Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Vulnerable Child Syndrome and Its Variants.
Caricato da
Leila MargaridaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Vulnerable Child Syndrome and Its Variants.
Caricato da
Leila MargaridaCopyright:
Formati disponibili
Vulnerable
Its Variants
Morris
Green,
Child
Syndrome
MD*
In 1 964, Solnit
and Green1
described
a vulnerable
child syndrome
characterized,
among
other
clinical
manifestations,
by difficulty
with separation,
over protectiveness,
bodily
overconcerns,
and
school
underachievement.
This
constellation
of
symptoms
has been repeatedly
observed
by us and by others
in the
following
groups
and
of
children
(Table
1).1_3
1 Those who had experienced
a
serious
illness
in which
the parent
believed
the child would
die. Even
after full recovery,
the parent, almost
invariably
the mother,
endures
the
continuing
or recurrent
undisclosed
fear that the child is unusually
vulnerable to serious illness or accident
and
is destined
to die prematurely.
2. Those
who represent
for the
parent a significant
person
from the
past who died prematurely,
eg, a
brother of the mother who at 7 years
of age died suddenly
because
of meningococcemia
or a previous
child of
the parent who died with the sudden
infant death syndrome.
3. Those
whose
life or whose
mothers
life was at risk during pregnancy or delivery,
eg, because
of an
abruptio
placenta.
4. Those whose mothers
were informed
by the physician
during their
pregnancy that the fetus might die in
utero.
5. Those
whose
mothers
have a
history
of a threatened
miscarriage,
multiple spontaneous
abortions, or a
stillbirth.
That relativelyfew children in these
five groups
develop
the manifestations of the vulnerable
child syndrome
may be the result of considerable
individual
differences
in the way parents adapt to the threatened
loss of
a child, predisposing
parental
experiences,
protective
mechanisms,
and
the preventive
efforts
of physicians,
nurses, and social workers.
Risk factors include,
for example,
older par.
* Perry
W. Lesh Professor
and Chairman,
Department
of Pediatrics,
Indiana
University
School of Medicine,
Indianapolis,
IN 46223.
ents who have had many years of
infertility
or the young single mother
without
supportive
relatives
or
friends. Protective
factors include the
mothers
ready access
to her sick
baby or child during
the serious
illness, thoughtful
explanations
of the
infants
status communicated
as optimistically
as possible
by the physician, and repeated
opportunities
during the illness for the mother to share
her fears, worries,
and feelings
with
empathetic
health professionals
who
understand
the value of discussing
these issues.
Such preventive
interventions
are now more widely
provided than they were two decades
ago.
CLINICAL
EDUCATIONAL
16. The pediatrician
should be able
to differentiate
among the various
conditions
possibly responsible
for
a child who is said to be hyperactive, has regressed
in toilet training, and does not wish to be separated from his or her mother, distinguishing
among attention
deficit
disorder with hyperactivity;
adjustment reaction due to mother working outside the home, divorce, matemal depression,
birth of a sibling,
or family illness; conduct disorder;
sexual
abuse
or vulnerable
child
syndrome;
idiosyncratic
drug reaction; or neurodegenerative
disorder, and develop
an appropriate
plan for management
(Topics,
86/
87).
The physician
should
be able to
support the parents
of a critically
ill newborn.
If the baby recovers,
the physician
should
be able to
counsel the family so as to prevent
the vulnerable
child syndrome.
If
the baby dies, the physician
should
be able to help the parents
know
what to expect
in terms of reaction
to their loss and how to master
their grief reactions.
MANIFESTATIONS
The
complex
condition
encompassed by the term vulnerable
child
syndrome
cannot
be characterized
simply, because
of the many factors
that influence
its manifestations
and
the variability
of its symptomatology.
The following
clinical
features
are
commonly
but not invariably
present
in the fully expressed
syndrome
(Table 2). Variants
of the syndrome
will
be discussed
later.
1 . Pathologic
separation
difficulties
occur in which the mother
and child
rarely or never separate.
When separation
is unavoidable,
eg, during
hospitalization
of the mother,
the
child may reluctantly
be entrusted
to
a close relative,
such as the grandmother,
but other
baby-sitters
are
rarely used. Although
seemingly
unrecognized
by the parent,
the child
regularly
senses
and is made fearful
by the mothers
expectation
of his
vulnerability.
This concern
is communicated
in many subtle ways but
mainly through
the mothers
moods
and in her way of limiting the childs
autonomy
and independence
with inhibiting reservations.
Such apprehension can also be observed
in the
mothers way of experiencing
separation from the child. If the separation
anxiety
is not resolved
earlier,
the
child may resist school attendance.
2. Sleep problems
are common,
and the mother
may come
to the
pediatrics
in review
OBJECTIVES
physician
in near exhaustion.
The
child often sleeps in the parents
bed
or in a crib placed next to the mother
and in her direct
line of vision.
In
addition,
she may hover about
the
child
during
naps.
Although
the
mother
may report
that the baby
does not sleep well, it is the parent
who awakens
several
times a night
to check on the child. In doing so,
she unwittingly
manages
to awaken
the baby, in that way reassuring
herself that he or she is alive. The mother
is simply
unable
to sleep at night
unless she believes
her baby is safe
and sound.
3. In many cases,
the parent
is
unable to set age-appropriate
limits,
with the result that the child is disobedient,
argumentative,
and uncoop#{149}
vol. 8 no. 3 september
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
1986
PIR
75
Vulnerable
Child
Syndrome
mind,
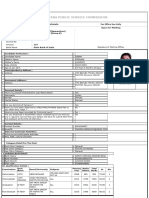
TABLE
1.
At-Risk Situationsfor
the Vulnerable Child Syndrome
TABLE
1. Recovery
from an illness in
which the parent thought
the
child would die
2. Premature death of a person
significant to the parent
3. The life of the mother or the
fetus was at risk during the
pregnancy
4. The mother was told that her
baby might die in utero
Child
5. A mother
taneous
with a history
abortions
2.
Clinical
Manifestations
of the Vulnerable
Syndrome
1.
2.
3.
4.
5.
Pathologic separation problems
Sleep problems
Discipline problems
Overprotectivness
Child
physically
abusive
to
mother
6. Hyperactivity
7. Excessive
maternal
concern
about child health; overuse of
medical care services
8. School underachievement
of spon-
or stillbirth
ie,
services
are
highly
characteristic
of
the vulnerable
child syndrome.
The
powerful
anticipatory
grief reaction
evoked when a parent suddenly
confronts the possible
death of the child
often is rekindled
with later illnesses,
no matter
how minor. Held hostage
by this emotional
ghost from the past,
PIR
76
pediatrics
in review
#{149}
Yudkin6
termed
the
this
this
unabetheir
pre-
mature
death,
no intimation
of this
association
is given in a routine
past
medical
history.
It is only in answer
to such questions
as, You seem very
worried
about
Mark.
Could
you be a
little more specific about that worry?
Has Mark ever been seriously
ill?
How sick was he then?
Was he
seriously
tell you
erative. This striking
lack of discipline
or out-of-control
behavior
may be
present
only in the mothers
presence, an observation
that contributes
even further
to her sense of ineptitude. The parent
seems to lose her
parenting
presence,
that nonverbal
projection
of an effective
mother analogous to command
presence
in the
armed services.
As a result,
she is
unable to provide
the certainty,
confidence,
and security
that young children need.
4. The overprotective,
overindulgent, oversolicitous,
and over vigilant
parent,
perceiving
the
child
as
younger
than he or she actually
is,
may keep him or her in a play pen
excessively,
confine
him or her in a
fenced
yard beyond
the usual age,
and forbid bicycling or contact sports.
A mothers
expectation
of her infants
development
may be significantly
influenced
by her estimate
of him or
her as sickly or vulnerable.45
5. The child may physically
abuse
the mother,
even publicly.
Although
resentful
and embarrassed
as the
child hits, bites, scratches,
or kicks
her, she simply cannot control
him.
6. Many of these children
are described
by the parent
as hyperactive.
7. Excessive
concerns
about the
childs health and overuse
of medical
what
second
diagnosis
or Why is
child being brought
to you at
moment?
Because
parents
are usually
ware that a relationship
exists
tween the childs symptoms
and
long-standing
fear of the childs
ill?
during
What
Marks
the mother
thus is overconcerned
about minor respiratory
infections,
fever, diarrhea,
limb pains and abdominal pain, or headache.
She worries
inordinately
about the childs
paleness, sickly appearance,
easy fatigabihity,
circles
under
his eyes,
blueness
when
crying,
breathing
too fast, and poor resistence.
Because of the mothers
inability to differentiate
a self-limited
from a poten-
you feel from
tially
certainty,
her nausea
and feeling
of
emptiness,
and her repeated
prayers
for her childs
recovery.
She is clearly
serious
illness,
she
brings
this
special child frequently
to physicians
and emergency
rooms so as not to
be too late. Although
her judgement
about the need of her other children
for medical
care may be good, that
sense seems to have been lost with
the vulnerable
child.
8. Although
school
underachievement and learning
difficulties
have a
more
subtle
association
with
the
childs fear of a premature
death, this
relationship
should
be kept in mind
as one
possible
explanation
for
school failure because
of the vulnerable childs inability to concentrate
on
learning.
DIAGNOSIS
The
vulnerable
child
syndrome
should be considered
as a diagnostic
possibility
when the clinical manifestations listed above are encountered,
when the reason for a visit is unclear,
when a mothers
concerns
about her
child seem greater
than warranted,
when a child has been seen the same
day by other
physicians,
when
a
mother
expresses
dissatisfaction
with previous doctors, and when she
seems to have something
else on her
vol. 8 no. 3 september
nurses
told
what
did the doctor
illness?
Did
you
the doctor
or
from
sensed that your child
In response
to such
mother
may
recall
or the
what
you
might die?
questions,
the
vividly
and
with
considerable
emotion
the apprehension and anxiety
that engulfed
her
during
the childs
illness.
She may
describe
in minute-by-minute
or hourby-hour
detail
what
the doctor
or
nurse said, her own bewildering
un-
relieved
at long
cret fear.
last to share
her se-
MANAGEMENT
Characteristically,
such
are
their
special,
not
other
the
parents
vulnerable
experiencing
children.
problems
Once
of
children
the
with
vulner-
able child syndrome
is recognized,
the physicians
clear statement,
following
a thorough
history
and conspicuously
meticulous
physical
examination,
that
the
child
is absolutely
physically
sound represents
the first
step in management.
The next therapeutic
measure
is to help the parents understand
and accept
the notion that the symptoms
represent
a
sequela
of the acute, life-threatening
illness or one of the other
experiences noted above that predispose
to this syndrome.
This may be facilitated by a statement
such as, Mothers who have had the horrible
experience
of believing
that their child
might die during an illness often continue to fear that he will die prematurely, even many years after his re-
1986
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
BEHAVIORAL
covery.
I would
guess
that youve
had
similar
fears about
Johnny.
If the parents
are able
to
and
use
assurance
that
their
the
physicians
child
is physically
accept
healthy
and if they are able to understand
the
causal relationship
between
present
behavior
and past experience,
the
problem
can largely
be managed
in
only one visit; on the other hand, if
the
visit
aged
hurried
of a vulnerable
in a cursory,
fashion
child
is man-
disinterested,
or the
and
parents
under-
lying anxiety
is not addressed,
the
mother
may leave the office
frustrated,
dissatisfied,
and
privately
angry.
Once the mutual reenforcement
of
anxiety and symptoms
is attenuated,
the parents
are able to set disciplinary
limits,
discontinue
treating
the child
as if he or she were
their
younger,
overprotectiveness,
reduce
initiate
de-
velopmentally
appropriate
sleeping
practices,
deal more effectively
with
separation,
judge
more
accurately
the seriousness
of the childs symptoms,
and
stop
recalling
to the
child
or to others
in the childs
hearing
the time that they almost
lost him
[her].
Not unexpectedly,
some pa
rental anxiety may remain or be reactivated
at times of illness; however,
the pediatrician
can readily help the
parents
understand
and tolerate
that
degree of discomfort.
PREVENTION
tive purpose
is served
by reminding
the parents of the seriousness
of the
illness. Such retrospective
comments
as, If he [she] had gotten
here an
hour
later,
we wouldnt
have
been
able to save him [her], or I thought
sure he [she] would die, are potentially harmful.
Because
it is not always
possible
to identify
specifically
which families
are at risk of developing
the vulnerable child syndrome,
the physicians
debriefing
of the parents
just before
the discharge
of an infant or child who
has been seriously
ill should include,
TABLE
3. Variants of the
Vulnerable
Child Syndrome
1. The illness-prone
child
2. Pseudo-fever
of unknown origin
3. Nondisease
and non-nondisease
4. Previous, serious family biomedical or psychiatric illness
5. Medically vulnerable children
VARIANTS
VULNERABLE
if true,
an unequivocable
statement
that the child is or will shortly
be fully
OF
THE
CHILD
SYNDROME
recovered,
that special
precautions
are unnecessary,
and that the child is
not destined
to be more vulnerable
to
illness in the future.
The physician
may also share his or her experience
In the families
discussed
above,
one
of the
parents,
usually
the
mother,
secretly
believes
that a specific child is destined
to die prematurely.
Her behavior,
and the response of the child, is linked to this
that,
continuing
after
a childs
recovery
from
an
In the
case
of those
infants
who
have survived
a perinatal
illness but
who remain at risk for neurologic
impairment
in the form of slow development,
cerebral
palsy, or a learning
disorder,
the pediatrician
should verbally recognize
the normalcy
of the
parents
worries,
share his or her belief that
the
provide
the assurance
infant
carefully
is doing
well,
and
that he or she
to an assessment
of the babys development
in subsequent health supervision
visits.
An early return appointment
should
be scheduled
if there are historical
factors,
such as the previous
death
of another child, that may predispose
a parent to the vulnerable
child syndrome.
Follow-up
is also indicated
when
there
is a question
as to
whether
the parents will adapt appropriately
to the crisis and when the
parents
seem unable
to accept
the
doctors assurance that the child is
now cured. Such follow-up
is especially important
if the physician
who
cared for the child during the serious
illness
is not to provide
continuing
care. In subsequent
visits for wellchild
supervision, the primary
care
physician
should regularly
check for
manifestations
of the vulnerable
child
synrome
and intervene
accordingly.
pediatrics
in review
fear.
In
variants
of
this
syndrome,
a parent may believe that
a specific child is unusually
susceptible to illness but not be especially
worried
about the possibility
of her
childs premature
death (Table 3). In
these cases, the chief manifestation
may be the especially
frequent
use of
medical care services
with behavioral
manifestations
less prominently
reported. Although
there is some overlap with what has been discussed
above, delineation
of these variations
may facilitate
their
diagnosis
and
management,
contribute
to a more
parsimonious
use of medical
services, and increase
the comfort
and
illness, parents may have a tendency
to become
overprotective
and overindulgent,
a response
that becomes
increasingly
disadvantageous
to all
concerned.
will attend
The
vulnerable
child
syndrome
dramatizes
a clear opportunity
for
prevention
of an emotional
and developmental
disorder
by helping parents adapt
successfully
during
and
following
a severe,
acute
illness
in
their child.7 Such illnesses
are psychologically
as well as physically
hazardous.
In talking with the parents
of an ill child, the physician
must convey the diagnosis,
treatment,
and
prognosis
without
overor understatement.
An occasional
physician
or nurse may tend to overestimate
the seriousness
of a childs
illness
and risk the development
of an iatrogenic disorder.
It is recognized,
however, that in the present legal climate,
physicians
may believe that the term
critically
ill must be used with all
seriously
ill children.
Once recovery
has occurred,
however,
no construc-
PEDIATRICS
function
of the
parents
and
children
affected.
1 . The illness prone child is a cornmon cause
for excessive
use of
health
services.
In a study
of 750
mothers
interviewed
at five general
ambulatory pediatric services, Lev?
found that 27% believed that the child
brought
for care was vulnerable,
ie,
uniquely threatened
by an episode
of
illness.9 Although
these patients differ
from those with the fully expressed
vulnerable
child syndrome
in that few
of the parents
express
a fear about
the childs imminent
death, they do
regard the child as special and different from
their
other
children.
Although
60% of these children
were
judged to be medically
vulnerable
because of an illness such as asthma,
no specific
illness was found in the
other 40%. The cause for this mater#{149}
vol. 8 no. 3 september
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
1986
PIR 77
Vulnerable
Child
Syndrome
nal behavior
in the case of the illnessprone child has not been extensively
investigated.
It is well-known,
however, that anxious
or depressed
parents tend to amplify the seriousness
of symptoms
and to worry
excessively. Other nonmedically
warranted
visits are initiated
because
the possibihity of a serious
illness has been
suggested
by a relative or the mother
has convinced
herself
that the description
of a serious disease she has
just read or heard about fits her child.
It is, of course,
helpful to know this if
one is to reassure
the mother
about
her real worry.
Some children
simply
have more
illness than others,
eg, poor children
experience
more illness than those
from more economically
advantaged
families.10
Starfield
et al11 12 hypothesizes that illness-prone
children may
have a genetic or an acquired
vulnerability that causes
them to respond
to stress factors
in a physiologically
different
fashion than their peers; on
the other hand, they may just experience a greater
burden
of environmental and social stressors.
She postulates
that the vulnerability
of children whose
frequent
use of health
services
is the result
of recurrent
acute illnesses
may derive from situations in which biologic,
psychiatric,
cognitive
and psychosocial
influences
are likely to interact.12
Other investigators
have relafed
social factors and life event stressors
to the
onset of iIlness.116
2. Pseudo-FUO
is a term used by
Kleiman17
to describe
the relatively
common
situation
in which
a child
referred
because
of fever
of unknown origin does not fulfill the criteria for that diagnosis,
ie, fever of
38.3#{176}C(101#{176}F)or higher
that persists for 2 or more weeks,
an absence of localizing
findings,
and an
inability to make an etiologic
diagnosis by the usual laboratory
means.
What is reported
by the parent
as
persistent
fever
is determined
by
the physician
to be a series of selflimited, usually viral, febrile illnesses.
In some instances
in which a pattern
of frequent
temperature-taking
had
been initiated,the parent simply misunderstood
the definition
of fever (a
rectal temperature
of 38.5#{176}Cor its
equivalent),
the normal diurnal variation of body temperature,
or the efPIR
78
pediatrics
in review
#{149}
and Stamm reported
that the morbidity of cardiac nondisease,
ie, children
with innocent
murmurs
who
were
mistakenly
thought
by their parents
to have heart disease,
included
needless restriction
of activity
and other
overprotective
measures.
If not given
a clear explanation,
parents
and children may confuse
an innocent
murmur with heart disease,
overestimate
the severity
of a minor congenital
defect, or believe that the child is vulnerable to a heart attack.
In these
cases,
both parents
and child need
to be firmly told that there is absolutely no reason
to restrict
activity
and that there is no danger of a heart
attack.
Nondisease
may be established
in
the patients
mind as a result of being
told of a normal
physical
variant,
a
erroneous
laboratory
result,
or a
false-positive
screening
test. A physicians
off-hand
remark,
inadequate
clarification
of what is said, self-diagnosis, or hypochondriasis
are other
possible
causes
for nondisease.
Automated
serum
laboratory
batteries
have also contributed
to the prevalence of nonnondisease,
eg, the report of a transiently
elevated
alkaline
phosphatase
level.
Unless
accomto miss?
If the physician
believes,
on the
panied by careful interpretation,
education,
and
counseling,
positive
basis of the history,
normal findings
screening
tests
such as those
for
on physical
examination,
and the
sickle cell trait, scoliosis,
or developchilds healthy appearance,
that true
mental progress
may also be misinfever of undetermined
origin is not
present,
laboratory
studies
should
terpreted
by the parent as implying
a
not be obtained.
Such procedures
serious illness or problem with resultreinforce
the parents
belief that there
ant anxiety and apprehension.21
is, indeed,
something
seriously
wrong
4. Familial
susceptibility:
When
a
with their child. In addition to a careful
serious
biomedical
or emotional
illness, especially
one that is geneticlarification
of the parents
worries
about the childs health and an explacally transmitted,
has previously
ocnation for the recurrent
or pseudocurred in the child or another
family
member,
the parents
may think of a
fever, the parents
and child should
be told authoritatively
by the physispecific
child as vulnerable
to the
cian that the child does not have a
same problem.
As a result, any comserious disease.
When the physician
plaint that might signal the onset of
is less certain, appropriate
screening
the feared disorder
carries a special
laboratory
tests may be indicated,
eg,
emotional
charge.
Because
such
symptoms
and signs as cough,
diara complete
blood cell count, sedimenrhea, irritability,
headache,
fever, failtation rate, platelet
count, urinalysis,
ure to thrive, limb pain, limp, seizures,
urine culture,
tuberculin
test, and, in
manifestations
are
endemic
areas, histoplasmin anti- and behavioral
commonplace,
such
hypervigilant
body titers.
3. Nondisease
and
non-nondisparents lead uneasy
lives. Children
who have been cured of leukemia
and
ease, terms suggested
by Meador18
and
Morrow19
respectively,
occur
their parents
may also be concerned
when a specific disorder
is suspected
about the late complications
of canbut not found.
In 1967, Bergman2#{176} cer treatment,
especially
delayed
effect of activity
and exercise
on elevation of core body temperature.
As
a result, temperatures
within the normal range were misjudged
by the parent to be low-grade
fever.
A number
of recent
family stressors may also be identified
in the
pediatric
interview.
In addition
to fever, the parent
may be concerned
about other complaints,
such as fatigue or weakness
and fear that the
child has an occult malignancy
or that
a chronic
illness such as rheumatoid
arthritis
may be developing.
Not only
is the temperature
taken frequently,
but the child
is kept
home
from
school. At times, pseudo-FUO
masks
school
refusal,
especially
when accompaned
by other complaints
such
as sore throat,
tiredness,
headache,
or recurrent
abdominal
pain. Worried
about the childs symptoms,
the parent repeatedly
asks the child questions that invite an affirmative
reply:
Do you have a headache?
Are you
tired? That the child has been absent
from school, often for weeks,
is usually not volunteered
by the parents.
This fact is usually
revealed
only in
response
to the question:
How much
school has this illness caused Johnny
vol. 8 no. 3 september
1986
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
BEHAVIORAL
fects on endocrinologic
function
and
the CNS as well as the possibility
of
relapse or a second malignancy.
5. Chronic
Illness:
Children
with a
variety of chronic
disorders
may be
medically
vulnerable.
Their successful adaptation
may be greatly
facihitated by the pediatricians
skilled and
thoughtful
help.22 The extent to which
the child regards
him- or herself
as
vulnerable
depends
upon the specific
disease
and organ involved,
the nature of his symptoms,
and such factors as the prognosis,
the age of the
child, personality,
intelligence,
sociocultural background,
previous
life experiences,
family relations,
and the
reactions
and support
from peers,
teachers,
parents,
and health professionals.
Patients
and parents
who understand
a disease
and its treatment
poorly may overestimate
its seriousness and, therefore,
feel highly vulnerable.
Failure and disappointment
may be built into their anticipation
of
many
new experiences.
The child
may react
more
strongly
than his
peers to changes
in school, moves of
the family, discord
between
parents,
illness or death of relatives
or friends,
a change
of physicians,
and other
stressors.
Even trivial illnesses
or injuries may be poorly tolerated.
Whether
told directly
or not, the
child knows
that the disease
is lifethreatening.
This feeling
of precariousness
is kept alive by the necessity for frequent
visits to the physician, special
diets,
warnings
about
reactions,
daily medications,
procedures, and repeated
hospitalizations.
The anxiety
of the child and family
may be dramatically
heightened
when
they learn that another
child with the
same disease has died. If the disorder
is an inherited
one, the apprehension
and sense of vulnerability
increases
exponentially when a sibling dies. Although fund-raising
activities
for specific diseases
may unwittingly
promote the anxiety of patients
and their
families by an emphasis
on the possible fatal outcome
of a disorder,
the
child and his parents
may be encouraged both by the possibility
of a cure
and the evidence
of widespread
caring and support.
Even the most mature parent finds
it difficult
to cope adequately
with
both their own feelings and the needs
of the medically
vulnerable
child. The
illness almost
always
alters their relationship.
Some parents abandon
all
discipline,
whereas
others
redouble
control. As in the vulnerable
child syndrome, a previously
secure and able
mother
may find herself
unable
to
decide whether
a symptom
is trivial
or serious,
and she may worry about
periorbital
puffiness,
circles under the
childs eyes, a change
in the color
of the childs urine, constipation,
fatigue, and shortness
of breath.
Nothing allays unwarranted
anxiety
and sense of vulnerability
as effectively as continuing,
competent,
conscientious
care. The child and his or
her family need to have prompt
access to their skilled physician
should
the need arise or have clear and defmite arrangements
for substitute
coyerage if that physician
is not to be
available.
In addition
to serving
to
demonstrate
continuing
interest,
regular return visits permit the physician
to keep posted on the familys
understanding
of the illness; the childs progress with his or her disease,
school,
and peers; parent-child
relations;
and
the adjustment
of the siblings.
Other medically
vulnerable
patients
include those who are prone to become ill very rapidly, eg, children who
have had a splenectomy,
the saltlosing form of the adrenogenital
syndrome,
sickle
cell anemia,
a CSF
shunt,
asthma,
familial
dysautonomia, an immunodeficiency
disorder,
infant apnea, or ventilatory
dependency. Home monitoring
and care of
babies with infant apnea or ventilatordependent
children are relatively
new
experiences.
Although
the benefits of
home care may include the promotion
of family unity, personal
attention
to
the childs needs,
and cost containment, it may also be accompanied
by
augmented
parental
anxieties,
inability to sleep, fatigue, disruption
of family life, and unrelenting
responsibility
as a result of which the parent finds
it difficult
to sleep, go to the bathroom, take a shower,
leave the child
with a baby-sitter,
or work outside of
the home!28
Minimal requirements
for such care
include
meticulous
preparation
and
training of the parents in resuscitation
techniques;
validation
of their ability
to perform
such interventions;
ongoing support
through
immediate
acpediatrics
in review
PEDIATRICS
cess to expert medical advice around
the clock; periodic
home visits by a
physician,
social worker,
technician,
or nurse; phone check-ups
with the
hospital
staff; and opportunities
for
respite provided
by appropriately
prepared baby-sitters
or brief hospital
admissions.
The guidelines
as to
when home monitoring
may be safely
stopped
have not been clearly established, and many parents
are reluctant to discontinue
use of the device
even on the physicians
recommendation.
OTHER
DIAGNOSTIC
CONSIDERATIONS
In addition
to the vulnerable
child
syndrome
and its variants,
a number
of other reasons
for bringing
a child
for medical
care in the absence
of a
biomedical
or psychologic
disorder
in
the child need to be considered.
1 Family crisis:
Although
not reported by the parent unless asked, a
current family crisis such as separation, divorce,
death, or serious illness
in another family member
is often the
motivating
impetus to bring a child for
medical care in the absence
of a pediatric disorder.
2. Need for support:
Parents
may
return
repeatedly
to physicians
offices,
pediatric
clinics,
and emergency rooms because
those settings
offer the only positive support
readily
available
to them.
Such visits may
also represent
for a stressed
parent
an indirect way to deal with his or her
own unhappiness
and problems.
Kaplan
et a13#{176}
stated
it well: The
medical
system
of the future
must
consider
becoming
human
development centers
(which
attend
to) the
social, the psychological
as well as
the
biological
aspects
of human
life....
Support
therapy
is but one
type of need input that such centers
should include as part of their development-adaptation
efforts.
3. Secondary
gain:
Parental
exploitation
of a childs symptoms
may
also lead to an inappropriate
use of
medical
services.
Because
of personal or family dissatisfactions,
an
occasional
mother
may need for her
child to be regarded
as recurrently
or
chronically ill. In such instances,
having a sick child seems
to provide
her a secondary
gain in the form of
.
vol. 8 no. 3 september
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
1986
PIR 79
Vulnerable
Child
Syndrome
the interest,
visits,
telephone
calls,
and concern
of friends and relatives.
It may also, at least temporarily,
divert attention
from serious difficulties
in the marriage
or evoke more interest from the father,
including,
perhaps, less drinking
and more time
spent at home. In divorced
families,
the child may be represented
to be ill
to prove that the custodial
or visiting
parent has been neglectful.
4.
Munchausen
syndrome
by
proxy,
in which
the symptoms
reported
by the mother
as present
in
the child are fabricated,
is another
cause for inappropriate
use of medical care. The history
may reveal repeated
visits to different
physicians
and emergency
rooms,
many hospitalizations
of the child, and multiple
invasive
procedures
without
a specific diagnoses.
2. Benjamin
mg
pediatricians
gastroenteritis
4.
5.
6.
7.
8.
SUMMARY
10.
The vulnerable
child syndrome
and
its variants
are frequent causes for
excessive
use of health services,
behavioral
symptoms,
and much family
distress. The pediatrician can play a
central
role in their primary
and secondary prevention,
early recognition,
and treatment.
11.
1. Green
M, Solnit AJ: Reactions
to the
threatened
loss of a child: A vulnerable
child syndrome.
Pediatrics
1964;34:58-66
worry
concerning
in early childhood
severe
later
behavior. J Pe-
63:633-641
12. Starfield B, Katz H, Gabriel
A, et al: Morbidity in childhood-A
longitudinal
view. N
EngI J Med 1 984;31 0:824-829
13. Beautrais
AL, Fergusson
DM, Shannon
FT: Life events and childhood
morbidity:
A prospective study. Pediatrics
1982;
70:934-940
14. Haggerty
RJ: Life stress, illness, and social support.
Dev Med
Child
Neurol
1 980;22:391
-400
15. Green M: The adaptation
of children and
families:
The new pediatric
agenda, in
Green M (ed): The Psychological
Aspects
of the Family: The New Pediatrics.
Lexing-
pediatrics
in review
#{149}
vol. 8 no. 3 september
1 8.
19.
20.
21
22.
23.
24.
25.
26.
27.
28.
29.
30.
ton, MA, Lexington
Books,
1985, pp 112
Mechanic
D: The influence of mothers on
their childrens
health attitudes and behavor. Pediatrics
1964:33:444-453
Kleiman MB: The complaint
of persistent
fever: Recognition
and management
of
pseudo fever of unknown
origin. Pediatr
Clin North Am 1982:29:201-208
Meador CK: The art and science of nondisease. N Engi J Med 1 965;272:92-95
Morrow
G Ill: A case of non-nondisease.
Am J Dis Child 1 985;1 39:655
Bergman A: The morbidity
of cardiac nondisease in schoolchildren.
N Engl J Med
1967;276:1008-1
013
Whitten CF: Sickle-cell
programming-An
imperiled
promise.
N Engi J Med 1973;
288:318-319
Green M: The care of the child with a longterm life threatening
illness, in Green M,
Haggerty
RJ (eds): Ambulatory
Pediatrics,
ed 1 . Philadelphia,
WB Saunders
Co,
1968, pp 659-665
Black L, Hersher L, Steinschneider
A: Impact of the apnea monitor
on family life.
Pediatrics
1 978;62:681
-685
Nelson NM: But who shall monitor
the
monitor?
Pediatrics
1 978;61 :663-665
Cain LP, Kelly DH, Shannon DC: Parents
perceptions
of the psychological
and social impact of home monitoring.
Pediatrics
1 980;66:37-41
Southall DP: Home monitoring
and its role
in the sudden infant death syndrome.
Pediatrics 1983;72:1 33-137
Wasserman
AL: A prospective
study of
the impact
of home monitoring
on the
family. Pediatrics
1 984;74:323-329
Frates RC Jr. Splaingard
ML, Smith EO,
et al: Outcome
of home mechanical
ventilation
in children.
J Pediatr
1985;106:
850-856
Green M: Commentary
on James DH Jr,
Ackerman
TJ, Patterns
of primary
care
that create dependency.
Am J Dis Child
1984;1 38:534
Kaplan BH, Cassel
JC, Gore 5: Social
support
and health.
Med Care 1977;
15(suppl 5):47-58
of Corrections
The correct answers to question
issue are: A,B,E, not B,E as stated.
80
1 7.
on
disturbances
in the childs
diatr 1975;87:809-814
McCormick
MC, Shapiro
5, Staruield B:
Factors associated
with maternal opinion
of infant development-Clues
to the vulnerable child? Pediatrics
1 982;69:537543
Bentovim
A: Emotional
disturbances
of
handicapped
preschool
children and their
families-Attitudes
to the child. Br Med J
1 972;3:579-581
Yudkin 5: Six children with coughs:
The
second
diagnosis.
Lancet
1961;2:561563
Green M: The role of the pediatrician
in
the delivery of behavioral
services. J Dev
Behav Pediatr 1985;6:190-193
Levy JC: Vulnerable
children: Parents perspectives
and the use of medical care.
Pediatrics
1 980;65:956-963
Green M: The vulnerable
child: Intimations
of
mortality.
Pediatrics
1980;
65:1042-1
043
Egbuonu
L, Starfield
B: Child health and
social status. Pediatrics
1 982;69:550-557
Starfield B, van den Berg BJ, Steinwachs
DM, et al: Variations in utilization of health
services
by children.
Pediatrics
1979;
Department
PIR
1 6.
48:284-290
3. Sigal J, Gagnon P: Effects of parents and
9.
REFERENCES
PY: Psychological
problems
folrecovery
from acute life-threatenillness. Am J Orthopsychiatry
1978;
lowing
4 of the Self-Evaluation
quiz in the March
1986
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
1986
Vulnerable Child Syndrome and Its Variants
Morris Green
Pediatrics in Review 1986;8;75
DOI: 10.1542/pir.8-3-75
Updated Information &
Services
including high resolution figures, can be found at:
http://pedsinreview.aappublications.org/content/8/3/75
Permissions & Licensing
Information about reproducing this article in parts (figures, tables) or in its
entirety can be found online at:
http://pedsinreview.aappublications.org/site/misc/Permissions.xhtml
Reprints
Information about ordering reprints can be found online:
http://pedsinreview.aappublications.org/site/misc/reprints.xhtml
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
Vulnerable Child Syndrome and Its Variants
Morris Green
Pediatrics in Review 1986;8;75
DOI: 10.1542/pir.8-3-75
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://pedsinreview.aappublications.org/content/8/3/75
Pediatrics in Review is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1979. Pediatrics in Review is owned, published, and
trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove
Village, Illinois, 60007. Copyright 1986 by the American Academy of Pediatrics. All rights reserved.
Print ISSN: 0191-9601.
Downloaded from http://pedsinreview.aappublications.org/ at Universite De Sherbrooke on April 13, 2015
Potrebbero piacerti anche
- Preparation and Education for Parenthood: A Pathway to Understanding the Carer's Role in Infant EducationDa EverandPreparation and Education for Parenthood: A Pathway to Understanding the Carer's Role in Infant EducationValutazione: 5 su 5 stelle5/5 (1)
- CDC Connectiveness BookletDocumento24 pagineCDC Connectiveness BookletDominique Harmon100% (1)
- Well-Child Care in Infancy: Promoting Readiness for LifeDa EverandWell-Child Care in Infancy: Promoting Readiness for LifeNessuna valutazione finora
- Prevention and Control of Infectious DiseaseDocumento33 paginePrevention and Control of Infectious DiseaseGada Abdulcader100% (1)
- Educational Leadership: a Student-Centered ApproachDa EverandEducational Leadership: a Student-Centered ApproachNessuna valutazione finora
- Child Psychopathology PSY 3223, SECTION 12: Instructor: Samantha ConnollyDocumento37 pagineChild Psychopathology PSY 3223, SECTION 12: Instructor: Samantha Connollylwitek02Nessuna valutazione finora
- Caring for Children with Special Healthcare Needs and Their Families: A Handbook for Healthcare ProfessionalsDa EverandCaring for Children with Special Healthcare Needs and Their Families: A Handbook for Healthcare ProfessionalsLinda L. EddyNessuna valutazione finora
- Senior Project PresentationDocumento13 pagineSenior Project Presentationapi-535239899Nessuna valutazione finora
- NURSING THE CHILDBEARING FAMILY: Passbooks Study GuideDa EverandNURSING THE CHILDBEARING FAMILY: Passbooks Study GuideNessuna valutazione finora
- Education Program On Childhood ObesityDocumento8 pagineEducation Program On Childhood ObesityAssignment Help AustraliaNessuna valutazione finora
- Collaborative Problem Solving: An Evidence-Based Approach to Implementation and PracticeDa EverandCollaborative Problem Solving: An Evidence-Based Approach to Implementation and PracticeAlisha R. PollastriNessuna valutazione finora
- Health EducationDocumento15 pagineHealth EducationNashter ArajainNessuna valutazione finora
- WHO Promoting Adolescent Sexual and Reproductive Health Through Schools in Low Income Countries - An Information BriefDocumento24 pagineWHO Promoting Adolescent Sexual and Reproductive Health Through Schools in Low Income Countries - An Information BriefOwais KhanNessuna valutazione finora
- A Guide For Monitoring Child Development in Low - and Middle-Income CountriesDocumento11 pagineA Guide For Monitoring Child Development in Low - and Middle-Income Countriesanisetiyowati14230% (1)
- Unit PlanDocumento9 pagineUnit PlanMradul PrajapatiNessuna valutazione finora
- A Brief History of Mental Health CareDocumento3 pagineA Brief History of Mental Health Carexiang jinNessuna valutazione finora
- Skills For Care Presentation Web Version Standard 4Documento11 pagineSkills For Care Presentation Web Version Standard 4Georgiana GeorgyNessuna valutazione finora
- 15 How To Answer Those Tough Questions About Elder Abuse Toughquestions 2012Documento5 pagine15 How To Answer Those Tough Questions About Elder Abuse Toughquestions 2012api-309082881Nessuna valutazione finora
- Asthma: Practice GapDocumento21 pagineAsthma: Practice GapMichelleHanNessuna valutazione finora
- FGM PresentationDocumento10 pagineFGM Presentationapi-319323494Nessuna valutazione finora
- Ardimer, Joname P. Beed-A1Documento23 pagineArdimer, Joname P. Beed-A1Glenn disha PagayonNessuna valutazione finora
- FilariasisDocumento8 pagineFilariasisTheeya QuigaoNessuna valutazione finora
- Elder Abuse Neglect ReportDocumento31 pagineElder Abuse Neglect ReportPatricia MariaNessuna valutazione finora
- Interview Questions 5Documento5 pagineInterview Questions 5api-502274542Nessuna valutazione finora
- Therapeutic Relationship: Rubilyn A. Bulquerin-Sumaylo, RN, MSN, LPTDocumento24 pagineTherapeutic Relationship: Rubilyn A. Bulquerin-Sumaylo, RN, MSN, LPTRubz BulquerinNessuna valutazione finora
- Drug Awareness and Prevention Program PDFDocumento6 pagineDrug Awareness and Prevention Program PDFMarcos Bulay OgNessuna valutazione finora
- MUMJ Pediatric Rash QuizDocumento4 pagineMUMJ Pediatric Rash QuizTarran PhagooNessuna valutazione finora
- Pediatric EmergenciesDocumento47 paginePediatric EmergenciesahmedNessuna valutazione finora
- CICMH Mental Health Crisis Response On Campus ToolkitDocumento34 pagineCICMH Mental Health Crisis Response On Campus ToolkitProyecto IMABIS100% (1)
- Research Proposal-Salvatory B. GibuyiDocumento28 pagineResearch Proposal-Salvatory B. GibuyiErick JohnNessuna valutazione finora
- Bullying: Submitted byDocumento4 pagineBullying: Submitted byJelors Ocon EstacioNessuna valutazione finora
- Feature StoryDocumento5 pagineFeature Storyapi-586108255Nessuna valutazione finora
- Fowler Thesis 2015Documento76 pagineFowler Thesis 2015Isaiah Samuel De GraciaNessuna valutazione finora
- Unit 29 Health PromotionDocumento4 pagineUnit 29 Health Promotionchandni0810100% (1)
- Youlia Weber - Trauma 101 For Educators - Eduu 602Documento6 pagineYoulia Weber - Trauma 101 For Educators - Eduu 602api-542152634Nessuna valutazione finora
- Psychological ChangesDocumento36 paginePsychological ChangesAndrei La MadridNessuna valutazione finora
- Nursing Students' Views On The COVID 19 Pandemic and Their Percieved Stress LevelsDocumento7 pagineNursing Students' Views On The COVID 19 Pandemic and Their Percieved Stress LevelsAudy SaviraNessuna valutazione finora
- Children With Mental Disorders: Making Sense of Their Needs and The Systems That Help ThemDocumento24 pagineChildren With Mental Disorders: Making Sense of Their Needs and The Systems That Help Thembellydanceafrica9540Nessuna valutazione finora
- AEMT - Operations Exam PracticeDocumento25 pagineAEMT - Operations Exam PracticeEMS Director100% (1)
- Research ProposalDocumento3 pagineResearch Proposalapi-336898508100% (1)
- What Is Response To Intervention?: Universal ScreeningDocumento1 paginaWhat Is Response To Intervention?: Universal Screeningapi-395007443Nessuna valutazione finora
- 1.1 Concept of HealthDocumento31 pagine1.1 Concept of HealthDIPENDRA KUMAR KUSHAWAHANessuna valutazione finora
- Core Character Traits Final Version 2-29-08Documento4 pagineCore Character Traits Final Version 2-29-08sameerb100% (1)
- Child Care 1 - Responsibilites of The CaregiverDocumento2 pagineChild Care 1 - Responsibilites of The Caregiverrushie23Nessuna valutazione finora
- WHO - Health Researchers GuideDocumento235 pagineWHO - Health Researchers Guidejonlim78Nessuna valutazione finora
- Nursing Negligence and Nurse MalpracticesDocumento2 pagineNursing Negligence and Nurse MalpracticesblazegomezNessuna valutazione finora
- Artifact 2 Multi Lesson Plan Edu 280Documento6 pagineArtifact 2 Multi Lesson Plan Edu 280api-541064639Nessuna valutazione finora
- Concept of Health and IllnessDocumento29 pagineConcept of Health and IllnessMelchor Felipe SalvosaNessuna valutazione finora
- Dummy ReportDocumento29 pagineDummy ReportnaquiahoNessuna valutazione finora
- Developmental Dysplasia of The Hip - Clinical Features and Diagnosis - UpToDateDocumento13 pagineDevelopmental Dysplasia of The Hip - Clinical Features and Diagnosis - UpToDateFernandoVianaNessuna valutazione finora
- Section One - About Disability: Sensory: Neurological: PhysicalDocumento4 pagineSection One - About Disability: Sensory: Neurological: Physicalvenkata ramakrishnaiahNessuna valutazione finora
- Physical Abuse in ChildrenDocumento113 paginePhysical Abuse in ChildrenDan Matthew BuriasNessuna valutazione finora
- Ecomap Activity PDF Format Free TemplateDocumento3 pagineEcomap Activity PDF Format Free TemplatecmateusrNessuna valutazione finora
- Ethical and Legal Issues inDocumento9 pagineEthical and Legal Issues inLina Mahayaty SembiringNessuna valutazione finora
- Speech OutlineDocumento3 pagineSpeech Outlinekarlymae33% (3)
- Nursing Family Community Wellness Diagnoses SuttonDocumento6 pagineNursing Family Community Wellness Diagnoses SuttonMaria LpzNessuna valutazione finora
- Final Written Resaerch Report. JOHRYL ANDRADADocumento12 pagineFinal Written Resaerch Report. JOHRYL ANDRADASANNY OMELANessuna valutazione finora
- Child DevelopmentDocumento9 pagineChild DevelopmentNoor AftabNessuna valutazione finora
- Assisted Reproductive TechnologyDocumento2 pagineAssisted Reproductive TechnologyHafiz JusohNessuna valutazione finora
- Child in The Family and Community RevisedDocumento22 pagineChild in The Family and Community Revisedokwadha simionNessuna valutazione finora
- Pot of Gold Self Esteem Activity - Counselor KeriDocumento6 paginePot of Gold Self Esteem Activity - Counselor KeriLeila MargaridaNessuna valutazione finora
- Growth Mindset Printable Book Updated PDFDocumento5 pagineGrowth Mindset Printable Book Updated PDFLeila MargaridaNessuna valutazione finora
- Growth Mindset Printable Coloring SheetsDocumento8 pagineGrowth Mindset Printable Coloring SheetsLeila MargaridaNessuna valutazione finora
- Feelings Tracker - Counselor KeriDocumento1 paginaFeelings Tracker - Counselor KeriLeila MargaridaNessuna valutazione finora
- Cognitive Development - Past, Present, and FutureDocumento8 pagineCognitive Development - Past, Present, and FutureLeila MargaridaNessuna valutazione finora
- Challenging Cognitive Distortions HealthyPsych - ComDocumento1 paginaChallenging Cognitive Distortions HealthyPsych - ComLeila MargaridaNessuna valutazione finora
- Cognitive Coping and Childhood Anxiety Disorders - ImpressoDocumento8 pagineCognitive Coping and Childhood Anxiety Disorders - ImpressoLeila MargaridaNessuna valutazione finora
- The Development of Normal Fear - A Century of ResearchDocumento24 pagineThe Development of Normal Fear - A Century of ResearchLeila MargaridaNessuna valutazione finora
- Prevalence and Development of Anxiety DisordersDocumento8 paginePrevalence and Development of Anxiety DisordersLeila MargaridaNessuna valutazione finora
- Effect of Anxiety Reduction On Children's School Performance and Social AdjustmentDocumento6 pagineEffect of Anxiety Reduction On Children's School Performance and Social AdjustmentLeila MargaridaNessuna valutazione finora
- Cognitive Processing in Children - Relation To Anxiety and Family Influences - ImpressoDocumento7 pagineCognitive Processing in Children - Relation To Anxiety and Family Influences - ImpressoLeila MargaridaNessuna valutazione finora
- Cunningham2004 PDFDocumento10 pagineCunningham2004 PDFLeila MargaridaNessuna valutazione finora
- Cognitive Processing in Children - Relation To Anxiety and Family Influences - ImpressoDocumento7 pagineCognitive Processing in Children - Relation To Anxiety and Family Influences - ImpressoLeila MargaridaNessuna valutazione finora
- Unraveling The Mysteries of Anxiety and Its Disorders From The Perspective - ImpressoDocumento17 pagineUnraveling The Mysteries of Anxiety and Its Disorders From The Perspective - ImpressoLeila MargaridaNessuna valutazione finora
- Anxiety Disorders in Children - Family Matters (MODELO ETIOLOGICO)Documento16 pagineAnxiety Disorders in Children - Family Matters (MODELO ETIOLOGICO)Leila MargaridaNessuna valutazione finora
- Cognitive Errors, Anxiety Sensitivity, and Anxiety Control Beliefs - Their Unique and Specific Associations With Childhood Anxiety Symptoms.Documento29 pagineCognitive Errors, Anxiety Sensitivity, and Anxiety Control Beliefs - Their Unique and Specific Associations With Childhood Anxiety Symptoms.Leila MargaridaNessuna valutazione finora
- Manual For Mental Health Continuum Short FormDocumento6 pagineManual For Mental Health Continuum Short FormShabeel HamNafNessuna valutazione finora
- Anxiety in Children - Perceived Family Environments and Observed Family InteractionDocumento14 pagineAnxiety in Children - Perceived Family Environments and Observed Family InteractionLeila MargaridaNessuna valutazione finora
- Associations Between Maternal and Paternal Parenting Behaviors, Anxiety and Its Precursors in Early Childhood - A Meta-Analysis.Documento65 pagineAssociations Between Maternal and Paternal Parenting Behaviors, Anxiety and Its Precursors in Early Childhood - A Meta-Analysis.Leila MargaridaNessuna valutazione finora
- Anxiety Disorders During Childhood and Adolescence Origins and TreatmentDocumento33 pagineAnxiety Disorders During Childhood and Adolescence Origins and TreatmentCellaNessuna valutazione finora
- Construct ValidityDocumento20 pagineConstruct ValidityCorina IcaNessuna valutazione finora
- Theme Based Word Problems Based On Chapter 1: Math Grade 7Documento3 pagineTheme Based Word Problems Based On Chapter 1: Math Grade 7api-537694937Nessuna valutazione finora
- Gadget-Based Digital Literacy in Learning Writing Skills For Elementary School StudentsDocumento8 pagineGadget-Based Digital Literacy in Learning Writing Skills For Elementary School StudentsJouda ArfaouiNessuna valutazione finora
- Grade 5 DLL English 5 Q2 Week 6Documento4 pagineGrade 5 DLL English 5 Q2 Week 6kotarobrother2350% (2)
- HSC4537 SyllabusDocumento10 pagineHSC4537 Syllabusmido1770Nessuna valutazione finora
- Pedigree Analysis WorksheetDocumento6 paginePedigree Analysis WorksheetLloaana 12Nessuna valutazione finora
- Experience 5 Year: Career SummaryDocumento2 pagineExperience 5 Year: Career SummaryAshok SharmaNessuna valutazione finora
- Explanatory Models and Practice Models of SHRDDocumento5 pagineExplanatory Models and Practice Models of SHRDSonia TauhidNessuna valutazione finora
- Degraded words in Fran Meneses' YouTube blog (Восстановлен)Documento32 pagineDegraded words in Fran Meneses' YouTube blog (Восстановлен)10A opshNessuna valutazione finora
- Edci 514 Lesson Plan PWP Module 3Documento10 pagineEdci 514 Lesson Plan PWP Module 3api-265028034Nessuna valutazione finora
- Tax Exemption of Educational InstitutionsDocumento1 paginaTax Exemption of Educational InstitutionsWendz GatdulaNessuna valutazione finora
- Script For The ReportDocumento11 pagineScript For The ReportJaneiel Fae LipanaNessuna valutazione finora
- HKUL - Contact UsDocumento10 pagineHKUL - Contact Usyip90Nessuna valutazione finora
- University of Santo TomasDocumento3 pagineUniversity of Santo TomasKARL JOSHUA ARON0% (1)
- Guidelines For Internship Report BBADocumento20 pagineGuidelines For Internship Report BBAumesh aryaNessuna valutazione finora
- Anderson Piano Syllabus 2020-2021Documento5 pagineAnderson Piano Syllabus 2020-2021Desmond AndersonNessuna valutazione finora
- TAHSILDAR Application FormDocumento2 pagineTAHSILDAR Application FormAmit PanchalNessuna valutazione finora
- Iom 1 PDFDocumento1 paginaIom 1 PDFthishaniNessuna valutazione finora
- The Implementation of Social Work Hybrid Program in Medical Mission Group College of General Santos City, Incorporated: Basis For Curriculum Development PlanDocumento14 pagineThe Implementation of Social Work Hybrid Program in Medical Mission Group College of General Santos City, Incorporated: Basis For Curriculum Development PlanPsychology and Education: A Multidisciplinary JournalNessuna valutazione finora
- Naturalism and EducationDocumento2 pagineNaturalism and EducationAiza JamitoNessuna valutazione finora
- Esl Lesson Plan For Ed EndingDocumento6 pagineEsl Lesson Plan For Ed EndingMiriam Garcia RodriguezNessuna valutazione finora
- Inverse Cube LawDocumento2 pagineInverse Cube LawmissuedNessuna valutazione finora
- Indicators of Cognitive and MetacognitiveDocumento1 paginaIndicators of Cognitive and MetacognitiveMiguel Angelo AnggamNessuna valutazione finora
- A Review On Computational Methods Based On Machine Learning and Deep Learning Techniques For Malaria DetectionDocumento5 pagineA Review On Computational Methods Based On Machine Learning and Deep Learning Techniques For Malaria DetectionGopi ChandNessuna valutazione finora
- Is Lacans Theory of The Mirror Stage Still ValidDocumento10 pagineIs Lacans Theory of The Mirror Stage Still ValidEmin MammadovNessuna valutazione finora
- The One Who Is Not Loyal To The Motherland... Can Never Be Loyal To Anyone... - KushDocumento5 pagineThe One Who Is Not Loyal To The Motherland... Can Never Be Loyal To Anyone... - KushanonymousNessuna valutazione finora
- Hci 101Documento11 pagineHci 101Divine ManaloNessuna valutazione finora
- 8th Grade Fitness Unit PlanDocumento48 pagine8th Grade Fitness Unit Planapi-214597204100% (4)
- The Differences Between Academic and Professional CredentialsDocumento3 pagineThe Differences Between Academic and Professional CredentialsGaus MohiuddinNessuna valutazione finora
- Grammatical Competence and Models of L2 LearningDocumento11 pagineGrammatical Competence and Models of L2 LearningMorten Oddvik100% (6)