Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
ADHD
Caricato da
kylieverCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
ADHD
Caricato da
kylieverCopyright:
Formati disponibili
Dr Diane Mullins, RCSI Tutor in Psychiatry, St Itas Hospital, Portrane
Attention deficit hyperactivity disorder (ADHD) / diagnosis and management of ADHD
Diagnostic criteria (DSM-IV)
Inattention
o Failure to give close attention to detail or makes careless mistakes in schoolwork,
work or other activities
o Difficulty sustaining attention in tasks or play
o Does not seem to listen when spoken to directly
o Does not follow through on instructions and failure to finish schoolwork or chores
o Difficulty organising tasks and activities
o Avoids, dislikes or reluctant to engage in tasks that require sustained mental effort
(i.e. schoolwork or homework)
o Looses things needed for tasks or activities (i.e. toys, school assignments, pencils,
books)
o Easily distracted by extraneous stimuli
o Forgetful in daily activities
Hyperactivity
o Fidgets with hands or feet or squirms in seat
o Leaves seat in classroom or other situations in which remaining seated expected
o Runs about or climbs excessively in situations in which it is inappropriate
o Difficulty playing or engaging quietly in leisure activities
o Often on the go or acts as if driven by a motor
o Talks excessively
Impulsivity
o Blurts out answers before questions have been completed
o Difficulty awaiting turn
o Interrupts or intrudes on others (i.e. butts into conversations or games)
Other criteria
o Symptoms present before age 7 years
o Symptoms present in two or more settings (e.g. school and at home)
o Impairment in social, academic or occupational functioning
o Symptoms do not occur exclusively during the course of a pervasive developmental
disorder, schizophrenia, or other psychotic disorder and are not better accounted for
by another mental disorder (e.g. mood disorder, anxiety disorder, dissociative disorder
or a personality disorder)
Epidemiology
Incidence in USA is 2-5%, while in the UK it is reported as 1%
Male > females
Aetiology
Genetics
o Both parents and siblings of a child with ADHD are more likely to have ADHD than
the general population
o conduct disorder and substance misuse in parents
Environmental
o Low birth weight, tobacco, alcohol and cocaine misuse during pregnancy
Neurological
o Functional imaging shows frontal metabolism & frontal lobe hypoperfusion
Neurotransmitters
o DA and NA dysregulation in prefrontal cortex
Psychosocial stress & family dysfunction
Comorbidity
Specific learning disorders (60%)
Dr Diane Mullins, RCSI Tutor in Psychiatry, St Itas Hospital, Portrane
Conduct disorder and oppositional defiant disorder (40%)
Substance misuse
Depression
Anxiety disorder
PTSD
OCD
Bipolar disorder
Tics
Tourettes syndrome
Bulimia
Dyslexia
Outcome
Approx 20% develop dissocial personality traits
15-20% develop substance misuse
High rates of suicidality
Poor self-esteem
Unemployment
ADHD symptoms may persist into adulthood
Inattention is often the last remitting symptom
Assessment (involve parent, child & school)
Interview with parents: full developmental history, medical and family history and assess
family functioning
Interview with child: evaluate for physical or comorbid psychiatric disorder and
assessment attachment style and level of activity
Collateral information from school. A school visit to observe behaviour in the classroom
may be useful
Connors Assessment Scale given to parents & teacher (= rating scale for ADHD)
Treatment
Biological
o CNS stimulants i.e. Methylphenidate (Ritalin) and Dextroamphetamine
Short, intermediate and long-acting stimulants exist
Side effects of Methylphenidate
Growth retardation
appetite & weight
sleep
BP & pulse changes (both or ), angina, cardiac arrhythmias
Chest pain
Confusion
Headaches
Hypersensitivity (rash, fever, arthralgia)
Rebound behaviour (when the effects of the medication begin to )
Tics / Tourettes syndrome
Depression
Irritability
Psychosis
Monitor for side effects of stimulants at each review, i.e. pulse, BP, weight,
height
The use of Drug Holidays is recommended i.e. withholding the drug on
weekends and during school holidays
o Atomoxetine (norepinephrine receptor inhibitor)
Dr Diane Mullins, RCSI Tutor in Psychiatry, St Itas Hospital, Portrane
Second line agents: antidepressants (i.e. bupropion and venlafaxine) and -adrenergic
receptor agnosist (i.e. clonidine)
Psychotherapy
o Social skills training, behavioural intervention, individual psychotherapy, family
therapy and special education when indicated
o
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Conners 3rd EditionDocumento11 pagineConners 3rd Editionapi-25939041967% (3)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Conners QuestionaireDocumento1 paginaConners QuestionaireSaiPremaVijayawadaNessuna valutazione finora
- DSM 5 - DSM 5Documento7 pagineDSM 5 - DSM 5Roxana ClsNessuna valutazione finora
- Achalasia: Department of MedicineDocumento21 pagineAchalasia: Department of Medicinekyliever100% (1)
- Usa Walnut Varieties 0Documento48 pagineUsa Walnut Varieties 0Oleg Tirsina100% (2)
- Hernia OSCE ExaminationDocumento3 pagineHernia OSCE ExaminationkylieverNessuna valutazione finora
- History:: Breast History and ExaminationDocumento4 pagineHistory:: Breast History and ExaminationkylieverNessuna valutazione finora
- An Overview of Cognitive Behavioral Therapy Webinar SlidesDocumento35 pagineAn Overview of Cognitive Behavioral Therapy Webinar Slideskyliever100% (1)
- OG 2.2 Anatomy of The Female Pelvis: Og 1.8 The Cardiotocograph Class Course Obstetrics and Gynaecology Code Title DateDocumento27 pagineOG 2.2 Anatomy of The Female Pelvis: Og 1.8 The Cardiotocograph Class Course Obstetrics and Gynaecology Code Title Datekyliever100% (2)
- Thyroid Gland OSCE ExaminationDocumento13 pagineThyroid Gland OSCE ExaminationkylieverNessuna valutazione finora
- ENT Emergency: James Paul O'NeillDocumento43 pagineENT Emergency: James Paul O'NeillkylieverNessuna valutazione finora
- OsteoarthritisDocumento40 pagineOsteoarthritiskylieverNessuna valutazione finora
- b2 s3 WritingDocumento8 pagineb2 s3 WritinglilalilakNessuna valutazione finora
- ENT EmergencyDocumento57 pagineENT EmergencykylieverNessuna valutazione finora
- First Grade Science Seasons LessonDocumento10 pagineFirst Grade Science Seasons Lessonapi-273149494100% (2)
- A Brief Legal History of Philippine EducationDocumento6 pagineA Brief Legal History of Philippine EducationZahjid CallangNessuna valutazione finora
- State and District Academic Standards Professional DevelopmentDocumento15 pagineState and District Academic Standards Professional Developmentapi-506887250Nessuna valutazione finora
- Thought Record Sheet AngerDocumento2 pagineThought Record Sheet AngerkylieverNessuna valutazione finora
- Psychopathy Checklist-Revised (PCL-R) : January 2016Documento5 paginePsychopathy Checklist-Revised (PCL-R) : January 2016kylieverNessuna valutazione finora
- Psychopathy Checklist: Screening Version (PCL:SV) : January 2016Documento5 paginePsychopathy Checklist: Screening Version (PCL:SV) : January 2016kylieverNessuna valutazione finora
- Wwa NodosumDocumento21 pagineWwa NodosumMu AbNessuna valutazione finora
- This Dysfunctional Thought Record Worksheet Is Divided Into 7 ColumnsDocumento2 pagineThis Dysfunctional Thought Record Worksheet Is Divided Into 7 ColumnskylieverNessuna valutazione finora
- Core Belief WorksheetDocumento1 paginaCore Belief WorksheetkylieverNessuna valutazione finora
- Pyoderma GangrenosumDocumento35 paginePyoderma GangrenosumkylieverNessuna valutazione finora
- AcromegalyDocumento2 pagineAcromegalykylieverNessuna valutazione finora
- Perinatal MedicineDocumento39 paginePerinatal MedicinekylieverNessuna valutazione finora
- PsychopathologyDocumento22 paginePsychopathologykylieverNessuna valutazione finora
- Diabetes Mellitus Type I DMI: Department of Family Medicine and General Practice RcsiDocumento25 pagineDiabetes Mellitus Type I DMI: Department of Family Medicine and General Practice RcsikylieverNessuna valutazione finora
- Maryam Fuad Ali - SC1 Obgyn: FibroidsDocumento1 paginaMaryam Fuad Ali - SC1 Obgyn: FibroidskylieverNessuna valutazione finora
- OG 1.3 - Preconception and Prenatal Care Jan 2015Documento19 pagineOG 1.3 - Preconception and Prenatal Care Jan 2015kylieverNessuna valutazione finora
- OG 1.4 - Normal Labour + Delivery - Jan 2015Documento20 pagineOG 1.4 - Normal Labour + Delivery - Jan 2015kylieverNessuna valutazione finora
- AutismDocumento3 pagineAutismkylieverNessuna valutazione finora
- Pediatric DermatologyDocumento10 paginePediatric DermatologykylieverNessuna valutazione finora
- Age Related Macular DegenerationDocumento26 pagineAge Related Macular DegenerationRebecca WongNessuna valutazione finora
- RecommendationDocumento1 paginaRecommendationAyush KumarNessuna valutazione finora
- Sosc1960 HkustDocumento4 pagineSosc1960 HkustMary LamNessuna valutazione finora
- V Turner Symbol Process SystemDocumento21 pagineV Turner Symbol Process SystemAlexandra Elizzabeth AndriesNessuna valutazione finora
- Future of Elearning in IndiaDocumento14 pagineFuture of Elearning in IndiaAnu Khurana ChawlaNessuna valutazione finora
- A Level Pure1 Oct2021 Mark SchemeDocumento27 pagineA Level Pure1 Oct2021 Mark Schememzino100406Nessuna valutazione finora
- Rebecca A. Endaya Beed-Iii Art Education: ExploreDocumento5 pagineRebecca A. Endaya Beed-Iii Art Education: ExploreBhecca Endaya0% (1)
- School Form 9 Report Card 2022Documento63 pagineSchool Form 9 Report Card 2022CYNTHIA CUSTODIONessuna valutazione finora
- Lipmans Thinking in Education PDFDocumento7 pagineLipmans Thinking in Education PDFLaura Nicoleta BorhanNessuna valutazione finora
- Sample of Form 4 English Daily Lesson Notes (For 21-25 Apr 2014)Documento3 pagineSample of Form 4 English Daily Lesson Notes (For 21-25 Apr 2014)globalventure557134100% (1)
- RA MASTERPLUMBING CDO July2018 PDFDocumento10 pagineRA MASTERPLUMBING CDO July2018 PDFPhilBoardResultsNessuna valutazione finora
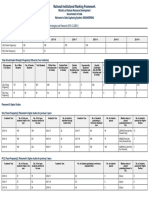
- Institute Name: Ambedkar Institute of Advanced Communication Technologies and Research (IR-E-C-32851)Documento7 pagineInstitute Name: Ambedkar Institute of Advanced Communication Technologies and Research (IR-E-C-32851)Ravi Ranjan KumarNessuna valutazione finora
- Wayne Visser: Speaker Biography Idea-Monger, Story-Teller, Meme-WeaverDocumento27 pagineWayne Visser: Speaker Biography Idea-Monger, Story-Teller, Meme-WeaverZola1348Nessuna valutazione finora
- PLC StrategiesDocumento3 paginePLC StrategiesGan Zi XiNessuna valutazione finora
- Madriaga, Rona Frances A.Documento6 pagineMadriaga, Rona Frances A.Jason L. Saldua,BSN,RNNessuna valutazione finora
- 2nd Periodical PerDevDocumento1 pagina2nd Periodical PerDevAbigail N. DitanNessuna valutazione finora
- EceDocumento67 pagineEceaditya_pundirNessuna valutazione finora
- 3 - Individual Differences Among LearnersDocumento8 pagine3 - Individual Differences Among LearnersDg HasmahNessuna valutazione finora
- Ciencias Sociales: Infinite Upware Soft S.A.SDocumento12 pagineCiencias Sociales: Infinite Upware Soft S.A.SSergio GarcíaNessuna valutazione finora
- Validacao Escala Espiritualidade Pinto - Pais RibeiroDocumento7 pagineValidacao Escala Espiritualidade Pinto - Pais RibeiroLucasFelipeRibeiroNessuna valutazione finora
- College of New Caledonia Application FormDocumento2 pagineCollege of New Caledonia Application Formdaljit8199Nessuna valutazione finora
- Abrams - Peirce, Kant, and Apel On Transcendental Semiotics. The Unity of Apperception and The Deduction of The Categories of SignsDocumento52 pagineAbrams - Peirce, Kant, and Apel On Transcendental Semiotics. The Unity of Apperception and The Deduction of The Categories of Signskafirun100% (1)
- Detailed Lesson Plan For Submission No 4Documento5 pagineDetailed Lesson Plan For Submission No 4Tromar Castillo LorestoNessuna valutazione finora
- Digital Footprint AssignmentDocumento2 pagineDigital Footprint AssignmentPAING LIN HTIKENessuna valutazione finora
- Basic National Education - Report of The Zakir Husain CommitteeDocumento205 pagineBasic National Education - Report of The Zakir Husain CommitteeMehwash DilshadNessuna valutazione finora
- Nwineh, L.1 & Okwelle, P.C.2 1Documento11 pagineNwineh, L.1 & Okwelle, P.C.2 1paul okwelleNessuna valutazione finora