Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
A&P 302 Heart Lecture Notes
Caricato da
BethanyCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
A&P 302 Heart Lecture Notes
Caricato da
BethanyCopyright:
Formati disponibili
A&P 302 Heart Lecture Notes:
If heart muscle become ischemic it doesnt work as well then pts
start experiencing chest pain then part of the muscle dies if it lasts
long enough (MI)
The heart has a VARIBLE demand for O2. At rest, it doesnt require
much.
There are 2 components that change the demand for of O2
1) The FASTER the heart rate the MORE O2 consumed and
2) Contractility, the heart has the ability to beat harder if necessary (if
it beats header = more O2 used)
Heart w/ O2 deficit look at two sides
1) how much is the heart burning,
2) how much is being supplied
The Heart Function:
Circulates blood
Also has endocrine function (produces hormone)
The Heart Size:
About the size of the fist
250 350 grams
There are 2 ways for the heart to become enlarged
1) It gets bigger on outside (causing the muscle to get thin = cant
contract as well) why? d/t chronic O2 deprivation or viral infection
(especially in young people) or,
2) The muscle can get very thick why would it get thicker? Higher BP
makes the heart thick
Heart DOSENT base contractility based on O2 demand
The Heart Location:
Enclosed in the mediastinum
2/3 lie left of the midsternal line
Extends from the 2nd rib to the 5th intercostal space
o Just left of the nipple exists the point of maximal intensity (PMI)
o PMI if it is enlarged you will feel it move
Base is on top, apex is on bottom
Heart should be half the size of the chest
What else would change position of heart in chest? Pneumothorax
The Heart Coverings:
Enclosed by the pericardium
2 layers
1) Fibrous pericardium
2) Serous pericardium
There are actually two serous pericardium
The Heart Fibrous Pericardium:
Protects the heart
Anchors the heart to surrounding structures
Prevents over filling of the heart!!
Fibrous pericardium is made of collagen and does NOT stretch
(remember: collagen has a high tensile strength)
How hard the heart beats is due in part to how much blood is IN the
heart. The heart stretches as blood is put in.
And remember, cardiac muscle is somewhere between skeletal and
smooth muscle. If you stretch it a little bit it works better, but if you
stretch it too much and it wont work
How does it fill with blood?? Workhorse is the Ventricle (have to
prevent overfilling)!
The Heart Serous Pericardium:
Parietal layer
o Parietal layer does NOT cover the body wall
Visceral layer or epicardium
Serous Pericardium Parietal Layer:
At the superior margin attaches to the large arteries
Serous Pericardium Visceral Layer:
Cover the external surface of the heart
Also known as the epicardium
Serous Pericardium Pericardial Cavity:
Slitlike cavity between the visceral and serous layer
Acts as a lubricant
There is a little bit of fluid in between the serous pericardium (it acts
as lubricant) you can get inflammation in there
Too much fluid around the heart (pericardial cavity) = heart wont be
able to properly fill = cardiac tamponade this is an EMERGENCY!!
The Heart Layers of the Heart:
1) Epicardium
On the outside, often infiltrated with fat
2) Myocardium
3) Endocardium
Layers of the Heart Epicardium:
Visceral layer of the serous pericardium
Often infiltrated with fat
o Why would you want to have fat around the heart? protects
against mechanical trauma
Layers of the Heart Myocardium:
2 components:
1) Cardiac muscle
2) Fibrous skeleton of the heart
Myo = muscle
Myocardium Cardiac Muscle:
The layer that contracts
Tissues fibers are arranged in spirals or circular bundles
Muscle cells are tethered to each other by crisscrossing connective tissue
Has to contract from the bottom and work its way up that way it
doesnt pinch itself off
Myocardium Fibrous Skeleton of the Heart:
Network of collagen and elastin fibers
Provides additional support to the great vessels and the valves
Anchors the cardiac muscles
o Anchors muscles so that when they contract it gives a meaningful
movement
Layers of the Heart Endocardium:
Glistening white sheet of endothelium
o Remember, endothelium also lines the BLOOD vessels
o Why is the heart also lined with this? Because during embryologic
development the heart starts off as one long blood vessel
Continuous with the endothelial lining of the blood vessels
The Heart Components:
Knowing blood flow, will be helpful on the practical!
Two superior atria
o Atria is extremely thin and very tiny! It is more or less just a
holding sac for blood
Two inferior ventricles
Interatrial septum
Interventricular septum
Flow of Blood:
Blood Comes/enter in through the inferior and superior vena cava then
enters right atrium travels through the right AV valve into the right
ventricle from right ventricle it travels through the pulmonic valve into
the pulmonary trunk (then it come through the lungs and enters the
pulmonary veins) from the pulmonary veins blood enters the left atrium
then goes through the left AV valve into the left ventricle from the left
ventricle goes through the aortic valve into the aorta
The Heart Atria:
Externally small protruding appendages called auricles
o Q on Test! - these is another embryologic remnant known as
the auricle it looks like a honeycomb on the inside it has
ZERO function, just from when you were in utero
Internally has 2 parts
o Smooth walled posterior part
o Ridged anterior wall containing pectinate muscles
o Picante muscles is the most missed question on the test
AND practical
o The PECTINATE MUSCLES are in the atria!
o The PAPILLARY MUSCLES are in the ventricles!
Atria Internal Structure:
Anterior and posterior divided by a C-shaped ridge called the crista terminalis
Interatrial septum has a shallow depression called the fossa ovalis remnant of the
foramen ovale
The intratrial septum has a hole embryonically that is known as the
foramen ovale, when your born its called the fossa ovalis why do we
have it? Embryos dont breathe, but you want blood to go from left to
the right side of heart skipping the lungs
In the fetus the RIGHT side generates more pressure.
Left side of heart at rest generates 7x more pressure than the right
side.
Kids with hole in heart usually the fossa ovalis just didnt close off
But if it closes off too soon the baby will die in utero
Atria Functional Structure:
Receiving chamber for blood returning to the heart
Contract minimally therefore walls are very thin
70% of filling that takes place is PASSIVE
30% is the atria contracting = atrial kick
Atria Venous Return Right:
Superior vena cava drains everything above the diaphragm
Inferior vena cava blood returns from below the diaphragm
Coronary sinus collects blood from the myocardium
o Coronary sinus the heart muscle is too thick for the blood going
through it to supply it with oxygen, so it has to have its own
blood supply.
o Coronary arteries supply blood to the heart muscle, but it has to
return to the right atrium, does this via the coronary sinus
o Right atrium has 3 things drain into it, the superior vena cava,
inferior vena cava, and the coronary sinus
Atria Venous Return Left:
4 pulmonary veins
The Heart Ventricles:
Makes up most of the volume of the heart
Right ventricle forms the anterior surface of the heart, left ventricle dominates the
posteroinferior surface
Ventricles - Biggest part, thickest part, its what generates the pressure
Right does NOT generate as much pressure as left, important d/t the
thickness of the left myocardium vs the right It doesnt have to be as
thick
Ventricles Internal:
Irregular ridges of muscles called trabeculae carneae
Cone like papillary muscles attached to valves
Papillary muscles are attached to valves by the chordae tendineae
Ventricles Structure:
Very thick myocardium
Ventricles Flow:
Right ventricle pumps blood through the pulmonary trunk
Left ventricle ejects blood into the aorta
The Heart Pathways:
Pulmonary circuit right side
Systemic circuit left side
The Heart Pulmonary Circuit:
Receives oxygen depleted, carbon dioxide rich blood
Short, low pressure system
Blood goes through and returns from the lungs
You dont want a lot of pressure going into the lungs (eg primary
pulmonary hypertension)
The Heart Systemic Circuit:
Oxygenated blood returns via the pulmonary vein
High pressure, long system
Encounters 5 (he says 7x) times as much pressure
The Heart Coronary Circulation:
The heart receives very little nourishment from the blood going through the circuits
Myocardium is to thick to be served by the blood going through the heart
Provides O2 to the heart itself
Coronary artery bypass graft (CABG) done when there is a problem
with coronary circulation
Coronary Circulation Delivery of Blood:
Delivery is impeded during contraction
Extremely important principle! Lots of physiologic principles will be on
the test, if you can follow logic it will be easier.
The coronary arteries ONLY provide O2 to the heart when the heart is at
REST (in between beats) for 2 reasons
1) When the heart contracts arteries are pinched off
2) The aortic valve is like a cup, when it opens it is filled with blood,
when the valve is closed it rests against the aorta where the
coronary artery is
ON TEST:
o Myocardium compresses the arteries
o The open aortic valve blocks the entrances to the coronary arteries
When heart is at REST that is filling time = diastole
When it beats = systole
Whats wrong with this system? With the heart and specifically HR, the
filling time gets shorter when the heart is using more O2. When the
heart is beating faster the filling time is shorter and it is giving itself
less blood.
Coronary Circulation Arterial Components:
Left coronary artery
o Anterior interventricular artery
o Circumflex artery
Right coronary artery
o Marginal artery
o Posterior interventricular artery
HAVE to be able to tell which part of the heart is serves
Coronary Circulation Left Coronary Artery:
Arises from the base of the aorta
Runs toward the left side of the heart
Left Coronary Artery Anterior Interventricular Artery:
Location follows the anterior interventricular sulcus
Serves interventricular septum and the anterior wall of each ventricle
Aka: left anterior descending (LAD)
Interventricular artery runs right over the ventricular septum so it
serves both the right and left ventricle its called anterior because the
heart is tilted a little bit
Left Coronary Artery Circumflex Artery:
Location follows the inferior portion of the left atrium posteriorly
Serves left atrium and the posterior wall of the left ventricle
How to remember outside of circle is called circumference this one
goes in a circle in a grove between the atria and it serves both the left
atrium and left ventricle
Coronary Circulation Right Coronary Artery:
Originates at the base of the aorta
Courses the right side of the heart
Right Coronary Artery Marginal Artery:
Location anteroinferior portion of the heart
Serves lateral right side of the heart
At the bottom of the heart
Right Coronary Artery Posterior Interventricular Artery:
Location posterior heart
Serves the posterior ventricular wall
Mirror image of the anterior ventricular artery, it also serves the left
and right ventricle
Why is it important to remember? With MI it is usually d/t a blockage
with one of these arteries its how you read an EKG.
Coronary Circulation Cardiac Veins:
Coronary sinus
o Great cardiac vein
o Middle cardiac vein
o Small cardiac vein
Anterior cardiac vein drains directly into the right atrium
Dont have to remember all these veins except for the anterior cardiac
vein
Anterior cardiac vein also drains directly into the right atrium.
Coronary Sinus Tributaries: DONT have to know where they drain!
Great cardiac vein in the anterior ventricular sulcus
Middle cardiac vein in the posterior ventricular sulcus
Small cardiac vein runs along the hearts inferior margin
Venous Circulation Anterior Cardiac Vein:
Empties directly into the right atrium
Heart Valves Components:
Atrioventricular valves
o Tricuspid
o Bicuspid or mitral
Semilunar valves
o Aortic semilunar
o Pulmonary semilunar
Picture is important, look and see the aortic valve is right in the middle.
Top is anterior, bottom is posterior. The most anterior structure is the
pulmonary trunk
Also acceptable to say right and left AV valve
Big difference between sets of valves AV valves are leaflets attached
to chordae tendineae. Pressure closes them
Semilunar valves are CUSPS, there are no strings attached to them.
Blood closes them (they fill up with blood)
Atrioventricular Valves Function/Structure:
Prevents backflow into the atria when the ventricles are contracting
Closes with building pressure
Chordae tendinae an anchoring cable
Papillary muscle the anchor the chordae tendinae is attached to
Act to keep valves closed
Ventricle fills with blood and starts to contract, -- pressure gets higher
and the valves come up together and shut
The chordae tendineae prevents the valve from opening up the other
way would cauue a murmur or regurgitation
Atrioventricular Valves Tricuspid Valve:
Right side
Three flexible cusps
Atrioventricular Valves- Bicuspid or Mitral Valve:
Left side
Two flexible cusps
Mitral valve prolapse usually seen in women late teens, early 20s.
Cardinal sign is hearing a clicking sound. Midsystolic click (heard in the
middle of the heart sounds). Doesnt cause any problems.
If there are problems its usually atypical chest pain
With angina really isnt painful its a heavy pressure on the chest.
Atypical chest pain would be a sharp chest pain NOT MI related (you
dont get sharp pain with MI), but you also see tachycardia with
atypical chest pain
Mitral valve syndrome people with it are strange?
Semilunar Valves Function/Structure:
Prevents backflow into the ventricles
Opens when interventricular pressure rises above arterial pressure
Three pocket like cusps
When the ventricle relaxes the cusps fill with blood and close
Has the cusps, fills with blood 3 cusp for each
Ventricles contract and pushes blood out. When heart stops beating,
pressure drops
The Heart Cardiac Muscle Fibers:
Striated
Cells are short, fat, branched, and interconnected
Intercellular space is filled with loose connective tissue matrix that acts as
a tendon and an insertion
Cardiac Muscle Fibers Functional Structure:
Membranes interlock with adjacent fibers junctions are called intercalated discs
Intercalated discs contain desmosomes and gap junction
Myocardium acts as a single coordinated unit! Heart contracts by an
organ, the whole organ contracts at the same time. WIL BE ON TEST!!!
Desmosomes are seen in areas of high mechanical stress, it anchors
Contraction Cardiac vs. Skeletal:
Means of Stimulation
Organ vs Motor Unit Contraction
Refractory Period
Excitation-Coupling
Cardiac vs. Skeletal Means of Stimulation:
Skeletal muscle is innervated by a nerve
Cardiac muscle has self excitable tissue that cycle producing automaticity
Cardiac vs. Skeletal - Contraction
Skeletal a motor unit contracts
Cardiac the whole organ contracts
Cardiac vs. Skeletal Refractory Period:
Skeletal lasts 250ms slower d/t the alternating motor units contracting
Cardiac lasts 1 2ms
Refractory period is shorter in heart than skeletal muscle
After you fire an action potential there is a refractory period where it
cant fire any more
Cardiac vs. Skeletal Excitation-Coupling:
Skeletal and cardiac are the same except:
o When sodium gates open so do slow calcium gates supplying 20% of the total
calcium needed.
- This triggers the release of calcium from the sarcoplamsic reticulum.
Gap junctions are what allows the organ to contract as a whole organ.
They are just holes that calcium is allowed to pass through
The Heart Energy Requirement:
Cardiac muscle can only utilize the aerobic pathway
Readily able to adapt to whatever fuel is available
2 important points.
1) Heart can use ANY nutrient available,
2) but it is aerobic, it HAS to have oxygen
2 terms if not enough oxygen to tissue
1) hypoxia not enough adequate oxygen supply going IN
2) ischemia not necessarily to due with the amount of oxygen going
it, instead it has used too much. VERY important, the balance
cannot use more oxygen than what is being supplied
The Heart Regulation of Rate:
Sympathetic and parasympathetic innervation alters the heart rate
In the absence of autonomic innervation, the heart continues to beat regularly
Ischemia vs infarction
- Ischemia not getting enough o2 but cells are still alive, goes
to infarction if too log and the cells die.
- MI means muscle cells have died
How to know if pt has MI? EKG will suggest it, but not
definitive. Will see products from the dead cells in the
blood, that is the definitive way to tell
Sinoatrial node is in the atrium it is the pacemaker of the heart.
Do NOT have to have a brain to have the heart beat.
What causes HR to vary?
- The autonomic NS, the sympathetic NS increases the HR, the
parasympathetic NS decreases HR
One minor thing that goes with that, the sympathetic system can get
he HR over 100
The parasympathetic system should NOT get the HR below 60
Autonomic system the HR would stay around 100
If you turn it on and youre at rest it should stay at 100. At rest the
parasympathetic NS controls heart rate its called Autonomic tone.
Epinephrine comes to the heart from 2 places
1) directly from the nerves itself and
2) adrenal medulla and enters the blood
Rate is regulated by the intrinsic cardiac conduction system
The heart contains autorhythmic cells
Regulation of Rate Autorhythmic Cells:
Have an unstable resting potential
Continuously depolarizes
Membrane changes are called pacemaker potentials or prepotentials
Autorhythmic cells if looking at Sinoatrial node it goes to resting
membrane potential right after firing off one, but it immediately starts
to depolarize immediately on its own
Your HR is dependent on how fast the SA node fires off action
potentials
Regulation of Rate Sequence of Excitation:
1) Sinoatrial node
2) Atrioventricular node
3) Atrioventricular bundle
4) Right and left bundle branches
5) Purkinje fibers
Sequence of events where SA node finally starts and were it ends up
Intranodial pathway
Sequence of Excitation Sinoatrial Node (SA):
Crescent shaped
Located in the right atrial wall just inferior to the entrance of the vena cava
The hearts pacemaker
Produces sinus rhythm
If someone has a Regular HR, then it is known as having normal sinus
rhythm (NSR).
In sinus rhythm denotes that the SA node is running the show.
Sequence of Excitation Atrioventricular Node:
Located in the inferior interatrial septum above the tricuspid valve
The depolarization wave spreads from the sinoatrial node to the atrioventricular node by
the internodal pathway
Impulse is delayed for about 0.1 seconds
Delay allows for atria to contract and fill the ventricle before the ventricle
contracts
Atria cannot generate a lot of pressure, the ventricles can because
they are thick walled.
Blood pressure from low to high
If atria and ventricles are contracting at the same time which way will
blood flow? Into the atrium, dont want to flowing back (regurgitation)
So you contract atria first and then the ventricle by the AV node
action potential goes there and is delayed 0.1 seconds
Sequence of Excitation Atrioventricular Bundle:
Located in the superior part of the interventricular septum
The only electrical connection between the atria and ventricles
Also called the bundle of His
AV bundle = the Bundle of His
Goes to the septum there are two bundles the left and right
Bundle branch block one of the two bundles arent conducting the
impulse anymore (can have either left or right bundle branch block but
CANT have both because the heart wouldnt beat, you would die if it
happens)
Buddle branches first point where you see contraction of muscle. First
see the septum contract so that it doesnt move to the left or right
(since on side is stronger than the other) to get the most amount blood
out.
But no matter how hard the ventricles contracts it wont get ALL the
blood out
Sequence of Excitation Right and Left Bundle Branches:
Atrioventricular bundle goes a short distance and then splits
The bundle branches course along the interventricular septum to the apex of the heart
Excites septal cells
First part of the conduction system to start a muscle contraction
Sequence of Excitation Purkinje Fibers:
Complete the pathways through the interventricular septum, heart apex, and ventricular
walls in that order
Also supplies the papillary muscles Papillary muscle contract and hold the
valve so it doesnt pop open
Regulation of Rate Modifying that Basic Rhythm:
Sympathetic
Parasympathetic
Modifying Basic Rhythms Sympathetic: From a clinical standpoint this
is the most important slide in the whole lecture.
Cardioacceleratory center
T1 T5 level
Norepinephrine from the adrenal medulla
Innervates the sinoatrial node, atrioventricular node, heart muscle, and
coronary arteries
Increases heart rate and contractility
o Contractility is how hard the muscle works.
o It is variable.
o Important thing, how hard the heart beats is in relation to how
much O2 it is using (beating harder = more O2). One of the two
things that can increase O2 consumption with the other being HR.
o If you increase HR and contractility increase oxygen demand
(increase myocardial oxygen consumption)
o Why is this a bad thing? Oxygen delivery decreases as HR and
contractility increase
o Epinephrine causes arteries to constrict EXCPT for coronary
arteries which dilate. But it doesnt matter because
1) they are closed off by the aortic valve and
2) the contract muscle is squeezing the muscle shut when the
heart is working
Dilates the coronary arteries
Modifying Basic Rhythms Parasympathetic:
Vagus nerve
Innervates the sinoatrial and atrioventricular node
Decreases the heart rate
Questionably decreases contractility
Equally important as last slide
Innervates the SA and AV node so it decreases the HR
Vagal response HR and respiratory drop and pt passes our
Talk about BP:
Anything over 140 hypertension, and anything over 80 is too high
Can see some pt with high systole and normal diastole isolated
systolic hypertension normally seen in elderly
Treating high BP the FIRST thing you do is take away sodium. Other
risk factor is obesity. Hypertension is a silent killer, if they get
symptoms like headache they are getting ready to die.
Only see high blood pressure in elderly is US with salt intake
The Heart The Cardiac Cycle:
Systole contraction
Diastole rest/filling
o Thing of diastole in terms of filling filling the ventricle but also
the coronary arteries
Cardiac cycle is EXTEREMLY!!!! Important for understanding
Talk about BP:
Anything over 140 hypertension, and anything over 80 is too high
Can see some pt with high systole and normal diastole isolted systolic
hypertension normally seen in elderly
Treating high BP the FIRST thing you do is take away sodium. Other
risk factor is obesity.
Hypertension is a silent killer, if they get symptoms like headache they
are getting ready to die.
Only see high blood pressure in elderly is U.S. with salt intake
The Cardiac Cycle Ventricular Filling:
Mid-to-late diastole
Pressure in the ventricle is low
Blood is flowing passively
Ventricular filling is mid to late diastole because the atria have to fill
first
Remember 70% of the ventricle fills passively
Filling time the amount that goes into the heart
1) how much blood is coming back to the heart
2) the BIG consideration is how much time the heart has to fill. Long
diastole = more blood in the heart
What determines the length of diastole? HR, the faster the HR the less
filling time and vice versa
Ventricular Filling Mid-to-Late Diastole:
AV valves are open
Aortic and pulmonary valves are closed
70% of ventricular filling occurs
They are open and closed based on pressure.
AV open because the atria pressure is higher than the ventricles
Aortic and pulmonary artery (?) are closed because there is more
pressure in the pulmonary trunk and the aorta than the ventricles
Atria contracts, finishes filling the ventricles (atrial kick)
After the atria has contracted the blood in the ventricle is called the end diastolic volume
(EDV)
o When the atria have finished, they have pushed in as much blood
s possible
Atria finishes putting in the other 30% in
Why is the atrial kick important? Because of Contractility (how hard the
heart beats), when contractility goes up, oxygen consumption also
increases.
The big point: For the most part as more blood is put in the ventricle,
that will INCREEASE contractility
NO atrial kick atrial fibrillation. = decreased contractility as well
The Cardiac Cycle Ventricular Systole:
Atria relax, ventricle contracts
Isovolumetric contraction phase short period of time when the ventricle begins to
contract but all the valves are closed
o When pressure starts to rise, for a very short time all valves close
o Isovolmetric contraction phase pressure in the ventricle exceed
pressure in the arteries so the aortic and pulmonic valves open
Ventricular pressure rises
Pulmonary and aortic valves open
This is called the ventricular ejection phase
When the valves open, blood is pushed out = ejection phase
The Cardiac Cycle Isovolumetric Relaxation:
Early diastole
Ventricles relax
Remaining blood is the end systolic volume (ESV)
Ventricle contracted, then it stopped and relaxes. But when the
ventricles contract it CANNOT push out all the blood. About 40% are
left behind = the end systolic volume
Isovolumetric Relaxation Diastole:
Pressure is rising in the atria as it is filling
After the aortic valve closes aortic pressure rises due to backflow known as the dicrotic
notch
If you put pressure monitor at base of aorta what you would see during
systole
The aorta (and pulmonary trunk) it has a lot of elastic fibers in it. In
order to maintan pressure inside, blood in the aorta stretches the
elastic fibers and like a balloon that isnt closed, the blood comes back
out d/t the pressure of the balloon pushing on it. The HEART IS
PACKING THE AORTA FULL OF BLOOD, so that when systole ends there
is still pressure in the aorta d/t the stretched elastic fibers
Part of the reason you see pressure drop is because blood is traveling
away from the heart
As the aorta is constricting (the blood is coming back) you will see a
transient rise in blood pressure before it comes back down = dicrotic
notch
What is important about the dicrotic notch coronary arteries are at base of
the aorta. If blood is traveling away from the aorta, then there isnt a
lot of blood being pushed in the coronary arteries. SOThe Dicrotic
notch represents the time when blood is being put in the coronary
arteries to feed the heart
The Heart Mechanics:
Cardiac Output
Regulation of Stroke Volume
Mechanics Cardiac Output:
Stroke volume the amount of blood pumped out in one beat
Stroke volume is : end diastolic volume minus end systolic volume
EDV ESV = SV
Stroke volume the amount of blood that is pushed out with one
contraction. Very easy calculation. Larger the stroke volume, the more
blood the heart packed into the aorta. The more it packs, the more it
stretches, and the higher the blood pressure
When heart is filled = end diastolic
End systolic contraction?
Just subtract end systolic with diastolic and you et stroke volume
Amount of blood pumped out each ventricle in 1 minute WILL BE ON
TEST
Formula: CO = HR X SV
Guaranteed this FORMULA WLL BE ON TEST!!!
Cardiac output how much blood is being ejected OVER 1 MINUTE
Ejection fraction what portion of the blood that enters the heart
leaves the heart (as said previously it will be around 65%) as the heart
starts to fail when that % drops.
Formula for calculating ejection fraction 2 different ways to write it.
EDV (end diastole volume) ESV / (divided by) EDV x 100 (if you
want it in percent)
TO simplify that equation: what is EDV ESV (its stroke volume) so
stroke volume over EDV
Stroke volume
____________
EDV
50%
40%
30%
20%
Is normal,
wont see very many problems,
will start to see symptoms,
really interfering with life,
And if in the teens you arent doing a whole lot (cant even get out of
bed)
Mechanics Stroke Volume:
The difference between the end diastolic volume (EDV) and the end systolic volume
(ESV)
Taking a break from PowerPoint:
From last slide, goes with it:
o Congestive heart failure = pump failure. The heart is failing to
deliver enough blood out versus how much came in
o So youre bringing a lot of blood IN but you arent pushing it OUT
o Most difficult concept: Pump failure shows up backwards! In CHF,
not worried about blood going into aorta (not the problem), you
can have isolated congested heart failure, on the left side, or
right side only, or on both sides.
o What you are going to see is either the lungs fill with fluid, or
swelling in the feet.
o If you have isolated left sided CHF, where is the fluid going to
back up? To the left (in the lungs, filled with fluid)
o If there is a problem on the right, right isolated CHF fluid builds
up in the extremities
o You can have isolated right sided HF, for a long period of time,
but you CANT have isolated left sided HF for a long period of time
d/t the left backing up to the right, it will keep backing up until it
is over on the right
o What would be the reason that there would be isolated right side
congestive heart failure only? Have to think about is where blood
goes. How blood passes through the heart. Blood from R side
side goes into the lungs, from L goes into the aorta (rest of
body).
o Why would you only have R sided only? Pulmonary hypertension
or because the lungs are still for other reason.
o If it is in the right side, the problem is actually with the lungs.
o If blood doesnt want to travel to the lungs, and there is swelling
in the feet this is called Cor pulmonale
Stroke Volume Regulation:
Preload
Contractility
Afterload
Regulate stroke volume: their terminology makes it very difficult to
understand
Have to give the significance of EACH of these
for the test!
The more blood you put in the heart the stronger contraction you have
= increased contractility
Preload the more blood you put in the heart the stronger the
contraction that is preload
Stroke Volume Preload:
Degree to which cardiac muscles are stretched before they contract
Stretching cardiac cells increases contractile force
Preload is secondary to venous return
Frank-Starling Law of the heart:
o Preload is the critical factor
Most important concept; cardiac filling is the MOST important factor
governing/determining contractility (strength of contraction) = the
Frank-Starling Law. NEED to remember
Stroke Volume Contractility:
Increase in contractile strength independent of muscle stretch
Directly due to calcium more Calcium in the heart cells
Under sympathetic control
Talking about NOT being due to stretch (contractility) any change that
is NOT due to venous return is called contractility.
Changes in this contractility is based on chemicals.
Sympathetic control increased contractility (?)
Contractility Other Influences:
Positive inotropic agents that increase contractility
Negative inotropic agents that decrease contractility
Can go either way be increased or decrease
Decreased negative inotrope
Increase positive inotrope
Contractility Positive Inotropic Agnets:
Hormones
o Glucagon produced by pancreas (also produced insulin) glucagon
does the opposite of insulin. If blood sugar starts to drop
increase of putting out insulin it puts out glucagon (positive
inotrope)
o Thyroxine thyroid hormone
o Epinephrine what is coming from sympathetic response
Drugs
o Digitalis Digitalis similar but not the same as digoxin.
WILL HAVE TO KNOW LIST for test!!!
o Aminophylline also known as Theodore was a drug used for
asthma. But is is a positive inotrope, it makes the heart beat
harder. Not longer used.
Contractility Negative Inotropic Agents:
Electrolytes
o Excessive hydrogen (acidosis)
o Extracellular potassium
Drugs
o Calcium channel blockers
o Beta blockers
Acidosis negative inotrope
Extracellular potassium stops the heart and CABG
Calcium channel blockers because calcium causes in increase in
contractility
Beta (adrenergic) blockers blocking the neurotransmitter/hormone
epinephrine (positive inotrope)
What are the 2 things major factors in determining how much O2 is
used
1) HR and
2) Contractility
If pt has coronary artery disease not adequate O2 to the heart. Two
thing syou want to control are HR and contractility, so you would use
abeta blocker
Practical applications:
o CHF too much blood to the heart not pumping enough.
Wouldntt give positive inotrope because the heart would then
sue too much O2 by increasing its contractility.
o Heres the big thing! By decreasing contractility with beta
blocker you can prevent a 2nd heart attack by 50%! If the beta
blocker starts to cause CHF then you have to back off of it.
How do you treat CHF? There are 2 ways
1) diuretic (Lasix),
2) furomoside. Just get all the water out!
Stroke Volume Afterload:
Pressure the ventricle must overcome to eject blood
Afterload is blood pressure
Only of consequence in hypertension
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Book of DragonsDocumento237 pagineBook of DragonsAl Denny100% (3)
- TKD Dictionary 2016 RevisionDocumento159 pagineTKD Dictionary 2016 RevisionLevi Simões100% (2)
- A&P 2 Respiratory Lecture NotesDocumento31 pagineA&P 2 Respiratory Lecture NotesBethanyNessuna valutazione finora
- Test 1.02 11 Test Taking Tips NRSNGcom PDFDocumento2 pagineTest 1.02 11 Test Taking Tips NRSNGcom PDFBethanyNessuna valutazione finora
- A&P GI System ChartDocumento5 pagineA&P GI System ChartBethanyNessuna valutazione finora
- A&P 302 Blood Lecture NotesDocumento20 pagineA&P 302 Blood Lecture NotesBethanyNessuna valutazione finora
- PSYC 212 Chapter 2Documento2 paginePSYC 212 Chapter 2BethanyNessuna valutazione finora
- PSYC 212 Chapter 14Documento4 paginePSYC 212 Chapter 14BethanyNessuna valutazione finora
- A&P 302 Blood Lecture NotesDocumento20 pagineA&P 302 Blood Lecture NotesBethanyNessuna valutazione finora
- PSYC 212 Chapter 1Documento6 paginePSYC 212 Chapter 1BethanyNessuna valutazione finora
- Chapter 2: Biological Beginnings: The Evolutionary PerspectiveDocumento1 paginaChapter 2: Biological Beginnings: The Evolutionary PerspectiveBethanyNessuna valutazione finora
- A&P 302 Heart Lecture NotesDocumento33 pagineA&P 302 Heart Lecture NotesBethanyNessuna valutazione finora
- PSYC 212 - Chapter 7 Study GuideDocumento2 paginePSYC 212 - Chapter 7 Study GuideBethanyNessuna valutazione finora
- Chemistry 100 - Week 3 Day 3:: Atoms, Molecules and Ions Are TINY!Documento2 pagineChemistry 100 - Week 3 Day 3:: Atoms, Molecules and Ions Are TINY!BethanyNessuna valutazione finora
- A&P 302 Blood Lecture NotesDocumento15 pagineA&P 302 Blood Lecture NotesBethany100% (1)
- A&P 301 Immunology NotesDocumento25 pagineA&P 301 Immunology NotesBethanyNessuna valutazione finora
- Chemistry 100 - Week 8 Day 1:: Chapter 5 - Chemical Quantities and Reactions A Chemical Equation GivesDocumento2 pagineChemistry 100 - Week 8 Day 1:: Chapter 5 - Chemical Quantities and Reactions A Chemical Equation GivesBethanyNessuna valutazione finora
- A&P 301 Central Nervous System OutlineDocumento40 pagineA&P 301 Central Nervous System OutlineBethanyNessuna valutazione finora
- A&P 302 Reproductive System Lecture NotesDocumento38 pagineA&P 302 Reproductive System Lecture NotesBethany100% (1)
- A&P 302 Renal Lecture NotesDocumento58 pagineA&P 302 Renal Lecture NotesBethanyNessuna valutazione finora
- A&P 302 Endocrine ChartDocumento7 pagineA&P 302 Endocrine ChartBethanyNessuna valutazione finora
- A&P 302 GI:Digestive System Lecture NotesDocumento51 pagineA&P 302 GI:Digestive System Lecture NotesBethanyNessuna valutazione finora
- Chemistry 100 - Week 5 Day 2:: RD STDocumento2 pagineChemistry 100 - Week 5 Day 2:: RD STBethanyNessuna valutazione finora
- PSYC 212 Chapter 2Documento2 paginePSYC 212 Chapter 2BethanyNessuna valutazione finora
- Games at MazedaDocumento7 pagineGames at MazedaMuhib H AdilNessuna valutazione finora
- Curriculum Vitae - Zulfa October 2011Documento4 pagineCurriculum Vitae - Zulfa October 2011Gusti Ryanda FazrinNessuna valutazione finora
- Ball Two Pieces Steel A105 / A216 WCB, 2000 - 1500 PSIG: Pressure Temperature RatingsDocumento2 pagineBall Two Pieces Steel A105 / A216 WCB, 2000 - 1500 PSIG: Pressure Temperature RatingsAlicia MartinezNessuna valutazione finora
- Zandronum Version HistoryDocumento35 pagineZandronum Version HistorySerhiiNessuna valutazione finora
- EMCP 4 Quick Start GuideDocumento2 pagineEMCP 4 Quick Start GuideBrian RomanoNessuna valutazione finora
- POLAR FavorDocumento10 paginePOLAR FavornetsheldonNessuna valutazione finora
- Kinesiology of Movements and Uderstanding The Planes and Axes of MovementsDocumento16 pagineKinesiology of Movements and Uderstanding The Planes and Axes of MovementsKharen Mancenido JacobNessuna valutazione finora
- Israel Football PhilosophyDocumento36 pagineIsrael Football PhilosophyAzamat AsanbekovNessuna valutazione finora
- Gaelic-Lesson Year 8Documento5 pagineGaelic-Lesson Year 8api-334831608Nessuna valutazione finora
- Concrete Mixer Rear Discharge Parts Catalog PDFDocumento215 pagineConcrete Mixer Rear Discharge Parts Catalog PDFtecnomaqvl04 tecnomaqNessuna valutazione finora
- THE ELDER SCROLLS - Oblivion - GuideDocumento330 pagineTHE ELDER SCROLLS - Oblivion - GuideMelanieReyesNessuna valutazione finora
- Section B5Documento2 pagineSection B5Muhammad AliNessuna valutazione finora
- New Microsoft Office Word DocumentDocumento38 pagineNew Microsoft Office Word DocumentPrateek Sahoo0% (1)
- Practice Used ToDocumento1 paginaPractice Used ToAndrea RosasNessuna valutazione finora
- Abdomen IntroductionDocumento32 pagineAbdomen Introductionpixiemedic100% (1)
- Mortal Kombat Finish Him Font - Google SearchDocumento1 paginaMortal Kombat Finish Him Font - Google SearchDouglas LemusNessuna valutazione finora
- BODYWEIGHT BODYBUILDING by Alexander IronDocumento26 pagineBODYWEIGHT BODYBUILDING by Alexander IronMario Rendon100% (2)
- Honda Accord Tourer 7th Gen Facelift AccessoriesDocumento16 pagineHonda Accord Tourer 7th Gen Facelift AccessoriesAOCUKNessuna valutazione finora
- Orc Custom ClassesDocumento2 pagineOrc Custom ClassesDaniel CleryNessuna valutazione finora
- Game Find-Your-Ideal-Partner - 95562Documento1 paginaGame Find-Your-Ideal-Partner - 95562Valentina BallesterosNessuna valutazione finora
- VSD Character Sheet FinalDocumento3 pagineVSD Character Sheet FinalSimon TrucmucheNessuna valutazione finora
- Lubricants For New Axor: Interval NO Operating Fluid Vehicle Type MB Oil Sheet CapacityDocumento1 paginaLubricants For New Axor: Interval NO Operating Fluid Vehicle Type MB Oil Sheet CapacityrudiNessuna valutazione finora
- Question Tags - Essay TaskDocumento1 paginaQuestion Tags - Essay TaskHidayatul HikmahNessuna valutazione finora
- Pilates For ScoliosisDocumento13 paginePilates For ScoliosisIoan-Alexandru CodarceaNessuna valutazione finora
- FMX 11 4x4 Tractor FM 44T B1CDX - VolvoDocumento5 pagineFMX 11 4x4 Tractor FM 44T B1CDX - VolvoFernando José FerreiraNessuna valutazione finora
- Three Men in A Boat: Jerome K. JeromeDocumento2 pagineThree Men in A Boat: Jerome K. JeromeLeonardo CampliNessuna valutazione finora
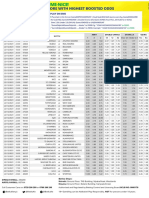
- Date Time Game Id Match 1 X 2 1X 12 X2 Over 2.5 Under 2.5 Yes NoDocumento2 pagineDate Time Game Id Match 1 X 2 1X 12 X2 Over 2.5 Under 2.5 Yes Nojust ANDROIDNessuna valutazione finora
- Ds GV HD de Tai NCKH Dot 1 NH 2023 2024 0210202345347CHDocumento8 pagineDs GV HD de Tai NCKH Dot 1 NH 2023 2024 0210202345347CHPhan Huy BaoNessuna valutazione finora