
98.49 0.78
7.88 1.83
(n=28)
09 (32.1%)
7.76 1.79
247.21 136.7
244.25 147.68
14.45 4.51
14.04 4.07
344.39 74.09
7.62 2.85
14.86 5.31
0.0005*
H ion (nmol/L)
75.32 19.15
101.82 23.98
Fits
Hypotension
Ventilatory support
* Significant
21 (12.7%)
21 (12.7%)
10 (6%)
Table III: Adverse events and mortality.
Age groups
30 years
31 to 50 years
> 50 years
0.649
7.01 0.11
134.18 8.54
Adverse event
0.917
0.0005*
134.76 8.49
7.14 0.09
0.734
21.93 13.82
Sodium (mEq/L)
pH
0.019
10 (35.7%)
19 (67.9%)
15 (53.6%)
Number
36
62
0.74
0.0005*
0.002*
0.0001*
0.0001*
DISCUSSION
The authors specifically studied outcome of uremic
patients who were acidotic and in need of emergency
dialysis, which is a common scenario in Pakistan due to
late diagnosis or referral. Most of those patients, who
have an uneventful course within few days after starting
dialysis, usually do well subsequently. The total number
of patients with a span of 6 months, suggests that this is
still a frequent mode of presentation in Pakistan. The
average age of these patients (46.54 14.07 years) is
much less than that reported from USA11 but close to
that in other South Asian countries.12 The number of
males was almost twice that of females in this study.
This is contrary to the finding from community based
study from Karachi13 which did not find gender
difference in occurrence of kidney disease among
general population. The lesser number of females in this
study is probably due to gender bias and social
deprivation of females.
This study included patients with severe acidosis i.e.
pH < 7.3. The patients who eventfully expired had more
severe acidemia compared to those who survived.
Acidosis of such severity may lead to adverse
hemodynamic effects such as arteriolar dilatation and
depression of myocardial contractility.8 In an
experimental study, the effect of metabolic acidosis
induced by infusion of hydrochloric acid in pigs was
studied which showed that lowering of pH to 7.1 resulted
in diminished cardiac contractility and increased the
ventricular stroke work per minute.14 Numerous studies
on patients with lactic acidosis in critical care setting
have highlighted the adverse effects of profound
acidemia.15 The authors were unable to find any study
where effect of such profound metabolic acidosis in
uremic patients has been studied.
It is difficult to compare these patients (whose acidosis
is rapidly corrected by dialysis) with non-uremic patients
with lactic acidosis. More than 40% patients had
hyperkalemia but it had no effect on mortality. It is
probably because of the rapid removal of potassium in
process of hemodialysis. Patients who expired had
higher temperature and higher TLC as compared to
those who survived. This could be due to presence of
some unrecognized infection (such as UTI) or result
from systemic inflammation due to metabolic acidosis.
Patients with higher PCO2 (respiratory acidosis) had
Fits
7 (19.5%)
11 (17.8%)
Hypotension
6 (16.7%)
7 (11.3%)
Ventilatory support
Expired
5 (13.8%)
3 (8.3%)
7 (11.3%)
5 (8.1%)
96
13 (13.5%)
27 (28.1%)
13 (13.5%)
20 (20.8%)
Males
130
19 (14.6%)
22 (16.9%)
17 (13.1%)
19 (14.6%)
Total
31 (16%)
40 (20.6%)
25 (12.9%)
28 (14%)
Number of adverse events
Females
64
12 (18.8%)
Journal of the College of Physicians and Surgeons Pakistan 2016, Vol. 26 (1): 31-35
18 (28.1%)
8 (12.5%)
9 (14.1%)
33
Iqbal Ur Rehman, Muhammad Khalid Idrees and Shoukat
higher mortality. Patients with pure metabolic acidosis
have lower PCO2 due to respiratory compensation but
exhaustion of respiratory muscles leads to concomitant
respiratory acidosis (more pronounced among diabetic
CKD patients) and consequent higher morbidity and
mortality.16
Hypotension was the commonest adverse event
observed in 20.6% cases followed by fits (16%) and
12.9% patients required ventilator support. High
mortality rate (60%) observed in patients who were on
ventilator followed by hypotension (47.5%) and fits
(2.3%). Seizures are not uncommon in patients with
advanced uremia on presentation and are multi-factorial
in causation. Seizures in uremic patients can be a
manifestation of uremia, metabolic derangements or the
treatment of these derangements.17 Bergen and
colleagues reported the incidence of seizures (fits) of
approximately 10% in patients with chronic renal
failure.18 The lower frequency of seizures among our
study participants may be due to short period of
observation (72 hours).
Mechanical ventilation was required in 12.9% patients
which is less than 26% as reported by Rocha19 among
maintenance dialysis patients admitted in ICU. Patients
with advanced uremia often have pulmonary edema,
inability to clear upper airways and exhaustion due to
respiratory muscle fatigue. Similarly, 20.6% of our
patients had hypotension and required inotropic support
compared to 24% as reported by Rocha.19 The
difference in the two study populations is that there was
high proportion of patients with sepsis in the study of
Rocha while these patients had severe metabolic
acidosis.
The outcome of ESRD patients with advanced uremia
was quite dismal in this study. Fourteen percent patients
expired within 72 hours of admission. This is much
higher than the 6% mortality during first 90 days of start
of dialysis in USA.5 In Canada,20 early 90-day mortality
after initiation of dialysis was upto 34.7% of one year
mortality. However, there is wide variation in patient
mortality in different parts of the world. DOPPS found
that one-year mortality rates were 6.6% in Japan, 15.6%
in Europe and 21.7% in the USA and variability in
demographic and co-morbid conditions at inception of
dialysis could explain only part of the differences in
mortality rate between these countries.21 It has been
observed that both cardiovascular and noncardiovascular mortality risk factors are equally
increased among dialysis patients and should be
focused.22
In this study, frequency of expired patients was high in
above 50 years of age. This is well known phenomenon
that mortality increases with increasing age.20 Mortality
rate was similar in male and female patients in this study.
Gender difference has been reported in the survival of
34
new ESRD patients. Bloembergen et al. found that
males receiving chronic dialysis had a 22% higher
mortality than females, mostly because of excess risk of
acute myocardial infarction and malignancies.23
However, another study from European cohort showed
that young and diabetic women starting dialysis had
higher non-cardiovascular mortality risk than men while
females of 45 years old and above had lower
cardiovascular mortality than men.24 The authors did not
find such gender difference in this study. This may be
because of smaller number of females. Higher
frequency of hypotension, need of ventilatory support
and 100% mortality among patients, who survived to
have only one dialysis session, reflects that these
patients were more seriously sick. The dialysis
prescription was more or less the same among all the
patients and it is not possible to judge the effect of
dialysis on survival or mortality in this small single centre
study.
This study is, to the best of authors' knowledge, the first
of its kind from this part of the world which highlights the
high mortality rate among ESRD patients presenting
with advanced uremia and metabolic acidosis/acidemia
during first 72 hours of admission. It highlights the
importance of accurate reporting of events during initial
days of start of dialysis. Early referral to nephrologist
and attendance of pre-dialysis clinics may facilitate the
avoidance of central venous catheters, timely creation of
AV fistula, correction of anemia, mineral bone
metabolism and malnutrition, which ultimately improve
survival on dialysis.25
It is a single center study and observation period was
only 3 days, so co-morbid conditions other than ESRD
could affect the outcome and adverse events.
CONCLUSION
The morbidity and mortality of patients with ESRD are
serious concerns for patients presenting late with
advanced uremia and severe metabolic acidosis. Early
referral of patients, with ESRD before they develop
severe acidosis, will prevent significant morbidity and
mortality.
REFERENCES
1. Anand S, Bitton A, Gaziano T. The gap between estimated
incidence of end-stage renal disease and use of therapy. PLoS
ONE 2013; 8:e72860. Available at: http://www.plosone.org/
article/fetchObject.action?uri=info%3Adoi%2F10.1371%2Fjou
rnal.pone.0072860&representation=PDF. Accessed on April
18, 2014.
2. Wulf SK, Naghavi M. End-stage renal disease: unmet
treatment needs across the globe. Lancet 2013; 381:S150.
3. Rizvi SA, Naqvi SAA. Renal replacement therapy in Pakistan.
Saudi J Kid Dis Transpl 1996; 7:404-8.
4. Wasti AZ, Fatima N, Ashiq A, Khalid E. Cardio-renal profiling
with hs-CRP and its implications as a diagnostic tool in chronic
kidney disease patients. Int Sci Invest J 2013; 2:1-6.
Journal of the College of Physicians and Surgeons Pakistan 2016, Vol. 26 (1): 31-35
Outcome of ESRD with advanced uremia and acidemia
5. Soucie JM, McClellan WM. Early death in dialysis patients: risk
factors and impact on incidence and mortality rates. J Am Soc
Nephrol 1996; 7:2169-75.
6. Anees M, Mumtaz A, Nazir M, Ibrahim M, Rizwan SM, Kausar
T. Referral pattern of hemodialysis patients to nephrologists.
J Coll Physicians Surg Pak 2007; 17:671-4.
7. Yaqub S, Kashif W, Raza MQ, Aaqil H, Shahab A, Chaudhary
MA, et al. General practitioners' knowledge and approach to
chronic kidney disease in Karachi, Pakistan. Indian J Nephrol
2013; 23:184-90.
8. Kraut JA, Madias NE. Metabolic acidosis: pathophysiology,
diagnosis and management. Nat Rev Nephrol 2010; 6:274-85.
9. Movilli E, Bossini N, Viola BF, Camerini C, Cancarini GC, Feller P,
et al. Evidence for an independent role of metabolic acidosis
on nutritional status in haemodialysis patients. Nephrol Dial
Transplant 1998; 13:674-8.
10. Collins AJ, Foley RN, Gilbertson DT, Chen SC. The state of
chronic kidney disease, ESRD, and morbidity and mortality in
the first year of dialysis. Clin J Am Soc Nephrol 2009; 4:S5-11.
11. Soucie JM, McClellan WM. Early death in dialysis patients: risk
factors and impact on incidence and mortality rates. J Am Soc
Nephrol 1996; 7:2169-75.
12. Modi GK, Jha V. The incidence of end-stage renal disease in
India: a population-based study. Kidney Int 2006; 70:2131-3.
13. Alam A, Amanullah F, Baig-Ansari N, Lotia-Farrukh I, Khan FS.
Prevalence and risk factors of kidney disease in urban Karachi:
baseline findings from a community cohort study. BMC Res
Notes 2014; 7:179.
14. Stengl M, Ledvinova L, Chvojka J, Benes J, Jarkovska D,
Holas J, et al. Effects of clinically relevant acute hypercapnic
and metabolic acidosis on the cardiovascular system: an
experimental porcine study. Crit Care 2013; 17:R303.
15. Kimmoun A, Novy E, Auchet T, Ducrocq N, Levy B.
Hemodynamic consequences of severe lactic acidosis in
shock states: from bench to bedside. Crit Care 2015; 19:175.
16. Ikegaya N, Yonemura K, Suzuki T, Kato-Ohishi H, Taminato T,
Hishida A. Impairment of ventilatory response to metabolic
acidosis in insulin-dependent diabetic patients with advanced
nephropathy. Ren Fail 1999; 21:495-8.
17. de Lacerda GCB. Treating seizures in renal and hepatic failure.
J Epilepsy Clin Neurophysiol 2008; 14:46-50.
18. Bergen DC, Ristanovic R, Gorelick PB, Kathipalia S. Seizures
and renal failures. Int J Artif Organs 1994; 17:247-51.
19. Rocha E, Soares M, Valente C, Nogueira L, Jr HB, Godinho M,
et al. outcomes of critically ill patients with acute kidney injury
and end-stage renal disease requiring renal replacement
therapy: a case control study. Nephrol Dial Transplant 2009;
24:1925-30.
20. McQuillan R, Trpeski L, Fenton S, Lok CE. Modifiable risk
factors for early mortality on hemodialysis. Int J Nephrol 2012;
2012:435736.
21. Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T,
Andreucci VE, et al. Association of comorbid conditions and
mortality in hemodialysis patients in Europe, Japan, and the
United States: the Dialysis Outcomes and Practice Patterns
Study (DOPPS). J Am Soc Nephrol 2003; 14:3270-7.
22. de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas
LM, Ansell D, et al. Cardiovascular and non-cardiovascular
mortality among patients starting dialysis. JAMA 2009; 302:
1782-9.
23. Bloembergen W, Port FK, Mauger EA, Wolfe RA. Causes of
death in dialysis patients: racial and gender differences. J Am
Soc Nephrol 1994; 5:1231-42.
24. Carrero JJ, de Jager DJ, Verduijn M, Ravani P, De Meester J,
Heaf JG, et al. Cardiovascular and non-cardiovascular
mortality among men and women starting dialysis. Clin J Am
Soc Nephrol 2011; 6:1722-30.
25. Garcia-Garcia G, Briseo-Rentera G, Luqun-Arellan VH, Gao Z,
Gill J, Tonelli M. Survival among patients with kidney failure in
Jalisco, Mexico. J Am Soc Nephrol 2007; 18:1922-7.
Journal of the College of Physicians and Surgeons Pakistan 2016, Vol. 26 (1): 31-35
35
Potrebbero piacerti anche
- Handcuffs For The Guilty - Media Capture and Government AccountabilityDocumento20 pagineHandcuffs For The Guilty - Media Capture and Government AccountabilityMuneeb SikanderNessuna valutazione finora
- Cost Analysis of Tumor Downsizing For Hepatocellular Carcinoma IndiaDocumento3 pagineCost Analysis of Tumor Downsizing For Hepatocellular Carcinoma IndiaMuneeb SikanderNessuna valutazione finora
- 2002 The Political Economy of Government Responsiveness Theory and Evidence From India PDFDocumento38 pagine2002 The Political Economy of Government Responsiveness Theory and Evidence From India PDFMuneeb SikanderNessuna valutazione finora
- 2015 - Referrals Peer Screening and Enforcement in Consumer CreditDocumento31 pagine2015 - Referrals Peer Screening and Enforcement in Consumer CreditMuneeb SikanderNessuna valutazione finora
- Short Term Donor Outcomes After HepatectomyDocumento5 pagineShort Term Donor Outcomes After HepatectomyMuneeb SikanderNessuna valutazione finora
- Comparitive Statement T121210DHUS-20130213Documento29 pagineComparitive Statement T121210DHUS-20130213Muneeb SikanderNessuna valutazione finora
- Human Nature - Comparison of Apollolian and Dionysian DualitiesDocumento52 pagineHuman Nature - Comparison of Apollolian and Dionysian DualitiesMuneeb SikanderNessuna valutazione finora
- 2014 - Underinvestment in A Profitable Technology - Seasonal Migration in BangladeshDocumento79 pagine2014 - Underinvestment in A Profitable Technology - Seasonal Migration in BangladeshMuneeb SikanderNessuna valutazione finora
- 1982 Gecas - The Self-Concept. Conceptul de Autoeficacitate. Autoeficacitatea PerceputaDocumento34 pagine1982 Gecas - The Self-Concept. Conceptul de Autoeficacitate. Autoeficacitatea PerceputavoicekNessuna valutazione finora
- Roland Berger Tab How To Do Business in Iran 20151125Documento12 pagineRoland Berger Tab How To Do Business in Iran 20151125Muneeb SikanderNessuna valutazione finora
- 1949 Heidegger - The Question Concerning Technology, and Other EssaysDocumento222 pagine1949 Heidegger - The Question Concerning Technology, and Other EssaysJope Guevara100% (5)
- Textbook: Readings:: Cubs MSC Finance 1999-2000 Asset Management: Lecture 3Documento13 pagineTextbook: Readings:: Cubs MSC Finance 1999-2000 Asset Management: Lecture 3Atif SaeedNessuna valutazione finora
- ChangeManagement EN PDFDocumento32 pagineChangeManagement EN PDFMuneeb SikanderNessuna valutazione finora
- 2016 Hepatitis C Virus Prevalence and Genotype Distribution in Pakistan Comprehensive Review of Recent DataDocumento19 pagine2016 Hepatitis C Virus Prevalence and Genotype Distribution in Pakistan Comprehensive Review of Recent DataMuneeb SikanderNessuna valutazione finora
- Are We Ready For A New Epidemic of Under Recognized Liver Disease in South AsiaDocumento5 pagineAre We Ready For A New Epidemic of Under Recognized Liver Disease in South AsiaMuneeb SikanderNessuna valutazione finora
- Hepatocellular Carcinoma in PakistanDocumento2 pagineHepatocellular Carcinoma in PakistanMuneeb SikanderNessuna valutazione finora
- Math May 2008 MS C3Documento9 pagineMath May 2008 MS C3dylandonNessuna valutazione finora
- LBO DCF ModelDocumento38 pagineLBO DCF ModelMuneeb SikanderNessuna valutazione finora
- Import Substitution Industrialization in Latin AmericaDocumento29 pagineImport Substitution Industrialization in Latin AmericaMuneeb SikanderNessuna valutazione finora
- Edexcel GCE: Core Mathematics C2Documento20 pagineEdexcel GCE: Core Mathematics C2Muneeb SikanderNessuna valutazione finora
- Dashboard Reporting TemplateDocumento8 pagineDashboard Reporting TemplateMuneeb SikanderNessuna valutazione finora
- Math May 2008 MS C2Documento10 pagineMath May 2008 MS C2dylandonNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Atty. Represented Conflicting Interests in Property CaseDocumento35 pagineAtty. Represented Conflicting Interests in Property CaseStella C. AtienzaNessuna valutazione finora
- All Glory Book-1Documento187 pagineAll Glory Book-1fredkayf100% (1)
- Application for Test Engineer PositionDocumento3 pagineApplication for Test Engineer PositionAsz WaNieNessuna valutazione finora
- Unit 8Documento2 pagineUnit 8The Four QueensNessuna valutazione finora
- Flowera, Fruits and SeedsDocumento66 pagineFlowera, Fruits and SeedsNikkaMontil100% (1)
- Year 9 Autumn 1 2018Documento55 pagineYear 9 Autumn 1 2018andyedwards73Nessuna valutazione finora
- Life Cycle of A BirdDocumento3 pagineLife Cycle of A BirdMary Grace YañezNessuna valutazione finora
- Description Text About Cathedral Church Jakarta Brian Evan X MIPA 2Documento2 pagineDescription Text About Cathedral Church Jakarta Brian Evan X MIPA 2Brian KristantoNessuna valutazione finora
- Nokia CaseDocumento28 pagineNokia CaseErykah Faith PerezNessuna valutazione finora
- Professional Teaching ResumeDocumento2 pagineProfessional Teaching Resumeapi-535361896Nessuna valutazione finora
- English 7 1st Lesson Plan For 2nd QuarterDocumento4 pagineEnglish 7 1st Lesson Plan For 2nd QuarterDiane LeonesNessuna valutazione finora
- The CIA Tavistock Institute and The GlobalDocumento34 pagineThe CIA Tavistock Institute and The GlobalAnton Crellen100% (4)
- MRI BRAIN FINAL DR Shamol PDFDocumento306 pagineMRI BRAIN FINAL DR Shamol PDFDrSunil Kumar DasNessuna valutazione finora
- Bellak Tat Sheet2pdfDocumento17 pagineBellak Tat Sheet2pdfTalala Usman100% (3)
- Ebook Torrance (Dalam Stanberg) - 1-200 PDFDocumento200 pagineEbook Torrance (Dalam Stanberg) - 1-200 PDFNisrina NurfajriantiNessuna valutazione finora
- Vaishali Ancient City Archaeological SiteDocumento31 pagineVaishali Ancient City Archaeological SiteVipul RajputNessuna valutazione finora
- Sale DeedDocumento3 pagineSale DeedGaurav Babbar0% (1)
- Supplement BDocumento65 pagineSupplement BAdnan AsifNessuna valutazione finora
- English Proficiency Test (EPT) Reviewer With Answers - Part 1 - Online E LearnDocumento4 pagineEnglish Proficiency Test (EPT) Reviewer With Answers - Part 1 - Online E LearnMary Joy OlitoquitNessuna valutazione finora
- Demerger Impact on Shareholder WealthDocumento16 pagineDemerger Impact on Shareholder WealthDarshan ShahNessuna valutazione finora
- ID Kajian Hukum Perjanjian Perkawinan Di Kalangan Wni Islam Studi Di Kota Medan PDFDocumento17 pagineID Kajian Hukum Perjanjian Perkawinan Di Kalangan Wni Islam Studi Di Kota Medan PDFsabila azilaNessuna valutazione finora
- Lecture 22 NDocumento6 pagineLecture 22 Ncau toanNessuna valutazione finora
- COOKERY Grade 9 (Q1-W1)Documento2 pagineCOOKERY Grade 9 (Q1-W1)Xian James G. YapNessuna valutazione finora
- Casalla vs. PeopleDocumento2 pagineCasalla vs. PeopleJoan Eunise FernandezNessuna valutazione finora
- 05 Mesina v. PeopleDocumento7 pagine05 Mesina v. PeopleJason ToddNessuna valutazione finora
- Bobby Joe Public NoticeDocumento3 pagineBobby Joe Public NoticeUpscale International InvestmentsNessuna valutazione finora
- CS201 Midterm Solved MCQs With ReferenceDocumento4 pagineCS201 Midterm Solved MCQs With Referencegenome companyNessuna valutazione finora
- Pope Francis' Call to Protect Human Dignity and the EnvironmentDocumento5 paginePope Francis' Call to Protect Human Dignity and the EnvironmentJulie Ann BorneoNessuna valutazione finora
- (PC) Brian Barlow v. California Dept. of Corrections Et Al - Document No. 4Documento2 pagine(PC) Brian Barlow v. California Dept. of Corrections Et Al - Document No. 4Justia.comNessuna valutazione finora