Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Approach To Hypoglycemia in Infants and Children - UpToDate
Caricato da
Omar Nayef TaaniTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Approach To Hypoglycemia in Infants and Children - UpToDate
Caricato da
Omar Nayef TaaniCopyright:
Formati disponibili
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
OfficialreprintfromUpToDate
www.uptodate.com2016UpToDate
Approachtohypoglycemiaininfantsandchildren
Authors: AgnetaSunehag,MD,PhD,MoreyWHaymond,MD
SectionEditor: JosephIWolfsdorf,MB,BCh
DeputyEditor: AlisonGHoppin,MD
Alltopicsareupdatedasnewevidencebecomesavailableandourpeerreviewprocessiscomplete.
Literaturereviewcurrentthrough:Nov2016.|Thistopiclastupdated:Oct18,2016.
INTRODUCTIONInhealthyindividuals,maintenanceofanormalplasmaglucoseconcentrationdependsupon:
Anormalendocrinesystemforintegratingandmodulatingsubstratemobilization,interconversion,andutilization.
Functionallyintactenzymesforglycogensynthesis,glycogenolysis,glycolysis,gluconeogenesis,andutilizationofothermetabolicfuelsforoxidationandstorage.
Anadequatesupplyofendogenousfat,glycogen,andpotentialgluconeogenicsubstrates(eg,aminoacids,glycerol,andlactate).
Adultsarecapableofmaintaininganearnormalplasmaglucoseconcentration,evenwhenfastingforweeksor,inthecaseofobesesubjects,months[1].Incontrast,
healthyneonatesandyoungchildrenareunabletomaintainnormalplasmaglucoseconcentrationsafterevenashortfast(24to36hours)andexhibitaprogressive
declineinplasmaglucoseconcentrationtohypoglycemicvalues[2,3].
Congenitaloracquiredabnormalitiesinhormonesecretion,substrateinterconversion,andmobilizationofmetabolicfuelscontributetoabnormalitiesinglucoseproduction
andutilizationthatultimatelyresultinhypoglycemiainchildren.Theevaluationandtreatmentofthechildwithhypoglycemiarequireanunderstandingofthefactorsthat
regulateglucosemetabolismandtheuniqueaspectsofglucosemetabolismininfantsandyoungchildren.
Glucosehomeostasisandthediagnosticapproachtohypoglycemiaininfantsandchildrenwillbediscussedhere.Othertopicswithrelatedcontentinclude:
(See"Causesofhypoglycemiaininfantsandchildren".)
(See"Pathogenesis,screening,anddiagnosisofneonatalhypoglycemia".)
(See"Managementandoutcomeofneonatalhypoglycemia".)
(See"Hypoglycemiainchildrenandadolescentswithtype1diabetesmellitus".)
GLUCOSEHOMEOSTASISINNORMALINFANTSANDCHILDRENThroughoutgestation,maternalglucoseistransportedacrosstheplacentatomeetasubstantial
proportionoftheenergyneedsofthefetus.Theenzymesnecessaryforglycogensynthesisandglycogenolysisarepresentinthefetalliverlongbeforetheaccumulationof
glycogencanbedemonstrated.Duringthelastthreetofourweeksofgestation,hepaticglycogenstoresincreasetoreacharound5percentofliverweightatbirth,a
proportionthatishigherthanatanyothertimeinthelifecycle[4].Inanimals,theactivityofoneormoreimportantratelimitingenzymesofgluconeogenesis(pyruvate
carboxylase,phosphoenolpyruvatecarboxykinase,glucose6phosphatase,andfructose1,6diphosphatase)isabsentorverylowinthefetus,doesnotincreaseuntilthe
perinatalperiod,andreachesadultlevelsonlyafterseveralhourstodaysofextrauterinelife[4].Similarly,inhumans,hepaticglucoseproductionandgluconeogenesisare
absentduringfetallife[5],butrapidlyincreasewithinthefirstfewhoursoflife,eveninveryprematureinfants[6].
Atbirth,theinterruptionofplacentalbloodflowasaresultoftheclampingoftheumbilicalcordrequirestheinfanttoutilizehisorherownendogenoussubstratesand
challengesthenewbornwithhisorherfirstfast.Withtheclampingofthecord,thereisanimmediatereleaseofglucagon[7].However,despitetheglucagonsurge,plasma
glucosedecreasesoverthefirsttwohoursoflife.Thisisaccompaniedbyadecreaseininsulinandanincreaseinfreefattyacids(FFAs)andketonebodies[8].Byfourto
sixhoursoflife,theplasmaglucoseconcentrationisstabilizedorisincreasinginmostinfants.Muchofthisearlyglucoseproductionprobablycomesfromthemobilization
ofhepaticglycogen,sincehepaticglycogencontentdecreasesduringthefirstseveraldaysofextrauterinelife.Thisreleaseofhepaticglycogenfacilitatesasmooth
transitionfromthecontinuouslyfed(intrauterine)tothefastedorrelativelyfastedconditionofthefirsthourstodaysofextrauterinelife.However,hepaticglycogenstores
arequicklydepleted,andgluconeogenesismustbeginwithinhoursofbirthtomeetaneverincreasingproportionofendogenousglucoseproduction[6,8].
Intheprematureandterminfant,morethan90percentoftheglucoseisutilizedbythebrain.Thisvaluedecreasestoapproximately40percentofglucoseturnoverin
overnightfastedadults(figure1)[9].Thehigherratesofglucoseturnoverperkilogramofbodyweightininfantsandchildrenwhencomparedwithadultsareconsistentwith
therelativelyhigherproportionofbrainmasstobodysize,whichplacesinfantsandchildrenathigherriskofhypoglycemia[10,11].
Fattyacidmobilizationandoxidationplayacrucialroleinthemaintenanceofglucosehomeostasisininfantsandchildren.PlasmaFFAsandketonebodiescanbeusedby
avarietyofbodytissuesand,thus,decreasethedemandsofthesetissuesforglucoseasanenergysource.Thebrainisuniqueinthatitusesglucoseatarate20times
thatofotherbodytissues(pergram)andcannotuseFFAsdirectlysincetheyarenottransportedacrossthebloodbrainbarrier.However,ketonebodies(beta
hydroxybutyricacidandacetoaceticacid)aretransportedacrossthebloodbrainbarrier,andtheirmetabolismbythebraincanpartiallysupplanttheneedforglucose[1].
Themetabolicresponsetofastinginchildrenissimilartothatinadults,exceptthatchildrenhaveamorerapiddeclineinplasmaglucoseconcentrationandamorerapid
increaseintheplasmaconcentrationofketonebodiesthandoadults.Thesefindingssuggesttherelativelyhighglucoserequirementinchildrenmayacceleratethenormal
adaptivemechanism(s)offastingobservedinadults[3].
Duringthefirst8to10yearsoflife,therateoftotalbodyglucoseutilization(andproduction)increases,followedbyaplateauduringthenextfivetosevenyears,afterwhich
thenormaladultrate(833to944micromol/min[150to170mg/min])isachieved(figure2)[9].Studiesutilizingisotopicallylabeledglucoseindicatethat,byweight,ratesof
glucoseflux(productionandutilization)inadultsareapproximately11to13micromol/kgpermin(2to2.3mg/kgpermin)intheovernightpostabsorptivestate(14hour
fast)anddecreaseto9.8micromol/kgpermin(1.8mg/kgpermin)by30hoursoffasting[10].Therateofglucosefluxininfantsandchildrenafter4to14hoursoffastingis
nearlythreetimeshigher(35micromol/kgpermin[6mg/kgpermin])thanthatofadults,anddecreasesto23micromol/kgpermin(4mg/kgpermin)aftera30to40hour
fast[10,11].
Themobilization,use,andstorageofnutrientsisprimarilyorchestratedbytheclassicalactionsofhormones(eg,insulin,glucagon,catecholamines,cortisol,andgrowth
hormone),althoughmoresubtleinteractionsofotherfactors(eg,cytokines,neuronalinput,ghrelin,leptin,glucagonlikepeptide1[GLP1]postreceptoractivation
mechanism)arenowbeingrecognized.Insulinsecretionplaysacentralroleinglucosehomeostasisandisaffectedbyanumberoffactors,themostimportantofwhichis
theplasmaglucoseconcentration.Amoredetaileddescriptionofthesecretionandactionsofinsulinispresentedseparately.However,weprovideabriefdescriptionhere.
(See"Pancreaticbetacellfunction"and"Insulinaction".)
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
1/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Whentheplasmaglucoseconcentrationincreasesafteramealinnormalindividuals,glucoseistransportedintothepancreaticbetacellviathe
glucosetransporter2(GLUT2),isphosphorylatedbyglucokinase,andmetabolizedviatheglycolyticpathway.Thisresultsinanincreaseintheadenosine
triphosphate/adenosinediphosphate(ATP/ADP)ratio,whichclosestheKATPchannels,depolarizesthecellmembrane,openingtheCa++channels,resultinginfusionofthe
insulingranulewiththeplasmamembranecausinginsulinsecretion.Conversely,adecreaseinplasmaglucoseconcentrationresultsindecreasedglucosemetabolismin
thebetacell,whichleadstoareducedATP/ADPratio,openingoftheKATPchannels,hyperpolarizationofthecellmembrane,andclosureofCa++channels,thusblocking
Ca++influxandreducinginsulinsecretion.Fundamentalproblemsintheseprocessescanleadtoprofoundhypoglycemiainchildren[12].(See"Pathogenesis,clinical
features,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy".)
Duringcontrolledinsulininducedhypoglycemia,childrentypicallymountagreatercounterregulatoryhormoneresponse(eg,withcortisol,epinephrine,andglucagon)than
doadults[13,14].However,withrepeatedepisodesofhypoglycemia,secretionofcounterregulatoryhormoneswanes,leadingtodefectivecounterregulationand
"hypoglycemiaunawareness"inanindividualwithdiabetes.Intheabsenceofclassicalsymptomsofhypoglycemia,perhapsasaresultofthisprocess,thediagnosisof
hypoglycemiacanbemissedinsomechildrenformonths.
DEFINITIONOFHYPOGLYCEMIAFordiagnosticpurposes,wedefinehypoglycemiaasaplasmaglucosevalueof40mg/dL(2.22mM)atanyage(exceptduringthe
first48to72hoursoflife).Thisconcentrationshouldtriggeraformalevaluationtoidentifythecauseofthehypoglycemiaandtopreventitsrecurrence.Thisconcentration
shouldnotbeconstruedasidealornecessarilysafeovertime,andshouldonlybeusedinidentifyinganindividualatriskforand/ordiagnosinghypoglycemia.
Innewborns,aplasmaglucosevalueof50mg/dLisanappropriatethresholdtodistinguishinfantswhowarrantfurtherdiagnostictesting.Thisthresholdwassuggestedby
aconsensusconferencethatfocusedprimarilyonthenewbornperiod[15].Thisisarelativelyconservativethreshold,intendedtoavoiddischargingnewbornswhomay
haverisksforrecurrentandseverehypoglycemia.Similarly,whenusingapointofcare(bedside)glucometer,itisreasonabletouseathresholdof50mg/dLtoidentifya
childwhorequiresfurtherevaluation,includinglaboratorymeasurementofplasmaglucose.(See'Criticalsamples'below.)
Bytradition,laboratoriesmeasureplasmaglucose(fromsodiumfluoride,heparin,orethylenediaminetetraaceticacid[EDTA]containingtubes).Evenpointofcareglucose
valuesareadjustedintheircalibrationto"plasmaconcentrations."Alternatively,wholebloodglucosecanbemeasuredonanumberofglucoseanalyzers.However,whole
bloodglucoseconcentrationsareabout15percentlowerthanplasmaglucosemeasurements,andthisdifferenceshouldberecognizedwheninterpretingtheresults
[16,17].
Theprecisedefinitionofhypoglycemiaininfantsandchildrencontinuestobecontroversial.Thisisbecausenormaldistributionsofglucosevaluesdependonconditionsof
feedingandfasting,andalsovarywithclinicalfactorssuchasage,gestation,and/orweight(small,average,orlargeforgestationalage).Despitethisnaturalvariation,we
useasinglethresholdtodefinehypoglycemiafordiagnosticpurposesbecausetheoverallgoalofidentifyingchildrenwithhypoglycemiaistoprotecttheircentralnervous
systemsfromirreparabledamage.Thereisnoapriorireasonthatsomeindividuals(eg,aprematureorlowbirthweightinfant)shouldtoleratealowglucoseconcentration
betterthanothers(eg,anolderchild)infact,quitetheoppositemightbeargued.
ETIOLOGYOFHYPOGLYCEMIAHypoglycemiaoccurswhentherateofappearanceofglucoseintotheplasmaspaceislessthanitsrateofutilization.Thiscanbe
causedbydefectiveglucoseproduction,increasedglucoseutilization,orsomecombinationofthetwo.Formanyhypoglycemicconditions,themechanismisnotentirely
understood.
Ininfantsandchildren,importantcausesofhypoglycemiainclude(table1):
InbornerrorsofmetabolismMostofthedisordersofcarbohydratemetabolismandseveraldisordersofaminoacidandfatmetabolismarecharacterizedbydefective
glucoseproduction.Becauseoftheinteractionsofcarbohydrate,andaminoacidandfatmetabolisminthemaintenanceofnormalfuelhomeostasis,abnormalitiesin
themetabolismofasinglesubstratecanhavesecondaryeffectsonothermetabolicpathways.
Hyperinsulinism
EndogenousPersistenthyperinsulinemichypoglycemiaofinfancy(PHHI)orinsulinoma.Ingestionoforalhypoglycemicagents(sulfonylureas)alsostimulates
insulinsecretion.
ExogenousDuetoinsulinadministration.
OtherMiscellaneouscausesofhypoglycemiaincludeketotichypoglycemia,varioustoxicingestions(includingsulfonylureas,ethanol,andsalicylates),hormone
deficiencies,andmedicalconditionsthateitherincreaseglucoserequirements(eg,sepsis,shock,burns,tumors)oraffecttheliver'sabilitytoproduceglucose(eg,
Reyesyndrome,hepatitis,orothercausesofliverdysfunction).
Theseandothercausesofhypoglycemiainchildrenarediscussedelsewhere.(See"Causesofhypoglycemiaininfantsandchildren".)
CLINICALFEATURES
ChildrenandadultsInchildrenandadults,thesymptomsofhypoglycemiacanbedividedintotwocategories:thosecausedbytheautonomicresponseto
hypoglycemiaandthosecausedbyneuroglycopenia[14].
Neurogenic(autonomic)symptomsTheearlymanifestationsofhypoglycemiaarecausedbytheautonomicresponsetohypoglycemiaandincludesweating,
weakness,tachycardia,tremor,andfeelingsofnervousnessand/orhunger.Thesesymptomsandsignsusuallyoccuratplasmaglucoseconcentrationsbetween40and70
mg/dL(2.2and3.9mM),whicharehigherthantheplasmaglucoseconcentrationsthattriggerneuroglycopenicsignsandsymptoms.Therefore,theautonomicsymptoms
functionasa"warningsystem."However,withrepeatedorprolongedepisodesofhypoglycemia,thethresholdforautonomicsymptomsdecreasestothatfor
neuroglycopenicsymptoms.Thiscanresultintheappearanceofseveresymptomsofhypoglycemiawithlittleornowarning,termed"hypoglycemiaunawareness."(See
'Glucosehomeostasisinnormalinfantsandchildren'above.)
NeuroglycopenicsymptomsSymptomsandsignsthatdevelopwithprolongedorprofoundhypoglycemiaarecausedbyinsufficientsupplyofglucosetothebrain
(neuroglycopenia),andincludelethargy,irritability,confusion,uncharacteristicbehavior,andhypothermia.Inextremehypoglycemia,lossofconsciousness,seizure,or
comamayoccur.Thesesymptomsandsignsoccuratplasmaglucoseconcentrationsbetween10and50mg/dL(0.5to2.8mM).Severeandrepeatedepisodesof
hypoglycemiacanresultinpermanentcentralnervoussystemdamage,andoccasionallyindeath.
InfantsIninfants,thesignsofhypoglycemiaarefrequentlynonspecificandmayincludejitteriness,irritability,feedingproblems,lethargy,cyanosis,tachypnea,and
hypothermia,aswellasthesignsofsevereneuroglycopeniadescribedabove.Thesesymptomsarenotspecificforhypoglycemiaandmaybeearlymanifestationsofa
numberofotherdisorders,includingsepticemia,congenitalheartdisease,ventricularhemorrhage,andrespiratorydistresssyndrome.Infantsareatgreatestriskfor
hypoglycemiaduringthefirstfewdaysoflife.Neonatalhypoglycemiaisdiscussedseparately.(See"Pathogenesis,screening,anddiagnosisofneonatalhypoglycemia".)
IMMEDIATEMANAGEMENTTheimmediatemanagementoftheinfantorchildwithhypoglycemiainvolvesobtainingcriticalsamplesandadministeringparenteral
glucose.Thesestepsaresummarizedinarapidoverview(table2).
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
2/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
CriticalsamplesWhenthediagnosisofhypoglycemiaissuspectedandsupportedbyarapidmeasurementoftheplasmaglucoseconcentration(andbeta
hydroxybutyrate,ifavailableasapointofcaremeasurement),asampleofbloodshouldbeobtainedbeforetherapeuticintervention.Thissampleisusedtoconfirmthe
diagnosisofhypoglycemiaandassessforrelatedelectrolyteabnormalities.Ifthecauseofthehypoglycemiaisunknown,thiscriticalsampleisusedforadditional
biochemicalteststoinvestigateitscause,asdiscussedbelow.(See'Laboratorytesting'below.)
BloodDuringtheperiodofhypoglycemia,collecta5to10mLsampleofbloodbeforetherapeuticintervention.Thebloodshouldbedrawnintheappropriatetubes
accordingtotherequirementsofindividualclinicallaboratories.However,mostofthestudiescanbeperformedonbloodtreatedwithheparinorethylenediaminetetraacetic
acid(EDTA).Bloodsamplesshouldbetransportedonicetothelaboratory.Excessplasmashouldbestoredat70Cuntilalltheorderedresultsareavailable.
UrineIfthecauseofhypoglycemiaisunknown,thenthefirsturinevoidedduringorafterthehypoglycemicepisodeshouldbecollected.Aurinesampleshouldbe
testedforketones(ifplasmabetahydroxybutyrateisnotavailable)andreducingsubstances.Thepresenceofnonglucosereducingsubstancesintheurinesuggests
galactosemiaorhereditaryfructoseintoleranceifotherreducingsubstances(eg,streptomycin)areexcluded.(See"Galactosemia:Clinicalfeaturesanddiagnosis"and
"Causesofhypoglycemiaininfantsandchildren".)
Theremainingurineshouldbefrozenandsavedfortoxicologystudies,organicacids,dicarboxylicacids,and/oracylglycines,ifindicatedbysubsequentevaluation.(See
'Evaluationforthecauseofhypoglycemia'belowand"Approachtothechildwithocculttoxicexposure".)
Treatment
Glucosetherapy
ConsciouspatientIfthepatientisconsciousandabletodrinkandswallowsafely,arapidlyabsorbedcarbohydrate(eg,glucosetablets,glucosegel,tablesugar,
fruitjuice,orhoney)shouldbegivenbymouth.Anappropriatedoseforachildis10to20grams(or0.3grams/kg).Fifteengramscanbesuppliedby3glucosetablets,a
tubeofdextrosegelwith15grams4oz(120mL)fruitjuice6ouncesofnondietsodaoratablespoon(15mL)ofhoneyortablesugar.Thisprocessmayberepeatedin
10to15minutes.However,ifthehypoglycemiadoesnotimprovewithin15to30minutes,parenteralglucoseisrecommended.
PatientwithalteredconsciousnessInfantsandchildrenwithalteredconsciousnessand/orwhoareunabletosafelyswallowrapidlyabsorbedcarbohydrates
shouldbetreatedwithintravenous(IV)dextrose.IfIVaccessisnotreadilyavailable,thensubcutaneousorintramuscularglucagonshouldbegiven.(See'Glucagon'
below.)
InitialbolusGivedextrose,0.20to0.25grams/kgofbodyweight(maximumsingledose,25grams).Thisisusuallyachievedwith2.5mL/kgof10percentdextrose
solution,sinceextravasationofhigherconcentrationsofglucosewillleadtoseveretissuedamage.Thebolusshouldbeadministeredslowly(2to3mL/min),
regardlessofthepatient'sage.Thedextroseisgivenslowlytoavoidacutehyperglycemia,whichcancausereboundhypoglycemia.Somewhatlowerconcentrationof
dextrosesolutionisoftenusedformanagementofhypoglycemiainneonates.(See"Pathogenesis,screening,anddiagnosisofneonatalhypoglycemia".)
SubsequentinfusionAfterthebolus,plasmaglucoseshouldbemaintainedbyaninfusionofdextroseat6to9mg/kgperminute.Therateofglucoseinfusion
(mg/kgperminute)canbecalculatedasfollows:
Rateofinfusion(mg/kgpermin)=(Percentdextroseinsolutionx10xrateofinfusion[mLperhr])(60xweight[kg])
Thus,foraninfusionof10percentdextrosesolution:
3mL/kg/hourprovides5mg/kgperminute
5mL/kg/hourprovidesapproximately8mg/kgperminute
Higherdosesofdextrose(eg,0.5to1.0g/kg)aresometimesrecommendedfortheinitialbolus.However,ourclinicalexperienceinchildrenandinfants,andstudiesin
adults,suggestthatsuchdosesareexcessiveandarelikelytocausehyperosmolarityandhyperglycemia,whichcanresultinreboundhyperinsulinemiaandrecurrenceof
hypoglycemia[18,19].
Symptomatichypoglycemiacausedbysulfonylureaoverdoseismanagedwithbolusesofdextroseasdescribedabove,withclosemonitoringforrecurrenthypoglycemia.If
hypoglycemiarecursorbecomesmoresevere,octreotidehasbeenused[20]butuseofglucagonasaninfusionorminidoseglucagonmightalsobeconsidered[21].(See
"Sulfonylureaagentpoisoning".)
GlucagonIfIVaccessisnotreadilyavailableandthepatientisunabletosafelyswallowarapidlyabsorbedcarbohydrate,hypoglycemiamaybetreatedwith
glucagon,givenintramuscularlyorsubcutaneously(0.03mg/kguptoamaximumof1mg).
Glucagonisgenerallyeffectiveforinitialtreatmentofhypoglycemiacausedbyhyperinsulinemia(eg,inapatientwithdiabetestreatedwithexogenousinsulin),butmaynot
beeffectiveforothercausesofhypoglycemia.Moreover,theresponseisfrequentlytransient.Thus,ifthehyperinsulinemiapersists,repeatedadministrationofglucose
and/orglucagonmayberequired.Theresponsetoglucagonalsomayprovidediagnosticinformationforpatientsinwhomtheetiologyofhypoglycemiaisunknown.(See
'Glucagonstimulationtest'below.)
MonitoringDuringtheinitialtreatmentphase,theplasmaglucoseshouldbemonitoredevery30to60minutesandthedextroseinfusionadjustedaccordingly,untila
stableplasmaglucoseconcentrationbetween70and120mg/dL(3.9to6.7mmol/L)isattained[15].Thereafter,plasmaglucoseshouldbemonitoredeverytwotofour
hours.Ifratesofglucoseinfusiongreaterthan6to10mg/kgperminutearenecessarytomaintainnormalplasmaglucoseconcentrations,thepatient'shypoglycemiais
likelytobecausedbyhyperinsulinemia(eg,duetopersistenthyperinsulinemichypoglycemiaofinfancy[PHHI],alsoknownascongenitalhyperinsulinism[CHI]).(See
"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy".)
EVALUATIONFORTHECAUSEOFHYPOGLYCEMIATheresultsobtainedfromthehistory,physicalexamination,andinitialplasmasamplesshouldguidefurther
testing.
HistoryThehistoryinahypoglycemicchildshouldincludeathoroughexplorationofthepastmedicalhistory(includingperinatalhistory),detailsoftheacuteeventas
wellaspreviousepisodes,andfamilyhistory[22].
AgeatonsetAlthoughthereisconsiderableoverlap,theageofonsetofsymptomssuggestsdiagnosticcategories:
NeonatalperiodorthefirsttwoyearsoflifeMostinbornerrorsofmetabolism(includingcausesofhyperinsulinism)andcongenitalhormonedeficiencies.(See
"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy"and"Overviewofinheriteddisordersofglucoseandglycogen
metabolism".)
OneyeartoearlychildhoodKetotichypoglycemia,isolatedgrowthhormonedeficiency,andcortisoldeficiency.(See"Causesofhypoglycemiaininfantsandchildren",
sectionon'Ketotichypoglycemia'and"Causesofhypoglycemiaininfantsandchildren",sectionon'Hormonedeficiencies'.)
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
3/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
ToddlersandyoungchildrenIngestionshouldalwaysbeconsideredinthisagegroup.(See"Approachtothechildwithocculttoxicexposure"and"Causesof
hypoglycemiaininfantsandchildren",sectionon'Ingestions'.)
TriggersThedetailsoftheacuteeventshouldincludeinformationaboutthechild'sdietaryintakebeforetheeventandhelpstonarrowthedifferentialdiagnosis[23].
(See"Causesofhypoglycemiaininfantsandchildren".)
FastingstateDeterminewhetherthechildwasinthefedorfastingconditionatthetimeofhypoglycemia,orwhetheranacuteillnesspreventedthechildfrom
achievingadequatecarbohydrateintake.Thedegreeoffastingthatistoleratedbeforehypoglycemiadevelopsvarieswithageinhealthyinfantsandchildren,and
variesamongdifferentinbornerrorsofmetabolism.Patientswithcriticalillnesses,especiallysepsis,liverfailure,orrenalfailure,areatgreaterriskfordeveloping
hypoglycemia.
IngestionSpecificallyinquireaboutthepossibilitythatthechildmighthaveingestedsubstancesthatcancausehypoglycemia,includingalcohol,oralhypoglycemic
agents(sulfonylureasormeglitinides),aspirin,betablockers,quinine,orunripeackeefruit(astapleinJamaicandiets).(See"Approachtothechildwithocculttoxic
exposure".)
Specificfoods
Symptomsafteringestionofmilkproductsorfructosemayindicategalactosemiaorhereditaryfructoseintolerance,respectively.
Childrenwhohavehereditarydefectsofaminoacidororganicacidmetabolismmaydevelophypoglycemiashortlyaftertheingestionofprotein.(See"Organic
acidemias".)
PastmedicalhistoryTheperinatalhistoryshouldincludethebirthweight,gestationalage,andwhetherthechildhadhypoglycemicsymptomsatbirthorinthe
neonatalperiod.Itisimportanttoexplorethechild'spastmedicalhistoryandtoreviewavailablemedicalrecords,todeterminewhetherthechildhadotherepisodes
suggestiveofhypoglycemiathatmayhavebeenmissedordiagnosedasotherconditions(eg,seizuredisorder,etc).
FamilyhistoryAfamilyhistoryofReyesyndrome,unexplainedinfantdeaths,orotheraffectedfamilymemberssuggestsaninbornerrorofmetabolism,particularlya
fattyacidoxidationdefect[4,12,13].Hormonaldeficienciesandhyperinsulinismalsomayruninfamilies[24].(See"Causesofhypoglycemiaininfantsandchildren",section
on'Disordersoffattyacidmetabolism'.)
PhysicalexaminationTheexaminationmayprovideimportantcluestothediagnosis[15].
Thechild'sweightandlengthorheightshouldbemeasuredandplottedonanappropriategrowthchart,andthechild'sgrowthtrajectoryshouldbeevaluated.Short
staturemayindicatehypopituitarismorgrowthhormonedeficiency.Disordersofaminoacid,organicacid,andcarbohydratemetabolismareusuallyassociatedwith
failuretothrive,whereaschildrenwithfattyacidoxidationdisorderstypicallyhavenormalgrowth.Childrenwhoareunderweightforagemaybeatriskforketotic
hypoglycemia.Poorweightgainalsomaybecausedbyhypopituitarismandadrenocorticotropichormone(ACTH)deficiencyorunresponsiveness,andprimaryadrenal
insufficiency[25,26].
Feversuggestssepsisoranotherinfectioustrigger,whilehypothermiaisconsistentwithprolongedhypoglycemia(neuroglycopenia),sepsis,alcoholtoxicity,andsome
inbornerrorsofmetabolismthatimpairenergyutilization.
Midlinefacialdefects(eg,asinglecentralincisor,opticnervehypoplasia,cleftliporpalate)andmicrophallusorsmallnormalpenisorundescendedtesticlesinboys
mayindicatehypopituitarismand/orgrowthhormonedeficiency.(See"Diagnosisofgrowthhormonedeficiencyinchildren".)
Hepatomegalyand/orhypotoniasuggestaninbornerrorofmetabolism,suchasaglycogenstoragedisease,defectsingluconeogenesis,galactosemia,orhereditary
fructoseintolerance[25].(See"Overviewofinheriteddisordersofglucoseandglycogenmetabolism".)
Macrosomia,hepatosplenomegaly,andumbilicalherniamayindicateBeckwithWiedemannsyndrome.Hypoglycemiainaffectedpatientsusuallyislimitedtothe
neonatalperiod(ie,thefirstmonthoflife).(See"BeckwithWiedemannsyndrome".)
Hyperventilationmaybeacluetometabolicacidosisfromaninbornerrorofmetabolism.(See"Inbornerrorsofmetabolism:Epidemiology,pathogenesis,andclinical
features"and"Inbornerrorsofmetabolism:Metabolicemergencies".)
Hyperpigmentationmaybeacluetoadrenalinsufficiency.(See"Causesandclinicalmanifestationsofprimaryadrenalinsufficiencyinchildren".)
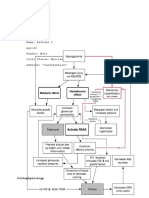
LaboratorytestingForpatientswithunexplainedhypoglycemia,thehistoryandphysicalexaminationareusedtodevelopclinicalsuspicionsandtheevaluationis
tailoredaccordingly(algorithm1).Asexamples,clinicalfeaturessuggestinganaccidentalortoxicingestionoraspecificinbornerrorofmetabolismshouldpromptspecific
testingforthesuspecteddisorder.
Ifthecauseofthehypoglycemiaisunknown,thefollowingtestsshouldbeperformedon"criticalsamples"collectedduringaperiodofhypoglycemia(eitherattheinitial
presentationorduringanelectivefast)[15]:
Plasmaglucose
Insulin
Cpeptide
Betahydroxybutyrate
Freefattyacids(FFAs)
Acylcarnitineprofile
Lactate
Ammonia
Urineorganicacids
Alsomeasurebloodelectrolytes,bloodureanitrogen(BUN),creatinine,aspartateaminotransferase(AST),andalanineaminotransferase(ALT),ifnotalreadydone.
Measurementsofbothgrowthhormoneandcortisolatthetimeofhypoglycemiaseldomprovidediagnosticinformation.However,shouldthechildhaveanyindicationsof
hypopituitarism(microphallus,centralfacialanomalies,growthfailure)orifthediagnosisremainsunclearfollowingtheinitialevaluation,considerationshouldbegivento
evaluatingthechildforhypothalamicorpituitarydeficiencies.Evaluationwouldincludebrainmagneticresonanceimaging(MRI)andlaboratorytestingforgrowthhormone,
cortisol,andthyroidfunction(T4andTSH)(algorithm1).
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
4/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
SubsequenttestingforunexplainedhypoglycemiaIfthecauseofthehypoglycemiaremainsunclearafterreviewingthecriticalsampleresults,weperformfurther
testingtonarrowthediagnosticpossibilities.Thesestepsmustbeperformedduringaperiodofhypoglycemia,eitherarisingspontaneouslyorinducedbyadiagnosticfast
undercarefullyestablishedconditions.Ifthefastinducesahypoglycemicepisode,thecriticalsamplesmustbeobtainedpriortotherapeuticinterventionandaglucagon
stimulationcarriedoutasdescribedbelow(algorithm1).Theglucagonstimulationtestwillnarrowthediagnosticpossibilitiesbyidentifyingorexcludinghyperinsulinemia.
ElectivefastIfthecauseofthehypoglycemiaremainsunclearandthecriticaldiagnosticsampleswerenotobtainedduringaspontaneousepisodeofhypoglycemia
(see'Criticalsamples'above),thenanelectivefastusuallyshouldbeperformedtodeterminethecauseofthehypoglycemia.Priortoperforminganelectivefast,the
plasmacarnitineandacylcarnitineconcentrationsshouldbeproventobenormal,toexcludethepossibilityofadefectinfattyacidorcarnitinemetabolism.Thisisbecause
hypoglycemiacancausesevereencephalopathyinchildrenwiththesedisorders.(See"Causesofhypoglycemiaininfantsandchildren",sectionon'Disordersoffattyacid
metabolism'and"Metabolicmyopathiescausedbydisordersoflipidandpurinemetabolism".)
Thedurationofthefastdependsuponthechild'sageandnormalfeedingpattern.Forinfantsandveryyoungchildrenwhoarenormallyfedeverythreetosixhours,the
fastmayconsistofomittingoneormorefeedings[27].Foranolderchild,whobyhistorytypicallyfastsovernight,a24to30hourfastshouldbeinitiatedaftertheevening
meal(ie,startingaround6PM).Childrenwhofastedaccordingtosuchaprotocoltendtodevelophypoglycemiaafter16to24hoursoffasting(ie,between10:00AMand
6:00PM),atimeduringwhichtheyshouldbeawakeandalert,andtheavailabilityofthephysicianandlaboratorystaffisoptimal.
Duringthefast,plasmaconcentrationsofglucose,insulin,betahydroxybutyrate,andlactateshouldbeseriallymonitoredandcomparedwithpublishedvaluesforafasting
study.Thetimingofsamplingisdependentontheplasmaglucosevalue.Wetypicallysampleeverytwotothreehourswhiletheplasmaglucoseremainsabove70mg/dL.
Astheplasmaglucosedecreasesbelowthisthreshold,wesamplemorefrequently(eg,hourly)toavoidprolongedhypoglycemia.
Ifhypoglycemiadevelops(plasmaglucose<40mg/dL[2.2mM]forchildrenandinfantsotherthannewborns):
Repeatmeasurementofglucose,insulin,Cpeptide,betahydroxybutyrate,andlactateconcentrations.
Measurefreefattyacids,ammonia,acylcarnitineprofile,andurineorganicacids
Measureplasmagrowthhormone,cortisol,andinsulinlikegrowthfactorbindingprotein1(IGFBP1)(althoughtheirinterpretationisnotalwaysclear).
Performaglucagonstimulationtest,asdescribedbelow.
Ifketotichypoglycemiaissuspected,theclinicianmayconsiderobtainingaplasmaalanineconcentrationatthetimeofhypoglycemiathisdisorderischaracterizedbylow
plasmaalaninewithnormallactateconcentration.
Ifhypoglycemiacannotbeinducedwithafastofreasonableduration,thechildshouldbedischargedafterthefamilyisinstructedinhomeglucosemonitoring,toensure
safetyandtoprovidefurtherdiagnosticinformation.Shouldthechildexperienceanadditionalepisodeofhypoglycemia,itisimperativethatthecriticalsamplesbeobtained
immediatelytoconfirmthehypoglycemiaandalsotoobtainthecriticalsamplesasdescribedabove.
GlucagonstimulationtestInthecaseofachildwithhypoglycemiaofunknowncause,aglucagonstimulationtest(orglucagonchallengetest)atthetimeof
hypoglycemiacanprovideveryusefuldiagnosticinformationaboutglycogenstores.
Thetestisperformedasfollows:Whilethechildishypoglycemic,glucagon(0.03mgperkg)isinfusedorgivenbyintramuscularinjection.Itiscriticallyimportantthat
plasmaglucoseconcentrationismeasuredwithinminutespriortogivingtheglucagon.Subsequently,wemeasureplasmaglucoseat10,20,and30minutes.Theinitial
samplesareprimarilytomakesurethattheplasmaglucoseconcentrationisnotcontinuingtodecrease.Aclearglycemicresponse(plasmaglucoserisesby>30mg/dL[2
mmol/L]withinthefirst30minutesafterglucagonadministration)inahypoglycemicchildsuggestshyperinsulinemia.Hyperinsulinemiacausesinappropriatesequestration
ofhepaticglycogenatthetimeofhypoglycemia,whichisthenreleasedinresponsetothepharmacologicdoseofglucagon.(See'Hyperinsulinism'below.)
InterpretationofresultsForpatientswithunexplainedhypoglycemia,thetestsonthe"criticalsamples"obtainedduringanepisodeofhypoglycemia(eitheratthe
timeofinitialpresentationorduringanelectivefast)andglucagonstimulationtestareusedtoidentifythetypeofdisordercausinghypoglycemia.
Wenarrowthediagnosticpossibilitiesinthefollowingsequence,assummarizedinthealgorithm(algorithm1).
Hyperinsulinism
Fattyacidoxidationdisorders
Disordersofgluconeogenesisand/orglycogenmetabolism
Wethenconfirmorrefinethediagnosticcategoryestablishedbythesetestsbyconsideringthedegreeofketosis.
HyperinsulinismFirst,wedeterminewhetheroneorbothofthefollowingcharacteristicsofhyperinsulinismarepresent(algorithm1):
PositiveglucagonstimulationtestAglycemicresponse(plasmaglucoserises>30mg/dL)toglucagonstimulationiscausedbyinappropriatehepaticglycogenstores,
andsuggestshyperinsulinemia.
InappropriatelyelevatedlevelsofinsulinPlasmainsulinconcentrationforanormalchildwhohasbecomehypoglycemicduetofastingisusually<15pmol/L(2
microIU/mL)andrarelygreaterthan35pmol/L(5microIU/mL),exceptinmarkedlyobesechildren.Plasmainsulinconcentrationsgreaterthan35pmol/L(5
microIU/mL)withconcomitantplasmaglucosevaluelessthan2.8mM(50mg/dL)aredistinctlyabnormal,regardlessoftheperiodoffasting.
Ifhyperinsulinemiaissuggestedbyoneorbothoftheabovemeasures,thenextstepistodetermineifitisofendogenousorexogenousorigin.AlowCpeptide
concentrationinapatientwithapositiveglycemicresponsetoaglucagonstimulationtestindicatesthatthesourceoftheinsulinisexogenousbecausethebetacell
cosecretesCpeptideinequimolaramountswithinsulin.
Iftheglucagonstimulationtestisclearlypositivebuttheplasmainsulinconcentrationsarelow(andtheCpeptidelevelisalsolow),thepossibilityofexogenousinsulin
administrationshouldbefurtherinvestigated[28].Thisisbecauserecombinantmodifiedhumaninsulinsmaynotbedetectedinthenewmonoclonalsandwichassaysused
bymanycommerciallaboratoriestomeasurespecificallyunmodifiedhumaninsulin.Inthiscase,polyclonalinsulinassaysmustbesoughttodetectexogenousinsulin.(See
"Causesofhypoglycemiaininfantsandchildren",sectionon'Hyperinsulinism'.)
Inaddition,lowconcentrationsofIGFBP1(ifmeasured),providessupportiveevidenceofinappropriatehyperinsulinemiabecauseinsulinpotentlyinhibitsIGFBP1
production[29].(See"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy",sectionon'Biochemicaltests'.)
FattyacidoxidationdisordersIfhyperinsulinemiaisexcluded,wedeterminewhetherthefollowingcharacteristicsarepresent,whichsuggestafattyacid
oxidationdisorder(algorithm1):
ElevatedFFAandacylcarnitineconcentrations.FFAconcentrationsmaybeveryhigh(>1.8mmol/L)infattyacidoxidationdisorders,butalsomaybemoderately
elevatedindisordersofgluconeogenesisorglycogenmetabolism.Thespecificacylcarnitineprofilehelpstoidentifythespecificfattyacidoxidationdisorder(table3).
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
5/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Mildormoderateketosis(betahydroxybutyrate<2.5mmol/L)becauseFFAscannotbeusedforketonebodyformation(table4)thislowlevelofketosisissometimes
termed"inappropriate"forthedegreeofhypoglycemia.
Incontrasttohyperinsulinism,thereisminimalglycemicresponsetoglucagonstimulation,andplasmaconcentrationsofinsulinandCpeptidearenormal.An
exceptionisthatsomedisordersoffattyacidoxidation(eg,hydroxyacylcoenzymeAdehydrogenase,HADH,previouslyknownasshortchainL3hydroxyacylCoA
dehydrogenasedeficiency,SCHAD)cancausedisturbanceofadenosinetriphosphate/adenosinediphosphate(ATP/ADP)ratiosinthebetacellandhavebeen
associatedwithhyperinsulinemia[30].Asaresult,thisdisorderisgroupedwiththemutationscausingpersistenthyperinsulinemichypoglycemiaofinfancy(PHHI).
(See"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy".)
DefectsingluconeogenesisorglycogenmetabolismNext,wedeterminewhetherthefollowingcharacteristicsarepresent,whichsuggestdefective
gluconeogenesisorglycogenmetabolism(algorithm1):
Normalacylcarnitineprofile,usuallywithmildormoderatelyelevatedFFAconcentrations.
Inchildrenwithsevereglucose6phosphatasedeficiency,thebaselineplasmalactateconcentrationwillbesignificantlyelevatedandmayincreasefurtherduringa
glucagonstimulationtest,withnoconcomitantriseinglucose.Forchildrenwithmilderdisease,thebaselinelactateconcentrationmaybeonlymildlyelevatedbutcould
increasedramaticallyduringaglucagonstimulationtest.
Mildormoderateketosis(betahydroxybutyrate<2.5mmol/L)becauseketonesarenotbeingsynthesizedappropriatelyinglycogenstoragediseasetype1(vonGierke
disease)andotherconditionsinwhichdefectivegluconeogenesisexist(table5).(See"Overviewofinheriteddisordersofglucoseandglycogenmetabolism".)
Incontrasttohyperinsulinism,thereisminimalglycemicresponsetoglucagonstimulation,andplasmaconcentrationsofinsulinandCpeptidearenormalorlow.
Mostbutnotallofthedisordersofglycogenolysisandgluconeogenesisareassociatedwithhepatomegalytheycanbefurtherdistinguishedbytheirclinicalfeatures(table
6andtable7),andbyspecificgenetictesting.(See"Causesofhypoglycemiaininfantsandchildren",sectionon'Disordersofcarbohydratemetabolism'.)
KetosisLast,wedeterminewhetherthepatienthadarobust("appropriate")ketoticresponsetotheepisodeofhypoglycemia,ideallymeasuredbyplasmabeta
hydroxybutyrateconcentration(algorithm1).Thisservestoconfirmorrefinethediagnosticcategoryestablishedbytheothertests:
MinimalketosisConsistentwithhyperinsulinemia.Becausethislackofaketoticresponsetohypoglycemiaisabnormal,itissometimestermed"inappropriate."
Mildormoderateketosis(betahydroxybutyrate<2.5mmol/L)Consistentwithdisordersofgluconeogenesisorglycogenmetabolismincludingglycogenstorage
diseasetypeI[31,32],andwithmostfattyacidoxidationdisorders.Themildketosisseeninthesedisordersisalsoconsideredabnormalor"inappropriate"forthe
degreeofhypoglycemia.
Markedketosis(betahydroxybutyrate>2.5mmol/L)Thisfindingisanormal(appropriate)responsetofasting,andisconsistentwithstarvationorprolongedfastingin
anindividualwithoutaninbornerrorofmetabolism.Thisdegreeofketosisisalsoconsistentwithketotichypoglycemia,adisorderofunknowncause,certainglycogen
storagediseases(types0,III,VI,andIX),orwithdeficienciesofgrowthhormoneorcortisol[33].(See"Causesofhypoglycemiaininfantsandchildren",sectionon
'Ketotichypoglycemia'and"Overviewofinheriteddisordersofglucoseandglycogenmetabolism".)
Disordersofaminoacidororganicacidmetabolismalsotendtohaveketosisduringhypoglycemia.Thepresenceorabsenceofhepatomegalyandmeasurementof
qualitativeurineorganicacidscanhelptodistinguishamongthesepossibilities.(See"Organicacidemias".)
Markedlyelevatedketoneswithrelativelymildhypoglycemiamaybeseenindisordersofketolysis.Thesedisordersarerareandcanbescreenedforbythefindingof
elevatedbetahydroxybutyrateafteranovernightfastandindeedeveninthefedstate(>0.2mmol/L).TheyincludesuccinylCoA:3ketoacidCoAtransferase(SCOT)
deficiency(MIM#245050),alphamethylacetoaceticaciduria(MIM#203750),andmonocarboxylasetransporter1(MCT1)deficiency(MIM#616095)[34].
AdditionaltestingOncethegeneralcategoryofdisorderisidentified,furtherdiagnostictestingcanbeperformedtoidentifythespecificdisorder.Avarietyofdisorders
arediagnosedwithDNAanalyses(eg,defectsinglycogenandfattyacidmetabolism,hyperinsulinemia,defectsingluconeogenesisorglycogenolysis).(See"Inbornerrors
ofmetabolism:Identifyingthespecificdisorder".)
Furtherinformationaboutidentifyingthespecificorderwithineachcategoryisavailableinseparatetopicreviews:
Endogenoushyperinsulinism(See"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy"and"Insulinoma".)
Fattyacidoxidationdisorders(See"Causesofhypoglycemiaininfantsandchildren",sectionon'Disordersoffattyacidmetabolism'and"Metabolicmyopathies
causedbydisordersoflipidandpurinemetabolism".)
Disordersofgluconeogenesisorglycogenmetabolism(See"Causesofhypoglycemiaininfantsandchildren",sectionon'Disordersofcarbohydratemetabolism'.)
Appropriateketosis(See"Causesofhypoglycemiaininfantsandchildren",sectionon'Ketotichypoglycemia'and"Causesofhypoglycemiaininfantsandchildren",
sectionon'Hormonedeficiencies'.)
Ifsuchtargetedtestingdoesnotestablishthediagnosis,thenotherprovocativetestsmaybeconsidered.Asexamples,galactose,fructose,andalaninetolerancetests
maybeperformedinchildrenwithsuspecteddefectsingluconeogenesis(see"Causesofhypoglycemiaininfantsandchildren"),orleucinetolerancetestsforsuspected
hyperinsulinismhyperammonemia(HIHA)syndrome(see"Pathogenesis,clinicalfeatures,anddiagnosisofpersistenthyperinsulinemichypoglycemiaofinfancy",section
on'Glutamatedehydrogenasedefects').However,asageneralrule,thesetestsshouldbeperformedonlyinselectedcircumstancesandbyindividualswhoare
experiencedintheirperformanceandinterpretation.
Ifthediagnosisandappropriatetherapycannotbereasonablydetermined,thechildshouldbetransferredtoacenterpreparedandexperiencedtomakeanevenmore
thoroughevaluationofthechild'sorfamilies'deoxyribonucleicacid(DNA).Usingtotalexomesequencingnewandpreviouslyunrecognizeddisordersmaybeidentified.
Rarely,aliverbiopsymaybenecessarytomeasuredeficienciesofhepaticenzymeswhenallelsehasbeenexhausted.(See"Inbornerrorsofmetabolism:Identifyingthe
specificdisorder".)
SUMMARYANDRECOMMENDATIONSHypoglycemiaininfantsandchildrenrequirespromptrecognitionandtreatmenttopreventpermanentneurologicsequelae.
Clinicalpresentationanddiagnosis
Symptomsofhypoglycemiaincludeneurogenic(autonomic)symptomsandneuroglycopenicsymptoms.Theseverityofsymptomsmayormaynotpredicttheseverity
ofthehypoglycemia.Neuroglycopenicsymptomstypicallyoccuratlowerplasmaglucoselevelsthanautonomicsymptoms.However,withrepeatedepisodesof
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
6/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
hypoglycemia,thethresholdglucoseconcentrationforadrenergicsymptomsdecreases,suchthattheymaynotappearbeforetheonsetofneuroglycopenicsymptoms.
(See'Clinicalfeatures'above.)
Autonomicsymptomsofhypoglycemiainchildrenandadultsareduetoincreasedadrenergicactivity,andincludesweating,weakness,tachycardia,tremor,and
feelingsofnervousness,and/orhunger.(See'Neurogenic(autonomic)symptoms'above.)
Neuroglycopenicsymptomsincludelethargy,irritability,confusion,behaviorthatisoutofcharacter,andhypothermia.Inextremehypoglycemia,seizureandcoma
mayoccur.(See'Neuroglycopenicsymptoms'above.)
Ininfants,symptomsofhypoglycemiaarenonspecificandincludejitteriness,irritability,feedingproblems,lethargy,cyanosis,andtachypnea.(See'Infants'above.)
Whenhypoglycemiaissuspected,arapid(bedside)plasmaglucosedeterminationshouldbeperformed.Ifitislow(50mg/dL[2.7mmol/L]forthisinitialbedside
measurement),criticalsamplesshouldbeobtainedbeforetreatment,ifthiscanbedonewithoutdelayingtreatment.Obtainingcriticalsamplesbeforetheinitiationof
therapy,andcollectingthefirstvoidedurinesample,candramaticallyimprovetheabilitytodiagnosetheetiologyofthehypoglycemiaandsimplifythesubsequent
diagnosticevaluation.(See'Criticalsamples'above.)
TreatmentTreatmentofhypoglycemiavarieswiththedegreeofhypoglycemiaandassociatedsymptoms.Thekeystepsfordiagnosisandtreatmentaresummarizedin
arapidoverview(table2).(See'Immediatemanagement'above.)
Ifthepatientisfullyconsciousandabletodrinkandswallowsafely,arapidlyabsorbedcarbohydrate(eg,glucosetablets,glucosegel,tablesugar,orfruitjuice)should
begivenbymouth.Ifthehypoglycemiadoesnotimprovewithin10to15minutes,parenteralglucosemustbeadministered.(See'Glucosetherapy'above.)
Individualswithalteredconsciousnessand/orwhoareunabletosafelyswallowarapidlyabsorbedcarbohydrateshouldbetreatedwithintravenous(IV)dextrose,ata
doseof0.2to0.25g/kgofbodyweight(maximumsingledose,25grams).Thisisusuallyachievedwith2.5mL/kgof10percentdextrosesolution,givenslowly(2to3
mL/min).(See'Glucosetherapy'above.)
SubsequentmanagementTheIVbolusdescribedaboveshouldbefollowedbyaninfusionofdextrose.Plasmaglucoseshouldbemonitoredevery30to60minutes
andthedextroseinfusionadjustedaccordingly,untilstableplasmaglucoseconcentrationbetween70and120mg/dL(3.9to6.7mmol/L)isattained.Thereafter,
frequencyofglucosemonitoringshouldbedecreasedaccordingtothepatient'sclinicalandbiochemicalresponses.(See'Glucosetherapy'above.)
SulfonylureaoverdoseSymptomatichypoglycemiacausedbysulfonylureaoverdoseismanagedwithbolusesofdextroseandsometimesalsowithoctreotide.(See
"Sulfonylureaagentpoisoning".)
Evaluationforthecause
Causesofhypoglycemiaincludeavarietyofinbornerrorsofmetabolism,hyperinsulinemia,toxicingestions,andavarietyofunderlyingillnesses(table1).The
evaluationtodeterminethecauseisguidedbythefindingsofthehistory,examination,andpreliminarylaboratoryresults.Asexamples,clinicalfeaturestosuggesting
anaccidentalortoxicingestionoraspecificinbornerrorofmetabolismshouldpromptspecifictestingforthesuspecteddisorder.(See'Evaluationforthecauseof
hypoglycemia'above.)
Ifthecauseofthehypoglycemiaisunclear,thecriticalsamplesobtainedduringanepisodeofhypoglycemiaareusedtoidentifythetypeofdisordercausing
hypoglycemia.Acontrolledelectivefastmaybenecessarytocollectthecriticalsamples,butshouldbeperformedonlyafterdisordersoffattyacidoxidationhavebeen
excludedbyperforminganacylcarnitineprofileandurineorganicacidsinthewellstate.Wenarrowthediagnosticpossibilitiesintocategoriesinastepwisesequence,
assummarizedinthealgorithm(algorithm1).(See'Subsequenttestingforunexplainedhypoglycemia'aboveand'Interpretationofresults'above.)
UseofUpToDateissubjecttotheSubscriptionandLicenseAgreement.
Topic5805Version18.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
7/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
GRAPHICS
Glucoseusebythebrainversusothertissues
Estimatedpercentageofglucoserateofdisappearance(Rd)usedbybrainandnonbraintissue
frominfancytoadulthood(n=141).Thetissuedatapointsrepresentthemeanvaluesfor
subjectswithbodyweights,inkg,of0.51.0,1.12.0,2.13.0,3.14.0,4.15.0,5.110,10.115,
15.120.0,20.130.0,30.140.0,40.150.0,50.160.0,60.170,and70.195.0,respectively.
DatafromHaymond,MW,Sunehag,A,EndocrinolMetabClinNorthAm199928:663.
Graphic76157Version1.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
8/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Glucoserateofdisappearance(Rd)
Totalglucoserateofdisappearance(Rd)(mmol/min)asafunctionofbodyweightfrominfancyto
adulthood(n=141bodyweightsrangefrom0.6to94kg).
DatafromHaymond,MW,Sunehag,A.Controllingthesugarbowl.Regulationofglucosehomeostasis
inchildren.EndocrinolMetabClinNorthAm199928:663.
Graphic64790Version1.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
9/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Causesofhypoglycemiaininfantsandchildren
Othernames
OMIM#
Disordersofcarbohydratemetabolism
Disordersofglycogenolysis
Glycogensynthetasedeficiency
GSDtype0a
240600
Glucose6phosphatasedeficiency
GSDtypeIa(vonGierkedisase)orIb
232200or232220
Debrancherdeficiency
GSDtypeIII
232400
Hepaticphosphorylasedeficiency
GSDtypeVI
232700
HepaticphosphorylaseBkinasedeficiency
GSDIXa1,IXbd
306000
Phosphoglucomutase1deficiency
CongenitaldisorderofglycosylationtypeIt
614921
Phosphomannomutase2deficiency
CongenitaldisorderofglycosylationtypeIa
212065
Mannosephosphateisomerasedeficiency
CongenitaldisorderofglycosylationtypeIb
602579
Fructose1,6bisphosphatasedeficiency
229700
Pyruvatecarboxylasedeficiency
266150
PEPCKdeficiency
261650
Galactosemia
230400others
Hereditaryfructoseintolerance
229600
Propionicacidemia
606054
Methylmalonicaciduria
277400others
Glutaricaciduriatype1
231670
201450,others
Persistenthyperinsulinemichypoglycemiaofinfancy
(PHHI)
Familialhyperinsulinemichypoglycemiacongenital
hyperinsulinism
256450601820others
Insulinoma(includinginassociationwithMEN1)
Exogenousadministrationofinsulin(eg,in
Munchausen'ssyndromebyproxyordiabetes
mellitus)
Growthhormonedeficiency
Cortisoldeficiency
Hypothyroidism
Oralhypoglycemics(eg,sulfonylureassuchas
glipizideorglyburide)causeshyperinsulinemia
Ethanol
Salicylates
Betablockers
Pentamidine
Heartdisease
Surgery
Criticalillness(eg,sepsis)
Hepaticfailure
Disordersofglycosylation
Disordersofgluconeogenesis
Disordersofaminoacidmetabolism
Disordersoffattyacidmetabolism
MediumchainacylCoAdehydrogenase(MCAD)and
others
Increasedutilizationofglucose
Hyperinsulinemia
Miscellaneous
Ketotichypoglycemia
Hormonedeficiencies
Ingestions
Other
OMIM:onlineMendelianinheritanceinmandatabaseGSD:glycogenstoragediseasePEPCK:phosphoenolpyruvatecarboxykinasePHHI:persistenthyperinsulinemichypoglycemiaof
infancyMEN1:multipleendocrineneoplasiatype1MCAD:mediumchainacylCoAdehydrogenase.
CourtesyofDrs.MoreyHaymondandAgnetaSunehag.
Graphic103015Version2.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
10/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Rapidoverviewforhypoglycemiainadolescentsandchildren,otherthanneonates
Clinicalfeatures
Anypatientwithacutelethargyorcomashouldhaveanimmediatemeasurementofbloodglucosetodetermineifhypoglycemiaisapossiblecause
Otherfindingsofhypoglycemiaarenonspecific*andvarybyage:
Infants
Irritability
Lethargy
Jitteriness
Feedingproblems
Hypothermia
Hypotonia
Tachypnea
Cyanosis
Apnea
Seizures
Olderchildrenandadolescents
Autonomicresponse(tendstooccurwithbloodglucose<50to65mg/dL)
Sweating
Tachycardia
Palpitations
Tremor
Nervousness
Hunger
Paresthesias
Pallor
Neuroglycopenia
Irritability
Confusion
Uncharacteristicbehavior
Weakness
Seizures
Coma
Occasionally,transientfocalneurologicdeficits
Diagnosis
Obtainrapidbedsidebloodglucoseconcentration(andhydroxybutyrate,ifavailableasapointofcaremeasurement)
Confirmthepresenceofhypoglycemiawithasimultaneouslydrawnplasmaglucose
Treat,asoutlinedbelow,ifthebedsidevalueislow(<70mg/dL[3.89mmol/L])insymptomaticpatients
Obtainabloodsampleforadditionaldiagnosticstudiespriortoglucoseadministration,ifpossible,andcollectthefirstvoidedurineafterthehypoglycemiceventinallinfantsand
youngchildrenwhoarenotbeingtreatedfordiabetesmellitusordonothaveaknowncauseforhypoglycemia
Treatment
Donotdelaytreatmentifsymptomatichypoglycemiaissuspected.However,everyreasonableeffortshouldbemadetoobtainarapidbloodglucosemeasurementpriorto
administeringglucose.
Giveglucosebaseduponthepatientslevelofconsciousnessandabilitytoswallowsafely(ie,alertenoughtodosoandwithintactgagreflex)asfollows:
Consciousandabletodrinkandswallowsafely:
Administer0.3g/kg(10to20g)ofarapidlyabsorbedcarbohydrate.15gissuppliedby3glucosetablets,atubeofgelwith15g,4oz(120mL)sweetenedfruitjuice,6oznondietsoda,or
atablespoon(15mL)ofhoneyortablesugar.Mayrepeatin10to15minutes.
Alteredmentalstatus,unabletoswallow,ordoesnotrespondtooralglucoseadministrationwithin15minutes:
GiveaninitialIVbolusofglucoseof0.25g/kgofdextrose(maximumsingledose25g). Thevolumeandconcentrationofglucosebolusisinfusedslowlyat2to3mLperminuteandbasedupon
age:
2.5mL/kgof10%dextrosesolution(D10W)ininfantsandchildrenupto12yearsofage(10%dextroseis100mg/mL)
1mL/kgof25%dextrose(D25W)or0.5mL/kgof50%dextrose(D50W)inadolescents(25%dextroseis250mg/mL50%dextroseis500mg/mL)
UnabletoreceiveoralglucoseandunabletoobtainIVaccess:
Giveglucagon0.03mg/kgIMorSQ(maximumdose1mg) :
Performbloodglucosemonitoringevery10to15minutesastheeffectsofglucagonmaybetransient
Establishvascularaccessassoonaspossible
Afterinitialhypoglycemiaisreversed,provideadditionalglucoseandtreatmentbaseduponsuspectedetiology:
GivechildrenandadolescentswithtypeIdiabetesmellitusanormaldiet
Givepatientswithanunknowncauseofhypoglycemiaintravenousinfusionofdextrose10%(6to9mg/kgperminute)titratedtomaintainbloodglucoseinasafeand
appropriaterange(70to150mg/dL[3.89to8.33mmol/L])
Givepatients,whohaveingestedasulfonylureaandhaverecurrenthypoglycemia,octreotide(dose:1to1.5mcg/kgIMorSQ,maximumdose150mcgevery6hours)in
additiontoglucose.(RefertoUpToDatetopiconsulfonylureapoisoning).
Measurearapidbloodandplasmaglucose15to30minutesaftertheinitialIVglucosebolusandthenmonitorevery30to60minutesuntilstable(minimumoffourhours)toensure
thatplasmaglucoseconcentrationismaintainedinthenormalrange(>70to100mg/dL[>3.89to5.55mmol/L])
Obtainpediatricendocrinologyconsultationforpatientswithhypoglycemiaofunknowncause
ObtainmedicaltoxicologyconsultationforpatientswithingestionoforalhypoglycemicagentsbycallingtheUnitedStatesPoisonControlNetworkat18002221222
oraccessthe
WorldHealthOrganization'slistofinternationalpoisoncenters(www.who.int/gho/phe/chemical_safety/poisons_centres/en/index.html)
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
11/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Admitthefollowingpatients:
Cannotmaintainnormoglycemiawithoralintake
Hypoglycemiaofunknowncause
Ingestionoflongactinghypoglycemicagents
Recurrenthypoglycemiaduringtheperiodofobservation
IV:intravenousIM:intramuscularSQ:subcutaneousD10W:10%dextroseinwaterD25W:25%dextroseinwaterD50W:50%dextroseinwater.
*Thesefindingsmayalsooccurininfantswithsepsis,congenitalheartdisease,respiratorydistresssyndrome,intraventricularhemorrhage,othermetabolicdisorders,andinchildrenand
adolescentswithavarietyofunderlyingconditions.
Specificlaboratorystudiestoobtaininchildrenincludebloodsamplesforglucose,insulin,Cpeptide,betahydroxybutyrate,lactate(freeflowingbloodmustbeobtainedwithouta
tourniquet),plasmaacylcarnitines,freefattyacids,growthhormone,andcortisol.
Higherdosesofglucose(eg,0.5to1g/kg[5to10mL/kgof10%dextroseinwateror2to4mL/kgof25%dextroseinwater])maybeneededtocorrecthypoglycemiacausedby
sulfonylureaingestion.(Formoredetail,refertoUpToDatetopiconsulfonylureaagentpoisoning).
Glucagonwillreversehypoglycemiacausedbyexcessendogenousorexogenousinsulinandwillnotbeeffectiveinpatientswithinadequateglycogenstores(prolongedfasting),ketotic
hypoglycemia,orareunabletomobilizeglycogen(glycogenstoragediseases).Ofnote,childrenmayexhausttheirglycogenstoresinaslittleas12hours.Otherconditionsinwhichglycogen
cannotbeeffectivelymobilizedincludeethanolintoxicationinchildren,adrenalinsufficiency,andcertaininbornerrorsofmetabolism(eg,adisorderofglycogensynthesisandglycogen
storagediseases).
Graphic83485Version5.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
12/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Algorithmforevaluationofaninfantorchildwithhypoglycemia
BUN:bloodureanitrogenAST:aspartateaminotransferaseALT:alanineaminotransferaseFFA:freefattyacidsPG:plasmaglucose:elevated:decreasedACTH:adrenocorticotropichormoneNH3:
ammoniaIGFI:insulinlikegrowthfactorIIGFBP3:insulinlikegrowthfactorbindingprotein3T4:thyroxineTSH:thyroidstimulatinghormone(thyrotropin).
*Plasmainsulinlevelsmaybeeitherloworhighifexogenousinsulinhasbeengiven(eg,inMunchausensyndromebyproxy).Thisisbecauserecombinantmodifiedhumaninsulinsmaynotbedetectedin
themonoclonal"sandwich"assaysusedbymanycommerciallaboratoriestomeasureunmodifiedhumaninsulin.Thus,iftheglucagonchallengetestispositive(riseinBG),butmeasuredplasmainsulin
concentrationsarelow(andtheCpeptidelevelisalsolow),polyclonalinsulinassaysmustbesoughttodetectexogenousinsulin.
Acylcarnitineelevationswillbeforaspecificfattyacidoxidationdisorder.
Whenthelactateiselevatedwithouthepatomegaly,considerorganicacidemia,ketolysisdefect,ormitochondrialrespiratorychaindisorder.Ifthelactateispresentwithisolatedhepatomegaly,glycogen
storagediseaseorgluconeogenesisdefectsaresuspected.
Defectsofketolysismaycausemarkedlyelevatedketonesinthesettingofmildhypoglycemia.Thesedisordersarerare,andincludeSCOTdeficiency(MIM#245050),alphamethylacetoaceticaciduria(MIM
#203750),andmonocarboxylasetransporter1deficiency(MIM#616095).
Thyroidfunctiontestsaremeasuredaspartoftheevaluationforpanhypopituitarism.Itisunlikelythatisolatedhypothyroidismcauseshypoglycemia.
Graphic99837Version3.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
13/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Disordersoffattyacidoxidation
Disorders
Acylcarnitineprofileabnormalities
Carnitineuptakedefect
Free(C0)carnitine
ShortchainacylCoAdehydrogenase(SCAD)deficiency
Butyryl(C4)carnitine
ShortchainhydroxyacylCoAdehydrogenase(SCHAD)deficiency
3hydroxybutyryl(C4OH)carnitine
MediumchainacylCoAdehydrogenase(MCAD)deficiency
Octanoyl(C8)carnitine
Decanoyl(C10)carnitine
Decenoyl(C10:1)carnitine
VerylongchainacylCoAdehydrogenase(VLCAD)deficiency
Tetradecenoyl(C14:1)carnitine
Tetradecanoyl(C14)carnitine
Tetradecendioyl(C14:2)carnitine
Dodecanoyl(C12)carnitine
Dodecenoyl(C12:1)carnitine
Hexadecanoyl(C16)carnitine
LongchainhydroxyacylCoAdehydrogenase(LCHAD)deficiency
Hydroxypalmitoyl(C16OH)carnitine
Hydroxyhexadecenoyl(C16:1OH)carnitine
Trifunctionalprotein(TFP)deficiency
Hydroxysteryl(C18OH)carnitine
Hydroxyoleyl(C18:1OH)carnitine
CarnitinepalmitoyltransferaseII(CPTII)deficiency
Carnitineacylcarnitinetranslocase(CACT)deficiency
Palmitoyl(C16)carnitine
Steryl(C18)carnitine
Oleyl(C18:1)carnitine
CarnitinepalmitoyltransferaseI(CPTI)deficiency
Free(C0)carnitine
MultipleacylCoAdehydrogenasedeficiency(glutaricacidemiatypeII)
Inmultiplenonhydroxylatedacylcarnitines
Listofcommonfattyacidoxidationdisordersandassociatedacylcarnitineabnormalities.Notethatthefirstnewbornscreenismostusefulfordiagnosisandthatacylcarnitineprofiles
maybenormalformilderphenotypeswhennotacutelyill.Additionally,forsomeofthelongerchaindisorders(eg,VLCADandCPTII),furthertestingsuchasDNAmutationanalysis
mayberequiredtoestablishadiagnosisdefinitively.
Graphic86411Version5.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
14/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Distinguishingbiochemicalfindingsofinbornerrorsofmetabolism
Findings
Maplesyrup
urinedisease
Urea
cycle
defects
Organic
acidemias
Disordersof
carbohydrate
metabolism
Fattyacid
oxidation
disorders
Mitochondrial
disorders
Peroxisomal
disorders
Lysosomal
storage
disorders
Metabolic
acidosis
++
Respiratory
alkalosis
Hyperammonemia
++
Hypoglycemia
Ketones
A/H
A/H
A/L
A/H
Lacticacidosis
++
:usuallyabsent:sometimespresent+:usuallypresent++:alwayspresentA:appropriateH:inappropriatelyhighL:inappropriatelylow.
*Withindiseasecategories,notalldiseaseshaveallfindingsfordisorderswithepisodicdecompensationclinicalandlaboratoryfindingsmaybepresentonlyduringacutecrisisfor
progressivedisorders,findingsmaynotbepresentearlyinthecourseofdisease.
Adaptedfrom:WeinerDL.MetabolicEmergencies.In:TextbookofPediatricEmergencyMedicine,5thed,FleisherGR,LudwigS,HenretigFM(Eds),Lippincott,Williams&Wilkins,Philadelphia
2006.p.1193.
Graphic76373Version5.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
15/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Disordersofglycogen/glucosemetabolism
Classification
Keyclinicalfindings
Diagnosis
Therapy
GSD0a(MIM#240600,glycogensynthase2deficiencyinliver)
Ketotichypoglycemia,no
hepatomegaly
Liverbiopsyandenzymetesting
DNAtesting
Uncookedcornstarch,
commercialglucosepolymers(eg,
Glycosade),livertransplantation
GSD0b(MIM#611556,muscleglycogensynthasedeficiency)
Cardiomyopathy,exercise
intolerance,weakness
Musclebiopsy(glycogen
depletion),enzymeassay,DNA
testing
Nospecifictreatment
GSDI(MIM#232200GSDIa,vonGierkedisease,glucose6
phosphatasedeficiencyGSDIbduetoqtransportdefect)
Ketotichypoglycemia,
hepatomegaly
DNAtesting,liverbiopsy,and
enzymeassay
Cornstarch,allopurinol,
granulocytecolonystimulating
factor(GCSF),commercial
glucosepolymers(eg,Glycosade),
livertransplantation
Lysosomalacidmaltasedeficiency(MIM#232300,Pompedisease,GSD
II*)
Hypotonia,muscleweakness,
hypertrophiccardiomyopathy,
rhabdomyolysis
Fibroblast,leukocyte,muscle,or
liverenzymeassayDNAtesting
Enzymereplacementtherapy,
commercialglucosepolymers(eg,
Glycosade),livertransplantation
Lysosomeassociatedmembraneprotein2(LAMP2)deficiency(MIM
#300257,Danondisease,GSDIIb *)
Hypotonia,hypertrophic
cardiomyopathy,rhabdomyolysis
Musclebiopsy,DNAtesting
Nospecifictreatment
GSDIII(MIM#232400,glycogendebrancherdeficiency)
Ketotichypoglycemia,
hepatomegaly
Fibroblastorliverenzymeassay
DNAtesting
Uncookedcornstarch,
commercialglucosepolymers(eg,
Glycosade),livertransplantation
GSDIV(MIM#232500,glycogenbranchingenzymedeficiency)
Hepatomegaly,cirrhosis,rare
neuromuscularpresentations,such
asfetalakinesiasequence,
myopathy,axonalneuropathy,adult
polyglucosanbodydisease
Fibroblast,muscle,orliverbiopsy
DNAtesting
Commercialglucosepolymers(eg,
Glycosade),livertransplantation
GSDV(MIM#232600,McArdledisease,musclephosphorylase
deficiency)
Fatigability,myoglobinuria,
rhabdomyolysis
Musclebiopsy,muscleenzyme
assay,DNAtesting
Sucrosepriortoexercise
GSDVI(MIM#232700,Hersdisease,liverphosphorylasedeficiency)
Hepatomegaly,mildhypoglycemia
Liverbiopsyandenzymeassay
DNAtesting
Commercialglucosepolymers(eg,
Glycosade),livertransplantation
GSDVII(MIM#232800,Taruidisease,phosphofructokinasedeficiency
inmuscle)
Fatigability,myoglobinuria,
rhabdomyolysis
Muscleenzymeassay,DNAtesting
Nospecifictreatment
Phosphoglyceratekinasedeficiency(MIM#311800)
Hemolysis,fatigability,
myoglobinuria,CNSdysfunction,
rhabdomyolysis
Muscle/RBCenzymeassayDNA
testing
Bonemarrowtransplantation
GSDIX(phosphorylasekinasedeficiencyIXa1,MIM#306000,formerly
GSDVIII,alpha2subunitdefectinliverIXb,MIM#261750,beta
subunitdefectinliverIXc,MIM#613027,gammasubunitdefectinliver
andmuscleIXd,MIM#300559,alphasubunitdefectinmuscle)
Hepatomegaly,mildhypoglycemia,
fatigability,exerciseintolerance
Liver/musclebiopsyenzyme
assayDNAtesting
Commercialglucosepolymers(eg,
Glycosade),livertransplantation
GSDX(MIM#261670,phosphoglyceratemutasedeficiency)
Fatigability,myoglobinuria,exercise
intolerance,rhabdomyolysis
Musclebiopsyandenzymeassay
DNAtesting
Nospecifictreatment
GSDXI(MIM#612933lactatedehydrogenaseA[LDHA,MIM#150000]
deficiencyandlactatedehydrogenaseBdeficiency[LDHB,MIM
#150100])
Fatigability,myoglobinuria,
rhabdomyolysis
MuscleorRBCenzymeassayDNA
testing
Nospecifictreatment
GLUT2deficiency(MIM#138160FanconiBickelsyndrome)
Growthretardation,renalFanconi
syndrome,galactosemia
Clinicalfeatures,DNAtesting
Smallmeals,cornstarch,
electrolytesasneeded
GSDXII(MIM#611881,aldolaseAdeficiency)
Hemolysis,jaundice,
myoglobinuria,muscleweakness,
fatigability,rhabdomyolysis
MuscleorRBCenzymeassayDNA
testing
Nospecifictreatment
GSDXIII(MIM#612932,betaenolasedeficiencyinmuscle)
Exerciseintolerance,increased
CPK,rhabdomyolysis
Musclebiopsy,enzymeassay,DNA
testing
Nospecifictreatment
GSDXIV(MIM#612934,phosphoglucomutase1deficiencyinmuscle)
Exerciseintolerance,
myoglobinuria,increasedCPK,
rhabdomyolysis,myoglobinuria
Musclebiopsy,enzymeassay,DNA
testing
Nospecifictreatment
GSDXV(MIM#613507,glycogenin1deficiencyinmuscle)
Muscleweakness,arrhythmias
Musclebiopsy(glycogen
depletion),DNAtesting
Nospecifictreatment
GSD:glycogenstoragediseaseMIM:MendelianinheritanceinmanDNA:deoxyribonucleicacidCNS:centralnervoussystemRBC:redbloodcellGLUT2:glucosetransporter2CPK:
creatininephosphokinase.
*Thesediseaseswereoriginallyclassifiedasglycogenstoragesdiseases.Itwassubsequentlyrecognizedthattheaccumulationofglycogeninlysosomesseeninthesediseasesisdueto
defectivelysosomalmetabolismratherthanenergydeficiencyfromglycogen/glucosemetabolism.Thus,theyareconsideredbothglycogenstoragediseasesandlysosomalstoragediseases.
Graphic54417Version12.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
16/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Clinicalandlaboratoryfeaturesofhepaticenzymedeficienciesofglycogenmetabolisminchildren
Enzyme
deficiency
Glycogen
synthase(GSD
0)
Lacticacid
*
Uricacid
Ketosis
+
Serumlipids
Response
toglucagon
Clinicalfeatures
Normalliversize
Neonatalonset
Severefastinghypoglycemia,butpostprandialhyperglycemiaandlactic
acidosis
Glucose6
phosphatase
(GSDI)
Hepatomegaly
Neonatalonset
Severefastinghypoglycemia
Somepatientshaveneutropenia,plateletdysfunction,renaldiseaseor
hypertension
Glycogen
debrancher
(GSDIII)
Normalor
Normal
Normalor
Normaltwo
hoursafter
glucosemeal,
butabsentafter
fast
Hepatomegaly
Onsetininfancy
Mildfastinghypoglycemia
Mayhavecardiacorskeletalmusclemanifestations(eg,elevatedCK)
MayhaveelevatedRBCglycogen
Hepatic
phosphorylase
(GSDVI)
Normal
Hepatic
phosphorylaseb
kinase
Normal
Normal
Normalor
Usuallynormal,
butvariable
Hepatomegaly
Onsetinearlychildhood
Mildfastinghypoglycemia
Normalor
Normalor
Normal
Hepatomegaly
Onsetinearlychildhood
Mildfastinghypoglycemia
Xlinkedinheritance
GSD:glycogenstoragediseaseCK:creatinekinaseRBC:redbloodcell+:present.
*Postprandial.
Graphic51949Version6.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
17/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
Clinicalandlaboratoryfeaturesofhepaticenzymedeficienciesofgluconeogenesisinchildren
Enzyme
deficiency
G6P
Lactic
acid
Uric
acid
Serum
lipids
Ketosis
Responseto
glucagon
Comment
Hepatomegaly
Neonatalonset
Severefastinghypoglycemia
Somepatientshaveneutropenia,plateletdysfunction,renaldiseaseor
hypertension
F16DP
(whenfed,notwhen
fasted)
Mild/moderatehepatomegaly
Moderatehypoglycemia
Onsetininfancy
Muscularweakness
Failuretothrive
Hyperalaninemia
PEPCK
Normal
Onsetininfancy
Severehypoglycemia
Elevatedtransaminases
Coagulationabnormalities
Fattyliver,fattykidneys
PC
Normal
Normalor
Onsetininfancy,withearlydeath
Mildhypoglycemia
Severementalretardation
Subacutenecrotizingencephalopathy
G6P:glucose6phosphataseF16DP:fructose1,6,diphosphatasePEPCK:phospholenolpyruvatecarboxykinasePC:pyruvatecarboxylase:increased:decreased+:present:may
ormaynotbepresent.
Graphic71999Version2.0
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
18/19
12/5/2016
ApproachtohypoglycemiaininfantsandchildrenUpToDate
ContributorDisclosures
AgnetaSunehag,MD,PhD Nothingtodisclose MoreyWHaymond,MD Consultant/AdvisoryBoards:AegerionPharmaceuticalsInc[Reviewaregistry(Metreleptin)]
AstraZeneca[diabetes(Exenatide)]DaiichiSankyo[WellkidsStudy(Colesevelamhydrochloride)]NationalInstitutesofHealth[Dataandsafetymonitoringboards(Life
Momstudy)]NovoNordisk[Obesity]XerisPharmaceuticals,Inc[Glucagonandhypoglycemia(nonaqueousglucagonformulation)]. JosephIWolfsdorf,MB,
BCh Nothingtodisclose AlisonGHoppin,MD Nothingtodisclose
Contributordisclosuresarereviewedforconflictsofinterestbytheeditorialgroup.Whenfound,theseareaddressedbyvettingthroughamultilevelreviewprocess,and
throughrequirementsforreferencestobeprovidedtosupportthecontent.AppropriatelyreferencedcontentisrequiredofallauthorsandmustconformtoUpToDate
standardsofevidence.
Conflictofinterestpolicy
https://www.uptodate.com/contents/approachtohypoglycemiaininfantsandchildren/print
19/19
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Nursing Diagnosis For DKADocumento6 pagineNursing Diagnosis For DKARhanne Bolante88% (24)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- UWorld Step 3 NotesDocumento91 pagineUWorld Step 3 Noteshellayeah75% (4)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Goljan Step 1 HY 36 Pages Notes PDFDocumento36 pagineGoljan Step 1 HY 36 Pages Notes PDFTyler Lawrence CoyeNessuna valutazione finora
- Chapter 18 - The NewbornDocumento6 pagineChapter 18 - The NewbornEunice Cortés0% (1)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Pediatrics Oral ExamDocumento13 paginePediatrics Oral ExamOmar Nayef TaaniNessuna valutazione finora
- High Yield PsychiatryDocumento43 pagineHigh Yield Psychiatryconfusedmage91% (11)
- Radiology NotesDocumento21 pagineRadiology NotesOmar Nayef Taani83% (6)
- Herb Drug Interaction Chart From MediherbDocumento5 pagineHerb Drug Interaction Chart From Mediherbquinn941Nessuna valutazione finora
- Orthodontics in Medically CompromisedDocumento189 pagineOrthodontics in Medically CompromisedAshish MathewNessuna valutazione finora
- أسئلة امتحان الإقامة تكنوDocumento10 pagineأسئلة امتحان الإقامة تكنومحمد حميدانNessuna valutazione finora
- Residency Exam JustDocumento19 pagineResidency Exam JustOmar Nayef TaaniNessuna valutazione finora
- British Council IELTS-Writing and Speaking ExamplesDocumento12 pagineBritish Council IELTS-Writing and Speaking ExamplesBehrooz YaghmaeyanNessuna valutazione finora
- Diagnosis and Management of Glucose-6-Phosphate Dehydrogenase Deficiency - UpToDateDocumento18 pagineDiagnosis and Management of Glucose-6-Phosphate Dehydrogenase Deficiency - UpToDateOmar Nayef TaaniNessuna valutazione finora
- Internal OSCE All Past Years QuestionsDocumento17 pagineInternal OSCE All Past Years QuestionsOmar Nayef TaaniNessuna valutazione finora
- What Is The Position of The Arm With An Erb's Palsy?: Hide Related Topic DetailsDocumento8 pagineWhat Is The Position of The Arm With An Erb's Palsy?: Hide Related Topic DetailsOmar Nayef TaaniNessuna valutazione finora
- Ielts Task 2 How To Write at A 9 LevelDocumento37 pagineIelts Task 2 How To Write at A 9 Leveljanit693984% (19)
- 12 Week Us Mle ScheduleDocumento5 pagine12 Week Us Mle ScheduleGaetano Di GiovanniNessuna valutazione finora
- British Council IELTS-Writing and Speaking ExamplesDocumento12 pagineBritish Council IELTS-Writing and Speaking ExamplesBehrooz YaghmaeyanNessuna valutazione finora
- Urology XDocumento3 pagineUrology XOmar Nayef TaaniNessuna valutazione finora
- Ielts Band 9Documento7 pagineIelts Band 9Omar Nayef TaaniNessuna valutazione finora
- Sickle Cell Anemia PDFDocumento2 pagineSickle Cell Anemia PDFOmar Nayef TaaniNessuna valutazione finora
- Mental Status Examination Rapid Record Form: CatatoniaDocumento3 pagineMental Status Examination Rapid Record Form: CatatoniaNicole TangcoNessuna valutazione finora
- Sickle Cell Anemia PDFDocumento2 pagineSickle Cell Anemia PDFOmar Nayef TaaniNessuna valutazione finora
- Thoracic TraumaDocumento9 pagineThoracic TraumaOmar Nayef TaaniNessuna valutazione finora
- Acute Abdomen in ChildrenDocumento12 pagineAcute Abdomen in ChildrenOmar Nayef TaaniNessuna valutazione finora
- Thoracic TraumaDocumento9 pagineThoracic TraumaOmar Nayef TaaniNessuna valutazione finora
- Obstetric and Gynecology Syllabus PDFDocumento1 paginaObstetric and Gynecology Syllabus PDFOmar Nayef TaaniNessuna valutazione finora
- Pharmacological Potentiality and Medicinal Uses of Ipomoea Aquatica A ReviewDocumento4 paginePharmacological Potentiality and Medicinal Uses of Ipomoea Aquatica A ReviewVianca DizonNessuna valutazione finora
- SRNA Orientation ChecklistDocumento40 pagineSRNA Orientation Checklistihtisham1Nessuna valutazione finora
- Pass Critical Care Endocrine Frcem ResourcesDocumento41 paginePass Critical Care Endocrine Frcem ResourcesYoussef SaadNessuna valutazione finora
- AlcoholismDocumento22 pagineAlcoholismChenly RocutanNessuna valutazione finora
- NovoRapid (Insulin Aspart) PDFDocumento113 pagineNovoRapid (Insulin Aspart) PDFAchmad SuryadiNessuna valutazione finora
- Multiple Choice Questions (MCQ) Topic Quiz Communication and HomeostasisDocumento29 pagineMultiple Choice Questions (MCQ) Topic Quiz Communication and HomeostasisS RamoutarNessuna valutazione finora
- Presenter: Dr. P. Usha Rani Resident, ASRAMS, EluruDocumento60 paginePresenter: Dr. P. Usha Rani Resident, ASRAMS, EluruDivya Rekha KolliNessuna valutazione finora
- Diabetes MellitusDocumento11 pagineDiabetes MellitusChristinaRegatilloNessuna valutazione finora
- Faysal Bas It,+12-15Documento4 pagineFaysal Bas It,+12-15IT RSMPNessuna valutazione finora
- Humulin R: Regular U-500 (Concentrated) Insulin Human Injection, Usp (Rdna Origin)Documento7 pagineHumulin R: Regular U-500 (Concentrated) Insulin Human Injection, Usp (Rdna Origin)Rebecca BlackburnNessuna valutazione finora
- ADA-EASD Consensus Report 2022 - Diab CareDocumento34 pagineADA-EASD Consensus Report 2022 - Diab CarePéter BarnaNessuna valutazione finora
- Coping With AnxietyDocumento10 pagineCoping With AnxietyRenato De GuzmanNessuna valutazione finora
- Blood Glucose MonitoringDocumento20 pagineBlood Glucose Monitoringask1400100% (1)
- Diabetes MellitusDocumento49 pagineDiabetes MellitusValarmathiNessuna valutazione finora
- Ms DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesDocumento9 pagineMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesMs DiabetesLariza LopegaNessuna valutazione finora
- Surprising Benefits of Bitter Melon For DiabetesDocumento41 pagineSurprising Benefits of Bitter Melon For DiabetesnajihahNessuna valutazione finora
- NCMB316 Lec MidtermDocumento28 pagineNCMB316 Lec Midterm2 - GUEVARRA, KYLE JOSHUA M.Nessuna valutazione finora
- Finals ReviewerDocumento3 pagineFinals ReviewerMary Ann SacramentoNessuna valutazione finora
- Nutrition Essentials A Personal Approach 1st Edition Schiff Solutions Manual 1Documento14 pagineNutrition Essentials A Personal Approach 1st Edition Schiff Solutions Manual 1annie100% (60)
- Tugas Bahasa Inggris "Diabetes": Shendy Wira Putra (183310822)Documento6 pagineTugas Bahasa Inggris "Diabetes": Shendy Wira Putra (183310822)Adilla SyafniNessuna valutazione finora
- CKD Case StudyDocumento8 pagineCKD Case StudyEspiridionNessuna valutazione finora
- Exercise 5 Endocrine Lab RepDocumento22 pagineExercise 5 Endocrine Lab RepChippy RabeNessuna valutazione finora
- Petition SC11-1622 Writ Mandamus Florida Supreme Court Jan-09-2012Documento59 paginePetition SC11-1622 Writ Mandamus Florida Supreme Court Jan-09-2012Neil GillespieNessuna valutazione finora
- Robert WillnerAids DenialistDocumento40 pagineRobert WillnerAids Denialistsibby11Nessuna valutazione finora
- EndocrineDocumento5 pagineEndocrineChaina MacaspacNessuna valutazione finora
- 10 11648 J Ijde 20200502 12Documento4 pagine10 11648 J Ijde 20200502 12AdemoluNessuna valutazione finora