Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Jaundice and HEG
Caricato da
Niluh Ita Pasyanti0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
48 visualizzazioni2 pagineThis case report describes a woman who experienced recurrent jaundice during the first trimester of three consecutive pregnancies, each time shortly after the onset of severe vomiting (hyperemesis gravidarum). Laboratory tests showed increased liver enzymes and conjugated hyperbilirubinemia. Liver biopsies revealed few necrotic hepatocytes. Jaundice resolved rapidly each time after vomiting ceased. This observation supports a causal relationship between severe vomiting from hyperemesis gravidarum and the development of jaundice in pregnant women.
Descrizione originale:
heg
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoThis case report describes a woman who experienced recurrent jaundice during the first trimester of three consecutive pregnancies, each time shortly after the onset of severe vomiting (hyperemesis gravidarum). Laboratory tests showed increased liver enzymes and conjugated hyperbilirubinemia. Liver biopsies revealed few necrotic hepatocytes. Jaundice resolved rapidly each time after vomiting ceased. This observation supports a causal relationship between severe vomiting from hyperemesis gravidarum and the development of jaundice in pregnant women.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
48 visualizzazioni2 pagineJaundice and HEG
Caricato da
Niluh Ita PasyantiThis case report describes a woman who experienced recurrent jaundice during the first trimester of three consecutive pregnancies, each time shortly after the onset of severe vomiting (hyperemesis gravidarum). Laboratory tests showed increased liver enzymes and conjugated hyperbilirubinemia. Liver biopsies revealed few necrotic hepatocytes. Jaundice resolved rapidly each time after vomiting ceased. This observation supports a causal relationship between severe vomiting from hyperemesis gravidarum and the development of jaundice in pregnant women.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 2
Gut, 1984, 25, 1414-1415
Case report
Recurrent jaundice caused by recurrent hyperemesis
gravidarum
D LARREY, B RUEFF, G FELDMANN, C DEGOTT,
G DANAN, AND J P BENHAMOU
From The Unite de Recherches de Physiopathologie Hepatique (INSERM), and The Service d'Anatomie et de
Cytologie Pathologiques, Hopital Beaujon, Clichy, France
SUMMARY The existence of jaundice induced by hyperemesis gravidarum is controversial. We
report the case of a woman who suffered from three episodes of jaundice during the first trimester
of three consecutive pregnancies, a few days after the onset of hyperemesis gravidarum. Jaundice
was caused by conjugated hyperbilirubinaemia. Serum alanine aminotransferase activity was
increased and scarce necrotic hepatocytes were shown on light and electron microscopic
examinations. Cessation of vomiting was rapidly followed by complete recovery. This
observation supports the view that severe vomiting can cause jaundice in pregnant women.
Hyperemesis gravidarum had long been a
recognised cause of jaundice. 1-6 Since 1960,
however, several authors have questioned the causal
relationship between hyperemesis gravidarum and
jaundice, and attributed jaundice affecting pregnant
women with severe vomiting to chloroform,78
antiemetic drugs,9 or viral hepatitis.7 9 Hyperemesis
gravidarum is mentioned as a cause of daundice in
some recent handbooks of hepatology, l1 but not
in others.12-14 In this report, we describe the case of
a woman in whom the development of jaundice was
distinctly related to hyperemesis gravidarum: this
patient suffered from three episodes of jaundice
during the first trimester of three consecutive
pregnancies, a few days after the onset of severe
vomiting.
aminotransferase was 22 times the upper limit of
normal; serum bilirubin was 102 ,umol/l; vomiting
stopped after parenteral administration of metoclopramide; jaundice then diminished rapidly; at the
18th week of pregnancy, serum alanine aminotransferase and serum bilirubin were normal. In
December 1979, at the ninth week of her third
pregnancy, six days after the onset of hyperemesis
gravidarum, jaundice developed again; serum
alanine aminotransferase was eight times the upper
limit of normal; serum bilirubin was 78 ,umol/l; the
liver and biliary tract were normal on ultrasonography; vomiting stopped after parenteral administration of metoclopramide; a normal diet was
resumed and serum alanine aminotransferase and
serum bilirubin returned to normal; spontaneous
abortion occurred at the 15th week. In May 1981, at
Case report
the 10th week of her fourth pregnancy, six days after
the onset of hyperemesis gravidarum, the patient
A 30 year old woman was admitted to H6pital was jaundiced again; serum alanine aminoBeaujon on 28 May, 1981 with jaundice. In 1976, transferase was five times the upper limit of normal;
during her first pregnancy, she suffered from mild serum bilirubin was 58 ,urmol/l. On 28 May, 1981 at
vomiting and was not jaundiced. In January 1979, at the 12th week of pregnancy, the patient was
the fifth week of her second pregnancy, one week admitted to Hopital Beaujon for further investiafter the onset of hyperemesis gravidarum, jaundice gations.
developed; the liver size was normal; serum alanine
On admission, the patient complained of
abundant vomiting; the weight loss was 11 kg. She
was jaundiced and the liver span was 8 cm on the
Address for correspondence: Dr D Larrey, INSERM U 24, H6pital Beaujon,
92118 Clichy, France.
right miclavicular line. Serum bilirubin was 100
Received for publication 21 February 1984
,umol/l; serum conjugated bilirubin 85 ,umol/l; serum
1414
Recurrent jaundice caused by recurrent hyperemesis gravidarum
alanine aminotransferase seven times the upper
limit of normal; serum alkaline phosphatase normal;
prothrombin normal; HBsAg, anti-HBs, and antiHBc absent; anti-HA absent; red blood cell count
4 200 000/mm3; reticulocyte count 48 000/mm3.
Histologic examination of a liver specimen taken by
percutaneous needle biopsy showed cholestasis and
scarce necrotic hepatocytes in the centrilobular
area. Oil red 0 staining on frozen section did not
show any cytoplasmic fatty vacuoles. Electron
microscopic examination showed deposits of
pigments within the lumen of few canaliculi which
were moderately dilated and had lost their
microvilli; a few necrotic hepatocytes were seen.
Intravenous administration of sulpiride was started
on 29 May and was followed by cessation of
vomiting on 31 May. Jaundice decreased rapidly and
disappeared on 10 June. Serum bilirubin, serum
alkaline phosphatase, and serum alanine aminotransferase were normal on 15 June. The patient
gave birth to healthy twins in November.
Discussion
The development of jaundice one week after the
onset of severe vomiting during the first trimester of
three consecutive pregnancies and the rapid
recovery after cessation of vomiting strongly suggest
a causal relationship between hyperemesis
gravidarum and icterus in our patient. This view is
reinforced by the following arguments: (a) jaundice
did not develop during our patient's first pregnancy
which was not accompanied by severe vomiting; (b)
our patient did not suffer from chronic liver disease;
(c) drug hepatitis can be excluded: metoclopramide
and sulpiride, the only two drugs which were given
to our patient, were administered after the onset of
jaundice; (d) jaundice because of obstruction of the
common bile duct, in particular by biliary stone, is
unlikely because of the absence of pain and normal
ultrasonography; (e) recurrent cholestasis of
pregnancy and acute fatty liver of pregnancy can be
excluded: these conditions do not develop during
the first trimester of pregnancy and are associated
with manifestations and liver lesions15 16 different
from those observed in our patient.
The mechanism of jaundice induced by hyperemesis gravidarum is obscure. Fasting reduces BSP
elimination and slightly increases serum aminotransferases in obese patients. 17 Fasting decreases
bile flow and bile salt excretion in the rat. 18
Kwashiorkor, a condition with prolonged
denutrition, can be associated with hyperbilirubinaemia and increased serum aminotransferases. 19 The view that fasting may contribute
to jaundice because of hyperemesis gravidarum is
1415
consistent with the observation that, even in the
absence of jaundice, BSP elimination is lower in
women with hyperemesis gravidarum than in those
with mild or without vomiting.2t) Jaundice might be
the major form of this usually subclinical hepatic
dysfunction.
References
1 Herold L. Die leberfunktion in der physiologischen
Schwangerschaft und bei der Hyperemesis gravidarum.
Arch Gynaekol 1939; 168: 509-24.
2 Verhage JC. Hyperemesis gravidarum. Ned Tijdschr
Verlosk Gynaecol 1940; 43: 36-74.
3 Millar D. The significance of jaundice in pregnancy. J
Obstet Gynaecol Br Emp 1954; 61: 405.
4 Thorling L. Jaundice in pregnancy. A clinical study.
Acta Med Scand 1955; 151: suppl 302: 1-123.
5 Meyer J. Ikterus und Schwangerschaft. Geburtshilfe
Fraunheilkd 1955; 15: 1013-19.
6 Klier E. Ikterus im Rahmen der Schwangershaftsfruhtoxikose. Wien Klin Wochenschr 1956; 68: 64-6.
7 Sheehan HL. Jaundice in pregnancy. Am J Obstet
Gynecol 1961; 81: 427-40.
8 Klatskin G. Toxic and drug-induced hepatitis. In:
Schiff L, ed. Diseases of the Liver 2nd ed. Philadelphia:
Lippincott, 1963: 453-538.
9 Iber FL. Jaundice in pregnancy-a review. Am J Obstet
Gynecol 1965; 91: 721-53.
10 Sherlock S. Diseases of the liver and biliary system. 6th
ed. Oxford: Blackwell Scientific Publications, 1981:
400-5.
11 Krejs GJ, Haemmerli UP. Jaundice during pregnancy.
In: Schiff L, ed. Diseases of the liver 5th ed. Philadelphia: Lippincott, 1982: 1561-80.
12 Sherlock S. Diseases of the Liver and Biliary System 5th
ed. Oxford: Blackwell Scientific Publications, 1975:
570-8.
13 Schaffner F, Popper H. Classification and mechanism
of cholestasis. In: Wright R, Alberti KGMM, Karran
S, Millward-Sadler GH, eds. Liver and Biliary Disease.
Pathophysiology. Diagnosis. Management. London:
Saunders, 1979: 296-323.
14 Benhamou JP. Foie et grossesse. In: Benhamou JP,
Sarles H, Gerolami A, eds. Foie, Pancreas, Voies
Biliaires. 3rd ed. Paris: Flammarion, 1980: 105-6.
15 Haemmerli UP. Jaundice during pregnancy with
special emphasis on recurrent jaundice during
pregnancy and its differential diagnosis. Acta Med
Scand 1966; 179: suppl 444: 1-111.
16 Holzbach RT. Jaundice in pregnancy-1976. Am J Med
1976; 61: 367-76.
17 Verdy M. BSP retention during total fasting.
Metabolism 1966; 15: 769-72.
18 Mahu JL, Duvaldestin P, Dhumeaux D, Berthelot P.
Biliary transport of cholephilic dyes: evidence for two
different pathways. Am J Physiol 1977; 232: E445-50.
19 Webber BL, Freiman I. The liver in Kwashiorkor.
Arch Pathol 1974; 98: 400-8.
20 Adams RH, Gordon J, Combes B. Hyperemesis
gravidarum. I. Evidence of hepatic dysfunction. Obstet
Gynecol 1968; 31: 659-64.
Potrebbero piacerti anche
- Acute Fatty Liver of Pregnancy: Letter To EditorDocumento2 pagineAcute Fatty Liver of Pregnancy: Letter To EditorsaryindrianyNessuna valutazione finora
- Falciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesDocumento3 pagineFalciparum Malaria Complicated With Acute Pancreatitis: A Report of Case SeriesMuhammad Taufik AdhyatmaNessuna valutazione finora
- 54 Shivraj EtalDocumento3 pagine54 Shivraj EtaleditorijmrhsNessuna valutazione finora
- Higado Graso y Embarazo PDFDocumento4 pagineHigado Graso y Embarazo PDFSebastian Hernandez MejiaNessuna valutazione finora
- Acute Fatty Liver With PregnancyDocumento50 pagineAcute Fatty Liver With PregnancyDr. mohammed100% (1)
- Journal Presentation: The New England Journal of Medicine Case Records of The Massachusetts General HospitalDocumento49 pagineJournal Presentation: The New England Journal of Medicine Case Records of The Massachusetts General HospitalSomnath SenguptaNessuna valutazione finora
- Al12 1 JuvenileDocumento24 pagineAl12 1 JuvenileDiego Alberto Hernández CatalánNessuna valutazione finora
- EMQsDocumento30 pagineEMQsnob2011nob100% (1)
- 10-Month-Old Patient With Severe Abdominal Distention and LethargyDocumento7 pagine10-Month-Old Patient With Severe Abdominal Distention and Lethargycamille nina jane navarroNessuna valutazione finora
- Today's: Diseases of The AlimentaryDocumento3 pagineToday's: Diseases of The AlimentaryArix BakaNessuna valutazione finora
- Gallbladder IIDocumento22 pagineGallbladder IIAli SafaaNessuna valutazione finora
- Benign Pancreatic Hyperenzymemia or Gullo's Syndrome: LetterDocumento4 pagineBenign Pancreatic Hyperenzymemia or Gullo's Syndrome: LetterbogdanotiNessuna valutazione finora
- Normal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyDocumento4 pagineNormal Protein Diet and L-Ornithine-L-Aspartate For Hepatic EncephalopathyElisa SalakayNessuna valutazione finora
- Recurrent Hepatic Coma in A Chronic Hemooial Ysis Patient: Successful Treatment by CapoDocumento4 pagineRecurrent Hepatic Coma in A Chronic Hemooial Ysis Patient: Successful Treatment by CapoEka HandreanNessuna valutazione finora
- Painless Jaundice CaseDocumento8 paginePainless Jaundice CaseStarr NewmanNessuna valutazione finora
- en Choledocholithiasis During Pregnancy MulDocumento6 pagineen Choledocholithiasis During Pregnancy MulJuan SlaxNessuna valutazione finora
- Hepatocellular Carcinoma Causing Severe.1057Documento1 paginaHepatocellular Carcinoma Causing Severe.1057Vardan KocharNessuna valutazione finora
- Biloma After Laparoscopic Cholecystectomy: Case ReportDocumento3 pagineBiloma After Laparoscopic Cholecystectomy: Case ReportAlpriyando Rindy AgustinusNessuna valutazione finora
- Fatty Liver in Pregnancy - StatPearls - NCBI BookshelfDocumento6 pagineFatty Liver in Pregnancy - StatPearls - NCBI BookshelfAndres Pimentel AlvarezNessuna valutazione finora
- Acute Pancreatitis With Normal Serum Lipase: A Case SeriesDocumento4 pagineAcute Pancreatitis With Normal Serum Lipase: A Case SeriesSilvina VernaNessuna valutazione finora
- PancreatitisDocumento7 paginePancreatitisavigenNessuna valutazione finora
- Colangitis FelinaDocumento22 pagineColangitis FelinaJuan K SeguraNessuna valutazione finora
- Gastroentrology LastDocumento48 pagineGastroentrology LastAbdallah K. RamadanNessuna valutazione finora
- Pancreatitis INCDocumento5 paginePancreatitis INCAmber BlodduweddNessuna valutazione finora
- Pyloric Stenosis ChibuezeDocumento12 paginePyloric Stenosis ChibuezeChibueze AfugbuomNessuna valutazione finora
- Maternal and Perinatal Outcome in Severe Pregnancy Related Liver DiseasesDocumento5 pagineMaternal and Perinatal Outcome in Severe Pregnancy Related Liver Diseasesadrip234Nessuna valutazione finora
- Acute Fatty Liver of Pregnancy: A Case ReportDocumento0 pagineAcute Fatty Liver of Pregnancy: A Case ReportnajmulNessuna valutazione finora
- Case Scenario GastroDocumento3 pagineCase Scenario Gastroprosie392Nessuna valutazione finora
- Gut 1962 Goulston 252 4Documento4 pagineGut 1962 Goulston 252 4LedenaBjavoglaNessuna valutazione finora
- Gasteroenterology 151 200Documento30 pagineGasteroenterology 151 200Ahmed Kh. Abu WardaNessuna valutazione finora
- Elevated Deoxycholic Acid and Idiopathic Recurrent Acute PancreatitisDocumento3 pagineElevated Deoxycholic Acid and Idiopathic Recurrent Acute PancreatitisMaria LimaNessuna valutazione finora
- Case Report Hepato FinalDocumento29 pagineCase Report Hepato FinalBangkit PutrawanNessuna valutazione finora
- Acute Fatty Liver of Pregnancy: An Update On Pathogenesis and Clinical ImplicationsDocumento8 pagineAcute Fatty Liver of Pregnancy: An Update On Pathogenesis and Clinical ImplicationsRembulanAyuNiendhitaPutriNessuna valutazione finora
- Management of Pregnancy JaundiceDocumento28 pagineManagement of Pregnancy JaundiceShailani Thakur100% (1)
- Jaundiceandpregnancy JIACMDocumento7 pagineJaundiceandpregnancy JIACMHaekal HafizhNessuna valutazione finora
- Test #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyDocumento47 pagineTest #24 Q.Id 863 Question 1 of 39 Item Review Division: HepatologyJahangir AlamNessuna valutazione finora
- Liver Cirrhosis Marking KeyDocumento5 pagineLiver Cirrhosis Marking KeyChristone “Zuluzulu” ZuluNessuna valutazione finora
- Trousseau's Syndrome in CholangiocarcinomaDocumento7 pagineTrousseau's Syndrome in CholangiocarcinomaAnna MariaNessuna valutazione finora
- Pancreas QuestionDocumento7 paginePancreas QuestionRumana Ali100% (1)
- 1455-1 FullDocumento7 pagine1455-1 FullVeronica SbNessuna valutazione finora
- At Two: Was SeDocumento3 pagineAt Two: Was Seida ayu agung WijayantiNessuna valutazione finora
- TAYLOR 1984 AnaesthesiaDocumento3 pagineTAYLOR 1984 Anaesthesiapolly91Nessuna valutazione finora
- Jaundice and Pregnancy: Lessons From PracticeDocumento4 pagineJaundice and Pregnancy: Lessons From PracticeFranz Huber QueiroloNessuna valutazione finora
- 2Documento3 pagine2Liezl Ann BautistaNessuna valutazione finora
- Budd-Chiari Syndrome: A Clinical ApproachDocumento5 pagineBudd-Chiari Syndrome: A Clinical ApproachTrisNessuna valutazione finora
- Case 2Documento3 pagineCase 2Vivi DeviyanaNessuna valutazione finora
- Hypertension IN PregnanciesDocumento36 pagineHypertension IN Pregnanciesdaniel mitikuNessuna valutazione finora
- Anna C. Graml NUTN 515 Prof. Jessie Pavlinac: The Case of The "Enterocutaneous Fistula"Documento6 pagineAnna C. Graml NUTN 515 Prof. Jessie Pavlinac: The Case of The "Enterocutaneous Fistula"Athira SMNessuna valutazione finora
- PEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827Documento197 paginePEDIATRIC SURGERY - A Comprehensive Textbook For africa.-SPRINGER NATURE (2019) - 631-827adhytiyani putriNessuna valutazione finora
- Cirrhosis With Portal Hypertension in PregnancyDocumento2 pagineCirrhosis With Portal Hypertension in PregnancyIOSRjournalNessuna valutazione finora
- Vomiting With Failure To ThriveDocumento20 pagineVomiting With Failure To ThriveEmily EresumaNessuna valutazione finora
- GI Summer Review - Answers - Bosch (2013)Documento16 pagineGI Summer Review - Answers - Bosch (2013)Jessica MooreNessuna valutazione finora
- The Case: Canine Urinary Obstruction: Blood WorkDocumento5 pagineThe Case: Canine Urinary Obstruction: Blood WorkNicku MalanceaNessuna valutazione finora
- 3.4 Paralytic Ileus Due To Potassium Depletion. Dr. S. GieveDocumento3 pagine3.4 Paralytic Ileus Due To Potassium Depletion. Dr. S. GieveDaru KristiyonoNessuna valutazione finora
- Case Report: Elevated Amylase in ChildhoodDocumento2 pagineCase Report: Elevated Amylase in ChildhoodSava GabrielNessuna valutazione finora
- Case Report: Elevated Amylase in ChildhoodDocumento2 pagineCase Report: Elevated Amylase in ChildhoodSava GabrielNessuna valutazione finora
- Isolated Case of Chilaiditi SyndromeDocumento2 pagineIsolated Case of Chilaiditi SyndromeAthiyatunAnnisaNessuna valutazione finora
- Pregnancy - AppendicitisDocumento9 paginePregnancy - AppendicitisOnyekachi OjiakuNessuna valutazione finora
- Textbook of Pediatrics. 18th Ed. USA: Saunders Elsevier, 2632-2646Documento1 paginaTextbook of Pediatrics. 18th Ed. USA: Saunders Elsevier, 2632-2646Niluh Ita PasyantiNessuna valutazione finora
- Fourniers GangreneDocumento12 pagineFourniers GangreneNiluh Ita PasyantiNessuna valutazione finora
- Ileus ObstructiveDocumento14 pagineIleus ObstructiveNiluh Ita PasyantiNessuna valutazione finora
- Reti No Blast OmaDocumento11 pagineReti No Blast OmaNiluh Ita PasyantiNessuna valutazione finora
- Baba, 2010Documento7 pagineBaba, 2010Sabrine DwigintNessuna valutazione finora
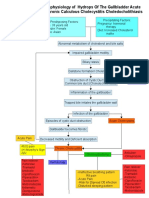
- Pathophysiology of CholecystitisDocumento2 paginePathophysiology of CholecystitisAnonymous gDp7y3Cl82% (22)
- Choledocal CystDocumento11 pagineCholedocal CystBilly JonatanNessuna valutazione finora
- Lista-OTC-25 11 2022Documento54 pagineLista-OTC-25 11 2022ValeraNessuna valutazione finora
- Date Year Hs Code Product QuantityunitDocumento45 pagineDate Year Hs Code Product QuantityunitProschool HyderabadNessuna valutazione finora
- Liver Structure Funciton QnsDocumento4 pagineLiver Structure Funciton QnsNoora AttariNessuna valutazione finora
- Liver Function Test: Presented By: Vikas Kumar JR-1Documento19 pagineLiver Function Test: Presented By: Vikas Kumar JR-1vikasNessuna valutazione finora
- He Pat EctomyDocumento4 pagineHe Pat Ectomysharjil chaudhryNessuna valutazione finora
- Liver Function Tests and How To Relate ThemDocumento82 pagineLiver Function Tests and How To Relate ThemG VenkateshNessuna valutazione finora
- Progressive Familial Intrahepatic Cholestasis in ChildrenDocumento3 pagineProgressive Familial Intrahepatic Cholestasis in ChildrenPaul HartingNessuna valutazione finora
- Atresia BilierDocumento11 pagineAtresia BilierLaura ChandraNessuna valutazione finora
- Approach To The Patient With Abnormal Liver Tests - UpToDateDocumento26 pagineApproach To The Patient With Abnormal Liver Tests - UpToDateGabrielle AndersonNessuna valutazione finora
- Chronic Liver Diseases & PLCCDocumento56 pagineChronic Liver Diseases & PLCCibnbasheer100% (5)
- Tratamiento Médico de Los Pólipos Vesiculares. Estudio PilotoDocumento3 pagineTratamiento Médico de Los Pólipos Vesiculares. Estudio Pilotomeche1989Nessuna valutazione finora
- Case Study Sa Surgical WardDocumento8 pagineCase Study Sa Surgical WardAiza ToledanaNessuna valutazione finora
- Acute CholecystitisDocumento3 pagineAcute CholecystitisًNessuna valutazione finora
- CC 2 Activity 2Documento5 pagineCC 2 Activity 2Valdez Francis ZaccheauNessuna valutazione finora
- Liver Fibrosis ProgressDocumento9 pagineLiver Fibrosis ProgressTaufik Rizkian AsirNessuna valutazione finora
- Safe Laparoscopic Cholecystectomy An Illustrated AtlasDocumento171 pagineSafe Laparoscopic Cholecystectomy An Illustrated AtlasText OK100% (2)
- Biliary Tree LectureDocumento58 pagineBiliary Tree Lecturesgod34Nessuna valutazione finora
- Hepatic Research PaperDocumento7 pagineHepatic Research Paperapi-349474075Nessuna valutazione finora
- Liver & Biliary DiseaseDocumento41 pagineLiver & Biliary Diseasesaump3Nessuna valutazione finora
- LIVER SlidesDocumento144 pagineLIVER SlidesChiiraq EugeneNessuna valutazione finora
- DILIDocumento14 pagineDILIfadi01234Nessuna valutazione finora
- 21 Obstructive JaundiceDocumento12 pagine21 Obstructive JaundicejumaymayaNessuna valutazione finora
- Gallbladder and Extrahepatic Biliary System - FinlDocumento14 pagineGallbladder and Extrahepatic Biliary System - FinlJoevet T. TadlasNessuna valutazione finora
- Caroli Disease and CholangiocarcinomaDocumento10 pagineCaroli Disease and CholangiocarcinomaDanielle Foster100% (1)
- HIV Drug Chart (2021)Documento1 paginaHIV Drug Chart (2021)savNessuna valutazione finora
- Pemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)Documento51 paginePemeriksaan Fungsi Hati .: Prof. Dr. Adi Koesoema Aman SPPK (KH)kiki rawitriNessuna valutazione finora
- Acute and Chronic CholecystitisDocumento10 pagineAcute and Chronic Cholecystitisissam_1994Nessuna valutazione finora
- RP CatatalogoDocumento15 pagineRP CatatalogoGram Farmacias GINessuna valutazione finora