Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Oxygen React...
Caricato da
hamzaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Oxygen React...
Caricato da
hamzaCopyright:
Formati disponibili
LETTERS TOTHE EDITOR
Higher levels of reactive oxygen species are
associated with anergy in chronic lymphocytic
leukemia
There is a growing interest in the role of reactive oxygen
species (ROS) in chronic lymphocytic leukemia (CLL) in
which tumor cells accumulate higher levels of such species
than do normal B cells.1-3 As in other cells, mitochondria
appear to be the main source of ROS and CLL cells have an
increased mitochondrial mass compared to that of normal
B cells.2,4 Higher levels of ROS confer increased sensitivity
to induction of apoptosis by agents which further enhance
ROS and it may be possible to exploit this as the basis for
new treatments.1,2,5
Although ROS levels are generally higher in CLL cells
than in normal B cells, the levels vary considerably
between patients samples.1-3,5,6 Analyses have mainly been
performed on samples from patients with more advanced
disease and, in that setting, prior therapy appeared to be a
major determinant of ROS levels.3,5,6 This may reflect a
direct effect of drugs on ROS production, perhaps linked to
accumulation of mitochondrial DNA damage.6 However, a
recent study demonstrated variable ROS levels in cells from
untreated patients2 indicating an influence of other factors.
The B-cell receptor (BCR) is now recognized as a key
determinant of variable behavior of CLL7 and is a target for
therapeutic attack. Antigen engagement appears to be iterative, with the outcome being either proliferation or anergy, a balance likely to influence disease outcome.7,8 Anergy
A
480
542
520a
494
560
343
393
476
Counts
ii
CM-H2DCFDA
Counts
PBMC
CD19+/CD5+
CM-H2DCFDA
ii
iii
Relative surface IgM
Ica2+ mobilization (% cells)
i
CM-H2DCFDA
Fluorescence (GeoMFI)
U-CLL M-CLL
CM-H2DCFDA
Fluorescence (GeoMFI)
iv
CM-H2DCFDA
Fluorescence (GeoMFI)
Figure 1. Inter-patient variability in ROS levels. (Ai) CLL peripheral blood monocuclear cells
(PBMC) were recovered from cryopreservation, rested for 3 h and then stained with CMH2DCFDA for 1 h at 37C prior to flow cytometric analysis. Representative results for six of
33 samples analyzed. Shaded areas represents unlabeled, control cells. Open areas represents CM-H2DCFDA-labeled cells. (Aii) As (Ai), except a proportion of the sample was additionally incubated with anti-CD19 and anti-CD5 antibodies prior to flow cytometry. (B)
Correlations between mean CM-H2DCFDA fluorescence (GeoMFI) in CLL PBMCs and (i) IGHV
mutation status; (ii) anti-IgM-induced calcium; (iii) sIgM expression and (iv) cell viability.
Results of statistical comparisons are shown. (i) Mann-Whitney test; (ii-iv) Spearman correlation.
Cell viability (%)
CM-H2DCFDA
Fluorescence (GeoMFI)
haematologica 2015; 100:e265
LETTERS TOTHE EDITOR
to segregate samples into two groups based on ROS levels
and correlations with time-to-first treatment (TTFT). Using
a ROC-derived cut-off of 2483, high ROS levels were associated with a significantly longer TTFT (Figure 2A). As
expected, expression of mutated IGHV genes (M-CLL) was
also associated with a significantly longer TTFT (Figure 2B).
A
Percent remaining
100
ROS > 2483
ROS < 2483
80
60
P=0.003
40
20
0
0
100 200 300
TTFT (months)
400
100
Percent remaining
is characterized by strong down-modulation of both
expression and function of sIgM, and is evident in all CLL
but predominates in cases expressing mutated IGHV genes
(M-CLL) and is associated with a good prognosis. By contrast, growth-promoting BCR signaling is more evident in
cases expressing unmutated IGHV genes (U-CLL) and is
associated with progressive disease. In this work, we investigated potential links between ROS, anergy and clinical
progression in CLL.
We used the ROS-sensitive fluorescent probe CMH2DCFDA to quantify ROS in peripheral blood mononuclear cells from 33 patients (Figure 1Ai and Online
Supplementary Table S1). ROS measurements were made on
singlet, viable cells (based on forward and side scatter in
flow cytometry analysis). We focused mainly (27/33) on
untreated patients to avoid perturbing effects of
chemotherapy, and the majority (27/33) had stage A disease. Samples generally contained a high proportion of
CD19+CD5+ CLL cells (median 93%) to reduce contamination by non-malignant cells. Moreover, combined staining
with CM-H2DCFDA and anti-CD19 and anti-CD5 antibodies in a subset of randomly selected samples demonstrated
that quantification of ROS in total peripheral blood
mononuclear cells and CD19+CD5+ cells yielded very similar results, including in sample 520A which contained
~80% CLL cells (Figure 1Aii). Repeat testing of samples on
separate occasions confirmed high reproducibility of CMH2DCFDA measurements (data not shown) and staining
with a mitochondrial ROS-specific probe confirmed that
CLL cells produced substantial levels of mitochondriaderived ROS (Online Supplementary Figure S1).2
ROS levels were highly variable between individual samples (Figure 1B and Online Supplementary Table S1). We first
compared ROS levels with IGHV status and detected relatively low but consistent expression within U-CLL, but significantly higher and more heterogeneous expression in
M-CLL (Figure 1Bi). There was also a significant negative
association with sIgM signaling capacity, pointing to a correlation with anergy which predominates in M-CLL (Figure
1Bii).8 There was also an inverse correlation between ROS
levels and sIgM expression (Figure 1Biii). Cell viability was
generally high (median 84%) in the samples. However,
there was a significant inverse correlation between ROS
levels and cell viability (Figure 1Biv).
We also investigated potential correlations between ROS
levels and disease behavior using Kaplan-Meier analysis.
Receiver operating characteristic (ROC) analysis was used
M-CLL
U-CLL
80
60
P=0.02
40
20
0
0
100 200 300
TTFT (months)
400
Figure 2. Association between elevated ROS and better prognosis.
(A) Kaplan-Meier analysis of correlation between mean CMH2DCFDA fluorescence (GeoMFI), as a measure of ROS, and time
to first treatment (TTFT). (B) Kaplan-Meier analysis of correlation
between IGHV mutation status and TTFT within the cohort of
patients studied.
B
P=0.03
ii
Relative CXCR4 (GeoMFI)
348
Counts
CM-H2DCFDA
CXCR4
Low
High
ROS level
haematologica 2015; 100:e266
Figure 3. Heterogeneity of ROS in
primary CLL. CLL samples were
recovered from cryopreservation,
rested for 3 h and then stained
with CM-H2DCFDA and anti-CD19,
anti-CD5 and anti-CXCR4 antibodies prior to flow cytometric analysis. (A) Representative flow analysis showing (i) CM-H2DCFDA fluorescence in CD19+CD5+ cells and
(ii) CXCR4 expression in ROSlow
and ROShigh sub-populations. (B)
Quantitative data for CXCR4
expression in ROSlow and ROShigh
sub-populations from four CLL
samples analyzed.
LETTERS TOTHE EDITOR
In addition to inter-sample variation, CM-H2DCFDA
staining also revealed intra-sample heterogeneity in ROS
levels (Figure 1Ai). Relatively discrete sub-populations were
detected in samples from 16/33 patients. Similar results
were obtained when we specifically quantified ROS in
CD5+CD19+ cells confirming that this heterogeneity exists
within the malignant clone (Figure 1Aii). Subpopulations
were somewhat more common in U-CLL (9/14) than in MCLL (7/19) although this difference was not statistically significant (data not shown).
We performed co-staining with CM-H2DCFDA and antiCXCR4 to probe the basis for intraclonal ROS heterogeneity. CXCR4 is strongly down-modulated following
CXCL12 engagement in tissues; reduced CXCR4 expression therefore marks cells that have recently emigrated
from tissues to blood.9,10 In 4/4 randomly selected samples
(3 M-CLL, 1 U-CLL), there was an inverse relationship
between CXCR4 and ROS and, on average, CXCR4
expression was 2.1-fold higher in ROSlow cells than in ROShi
cells (Figure 3A,B). Thus, ROS levels are higher within the
most recently released cells, suggesting that increased ROS
is a consequence of tissue-based stimulation.
Taken together, our results demonstrate that increased
ROS may be associated with anergy in CLL since ROS levels were highest in M-CLL, and in samples with strong
down-modulation of sIgM expression and function. CLL
anergy appears to be a feature of more indolent forms of
disease and high levels of ROS were also associated with
longer TTFT. Consistent with the idea that CLL anergy is
driven by antigen engagement within tissues,8 increased
ROS may also be a consequence of tissue-based stimulation since the highest levels of ROS were found in cells
with low CXCR4 that had been most recently released into
the circulation.9,10 Interestingly, gene expression profiling
revealed significant perturbation of ROS-related gene
expression between CXCR4lowCD5hi and CXCR4hiCD5low
sub-populations further supporting the idea that ROS production is a consequence of tissue-based stimulation
in vivo.10
The mechanisms that mediate increased levels of ROS in
anergic CLL cells remain unclear. One possibility is that
increased ROS is a consequence of anergy-promoting, antigen interactions acting via the BCR. We attempted to measure effects of anti-IgM stimulation on ROS levels of CLL
cells using CM-H2DCFDA (to quantify total ROS) or a
sIgM-localizing ROS probe, to specifically quantify ROS in
the vicinity of activated sIgM.11 However, we were unable
to detect consistent changes in ROS levels using either
approach (data not shown). Given the relatively low signaling capacity of CLL cells, more sensitive, regiospecific
probes will be required for meaningful investigation of
direct effects of sIgM of ROS production in CLL cells
in vitro. Moreover, responses induced by anti-IgM in
responsive samples in vitro most closely resemble positive,
growth-promoting signal responses and may therefore not
adequately model anergy-promoting antigen responses
in vivo.
Increased ROS may be a consequence of increased production and/or decreased metabolism via cellular antioxidant protective mechanisms. Mitochondrial-derived ROS
are mainly produced as a by-product of mitochondrial respiration and BCR signaling is known to modulate metabolism, including oxidative phosphorylation, with differences
between nave and anergic B cells.12 Thus, differences in
metabolism, perhaps linked to changes in mitochondrial
mass,2,4 between individual CLL samples may explain, at
least in part, variation in ROS levels. It is also possible that
ROS production may be linked to apoptosis. Interestingly,
although the viability of the samples studied was generally
high, we did identify a significant inverse correlation
between ROS levels and the proportion of viable cells. One
possibility is that increased ROS may be a consequence of
activation of cell death pathways. Alternatively, high levels
of ROS in CLL cells may promote susceptibility to apoptosis. Indeed, antioxidants can decrease CLL cell apoptosis.13,14
Although anergy is apparently benign, it is a reversible
state and anergic CLL cells may act as a reservoir of cells
which may be subject to subsequent growth-promoting
antigen signaling and/or acquire secondary genetic alterations.15 Regardless of the underlying mechanisms, the
observation that ROS are increased in anergic CLL cells
suggests that targeting anergic CLL cells using agents that
further elevate ROS levels may be an approach for selective
induction of apoptosis and allow effective elimination of
this important reservoir of malignant cells.
Adam Linley,1 Beatriz Valle-Argos,1 Andrew J. Steele,1
Freda K. Stevenson,1 Francesco Forconi,1,2
and Graham Packham1
1
Cancer Research UK Centre, Cancer Sciences Unit, University
of Southampton Faculty of Medicine, Southampton General
Hospital; and 2Department of Haematology, University Hospital
Southampton, UK
Acknowledgments: we are extremely grateful to the patients
involved in this study for the kind gift of their samples. We are very
grateful for the generous support of Drs Andrew Duncombe, Abraham
Jacob and Henri Grech and their associated clinical teams. We are also
very grateful for the support of Kathy Potter, Isla Henderson and Ian
Tracy.
Funding: this work was supported by Leukaemia and Lymphoma
Research, the CLL Global Research Foundation, Cancer Research UK,
the Southampton Experimental Cancer Medicine Centre and the
University of Southampton.
Correspondence: a.j.linley@soton.ac.uk
doi:10.3324/haematol.2014.120824
Key words: reactive oxygen species, ROS, anergy, chronic lymphocytic leukemia.
Information on authorship, contributions, and financial & other disclosures was provided by the authors and is available with the online version
of this article at www.haematologica.org.
References
1. Trachootham D, Zhang H, Zhang W, et al. Effective elimination of
fludarabine-resistant CLL cells by PEITC through a redox-mediated
mechanism. Blood. 2008;112(5):1912-1922.
2. Jitschin R, Hofmann AD, Bruns H, et al. Mitochondrial metabolism
contributes to oxidative stress and reveals therapeutic targets in
chronic lymphocytic leukemia. Blood. 2014;123(17):2663-2672.
3. Tomic J, Lichty B, Spaner DE. Aberrant interferon-signaling is associated with aggressive chronic lymphocytic leukemia. Blood. 2011;
117(9):2668-2680.
4. Carew JS, Nawrocki ST, Xu RH, et al. Increased mitochondrial biogenesis in primary leukemia cells: the role of endogenous nitric oxide
and impact on sensitivity to fludarabine. Leukemia. 2004;
18(12):1934-1940.
5. Zhou Y, Hileman EO, Plunkett W, et al. Free radical stress in chronic
lymphocytic leukemia cells and its role in cellular sensitivity to ROSgenerating anticancer agents. Blood. 2003;101(10):4098-4104.
6. Carew JS, Zhou Y, Albitar M, et al. Mitochondrial DNA mutations in
primary leukemia cells after chemotherapy: clinical significance and
therapeutic implications. Leukemia. 2003;17(8):1437-1447.
7. Packham G, Krysov S, Allen A, et al. The outcome of B-cell receptor
signaling in chronic lymphocytic leukemia: proliferation or anergy.
Haematologica. 2014;99(7):1138-1148.
8. Mockridge CI, Potter KN, Wheatley I, et al. Reversible anergy of
sIgM-mediated signaling in the two subsets of CLL defined by VHgene mutational status. Blood. 2007;109(10):4424-4431.
haematologica 2015; 100:e267
LETTERS TOTHE EDITOR
9. Coelho V, Krysov S, Steele A, et al. Identification in CLL of circulating
intraclonal subgroups with varying B-cell receptor expression and
function. Blood. 2013;122(15):2664-2672.
10. Calissano C, Damle RN, Marsilio S, et al. Intraclonal complexity in
chronic lymphocytic leukemia: fractions enriched in recently
born/divided and older/quiescent cells. Mol Med. 2011;17(1112):1374-1382.
11. Capasso M, Bhamrah MK, Henley T, et al. HVCN1 modulates BCR
signal strength via regulation of BCR-dependent generation of reactive oxygen species. Nat Immunol. 2010;11(3):265-272.
12. Caro-Maldonado A, Wang R, Nichols AG, et al. Metabolic repro-
gramming is required for antibody production that is suppressed in
anergic but exaggerated in chronically BAFF-exposed B cells. J
Immunol. 2014;192(8):3626-3636.
13. Steele AJ, Jones DT, Ganeshaguru K, et al. The sesquiterpene lactone
parthenolide induces selective apoptosis of B-chronic lymphocytic
leukemia cells in vitro. Leukemia. 2006;20(6):1073-1079.
14. Nilsson J, Soderberg O, Nilsson K, et al. Thioredoxin prolongs survival of B-type chronic lymphocytic leukemia cells. Blood. 2000;
95(4):1420-1426.
15. Caligaris-Cappio F. Anergy: the CLL cell limbo. Blood. 2014;
123(21):3214-3215.
haematologica 2015; 100:e268
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- ESU Mauritius Newsletter Dec 2014Documento8 pagineESU Mauritius Newsletter Dec 2014Ashesh RamjeeawonNessuna valutazione finora
- Atul Bisht Research Project ReportDocumento71 pagineAtul Bisht Research Project ReportAtul BishtNessuna valutazione finora
- MasterMind 1 Unit 5 Extra LifeSkills Lesson 2Documento2 pagineMasterMind 1 Unit 5 Extra LifeSkills Lesson 2Hugo A FENessuna valutazione finora
- Annexure 8: Medical Certificate (To Be Issued by A Registered Medical Practitioner) General ExpectationsDocumento1 paginaAnnexure 8: Medical Certificate (To Be Issued by A Registered Medical Practitioner) General ExpectationsMannepalli RamakrishnaNessuna valutazione finora
- Technique Du Micro-Enseignement Une Approche PourDocumento11 pagineTechnique Du Micro-Enseignement Une Approche PourMohamed NaciriNessuna valutazione finora
- Julie Jacko - Professor of Healthcare InformaticsDocumento1 paginaJulie Jacko - Professor of Healthcare InformaticsjuliejackoNessuna valutazione finora
- GB BioDocumento3 pagineGB BiolskerponfblaNessuna valutazione finora
- Oxford Reading Circle tg-4 2nd EditionDocumento92 pagineOxford Reading Circle tg-4 2nd EditionAreeb Siddiqui89% (9)
- Uptime Elements Passport: GineerDocumento148 pagineUptime Elements Passport: GineerBrian Careel94% (16)
- Sample Midterm ExamDocumento6 pagineSample Midterm ExamRenel AluciljaNessuna valutazione finora
- Fundamental Rights-Right To Equality, Prohibition of Discrimination, Right To Equality of OpportunityDocumento76 pagineFundamental Rights-Right To Equality, Prohibition of Discrimination, Right To Equality of OpportunityutkarshNessuna valutazione finora
- Introduction To ICT EthicsDocumento8 pagineIntroduction To ICT EthicsJohn Niño FilipinoNessuna valutazione finora
- Mathsnacks05 InfiniteDocumento1 paginaMathsnacks05 Infiniteburkard.polsterNessuna valutazione finora
- Conrail Case QuestionsDocumento1 paginaConrail Case QuestionsPiraterija100% (1)
- Shielded Metal Arc Welding Summative TestDocumento4 pagineShielded Metal Arc Welding Summative TestFelix MilanNessuna valutazione finora
- Islamic Meditation (Full) PDFDocumento10 pagineIslamic Meditation (Full) PDFIslamicfaith Introspection0% (1)
- Marketing PlanDocumento41 pagineMarketing PlanMark AbainzaNessuna valutazione finora
- Final Report - Solving Traveling Salesman Problem by Dynamic Programming Approach in Java Program Aditya Nugroho Ht083276eDocumento15 pagineFinal Report - Solving Traveling Salesman Problem by Dynamic Programming Approach in Java Program Aditya Nugroho Ht083276eAytida Ohorgun100% (5)
- Counselling and PsychotherapyDocumento12 pagineCounselling and PsychotherapyD.Sreenivasa ReddyNessuna valutazione finora
- Enunciado de La Pregunta: Finalizado Se Puntúa 1.00 Sobre 1.00Documento9 pagineEnunciado de La Pregunta: Finalizado Se Puntúa 1.00 Sobre 1.00Samuel MojicaNessuna valutazione finora
- Time Interest Earned RatioDocumento40 pagineTime Interest Earned RatioFarihaFardeenNessuna valutazione finora
- Equine PregnancyDocumento36 pagineEquine Pregnancydrdhirenvet100% (1)
- Counselling Goes To The Movies: Antwone Fisher (2002)Documento12 pagineCounselling Goes To The Movies: Antwone Fisher (2002)Azizul MohamadNessuna valutazione finora
- Percy Bysshe ShelleyDocumento20 paginePercy Bysshe Shelleynishat_haider_2100% (1)
- Contents Serbo-Croatian GrammarDocumento2 pagineContents Serbo-Croatian GrammarLeo VasilaNessuna valutazione finora
- Insomnii, Hipersomnii, ParasomniiDocumento26 pagineInsomnii, Hipersomnii, ParasomniiSorina TatuNessuna valutazione finora
- Fansubbers The Case of The Czech Republic and PolandDocumento9 pagineFansubbers The Case of The Czech Republic and Polandmusafir24Nessuna valutazione finora
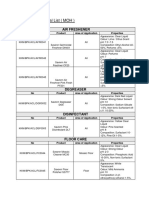
- Thermal Properties of Matter: Centre For Sceince StudyDocumento37 pagineThermal Properties of Matter: Centre For Sceince StudySalam FaithNessuna valutazione finora
- Approved Chemical ListDocumento2 pagineApproved Chemical ListSyed Mansur Alyahya100% (1)
- Insung Jung An Colin Latchem - Quality Assurance and Acreditatión in Distance Education and e - LearningDocumento81 pagineInsung Jung An Colin Latchem - Quality Assurance and Acreditatión in Distance Education and e - LearningJack000123Nessuna valutazione finora