Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Risk For Decreased Cardiac Output
Caricato da
Sid Artemis FriasDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Risk For Decreased Cardiac Output
Caricato da
Sid Artemis FriasCopyright:
Formati disponibili
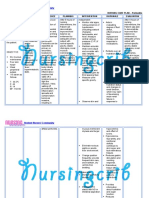
ASSESSME
NT
Subjective:
hirap akong
huminga. As
verbalized by
the patient
Objective:
Decreased
performance
Irritability
Jittery
behavior
V/S
taken as
follows:
T: 37.3
P: 89
R: 21
Bp: 120/70
DIAGNOSI
S
Decreased
Cardiac
Output
SCIENTIFIC
PLANNING
RATIONALE
Hyprlasia of the After the nursing
thyroid gland
intervention the
client will be
Increase t3 and able to maintain
t4 production
adequate cardiac
output for tissue
Increase amount needs as
of thyroid
evidenced by
hormone in
stable vital signs,
tissue
palpable
peripheral
Increase
pulses, good
vascularity and capillary refill,
blood flow
usual mentation,
and absence of
Increase cardiac dysrhythmias.
acitivity
Decrease
blinking
response in eyes
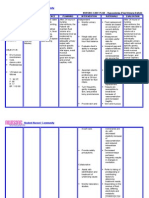
INTERVENTIONS
RATIONALE
EVALUATION
Monitor central venous pressure
(CVP), if available.
General or orthostatic hypotension may
occur as a result of excessive peripheral
vasodilation and decreased circulating
volume. Widened pulse pressure reflects
compensatory increase in stroke volume and
decreased systemic vascular resistance
(SVR).
Investigate reports of chest pain or
angina
Provides more direct measure of circulating
volume and cardiac function.
.Assess pulse and heart rate while
patient is sleeping.
May reflect increased myocardial oxygen
demands or ischemia.
Auscultate heart sounds, note extra
heart sounds, development of gallops
and systolic murmurs.
Provides a more accurate assessment of
tachycardia.
After the nursing
intervention the
client will be
able to
maintained
adequated
cardiac output
for tissue needs
as evidenced by
stable vital signs,
palpable
peripheral
pulses, good
capillary refill,
usual mentation,
and absence of
dysrhythmias.
independent
Monitor BP lying, sitting, and standing,
if able. Note widened pulse pressure.
Monitor ECG, noting rate and rhythm.
Document dysrhythmias.
Auscultate breath sounds. Note
adventitious sounds.
Palpitation
Cardiac failure
Monitor temperature; provide cool
environment, limit bed linens or
clothes, administer tepid sponge baths.
Observe signs and symptoms of severe
Prominent S1 and murmurs are associated
with forceful cardiac output of
hypermetabolic state; development of S3
may warn of impending cardiac failure.
Tachycardia (greater than normally
expected with fever and/or increased
circulatory demand) may reflect direct
myocardial stimulation by thyroid hormone.
Dysrhythmias often occur and may
compromise cardiac output.
thirst, dry mucous membranes, weak or
thready pulse, poor capillary refill,
decreased urinary output, and
hypotension.
Record I&O. Note urine specific
gravity.
Weigh daily. Encourage chair rest or
bedrest. Limit unnecessary activities.
Note history of asthma and
bronchoconstrictive disease, sinus
bradycardia and heart blocks, advanced
HF, or current pregnancy.
Observe for adverse side effects of
adrenergic antagonists: severe decrease
in pulse, BP; signs of vascular
congestion/HF; cardiac arrest.
Early sign of pulmonary congestion,
reflecting developing cardiac failure
Fever (may exceed 104F) may occur as a
result of excessive hormone levels and can
aggravate diuresis and/or dehydration and
cause increased peripheral vasodilation,
venous pooling, and hypotension.
Rapid dehydration can occur, which reduces
circulating volume and compromises
cardiac output.
Significant fluid losses through vomiting,
diarrhea, diuresis, and diaphoresis can lead
to profound dehydration, concentrated
urine, and weight loss.
Activity increases metabolic and circulatory
demands, which may potentiate cardiac
failure.
Administer IV fluids as indicated.
Collaborative:
Administer medications as indicated:
Thyroid hormone antagonists:
propylthiouracil (PTU),
[beta]-blockers: propranolol (Inderal)
Presence or potential recurrence of these
conditions affects choice of therapy. For
example: use of [beta]-adrenergic blocking
agents is contraindicated.
Indicates need for reduction or
discontinuation of therapy.
Rapid fluid replacement may be necessary
to improve circulating volume but must be
balanced against signs of cardiac failure and
need for inotropic support.
Collaborative:
May be definitive treatment or used to
prepare patient for surgery; but effect is
slow and so may not relieve thyroid storm.
Once PTU therapy is begun, abrupt
withdrawal may precipitate thyroid crisis.
Acts to prevent release of thyroid hormone
into circulation by increasing the amount of
thyroid hormone stored within the gland.
May interfere with RAI treatment and may
exacerbate the disease in some people.
Given to control thyrotoxic effects of
tachycardia, tremors, and nervousness and
is first drug of choice for acute storm.
Decreases heart rate or cardiac work by
blocking [beta]-adrenergic receptor sites
and blocking conversion of T4 to T3. If
severe bradycardia develops, atropine may
be required. Blocks thyroid hormone
synthesis and inhibits peripheral conversion
of T4 to T3.
Potrebbero piacerti anche
- Cardiac Failure: Definition: Compensatory Changes in Heart FailureDocumento5 pagineCardiac Failure: Definition: Compensatory Changes in Heart FailureMatyie SmkasNessuna valutazione finora
- Congestive Heart FailureDocumento6 pagineCongestive Heart Failureseigelystic100% (1)
- Integumentary SystemDocumento16 pagineIntegumentary Systemshenric16100% (8)
- Immunization in Children: Mary Beth F. Tanco, MD, FPPS Active Consultant Institute of Pediatrics and Child HealthDocumento92 pagineImmunization in Children: Mary Beth F. Tanco, MD, FPPS Active Consultant Institute of Pediatrics and Child HealthPolychase Magaoay100% (1)
- Ncp-Ob WardDocumento3 pagineNcp-Ob WardAshanti PiNessuna valutazione finora
- COCO OIL MTC - The Mystery of Autism Solved - Bruce FifeDocumento6 pagineCOCO OIL MTC - The Mystery of Autism Solved - Bruce Fifemarmar6382Nessuna valutazione finora
- NCPDocumento9 pagineNCPTracy Camille EscobarNessuna valutazione finora
- Telephone DirectoryDocumento4 pagineTelephone DirectoryAnonymous QL0z40Fs9vNessuna valutazione finora
- NCP Decreased Cardiac Output 1Documento2 pagineNCP Decreased Cardiac Output 1Arnel MacabalitaoNessuna valutazione finora
- Ineffective Renal Tissue PerfusionDocumento2 pagineIneffective Renal Tissue PerfusionHendra Tanjung100% (4)
- Ineffective Tissue PerfusionDocumento1 paginaIneffective Tissue PerfusionEm Castillo50% (2)
- Acute Pain Related To Tissue Trauma and InjuryDocumento4 pagineAcute Pain Related To Tissue Trauma and Injuryprickybiik50% (2)
- Myocarditis NCP 2Documento8 pagineMyocarditis NCP 2astro_aaron117375% (4)
- Ineffective Tissue PerfusionDocumento2 pagineIneffective Tissue PerfusionClaidelyn De Leyola100% (1)
- Abdominal Examination: OSCE ChecklistDocumento2 pagineAbdominal Examination: OSCE ChecklistWafa Abdalla100% (2)
- HEALTH TALK Care of Depression PatientDocumento17 pagineHEALTH TALK Care of Depression PatientAmit RanjanNessuna valutazione finora
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocumento4 pagineNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- Nursing Care Plan2 CVADocumento4 pagineNursing Care Plan2 CVAhermesdave1Nessuna valutazione finora
- NCP For SVTDocumento6 pagineNCP For SVTRen VillenaNessuna valutazione finora
- Nursing Care Plans For Decreased Cardiac OutputDocumento4 pagineNursing Care Plans For Decreased Cardiac OutputCarmela Balderas Romantco80% (5)
- Acute Heart FailureDocumento18 pagineAcute Heart FailureGeorge GeorgeNessuna valutazione finora
- Assessment Diagnosis Scientific Rationale Planning Interventions Rationale Evaluation Subjective: Short-Term OutcomeDocumento3 pagineAssessment Diagnosis Scientific Rationale Planning Interventions Rationale Evaluation Subjective: Short-Term OutcomeSid Artemis Frias100% (4)
- NCPDocumento4 pagineNCPRachel PerandoNessuna valutazione finora
- NCP AneurysmDocumento4 pagineNCP AneurysmJanielle Christine Monsalud100% (1)
- Types of Movement &, ExerciseDocumento23 pagineTypes of Movement &, ExerciseAhmed50% (2)
- NCP AfDocumento3 pagineNCP AfAngelica Mercado SirotNessuna valutazione finora
- WHO Classification of Head and Neck TumoursDocumento349 pagineWHO Classification of Head and Neck TumoursdrAlbertoVV100% (2)
- Lumunok at Huminga, Nabibilaukan Din Ako Madalas" AsDocumento4 pagineLumunok at Huminga, Nabibilaukan Din Ako Madalas" AsPatricia Ortega100% (1)
- Diagnosis and Management of Treatment Refractory HypothyroidismDocumento17 pagineDiagnosis and Management of Treatment Refractory HypothyroidismMerlyn AngelinaNessuna valutazione finora
- Heart FailureDocumento39 pagineHeart FailureMuhammad AsifNessuna valutazione finora
- Nursing Care Plan For Peritonitis NCPDocumento2 pagineNursing Care Plan For Peritonitis NCPderic86% (7)
- Ineffective Tissue PerfusionDocumento2 pagineIneffective Tissue PerfusionDiane ReyNessuna valutazione finora
- NCPDocumento3 pagineNCPJezza RequilmeNessuna valutazione finora
- Nursing Care PlanDocumento3 pagineNursing Care PlanJayalakshmi David50% (2)
- NCP - Excessive Fluid VolumeDocumento4 pagineNCP - Excessive Fluid VolumeryanNessuna valutazione finora
- NCPDocumento6 pagineNCPKyla Carbonel100% (1)
- Hypertension Nursing Care PlanDocumento1 paginaHypertension Nursing Care PlanSheila Mae Cabahug100% (1)
- NCP 1Documento1 paginaNCP 1hsiriaNessuna valutazione finora
- NCP Pain HypertensionDocumento3 pagineNCP Pain HypertensionEzron Kendrick Duran50% (2)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocumento2 pagineNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Nursing Care PlanDocumento9 pagineNursing Care PlanJam AbantaoNessuna valutazione finora
- CRF Fluid Volume Excess NCPDocumento3 pagineCRF Fluid Volume Excess NCPchubbielitaNessuna valutazione finora
- Deficit)Documento2 pagineDeficit)Lee DeeNessuna valutazione finora
- Activity Intolerance Related To AmeniaDocumento1 paginaActivity Intolerance Related To AmeniaSiti Syazana Mohamad MogriNessuna valutazione finora
- Nursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NDocumento2 pagineNursing Care Plan: Date/ Time Assessment Nursing Diagnosis Planning Intervention Evaluatio NnananaNessuna valutazione finora
- NCP and DStudyDocumento8 pagineNCP and DStudyJessica Rosan Hewald ManapatNessuna valutazione finora
- NCP For Ruptured AppendicitisDocumento2 pagineNCP For Ruptured AppendicitisJansen Arquilita RiveraNessuna valutazione finora
- NCP Risk Infection Papillary Thyroid CADocumento2 pagineNCP Risk Infection Papillary Thyroid CAjazvNessuna valutazione finora
- Ncp'sDocumento8 pagineNcp'sDuchess Kleine RafananNessuna valutazione finora
- NCP LocDocumento2 pagineNCP LocMel RodolfoNessuna valutazione finora
- Hyperthermia NCPDocumento3 pagineHyperthermia NCPJayr DiazNessuna valutazione finora
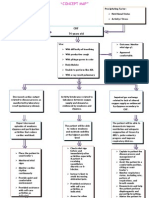
- Concept Map - Abby !Documento2 pagineConcept Map - Abby !Abegail Abaygar100% (3)
- TB, Ineffectivbe Breathing PatternsDocumento1 paginaTB, Ineffectivbe Breathing PatternsnikkilyceeNessuna valutazione finora
- Activity Intolerance Related To Decrease Blood FlowDocumento3 pagineActivity Intolerance Related To Decrease Blood FlowDarkCeades100% (3)
- Ncp-Ineffective Tissue Perfusion (Aortic Stenosis)Documento2 pagineNcp-Ineffective Tissue Perfusion (Aortic Stenosis)Daniel Vergara Arce67% (3)
- Nursing Care Plan Rheumatoid ArthritisDocumento3 pagineNursing Care Plan Rheumatoid ArthritisJashAnia MarIe EvArdo FloresNessuna valutazione finora
- Nursing Care PlanDocumento13 pagineNursing Care PlanCris Solis33% (3)
- NCP For CTTDocumento1 paginaNCP For CTTJen Rhae LimNessuna valutazione finora
- NCP InfectionDocumento3 pagineNCP InfectionPrince AhmirNessuna valutazione finora
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocumento3 pagineAssessment Diagnosis Planning Implementation Rationale Evaluationria_soriano_2Nessuna valutazione finora
- Nursing Care Plan Renal FailureDocumento2 pagineNursing Care Plan Renal FailureMark Jason Rabadan100% (1)
- Word Ncp.......... TetanusDocumento6 pagineWord Ncp.......... TetanusaianrNessuna valutazione finora
- Compartment Syndrome NCP (PAIN)Documento2 pagineCompartment Syndrome NCP (PAIN)eunica16Nessuna valutazione finora
- Heart To HeartDocumento110 pagineHeart To HeartmahyorwaNessuna valutazione finora
- Congestive Cardiac FailureDocumento20 pagineCongestive Cardiac FailureAnand VaghasiyaNessuna valutazione finora
- Congestive Heart Failure: Mulualem W.MD Dmu, Department of Internal Medicine For Ho StudentsDocumento27 pagineCongestive Heart Failure: Mulualem W.MD Dmu, Department of Internal Medicine For Ho Studentsmuluneh birhaneNessuna valutazione finora
- Clinical Aspect of Heart FailureDocumento67 pagineClinical Aspect of Heart FailureAri Bandana TasrifNessuna valutazione finora
- Hypertension: Nursing Care PlansDocumento7 pagineHypertension: Nursing Care PlansSamah AdnanNessuna valutazione finora
- HipotensiDocumento12 pagineHipotensiAfdhalia Khairunnisa SyammarhanNessuna valutazione finora
- Decreased Urine OutputDocumento3 pagineDecreased Urine OutputSj 斗力上Nessuna valutazione finora
- Cardiac Failure: Dr. Abdul Ghani WaseemDocumento33 pagineCardiac Failure: Dr. Abdul Ghani WaseemFarwaNessuna valutazione finora
- Nursing Care Plan HF FinalDocumento10 pagineNursing Care Plan HF FinalCristina L. JaysonNessuna valutazione finora
- Name of Drug Actions Indications Contraindications Nursing Responsibilities Brand NameDocumento1 paginaName of Drug Actions Indications Contraindications Nursing Responsibilities Brand NameSid Artemis FriasNessuna valutazione finora
- Joy Joy Joy LyricsDocumento1 paginaJoy Joy Joy LyricsSid Artemis FriasNessuna valutazione finora
- NJKFANFJKANSZJFNZDDocumento4 pagineNJKFANFJKANSZJFNZDSid Artemis FriasNessuna valutazione finora
- Name: - 2. AgeDocumento2 pagineName: - 2. AgeSid Artemis FriasNessuna valutazione finora
- V. Implementation Management A. MedicationsDocumento3 pagineV. Implementation Management A. MedicationsSid Artemis FriasNessuna valutazione finora
- Frias, Sid Artemis B. Bsn3ADocumento2 pagineFrias, Sid Artemis B. Bsn3ASid Artemis FriasNessuna valutazione finora
- International Journal of Pediatric OtorhinolaryngologyDocumento8 pagineInternational Journal of Pediatric OtorhinolaryngologySid Artemis FriasNessuna valutazione finora
- Graph Showing Hooke's Law. Extension Is Plotted Against ForceDocumento1 paginaGraph Showing Hooke's Law. Extension Is Plotted Against ForceSid Artemis FriasNessuna valutazione finora
- Frailty Definition FriedDocumento12 pagineFrailty Definition FriedSid Artemis FriasNessuna valutazione finora
- Validity of Fatigue Severity Scale PDFDocumento2 pagineValidity of Fatigue Severity Scale PDFSid Artemis FriasNessuna valutazione finora
- Validity of Fatigue Severity Scale PDFDocumento2 pagineValidity of Fatigue Severity Scale PDFSid Artemis FriasNessuna valutazione finora
- Frailty Definition FriedDocumento12 pagineFrailty Definition FriedSid Artemis FriasNessuna valutazione finora
- Validity of Fatigue Severity Scale 1.2Documento8 pagineValidity of Fatigue Severity Scale 1.2Sid Artemis FriasNessuna valutazione finora
- Precautions - Isolation Precautions - Guidelines Library - Infection Control - CDCDocumento6 paginePrecautions - Isolation Precautions - Guidelines Library - Infection Control - CDCKomite PPI RSUDPCNessuna valutazione finora
- NCM 106: Care of Clients With Problems in Cellular Aberrations, Acute Biologic Crisis, Emergency and Disaster NursingDocumento41 pagineNCM 106: Care of Clients With Problems in Cellular Aberrations, Acute Biologic Crisis, Emergency and Disaster NursingJhensczy Hazel Maye AlbaNessuna valutazione finora
- Schistosoma Japonicum..HandoutDocumento17 pagineSchistosoma Japonicum..HandoutKhairulAmranAn-naml100% (1)
- Life-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGDocumento2 pagineLife-Saving Esophageal Intubation in Neonate With Undiagnosed Tracheal Agenesis (A & A Case Reports, Vol. 9, Issue 1) (2017) DGDFGMahdi WashahaNessuna valutazione finora
- The ADHD Diagnosis GuideDocumento13 pagineThe ADHD Diagnosis GuideArunima KapoorNessuna valutazione finora
- Malignant Skin Tumours: Dr. Abdulqadir M. MoalimDocumento40 pagineMalignant Skin Tumours: Dr. Abdulqadir M. MoalimMaxamed DananNessuna valutazione finora
- Infectious Diseases For InternsDocumento60 pagineInfectious Diseases For InternsMaya SwariNessuna valutazione finora
- Eating DisordersDocumento3 pagineEating DisordersAscendente LunaNessuna valutazione finora
- Nursing Care Plan #1: Assessment Diagnosis (NANDA-based) Planning Implementation Rationale EvaluationDocumento9 pagineNursing Care Plan #1: Assessment Diagnosis (NANDA-based) Planning Implementation Rationale EvaluationJoe RealNessuna valutazione finora
- Blood Component TherapyDocumento8 pagineBlood Component TherapyquerokeropiNessuna valutazione finora
- Minor Disorders of PregnancyDocumento36 pagineMinor Disorders of Pregnancysamakayigrace808Nessuna valutazione finora
- Pituitary TumorsDocumento6 paginePituitary Tumorsapi-271668042Nessuna valutazione finora
- WCPD 2016 CP Diagnosis Treatment Infographic WORLD PDFDocumento1 paginaWCPD 2016 CP Diagnosis Treatment Infographic WORLD PDFGeorgina HughesNessuna valutazione finora
- Weather The Storm With Homeopathy - Homeopathy - Modern MedicineDocumento4 pagineWeather The Storm With Homeopathy - Homeopathy - Modern MedicineShubhankar BhowmickNessuna valutazione finora
- Guidelines TX of HPNDocumento3 pagineGuidelines TX of HPNjheyfteeNessuna valutazione finora
- Essentials of Communication Sciences Disorders 2nd Edition Ebook PDFDocumento61 pagineEssentials of Communication Sciences Disorders 2nd Edition Ebook PDFian.costa277100% (50)
- Distal Radius FracturesDocumento68 pagineDistal Radius Fracturescalvin_c_wangNessuna valutazione finora
- Sports Medicine Protocol Patella Fracture ORIFDocumento1 paginaSports Medicine Protocol Patella Fracture ORIFJuwitaNessuna valutazione finora
- 12 Lead Electrocardiogram (Ecg) Placement: Module DescriptionDocumento11 pagine12 Lead Electrocardiogram (Ecg) Placement: Module DescriptionHanna La MadridNessuna valutazione finora