Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Overview of The Treatment of Acute Lymphoblastic Leukemia in Children and Adolescents - UpToDate PDF
Caricato da
Isabella HosanaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Overview of The Treatment of Acute Lymphoblastic Leukemia in Children and Adolescents - UpToDate PDF
Caricato da
Isabella HosanaCopyright:
Formati disponibili
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
Official reprint from UpToDate
www.uptodate.com 2016 UpToDate
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents
Authors: Terzah M Horton, MD, PhD, C Philip Steuber, MD
Section Editor: Julie R Park, MD
Deputy Editor: Alan G Rosmarin, MD
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Oct 2016. | This topic last updated: Oct 13, 2016.
INTRODUCTION Acute leukemia is the most common form of cancer in children, comprising
approximately 30 percent of all childhood malignancies [1]. Of the acute leukemias, acute lymphoblastic
leukemia (ALL) occurs five times more commonly than acute myeloid leukemia (AML). Survival rates for
ALL have improved dramatically since the 1980s, with current five-year overall survival rates estimated at
greater than 85 percent [1-4]. Five-year event-free survival rates are >93 percent for low-risk groups [5].
This improvement in survival is due to treatment of a large number of children on sequential standardized
research protocols. Approximately 75 to 80 percent of children with newly diagnosed ALL participate in
such trials, the goals of which are to improve clinical outcomes while minimizing acute toxicities and lateoccurring adverse events.
The treatment of ALL in children is reviewed here. The epidemiology, presentation, classification, risk
group stratification, and outcome of childhood ALL are discussed separately. (See "Overview of the
presentation and diagnosis of acute lymphoblastic leukemia in children and adolescents" and "Risk group
stratification and prognosis for acute lymphoblastic leukemia in children and adolescents" and "Overview of
the outcome of acute lymphoblastic leukemia in children and adolescents".)
Although the majority of children with ALL will be cured, consultation with palliative care specialists may be
considered at the time of diagnosis as with any life-threatening condition or for pain management. (See
"Pediatric palliative care".)
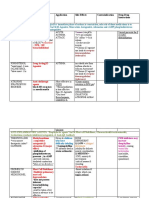
OVERVIEW OF TREATMENT Successful treatment of children with ALL involves administration of a
multidrug regimen that is divided into several phases (ie, induction, consolidation, and maintenance) and
includes therapy directed to the central nervous system (CNS). Most treatment protocols take two to three
years to complete, although the specific regimen varies depending upon immunophenotype and risk
category (table 1). (See "Risk group stratification and prognosis for acute lymphoblastic leukemia in
children and adolescents".)
At the time of diagnosis, patients with ALL commonly require transfusion support, treatment of suspected
or proven infections with broad-spectrum antibiotics, and, for patients with a high tumor burden, correction
of any metabolic imbalances such as hyperuricemia. A rare patient may require leukapheresis or exchange
transfusion to control extreme leukocytosis. (See "Red blood cell transfusion in infants and children:
Indications" and "Uric acid renal diseases", section on 'Acute uric acid nephropathy' and
"Hyperleukocytosis and leukostasis in hematologic malignancies".)
Despite improvements in supportive care, death resulting from treatment toxicity remains a challenge. In a
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
1/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
review of over 1000 children with ALL treated at St. Jude Children's Research Hospital, the estimated 10year cumulative incidence of treatment-related death was 2.9 percent [6]. Age was the only predictor of
death; children in the age bracket from one to nine years had a significantly lower risk of treatment-related
mortality than did either infants or older children. In a subsequent retrospective analysis of 8516 children
ages 0 to 19 years of age with newly-diagnosed ALL treated at US institutions, induction mortality was 1.12
percent [7]. Induction mortality was not associated with race or socio-economic status, but was increased
among children age <1 year (hazard ratio [HR] 3.34, 95% CI 1.22-9.13) and 10 to 19 years (HR 2.89, 95%
CI 1.55-5.41) and among those with cardio-respiratory or other organ failure (HR 145.4, 95% CI 37.8145.4).
INDUCTION THERAPY
Regimen Induction therapy is the initial phase of treatment. The primary goal of induction is
achievement of an initial complete remission (CR), defined as the eradication of all detectable leukemia
cells (less than 5 percent blasts) from the bone marrow and blood and the restoration of normal
hematopoiesis (>25 percent cellularity and normal peripheral blood counts). The induction therapy given
differs depending upon whether a t(9;22) translocation (Philadelphia chromosome) is present. While
t(9;22) translocation is uncommon in children, those with this translocation benefit from the addition of a
tyrosine kinase inhibitor that targets the aberrant expression of BCR-ABL.
t(9;22)/BCR-ABL1 negative ALL More than 90 percent of children and adolescents with ALL enter
complete remission (CR) at the end of induction therapy regardless of their initial risk grouping [8-17].
Induction therapy usually involves weekly administration of vincristine for three to four weeks, daily
corticosteroids (prednisone, prednisolone, or dexamethasone), and asparaginase. Asparaginase is
available as an E. coli derivative, either in its native form (L-asparaginase) or in its pegylated form
(Oncaspar) [18]. The pegylated form results in a longer period of asparagine depletion with comparable
toxicity [19]. L-asparaginase is no longer available for use in the United States. For patients with E. coli
asparaginase allergies, asparaginase is also available from Erwinia (Erwinase) [20]. A fourth agent such as
an anthracycline (eg, doxorubicin or daunorubicin) may be added to the three-drug regimen, particularly
for high-risk patients.
Response to therapy is often assessed by bone marrow examination during the induction phase of
treatment. In addition to morphologic response, bone marrow aspirates are also assessed for the presence
of minimal residual disease (MRD). Assessments can be performed by either quantitative polymerase chain
reaction (PCR) or by flow cytometry [21-23]. Both methods have shown that end-of induction and end-of
consolidation bone marrow MRD strongly correlate with survival [5,24,25]. (See "Clinical use of minimal
residual disease detection in acute lymphoblastic leukemia", section on 'MRD in children'.)
Early clearance of lymphoblasts from peripheral blood during the first week of therapy, clearance of blasts
from the bone marrow by the end of induction, and the presence or absence of MRD at the end of
induction therapy are important indicators of outcome. Patients who respond rapidly to the induction
regimen appear to have a more favorable outcome, whereas those who have a slow response or who fail
induction therapy have a more guarded prognosis [5,21-25]. This is discussed in more detail separately.
(See "Clinical use of minimal residual disease detection in acute lymphoblastic leukemia", section on 'MRD
in children'.)
t(9;22)/BCR-ABL1 positive ALL The t(9;22) translocation (Philadelphia chromosome) is a rare
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
2/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
mutation in children with ALL, with an incidence rate of <5 percent. Although the t(9;22)/BCR-ABL
translocation was formerly associated with a very poor prognosis, outcome has significantly improved with
the introduction of tyrosine kinase inhibitors (TKI), such as imatinib or dasatinib, to therapy regimens [2630]. In a prospective clinical trial from the Children's Oncology Group (COG), 91 children (age 1 to 21
years) with Philadelphia chromosome positive ALL were treated with intensive chemotherapy plus the TKI
imatinib [30]. Those treated from induction until the completion of therapy with imatinib had the best
outcome, with a five-year disease-free survival (DFS) of 70 percent. DFS was not statistically different
between patients treated with chemotherapy plus imatinib (7012 percent, n = 28) versus those who
underwent sibling donor hematopoietic cell transplant (HCT) (6511 percent, n = 21) or those receiving an
unrelated donor HCT (5915 percent, n = 13).
Patients with trisomy 21 Patients with trisomy 21/Down syndrome who develop ALL (DS-ALL) are
particularly susceptible to adverse events and treatment-related mortality. Intensive chemotherapy
regimens with high-dose methotrexate frequently result in severe mucositis, and children with DS-ALL have
an increased risk of severe infections [31]. An analysis of 653 children with DS-ALL demonstrated that
these patients have both a high rate of relapse (26 percent eight-year cumulative relapse incidence) and
an increased rate of two-year treatment-related mortality (7 versus 2 percent in non-DS-ALL) [32]. (See
"Overview of the outcome of acute lymphoblastic leukemia in children and adolescents", section on 'Down
syndrome'.)
Because of the increased incidence of infectious deaths in DS-ALL throughout all stages of chemotherapy
treatment (induction, consolidation, and maintenance) [33], patients are often treated on protocols with
reduced intensity chemotherapy, usually without evidence of inferior outcome [34]. In general, many
patients can be cured without the use of hematopoietic cell transplantation (HCT), which has been
associated with high treatment mortality.
Although cytogenetic changes other than trisomy 21 are uncommon with DS-ALL, those with concurrent
low-risk cytogenetics (ETV-RUNX1) comprise a risk group with an exceptionally good prognosis (eight-year
event-free survival 954 percent). This group, although uncommon, can be treated with less intense
chemotherapy [32]. Those with high-risk features can be successfully treated with reduced-intensity
conditioning followed by HCT. Outcomes, however, remain poor with three-year EFS of only 24 percent
[35].
Asparaginase inactivation and therapeutic drug monitoring Between 2 to 8 percent of patients
receiving E. coli asparaginase develop silent inactivation due to the production of neutralizing antiasparaginase antibodies [36,37]. Therapeutic drug monitoring of asparaginase activity can accurately
determine if a patient has neutralizing antibodies that are inactivating the target enzymatic activity of
asparaginase [37]. Those with neutralizing antibodies have asparaginase activity well below the therapeutic
threshold and can often be treated with Erwinia asparaginase as an effective alternative since there is only
approximately 10 percent antibody cross-reactivity between E. coli and Erwinia asparaginase preparations
[38]. (See "Infusion reactions to systemic chemotherapy", section on 'Formulations'.)
A retrospective study of 763 pediatric patients with ALL examined therapeutic drug monitoring and
suggested that lower doses of PEG-asparaginase can be used to maintain asparagine depletion [39];
these results will need to be confirmed in prospective clinical trials. It is currently unknown if decreasing the
asparaginase dose will result in fewer thrombotic or hemorrhagic complications. (See 'Thrombosis' below.)
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
3/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
Adverse effects Some children with ALL experience significant adverse effects during induction
chemotherapy. Toxicity can result from the chemotherapeutic agents or from the rapid elimination of a
large tumor burden (ie, tumor lysis syndrome). Life-threatening adverse effects of induction therapy
include tumor lysis syndrome, thrombosis, bleeding, and infection. Other acute side effects include
mucositis, pancreatitis, and hyperglycemia. Late effects of chemotherapy are discussed separately. (See
"Overview of the outcome of acute lymphoblastic leukemia in children and adolescents", section on 'Late
effects'.)
Tumor lysis syndrome Acute tumor lysis syndrome is the term applied to a group of metabolic
complications that may occur after the treatment of neoplastic disorders. The findings that may be seen
include hyperphosphatemia, hypocalcemia (caused by precipitation of calcium phosphate), hyperuricemia,
hyperkalemia, and acute renal failure. Rapid leukemic cell lysis after chemotherapy can cause overproduction and over-excretion of uric acid. The precipitation of uric acid in the tubules can lead to oliguric
or anuric renal failure known as uric acid nephropathy [40]. (See "Tumor lysis syndrome: Definition,
pathogenesis, clinical manifestations, etiology and risk factors" and "Acute kidney injury in children: Clinical
features, etiology, evaluation, and diagnosis".)
In a study of 328 children with ALL, the following four factors were identified as independent predictors of
tumor lysis syndrome on multivariate analysis [41]:
Age >10 years
Splenomegaly
Mediastinal mass
Initial white blood cell count >20,000/microL
Absence of all four of these risk factors indicated a low risk for development of tumor lysis syndrome, with a
negative predictive value of 98 percent and a sensitivity of 96 percent.
Prophylactic regimens to prevent acute uric acid nephropathy in children with ALL include the
administration of medications to reduce the production of uric acid (allopurinol or rasburicase, a
recombinant uricase that catalyzes oxidation of uric acid to the much more soluble compound allantoin),
and aggressive intravenous hydration [42]. Hemodialysis may be necessary to remove excess circulating
uric acid and phosphate in patients who develop acute renal failure and in whom adequate diuresis cannot
be achieved. These issues are discussed in detail separately. (See "Tumor lysis syndrome: Prevention and
treatment", section on 'Clinical impact of TLS'.)
Adverse effects of rasburicase include allergic reactions, including anaphylaxis, hemolysis, hemoglobinuria,
methemoglobinemia, and interference with uric acid measurements [43]. This agent is contraindicated in
patients with glucose-6-phosphate dehydrogenase deficiency because it can cause severe hemolysis [43].
Thrombosis Thrombotic events, including intracranial dural sinus thrombosis with hemorrhage, deep
vein thrombosis, and pulmonary embolism, have been reported with induction chemotherapy regimens for
ALL that include all forms of asparaginase [44]. Thrombosis is a major complication that may be lifethreatening and impact future therapy. In contemporary treatment protocols, the incidence of thrombotic
complications among children with ALL receiving asparaginase has varied among studies from as low as
1.8 percent to as high as 15 percent in children with prothrombotic risk factors [45]. Increased risk of
thrombosis occurs with increased age and the presence of a central venous catheter [46,47].
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
4/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
In a prospective trial of children and adolescents with ALL, thrombosis occurred in 63 of 1038 (6 percent)
and was most common among those age 15 years and older (21 percent) [47]. Most thromboses were in
the setting of asparaginase administration. Nine children died within 30 days of thrombosis with four deaths
directly attributable to the thrombosis. In addition, approximately half of patients alive after thrombosis had
delays or dose modifications of further asparaginase therapy.
A 2006 meta-analysis of 1752 children with ALL reported that 5.2 percent of patients developed a
thrombosis at some time during treatment (ie, from the start of induction through the end of maintenance)
[48]. Most (83 percent) of these events occurred during induction therapy. The following four risk factors
for thrombosis were identified in this population:
Treatment with asparaginase
Concomitant use of steroids
Thrombophilic genetic abnormalities
Presence of central venous lines
In a European study, these risk factors were used to develop a predictive model for identifying children with
ALL at the highest risk of thrombosis during induction with asparaginase-based therapy [49]. While the
2006 meta-analysis did not evaluate the impact of ABO blood group on the risk of thrombosis, a
subsequent large retrospective analysis reported an association between non-O blood group and age and
an increased risk of thrombosis [50]. Non-O blood type is a known risk factor for VTE in adults. (See
"Overview of the causes of venous thrombosis", section on 'Non-O blood type'.)
A retrospective analysis of 336 consecutively recruited children with ALL treated on different BerlinFrankfurt-Munster (BFM) study protocols found a lower incidence of thromboembolism when asparaginase
was used in conjunction with dexamethasone rather than prednisone (1.8 versus 10.4 percent) [51]. The
results of this study, limited by the small number of patients (n = 56) in the dexamethasone treatment
group, bear further scrutiny in prospective trials with larger numbers of patients.
Asparaginase depletes plasma asparagine, thereby inhibiting protein synthesis in leukemic cells and the
synthesis of several plasma proteins. The latter effect causes deficiencies of albumin, thyroxine-binding
globulin, and various coagulation proteins, including prothrombin, factors V, VII, VIII, IX, X, XI, fibrinogen,
antithrombin, protein C, protein S, and plasminogen [52,53]. These deficiencies result in prolongation of
the prothrombin time, activated partial thromboplastin time (aPTT), thrombin time, and hypofibrinogenemia,
with fibrinogen levels often less than 100 mg/dL. E. coli-asparaginase and Erwinia-asparaginase appear to
have equivalent risk of severe thrombosis, including central nervous system hemorrhage. (See "Druginduced thrombosis in patients with malignancy", section on 'L-asparaginase' and "Antithrombin
deficiency", section on 'Patients receiving asparaginase'.)
Bleeding Hemorrhage in children with ALL usually is caused by thrombocytopenia. Patients who
have platelet counts <10,000/microL are at greatest risk. Children with thrombocytopenia typically have
bleeding from the skin or mucus membranes; significant visceral bleeding is unusual. Intracranial
hemorrhages are rare but life-threatening events. Treatment or prevention of such bleeding is provided by
transfusion of platelets. (See "Clinical and laboratory aspects of platelet transfusion therapy", section on
'Leukemia and chemotherapy'.)
Patients who require prolonged antibiotic therapy may develop bleeding secondary to a vitamin-K
dependent coagulopathy. Patients with an elevated prothrombin time (PT) are treated with oral or
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
5/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
intravenous vitamin K (2.5 to 5.0 mg PO per day; or if bleeding, 1 to 2 mg IV as a single dose). (See "Betalactam antibiotics: Mechanisms of action and resistance and adverse effects", section on 'Hematologic
reactions'.)
Infection Children with newly diagnosed ALL are functionally neutropenic and lymphopenic at the
time of diagnosis and may develop further myelosuppression following chemotherapy. These children are
more susceptible to development of systemic bacterial, fungal, and viral infections (eg, varicella-zoster,
herpes simplex virus). Infections account for the majority of treatment-related mortality in this population.
As an example, in a retrospective review of 425 children who received induction therapy for ALL at a single
tertiary Canadian center, 20 percent of all patients experienced at least one documented infection [54].
Neutropenia was almost twice as common in those who developed infections compared with those without
infection. Patients with pre-existing conditions (ie, Down syndrome, congenital heart disease, pre-existing
immunodeficiency syndromes) were at highest risk of infections. The 85 infections included 65 bacterial, 15
viral, and 5 fungal infections. Infectious mortality was minimal (3 out of 425, or 1 percent) and included
deaths from both fungal (Candida albicans) and bacterial (Bacillus cereus) infections.
Details regarding infection-related deaths are also available from the prospective UKALL 2003 trial, which
reported 75 septic deaths among 3126 children (2.4 percent) with newly diagnosed ALL, accounting for 64
percent of treatment-related mortality [33]:
Although infection-related mortality was most common during induction therapy (48 percent), it also
occurred during consolidation (9 percent), delayed intensification (23 percent), and maintenance
therapy (20 percent). Underlying Down syndrome was associated with a significantly increased risk of
death due to sepsis (odds ratio 12) during all treatment periods. (See 'Patients with trisomy 21'
above.)
Most deaths occurred in neutropenic patients and within 48 hours of presentation with sepsis.
Most septic deaths with an identified pathogen were due to bacteria (68 percent), with fungal (20
percent) and viral (12 percent) pathogens being less common. The most commonly identified bacteria
were Pseudomonas, E. coli, and Enterococcus.
Because these infections are potentially life-threatening in any phase of therapy, fever in children who are
receiving chemotherapy must be evaluated and aggressively treated. The use of prophylactic antimicrobial
therapy is recommended, but the specific therapy varies by circumstance and institution. For example, the
use of an antimicrobial (sulfamethoxazole-trimethoprim, dapsone, or pentamidine) Pneumocystis
pneumonia prophylaxis is almost universal in the management of patients receiving chemotherapy, while
the administration of antifungals and antiviral agents is more individualized. (See "Fever in children with
chemotherapy-induced neutropenia".)
The role of colony-stimulating factors (granulocyte colony-stimulating factor and granulocyte macrophage
colony-stimulating factor) to prevent or manage infectious complications during ALL induction has not been
well studied. In one randomized, crossover study in 287 children with high-risk ALL, prophylactic use of
granulocyte colony-stimulating factor shortened periods of neutropenia, but did not reduce rates of febrile
neutropenia, serious infections, or the need for hospitalization; overall survival at six years was not affected
[55]. A systematic review has come to similar conclusions [56].
Neuropathy Virtually all patients receiving vincristine have some degree of neuropathy and
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
6/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
approximately 25 to 30 percent of children treated for ALL will develop clinically significant peripheral
neuropathy requiring dose reduction or treatment discontinuation. The rate may be significantly higher in
patients with a genetic predisposition (eg, single nucleotide polymorphism in the promoter region of
CEP72) [57]. The neuropathy involves both sensory and motor fibers and can manifest as paresthesias,
loss of reflexes, weakness, and autonomic neuropathies, including vocal cord paralysis. Patients with mild
neuropathy can usually continue to receive full doses of vincristine, but when symptoms increase in
severity and interfere with activities of daily living, dose reduction or discontinuation of the drug may be
necessary. Vincristine neuropathy is usually reversible but improvement is gradual and may take up to
several months. This is described in more detail separately. (See "Overview of neurologic complications of
non-platinum cancer chemotherapy", section on 'Vincristine'.)
Anaphylaxis Some chemotherapy and supportive medications, such as asparaginase, the
epipodophyllotoxins (etoposide and etopophosphamide), and uricase, can cause significant allergic
reactions, including anaphylaxis. Medications used to treat anaphylaxis should be readily available when
these drugs are administered. Anaphylactic reactions to PEG-asparaginase can be delayed by several
hours. Because of this delay, a period of observation following administration of PEG-asparaginase has
become common practice at many institutions. (See "Infusion reactions to systemic chemotherapy", section
on 'L-asparaginase'.)
HPA axis suppression The administration of daily corticosteroids during induction therapy results in
suppression of the hypothalamic-pituitary-adrenal (HPA) axis in most patients [58]. A study of 64 patients
showed that over 80 percent of children had significant suppression of cortisol release by
adrenocorticotropic hormone (ACTH) stimulation [59]. In this study, all patients had recovered normal
adrenal function by 10 weeks following induction chemotherapy. Because nearly all patients experienced
adrenal insufficiency during the first days after cessation of glucocorticoid treatment, it is recommended
that children with infections, trauma, or surgery occurring during or shortly after induction be treated with
glucocorticoid replacement. While the majority recovers HPA axis function within a few weeks after
corticosteroid cessation [59], HPA axis suppression lasted up to 34 weeks in one analysis [60]. For this
reason, glucocorticoid replacement following trauma, infection, or surgery should be considered on a caseby-case basis for children with ALL following induction. (See "Glucocorticoid withdrawal", section on
'Hypothalamic-pituitary-adrenal axis suppression' and "Diagnosis of adrenal insufficiency in children".)
Induction failure Induction failure, which occurs in fewer than 5 percent of cases, is defined by the
persistence of leukemic blasts in the blood, bone marrow, or any extramedullary site after four to six weeks
of induction therapy. Induction failure has historically been considered a particularly ominous sign and an
indication for allogeneic HCT [61]. Due to the rarity of induction failure, information regarding this
population has been limited to small numbers of patients enrolled on prospective clinical trials [62-64].
An international retrospective analysis from 14 cooperative study groups identified 44,017 children (18
years) with previously untreated ALL diagnosed from 1985 to 2000 [65], of which 1041 (2.4 percent) had
induction failure. In this cohort, patients with induction failure were more likely to have had at least one of
the following unfavorable features at presentation: male sex, older age (>6 years), high leukocyte count
(>100,000 cells/microL), T cell leukemia, central nervous system (CNS) involvement, or the 11q23 (MLL)
chromosomal rearrangement. These same unfavorable features, except for male sex and CNS
involvement, were also associated with reduced survival after induction failure. At a median follow-up of 8.3
years, the estimated overall survival (OS) at 10 years for patients with induction failure who did not
demonstrate t(9;22)(BCR-ABL1) was 32 percent. For the 624 patients with genetic data available, patients
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
7/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
could be stratified by karyotype with the following estimated 10-year OS:
High hyperdiploid cytogenetics (n = 55) 72 percent
Normal karyotype (n = 159) 36 percent
Other chromosomal aberration (n = 250) 30 percent
11q23/MLL abnormality (n = 50) 16 percent
These data highlight the heterogeneity of the induction-failure population and the need for individualized
treatment decisions. Although the estimated OS rate was similar among the 198 patients who underwent
HCT (43 percent) and the 427 patients who received chemotherapy alone (41 percent), the effect of HCT
on survival appeared to differ greatly according to karyotype risk subgroup. As an example, children
younger than six years with precursor B cell ALL without MLL rearrangement (ie, low-risk factors) appeared
to have higher survival rates when treated with chemotherapy alone rather than HCT (73 versus 59
percent). In contrast, older children and those with elevated white blood cells (WBC), T cell ALL, and
additional cytogenetic risk factors had higher survival rates with a matched related donor HCT rather than
chemotherapy alone (59 versus 35 percent). A similar study in Europe showed that adolescents and young
adults with T cell ALL also did better with allogeneic HCT compared with chemotherapy alone (67 versus
42 percent) [66].
A subset analysis of induction failures in a large prospective clinical trial suggested that overall survival for
patients with induction failure had improved somewhat with aggressive chemotherapy, with a four-year
overall survival of 60 percent [67].
In another study of 774 children with ALL (including T cell ALL) from the United States, 23 had persistent
leukemia after completion of induction therapy and were treated with additional induction chemotherapy.
Although 21 patients eventually achieved complete remission, their five-year event-free survival (EFS) was
only 16 percent (95% CI 0-31 percent) regardless of management regimen, compared with 82 percent
(95% CI 79-86 percent) in the group that achieved remission within one month and 79 percent (95% CI 7087 percent) in those who had protracted hypoplasia [63].
In a French study of 1395 children with ALL, a multivariate analysis identified three groups based upon
their risk for induction failure [64]. The intermediate- and high-risk groups had a 7- and 28-fold increase
risk of induction failure compared with the low-risk group. The low-risk group (n = 1080) had precursor B
cell ALL without the "Philadelphia" translocation, t(9;22). The intermediate-risk group had T cell ALL with
mediastinal involvement and the high-risk group had either the "Philadelphia" translocation or T cell ALL
without mediastinal involvement. The groups were treated based upon Berlin-Frankfurt-Munster study
(BFM) protocols. Overall, 53 patients failed induction therapy. With salvage therapy, 43 patients entered
complete remission, 39 after one second-line course of chemotherapy and four who required more than
one course. Both the overall survival rate and the EFS for the 53 patients who failed induction therapy
compared with those who responded to therapy were markedly lower (30 and 27 percent versus 85 and 75
percent, respectively).
A subset of patients with Philadelphia chromosome negative (BCR/ABL1 negative) ALL have a gene
expression signature profile similar to that seen with BCR/ABL1 positive disease. This "BCR/ABL1-like B
cell ALL" is clinically more aggressive than other BCR/ABL1 negative ALL and resistant to standard
chemotherapy. Detailed genomic analysis identified alternative mechanisms of activated kinase signalling
in the majority of BCR/ABL1-like B cell ALL that may be targeted with novel agents in the future. (See
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
8/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
"Cytogenetics and molecular genetics in acute lymphoblastic leukemia", section on 'BCR/ABL1-like B cell
ALL'.)
CNS PREVENTIVE THERAPY Leukemic involvement of the central nervous system (CNS) at the time of
diagnosis is an uncommon finding, occurring in fewer than 5 percent of patients [68,69]. However, before
the use of preventive CNS therapy, up to 80 percent of children with ALL who were in complete bone
marrow remission relapsed with "leukemic meningitis" [70].
The routine use of preventive CNS therapy is a major therapeutic advance in the treatment of childhood
ALL. CNS treatment usually begins during the induction phase and continues throughout the remainder of
the treatment regimen. Craniospinal radiotherapy has been replaced by intrathecal chemotherapy in
several CNS preventive therapy protocols. Current protocols contain either no CNS radiotherapy, or have
a significantly reduced dose of 12 to 18 Gy. Outcome data from these protocols have demonstrated that
replacement of craniospinal radiotherapy with frequent administrations of intrathecal therapy does not
compromise event-free or overall survival [4,71-77].
Craniospinal radiotherapy or cranial radiotherapy, once considered the standard of care, was effective in
preventing CNS leukemia but was associated with significant toxicity, such as cognitive impairment and
decreases in white matter volume [78,79]. Approximately 50 percent of children treated with 24 Gy
craniospinal radiation developed CNS changes detected by magnetic resonance imaging (MRI) (atrophy,
leukoencephalopathy, calcifications, or grey matter abnormalities), secondary brain tumors, and had
decreased performance on neuropsychological testing [80,81]. As an example, a cancer survivorship study
of 102 adult survivors of ALL who received radiotherapy suggested that there is a progressive decline in
attention and verbal functioning that persists into adulthood [82]. The long-term toxicities of cranial
radiation are discussed in more detail separately. (See "Overview of the outcome of acute lymphoblastic
leukemia in children and adolescents", section on 'CNS and cognition' and "Overview of the outcome of
acute lymphoblastic leukemia in children and adolescents" and "Delayed complications of cranial
irradiation".)
The efficacy of intrathecal prophylaxis was illustrated in a randomized trial from the Dana-Farber Cancer
Institute ALL Consortium, in which children with standard-risk ALL were assigned to receive either intensive
triple intrathecal chemotherapy (cytarabine/methotrexate/hydrocortisone) or 1800 cGy cranial radiation
with less frequent intrathecal therapy [71]. There was no difference between the two groups in five-year
event-free survival (EFS) (83 versus 86 percent) or the rate of CNS relapse (6 percent in each group). A
subsequent analysis of the neuropsychological outcomes found that cognitive function was in the average
range in both groups [72]. However, children who received 18 Gy or more of cranial radiotherapy had less
fluent language output and were less effective at modulating their behavior according to their parents.
A subsequent study evaluated the efficacy of regimens without cranial irradiation in 498 consecutive
children (age range 1 to 18 years) with ALL who were treated with triple intrathecal therapy and intensified
systemic chemotherapy based upon disease risk stratification after remission induction [4]. Intrathecal
cytarabine was initially administered on day 1 of remission induction and followed by subsequent triple
intrathecal chemotherapy (cytarabine/methotrexate/hydrocortisone). The number of intrathecal treatments
ranged from 13 to 25 and was based upon disease risk stratification and patient characteristics, including
CNS status of disease.
The following findings were noted:
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&search
9/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
The five-year event-free and overall survival rates were 86 and 94 percent, respectively.
The five-year cumulative risk was 3.9 percent for any CNS relapse (isolated, and combined CNS and
hematologic relapse) and 2.7 percent for isolated CNS relapse.
The five-year remission rate was significantly higher in the 71 patients who would have previously
received prophylactic cranial irradiation than 56 historical controls who received cranial irradiation (91
versus 73 percent).
A similar study of 156 children from Taiwan indicated that triple intrathecal therapy could be used to
replace radiotherapy, suggesting that replacement of radiotherapy with more intense intrathecal therapy
can be generalized to a wide variety of ALL protocols [76].
The results of these studies demonstrate that intrathecal therapy provides similar event-free and overall
survival in a cohort of children with ALL. However, all recommendations for CNS preventive therapies
should be evaluated in the context of the related systemic therapy regimens and should not be applied to
other treatments without more evidence. Some current protocols continue to incorporate lower dose cranial
radiation (<1800 cGy) for patients where CNS leukemia is felt to be a significant risk factor.
Although the incidence of neurotoxicity is reduced by intrathecal therapy, it is not eliminated and remains a
significant risk. Intrathecal chemotherapy (with either methotrexate alone, or methotrexate combined with
cytarabine and prednisone) is associated with acute neurotoxicity [83], including seizures and
leukoencephalopathy [83].
There is also an increasing body of evidence that CNS-directed therapy can impact attention and cognitive
function. These effects appear to be more significant in girls and children who are radiated at a younger
age. Because of the impact of these changes on functioning into adulthood, broad strategies for
educational and pharmacologic interventions have been developed to remediate established cognitive
dysfunction following childhood ALL [84].
POST-REMISSION THERAPY Consolidation or intensification therapy is the second phase of ALL
treatment and is initiated soon after attainment of complete remission (CR). Ongoing treatment is required
because small numbers of leukemic lymphoblasts remain in the bone marrow despite histologic and
molecular evidence of CR after induction therapy. In such cases, relapse occurs quickly if therapy is not
continued. The goal of post-induction chemotherapy is to prevent leukemic regrowth, reduce residual
tumor burden, and prevent the emergence of drug-resistance in the remaining leukemic cells.
There is evidence that leukemias undergo a process known as clonal evolution [85]. During induction, the
vast numbers of leukemia cells originating from the dominant subclone are eliminated. However, leukemiainitiating cells are often from a heterogeneous population at diagnosis, with individual patients having
multiple genetic subclones with leukemia-initiating potential [86]. These subclones are present within a
complex clonal architecture at diagnosis, and often potentially chemoresistant leukemia-initiation cells are
present but are undetectable by minimal residual disease (MRD) assays. Post-induction therapies can help
prevent the emergence of a drug resistance by eliminating these subdominant clones that were resistant to
induction therapy. (See "Detection of minimal residual disease in acute lymphoblastic leukemia" and
"Clinical use of minimal residual disease detection in acute lymphoblastic leukemia".)
Consolidation Consolidation therapy usually lasts from four to eight months. It commonly involves the
use of several different drug combinations and drugs with mechanisms of action that differ from those used
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
10/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
during the induction phase. Regimens often include the following drugs administered according to a variety
of schedules to maximize drug synergy and minimize the development of drug resistance [87,88]:
Cytarabine
Methotrexate
Anthracyclines (daunorubicin, doxorubicin)
Alkylating agents (cyclophosphamide, ifosfamide)
Epipodophyllotoxins (etoposide, etopophosphamide)
Intensification of therapeutic regimens is based upon the patient's risk group classification [89]. This has
allowed a reduction of intensification therapy for patients with good prognosis while providing more
intensive treatment for those in the high-risk groups. End of induction MRD, as well as cytogenetics and
molecular abnormalities, are the most important predictors of disease-free and overall survival [5,23,90].
Patients with detectable MRD have an increased risk of relapse following conventional chemotherapy.
Ongoing trials are evaluating the escalation of consolidation therapy intensity for patients who are MRD
positive following induction, and the reduction of therapy intensity in MRD negative cases. As an example,
in one trial (UKALL 2003), 533 patients clinically identified as having standard-risk or intermediate-risk ALL
at diagnosis and MRD positivity (leukemia cells >0.01 percent) in the bone marrow at the end of induction
therapy were randomly assigned to receive either standard or augmented post-remission therapy [91]. The
augmented therapy included additional doses of asparaginase, vincristine, and methotrexate. Augmented
therapy was associated with more adverse events including hypersensitivity, pancreatitis, and
mucositis/stomatitis. After a median follow-up of 70 months, augmented therapy resulted in superior fiveyear event-free survival (90 versus 83 percent; p = 0.04). However, overall survival was not statistically
different between the standard and augmented therapy groups (93 versus 89 percent, p = 0.16). Similar
strategies of therapy intensification for patients that are MRD positive after induction are underway in
Europe and the United States. (See "Clinical use of minimal residual disease detection in acute
lymphoblastic leukemia", section on 'MRD in children' and "Risk group stratification and prognosis for acute
lymphoblastic leukemia in children and adolescents", section on 'Minimal residual disease'.)
Delayed intensification Improved survival also has been gained with the addition of more intensive
therapy following consolidation, an approach known as delayed intensification [92-94]. Delayed
intensification involves the administration of a five- to eight-week "pulse" of intensive, multi-agent
chemotherapy similar to that administered during induction and consolidation. Delayed intensification
pulses were given either once [92,93] or twice [95,96] during the first six months of post-remission therapy.
Although the benefit of two pulses of delayed intensification has not been demonstrated [5,97], the addition
of a single delayed intensification pulse has improved survival for both standard and high-risk patients
[96,98].
The intensity of delayed intensification therapy is commensurate with the patient's risk grouping. As a
general rule, the higher the risk for treatment failure, the more aggressive intensification therapy is
required. This was demonstrated in a Children's Oncology Group trial of 1299 patients with higher risk ALL
that had rapid marrow response to induction therapy [99]. This study demonstrated that a more intensive
delayed intensification regimen resulted in improved event-free survival and overall survival at five years
compared with either standard therapy or longer duration of therapy.
During the delayed intensification phase of chemotherapy, most patients still have significant
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
11/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
myelosuppression and immunosuppression. They remain at risk for bacterial, viral, and fungal infections
during periods of neutropenia, and fevers should be aggressively treated. Patients can also experience
many of the same complications (eg, infection) seen during induction therapy, although these are usually
less common. (See 'Adverse effects' above.)
More aggressive treatment regimens involving multiple chemotherapeutic agents place high-risk patients at
risk for additional complications. High-risk ALL patients have an increased risk of secondary cancers
(associated with epipodophyllotoxins or radiation) and decreased fertility (a risk for adolescents receiving
alkylating agents). (See "Overview of the outcome of acute lymphoblastic leukemia in children and
adolescents", section on 'Late effects'.)
Allogeneic hematopoietic cell transplantation Selected patients with high-risk disease have an
increased incidence of relapse during delayed intensification chemotherapy [66,100,101]. This includes
patients with severe hypodiploid ALL (less than 46 chromosomes), those with MLL rearrangements, and
infants with ALL. With the exception of patients <1 year of age, patients with these cytogenetic and
molecular abnormalities are candidates for allogeneic hematopoietic cell transplantation (HCT) during first
remission. There is evidence that HCT offers a survival advantage to those >10 years of age with severe
hypodiploidy (and without Li-Fraumeni syndrome), high-risk T cell ALL [99], induction failure, and patients
>1 year of age with 11q23 rearrangements [65,66].
An HLA-matched sibling donor is usually preferred and evidence shows that transplants with an HLAmatched sibling donor are associated with fewer severe infections and pulmonary complications [102]. A
matched unrelated donor, however, is an acceptable alternative when a sibling donor is not available and
appears to result in similar clinical outcomes (event-free survival, overall survival, non-relapse mortality,
and relapse rates) [102]. A partially matched family member donor or umbilical cord blood is a reasonable
option for patients who do not have an HLA-identical matched donor. (See "Donor selection for
hematopoietic cell transplantation".)
In contrast, HCT has been associated with increased mortality in infants [103]. There is some evidence that
HCT has been more successful in infants using reduced intensity conditioning [104]. Further study is
needed to determine if HCT can improve outcomes in infants, particularly for those infants with MLL
rearrangements. [65,66,99]
MAINTENANCE THERAPY The overall treatment duration for most children with ALL is 30 to 42 months.
After completion of the consolidation or intensification phase of therapy, patients often receive a less
intensive continuation regimen (eg, maintenance chemotherapy) using daily oral 6-mercaptopurine (6-MP)
[105], weekly methotrexate with periodic vincristine, prednisone, and intrathecal therapy. 6-MP can be
administered as a tablet or as an oral suspension; although not yet the standard of care, the oral
suspension may allow for more accurate dosing in children [106]. Children and families must be educated
regarding the importance of maintenance therapy. The importance of compliance with 6-MP was illustrated
in a cohort study that demonstrated an association between decreased adherence rates and an increased
risk of relapse [107].
Although it is unclear whether all patients with ALL benefit from maintenance therapy that includes a
combination of pulse therapy vincristine and steroids in addition to a daily regimen of 6-MP and weekly
methotrexate, patients with standard-risk ALL who receive this combination appear to have a more
favorable long-term outcome than those treated with only 6-MP and methotrexate [108]. The optimal time
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
12/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
interval for vincristine plus steroid pulses is also unclear; this question is currently being studied in a large
prospective COG trial. Patients with high-risk ALL, such as infants with ALL, may require a more
aggressive continuation regimen with additional drug combinations.
During maintenance therapy, patients remain at risk for infection. Fever in children who are receiving
chemotherapy must be evaluated and treated aggressively, especially if the patient is either neutropenic or
has a central venous access device. Trimethoprim-sulfamethoxazole, dapsone, pentamidine, or
atovaquone prophylaxis is continued to prevent Pneumocystis pneumonia [109,110]. Therapy to prevent
Pneumocystis infection should be given during therapy and for at least three to six months following the
completion of treatment. Children and their household contacts should not be given live-virus
immunizations while the patient is receiving chemotherapy. (See 'Immunizations' below.)
PRIMARY CARE CONSIDERATIONS For practical reasons, most patients with ALL remain under the
primary care of their oncologists during the induction and consolidation portions of their chemotherapy.
Once a patient enters the less intensive maintenance therapy, however, the primary care provider (PCP)
can often provide routine medical care with scheduled visits to the oncologist for chemotherapy,
particularly if the family lives some distance from the oncology treatment center. When ALL therapy is
complete, the PCP resumes primary care for the patient, including visits for health maintenance and acute
illnesses.
During chemotherapy, the oncologist usually coordinates physical examinations, procedures, and imaging
studies. The PCP, however, plays an important role in encouraging patients to return to their oncologist for
scheduled visits and follow-up studies. Encouragement to maintain regularly scheduled follow-up visits with
their oncologist is particularly important after the completion of chemotherapy treatment. Communication
between the PCP and the oncologist is critical throughout the treatment process.
The purpose of frequent follow-up visits after the cessation of chemotherapy is to examine ALL survivors
for disease recurrence and to screen them for the long-term side effects. Patients are closely followed for
several years after completion of chemotherapy. Although there is no standard follow-up frequency,
patients are typically seen by their oncologist monthly for the first year after therapy completion and then at
less frequent intervals for the next two to four years. After three to five years, patients are followed on an
annual basis with a focus on long-term survivor issues. (See "Overview of the outcome of acute
lymphoblastic leukemia in children and adolescents", section on 'Late effects'.)
Immunizations Experience with vaccine administration in children undergoing cancer treatment is
limited and there are few published data regarding response to specific vaccines in patients receiving
immunosuppressive chemotherapy. Data from HIV-infected infants indicate that the risk of adverse events
after immunization is low [111].
Patients with ALL should receive only inactive immunizations during chemotherapy [111]. Live-virus
vaccines, such as MMR and oral poliovirus, are contraindicated. After completion of chemotherapy, the
patient should receive any missed vaccinations, including MMR and varicella.
Cancer patients have a variable response to the immunizations received while immunosuppressed. In
addition, children with ALL whose immunizations were up-to-date at the time of diagnosis may fail to
maintain protective antibody titers after completion of chemotherapy [112,113]. For this reason, it is
recommended that antibody titers be checked three to six months after the completion of chemotherapy,
and that children be revaccinated if they have low antibody titers [111,114]. (See "Immunizations in patients
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
13/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
with cancer".)
Patients whose therapy included hematopoietic cell transplantation often repeat their immunization series
beginning approximately one year after transplantation. Testing of immune function may provide evidence
for safe immunization timing in these patients [111]. (See "Immunizations in hematopoietic cell transplant
candidates and recipients".)
Varicella vaccine Given the variability of chemotherapy regimens and the current decreasing
incidence of varicella, the American Academy of Pediatrics does not recommend routine varicella
vaccination for children actively receiving chemotherapy. If varicella vaccination is performed in a child in
remission without evidence of immunity, it should be undertaken with expert guidance and with the
availability of antiviral therapy should complications occur [115]. After the completion of therapy, varicella
titers should be checked and, in the absence the varicella titers, the varicella vaccine should be
readministered.
Influenza vaccine The annual influenza vaccine is recommended for children with ALL receiving
chemotherapy. It is also recommended that household contacts receive the flu vaccine to prevent patient
exposure during periods of neutropenia when the patient is severely immunocompromised. Family
members should not receive the nasal vaccine due to concerns that this live virus could spread to the child
with leukemia and result in severe systemic disease in the immunocompromised host.
Monitoring for relapse The signs and symptoms of ALL relapse typically are similar to those of initial
presentation. They include fever, malaise, bleeding, and bone pain. (See "Overview of the presentation
and diagnosis of acute lymphoblastic leukemia in children and adolescents".)
ALL relapse most commonly occurs in the bone marrow and usually presents with persistent peripheral
blood cytopenias. Healthcare providers should pay close attention to persistent abnormal blood counts in
the ALL survivor. Monitoring for the presence of minimal residual disease (MRD) is also common practice
in patients who have had a stem cell transplant as part of their treatment regimen. Prompt referral for bone
marrow examination is warranted if there is suppression of more than one cell line (white cells, red cells,
platelets) or unexplained suppression of one cell line that persists for longer than three to four weeks.
Prompt bone marrow examination is also warranted for patients with a history of a stem cell transplant that
have persistently positive MRD or recurrence of the cytogenetic abnormality associated with their initial
leukemia clone [116].
The second most common site of ALL relapse is the central nervous system (CNS). However, the
frequency of CNS relapse has diminished with the advent of initial prophylactic intrathecal therapy. CNS
relapse may manifest with symptoms of increased intracranial pressure (headache, morning vomiting),
nuchal rigidity, focal neurologic findings (particularly cranial nerve palsies), or papilledema.
Testicular relapse is uncommon (<5 percent) with current treatment regimens. Testicular relapse often
presents as unilateral, painless testicular enlargement [117]. Diagnosis is made by testicular biopsy.
Bilateral biopsies are indicated if testicular relapse is suspected, since leukemic cells are frequently found
in the contralateral testis [117]. Leukemic infiltrates rarely recur in other extramedullary sites, including the
ovary, kidney, skin, and eye.
RELAPSED DISEASE
Management Approximately 10 to 15 percent of children with ALL fail initial treatment. Relapse rates
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
14/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
are substantially higher (25 to 30 percent) in certain high-risk subgroups, such as adolescents with T cell
ALL or central nervous system (CNS) disease. Risk factors for relapsed ALL include age (<1 year or >10
years), initial CNS disease, slow clearance of disease, and molecular/cytogenetics alterations associated
with the emergence of chemoresistant leukemia subclones [118]. For patients over 10 years of age, there
is a near-linear relationship between age and risk of relapse, particularly in patients with pre-B cell ALL
[118]. Certain molecular alterations, including MLL rearrangements, CRLF2 overexpression [119], and
those with an intrachromosomal amplification (iAMP) [120] are at higher risk of relapse. Some of these
high-risk groups, such as those with CNS disease and iAMP mutations, do well if treated with more intense
initial chemotherapy [121,122]. Others, particularly those with early bone marrow relapse, IKZF1 mutations,
and MLL rearrangements, do better with allogeneic hematopoietic cell transplantation (HCT) once in
second remission [123].
The outcome for patients with relapsed ALL is guarded when compared with those without recurrence.
Relapse following ALL therapy remains the second most common cause of cancer-related death in
children. The vast majority of relapses occur within 2.5 years from diagnosis. For patients with T cell ALL,
recurrences more than 2.5 years from diagnosis may represent a second leukemia rather than a relapse of
the original leukemia. Late relapses in children with pre-B ALL, however, appear to represent clonal
evolution of the original disease [124].
Patients with relapsed ALL require aggressive reinduction therapy and intensification, often using agents
not administered in the original treatment protocol [125]. Patients with high-risk ALL, such as those over 10
years of age or those with high initial WBC counts, often do not respond well to treatment with additional
chemotherapy alone [126,127]. Patients who have CNS or testicular relapse require radiation therapy at
some point during the rescue therapy program [128].
The following novel agents have been used for the treatment of relapsed ALL (see "Treatment of relapsed
or refractory acute lymphoblastic leukemia in adults", section on 'Remission induction'):
Nelarabine, a prodrug converted in vivo to ara-GTP, has shown efficacy as a single agent for the
treatment of relapsed or resistant T cell ALL in children and adults. It is also being studied in newly
diagnosed T cell ALL. A trial by the Childrens Oncology Group (COG) has recently been completed
and analysis is ongoing. (See "Treatment of relapsed or refractory acute lymphoblastic leukemia in
adults", section on 'Nelarabine for T cell ALL'.)
Clofarabine is a nucleoside analogue structurally related to both fludarabine and cladribine.
Clofarabine disrupts nucleotide metabolism by inhibiting nucleoside incorporation into DNA, preventing
nucleotide pool recycling by inhibiting the enzyme ribonucleotide reductase, and disrupting
mitochondrial integrity, which results in the release of mitochondrial proteins that trigger apoptosis.
Clofarabine can be seen as a potential "bridge to transplant" since half of the responding relapsed
acute myeloid leukemia (AML) and ALL patients were able to receive a subsequent HCT [129].
Clofarabine has been combined with other cytotoxic chemotherapy including etoposide and
cyclophosphamide [130] as well as cytarabine [131]. Although effective, clofarabine in combination
with other chemotherapies has resulted in a high rate of infections and other adverse events. Further
research is needed to determine the most effective use of this agent in leukemia therapy.
Bortezomib is a proteasome inhibitor that prevents the degradation of misfolded proteins in the cell.
Preclinical work has shown that proteasome inhibitors synergize with steroids such as dexamethasone
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
15/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
in both pre-B and T cell leukemias [132,133]. This agent has shown promise in the treatment of both
pre-B ALL [134] and T cell ALL, and is currently being tested in clinical trials for newly diagnosed T
cell ALL and AML in the Children's Oncology Group.
Several other promising agents are currently in early clinical trials, including two immunotherapies:
The first immunotherapy is blinatumomab, a bi-specific antibody that binds T cells through CD3 and
targets pre-B ALL cells by binding to CD19. This agent has been very effective in eradicating minimal
residual disease in patients with relapsed pre-B ALL [135,136]. Because of its short half-life, the drug
is currently administered by continuous infusion; a delivery method will be logistically challenging and
may limit the usefulness of this agent in the outpatient setting. (See "Treatment of relapsed or
refractory acute lymphoblastic leukemia in adults", section on 'Blinatumomab'.)
The second immunotherapy is a CD19-directed T cell therapy that utilizes a chimeric antigen receptor
(CAR) to target pre-B ALL cells in patients with relapsed pre-B ALL. The CAR receptor has built-in
costimulatory factors that enhance the ability of cytotoxic T cells to eradicate pre-B leukemia cells
[137,138]. This therapy requires the production of individualized T cells using patient white blood cells,
a process that is time-consuming and labor-intensive. The broad use of CAR antibodies awaits the
ability of CAR specificity to be generalized to all patients with relapsed pre-B ALL. (See "Treatment of
relapsed or refractory acute lymphoblastic leukemia in adults", section on 'Chimeric antigen receptor T
cells'.)
Although patients in first relapse usually attain a second remission with induction chemotherapy, they often
relapse after short periods despite aggressive treatment. These patients are candidates for allogeneic
HCT once they have attained second remission [139,140].
Survival after relapse The survival rate of patients who relapse is dependent upon a variety of risk
factors. This was illustrated in a retrospective review of 1961 patients with a relapse from a cohort of 9585
enrolled children with ALL in the Children's Oncology Group clinical trials [141]. The following findings were
noted:
The strongest predictor of survival was the time of relapse from initial diagnosis. Patients who relapsed
less than 18 months after diagnosis had a poor outcome, with a five-year survival rate of
approximately 21 percent.
Five-year survival rates were higher in patients with isolated CNS relapse compared with isolated or
concurrent bone marrow relapse (59, 24, and 39 percent, respectively). A similar study determined
that patients with a late CNS relapse (greater than 18 months from diagnosis) fared better than those
with a relapse prior to 18 months from diagnosis (83 versus 46 percent) [142].
Patients with high-risk disease had a lower survival rate than those with lower risk disease. The lowest
survival rate was in patients with high-risk disease who relapsed before 18 months after diagnosis (15
percent).
After adjusting for site and time of relapse, multivariate analysis of 1391 patients demonstrated that
older age (>10 years), presence of CNS disease at diagnosis, male gender, and T cell disease were
associated with lower survival rates.
As noted above, important predictors of survival include the site and timing of relapse and the prior
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
16/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
treatment regimen. These findings have been confirmed in other prospective clinical trials [126,143,144].
Genetic features As with newly diagnosed disease, findings on routine cytogenetics and FISH
studies may help to stratify children with relapsed disease into prognostic groups. As an example, in
one study, the outcome of children with clinically standard-risk relapsed B cell precursor ALL who had
high-risk cytogenetic findings at relapse was similar to that of children with clinically high-risk relapsed
disease [145].
Site of relapse The long-term survival in ALL patients with bone marrow relapse varies from 5 to 60
percent and depends upon the additional treatment for relapse, standard versus high-risk initial
disease status, and time to relapse [126,143]. Children who have isolated CNS relapse fare better
than those who have bone marrow relapse, with five- to 10-year event-free survival rates of
approximately 54 percent [141]. However, those with early CNS relapse (<36 months from diagnosis)
tend to do less well, with survival rates of only 38 percent [146].
Time to relapse The longer the duration between relapse and the time of diagnosis, the better the
survival rate [126,141]. Patients who relapse after completion of chemotherapy fare better than those
who relapse while still on therapy. Patients with high-risk disease often relapse while still receiving
chemotherapy. For these patients, survival rates improve with increased duration of first remission.
Patients with low-risk disease tend to relapse after the completion of chemotherapy, often after a
prolonged time in remission.
Response to a second therapy regimen correlates directly with the length of first remission [147,148].
As an example, in the experience of the Children's Oncology Group, rates of survival after isolated
bone marrow relapse were 21 percent for those relapsing prior to 18 months from diagnosis versus 50
percent for those relapsing >36 months from diagnosis [141]. Although HCT appears to be more
successful than chemotherapy for patients who relapse early (ie, <36 months), its role in the
management of late failures is less well defined [139,149].
Phase of treatment Patients in the maintenance portion of their chemotherapy who are receiving
methotrexate and 6-mercaptopurine can be successfully treated with more aggressive chemotherapy
regimens. Patients who relapse while receiving induction or consolidation chemotherapy, however,
usually respond poorly to additional chemotherapy. Following reinduction, these patients are often
considered for HCT.
Treatment regimen Outcome also varies by the treatment regimen used at relapse. As an example,
a multicenter phase III randomized trial compared idarubicin with mitoxantrone in 216 children with
relapsed ALL [150]. Consolidation after this second induction was stratified based upon risk. Although
mitoxantrone did not result in an increase in complete remission (CR) rate after induction,
mitoxantrone resulted in significantly higher rates of progression-free (65 versus 36 percent), and
overall (69 versus 45 percent) survival at three years.
The prognosis at the time of relapse, however, does not appear to be related to the intensity of the initial
therapy regimen used in current treatment protocols, or the age at transplantation (ie, patients <14 years
versus 14 to 18 years) [151,152]. As an example, a report from the Childrens Oncology Group included
256 evaluable children with relapsed ALL whose initial ALL treatment was randomly assigned to include
either a standard intensity postinduction regimen or an augmented intensity postinduction regimen [151].
Three-year survival rates after relapse were similar in the two treatment groups (36 versus 39 percent).
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
17/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
INFORMATION FOR PATIENTS UpToDate offers two types of patient education materials, "The Basics"
and "Beyond the Basics." The Basics patient education pieces are written in plain language, at the 5th to
6th grade reading level, and they answer the four or five key questions a patient might have about a given
condition. These articles are best for patients who want a general overview and who prefer short, easy-toread materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more
detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who
want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail
these topics to your patients. (You can also locate patient education articles on a variety of subjects by
searching on "patient info" and the keyword(s) of interest.)
Basics topic (see "Patient education: Leukemia in children (The Basics)")
SUMMARY
Most children with newly diagnosed acute lymphoblastic leukemia (ALL) are treated on research
protocols with risk stratification based upon prognostic indicators available at the time of presentation
(table 1). Such research protocols have helped to standardize treatment, improve survival rates, and
reduce the long-term complications of therapy.
Although cure rates approach and may surpass 80 percent in many studies, significant challenges
remain, particularly for children with adverse prognostic indicators such as induction failure, MLL
rearrangements, IKZF1 mutations, or relapsed ALL. Novel therapies for these patients and the
implementation of new techniques to further refine risk stratification should further improve survival
rates in childhood ALL. (See 'Induction therapy' above.)
Because they are at risk for long-term complications, it is crucial that survivors of childhood ALL
continue regular follow-up with their oncologists after the cessation of chemotherapy. Long-term
complications are related to the type and intensity of the treatment regimen. Patients with high-risk
ALL receive more aggressive chemotherapy and are at greater risk for acute and chronic adverse
effects. (See "Overview of the outcome of acute lymphoblastic leukemia in children and adolescents".)
Use of UpToDate is subject to the Subscription and License Agreement.
Topic 6245 Version 40.0
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
18/21
11/14/2016
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
GRAPHICS
Clinical risk assignment and suggested therapies in childhood acute lymphoblastic
leukemia
Risk
group
Low
Features
ALL of the following:
Percent
Recommended
therapy
Projected
five-year
eventfree
survival
15 percent
C onventional
antimetabolitebased therapy
>95 percent
36 percent
Intensified
antimetabolite
therapy
90 to 95
percent
25 percent
Intensive multiagent
chemotherapy
88 to 90
percent
24 percent
C onsider
allogeneic
hematopoietic cell
transplantation in
first remission
<80 percent
1. NC I standard risk group*
2. Lesser risk cytogenetics:
Trisomies 4 and 10
or
ETV-RUNX1 (United States)
or
Hyperdiploid (Europe)
3. Rapid response to therapy
Average
EITHER of the following:
1. NC I standard risk group*
and
Rapid response to therapy
2. NC I standard risk group*
and
Lesser risk cytogenetics
and
Slow response to therapy
High
ANY of the following:
1. NC I high risk group
and
Rapid response to therapy
2. NC I standard risk group*
and
Slow response to therapy
3. C NS positive leukemia
4. Testicular leukemia
Very high
ANY of the following:
1. MRD+ at day 29
2. Induction failures
3. MLL rearrangements
or
iAMP21 amplification
4. Age <1 year (or >13 years if
treated on a C OG protocol)
Allogeneic
transplant not
recommended for
infants
Special
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
19/21
11/14/2016
groups
Overview of the treatment of acute lymphoblastic leukemia in children and adolescents - UpToDate
T cell ALL
Intensive multiagent
chemotherapy
66 to 80
percent [1,2]
Philadelphia chromosome
[t (9; 22)]
Intensive multiagent
chemotherapy
containing a BC RABL tyrosine
kinase inhibitor
70 percent
[3]
WBC : white blood cell count; NC I: National C ancer Institute; MRD: minimal residual disease; C NS: central
nervous system; MLL: mixed lineage leukemia gene; iAMP21: intrachromosomal amplification of chromosome
21; C OG: C hildren's Oncology Group; ALL: acute lymphoblastic leukemia.
* NC I standard risk group: WBC <50,000/microL AND age one to <10 years.
MRD negative at days 8 and 29 (rapid response to therapy).
MRD positive at day 8 and negative at day 29 (slow response to therapy).
NC I high risk group: WBC 50,000 microL OR age 10 years (up to 13 years if treated on a C OG protocol).
With some exceptions.
References:
1. Dunsmore KP, Devidas M, Linda SB, et al. Pilot study of nelarabine in combination with intensive
chemotherapy in high-risk T-cell acute lymphoblastic leukemia: a report from the Children's Oncology
Group. J Clin Oncol 2012; 30:2753.
2. Asselin BL, Devidas M, Wang C, et al. Effectiveness of high-dose methotrexate in T-cell lymphoblastic
leukemia and advanced-stage lymphoblastic lymphoma: a randomized study by the Children's Oncology
Group (POG 9404). Blood 2011; 118:874.
3. Schultz KR, Carroll A, Heerema NA, et al. Long-term follow-up of imatinib in pediatric Philadelphia
chromosome-positive acute lymphoblastic leukemia: Children's Oncology group study AALL0031.
Leukemia 2014; 28:1467.
Graphic 71649 Version 5.0
https://www.uptodate.com/contents/overview-of-the-treatment-of-acute-lymphoblastic-leukemia-in-children-and-adolescents/print?source=search_result&searc
20/21
Potrebbero piacerti anche
- Principles of Cancer Biology 1st EditionDocumento57 paginePrinciples of Cancer Biology 1st Editiondarren.barnett949100% (44)
- Case Study AllDocumento22 pagineCase Study AllGeraldine Gallaron - CasipongNessuna valutazione finora
- Key chemotherapy drugs and their mechanismsDocumento7 pagineKey chemotherapy drugs and their mechanismsNoelani-Mei AscioNessuna valutazione finora
- Hematology & Oncology - Passmedicine 2012Documento64 pagineHematology & Oncology - Passmedicine 2012dheajst100% (1)
- Pharmacology - CANCER FinalDocumento18 paginePharmacology - CANCER FinalCarol NavidadNessuna valutazione finora
- Drug Name Mechanism Application Side Effects Contraindication Drug-Drug InteractionsDocumento3 pagineDrug Name Mechanism Application Side Effects Contraindication Drug-Drug Interactionsazhar hussinNessuna valutazione finora
- Blood Administration: NRS 108 Essec County CollegeDocumento22 pagineBlood Administration: NRS 108 Essec County CollegeDiah Puspita RiniNessuna valutazione finora
- HaemoglobinDocumento47 pagineHaemoglobinPreethi AbhilashNessuna valutazione finora
- Interpretation of Liver Enzyme Tests - A Rapid GuideDocumento3 pagineInterpretation of Liver Enzyme Tests - A Rapid Guidesserggios100% (2)
- Fibroids ADocumento242 pagineFibroids Anautilus81100% (1)
- Fast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsDa EverandFast Facts: Measurable Residual Disease: A clearer picture for treatment decisionsNessuna valutazione finora
- Hematology Review 2021-2Documento142 pagineHematology Review 2021-2Maram AbdullahNessuna valutazione finora
- HRSDocumento63 pagineHRSPriya KalariaNessuna valutazione finora
- Fluid Resuscitation and Organ Perfusion EvaluationDocumento66 pagineFluid Resuscitation and Organ Perfusion EvaluationDewiRatnasariNessuna valutazione finora
- Bone Marrow TransplantationDocumento21 pagineBone Marrow TransplantationMorrison George100% (1)
- ALL Case PresentationDocumento43 pagineALL Case PresentationMonica MoralesNessuna valutazione finora
- Stem Cell TransplantationDocumento13 pagineStem Cell TransplantationMylls MondejarNessuna valutazione finora
- Step 2 CK Review - HematologyDocumento18 pagineStep 2 CK Review - Hematologyrsmd1986Nessuna valutazione finora
- 3 Bone Marrow ExaminationDocumento105 pagine3 Bone Marrow ExaminationShourav SarkarNessuna valutazione finora
- Clinical Presentation, Pathologic Features, Diagnosis, and Differential Diagnosis of Chronic Lymphocytic Leukemia - UpToDateDocumento23 pagineClinical Presentation, Pathologic Features, Diagnosis, and Differential Diagnosis of Chronic Lymphocytic Leukemia - UpToDateJosé Martínez100% (1)
- Cancer ChemotherapyDocumento9 pagineCancer ChemotherapyJennicaNessuna valutazione finora
- Diabetic Emergencies Case StudiesDocumento32 pagineDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Guidelines in ChemotherapyDocumento36 pagineGuidelines in ChemotherapyIndonesian Journal of Cancer100% (1)
- Hematology MCQSDocumento36 pagineHematology MCQSLorelie ChenNessuna valutazione finora
- What Is A Bone Marrow Transplant?Documento4 pagineWhat Is A Bone Marrow Transplant?Krisna AgustiniNessuna valutazione finora
- What Is HyperlipidemiaDocumento9 pagineWhat Is Hyperlipidemiaichanara100% (2)
- Bone Marrow TransplantDocumento8 pagineBone Marrow TransplantPSRI hospitalNessuna valutazione finora
- Managing Hyperleukocytosis in Acute LeukemiaDocumento10 pagineManaging Hyperleukocytosis in Acute LeukemiaNaty AlvarezNessuna valutazione finora
- UrosepsisDocumento22 pagineUrosepsisWita Ferani KartikaNessuna valutazione finora
- Orientation To Blood Bank 2Documento24 pagineOrientation To Blood Bank 2Darshita SharmaNessuna valutazione finora
- 2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Documento5 pagine2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Lloyd LinNessuna valutazione finora
- LSM4225-1 CytogeneticsDocumento63 pagineLSM4225-1 CytogeneticseveNessuna valutazione finora
- Hematological Diseases and Anemia ClassificationDocumento6 pagineHematological Diseases and Anemia ClassificationBhavya agarwalNessuna valutazione finora
- Acute Myeloid Leukemia in Children 2016Documento10 pagineAcute Myeloid Leukemia in Children 2016Jorge Eduardo Espinoza RiosNessuna valutazione finora
- Acute Lymphoblastic LeukemiaDocumento7 pagineAcute Lymphoblastic LeukemiaSahara EffendyNessuna valutazione finora
- Acute Lymphocytic LeukemiaDocumento7 pagineAcute Lymphocytic LeukemiaKim Enrico JumarangNessuna valutazione finora
- Empirical Treatment of Sepsis in AdultsDocumento11 pagineEmpirical Treatment of Sepsis in AdultsMarnia SulfianaNessuna valutazione finora
- Immune Thrombocytopenic Purpura PDFDocumento12 pagineImmune Thrombocytopenic Purpura PDFAlvin PratamaNessuna valutazione finora
- Relapsed Refractory AMLDocumento114 pagineRelapsed Refractory AMLKishoreChandraKoradaNessuna valutazione finora
- Understanding Thalassemia: Causes, Symptoms and TreatmentDocumento19 pagineUnderstanding Thalassemia: Causes, Symptoms and TreatmentJayricDepalobosNessuna valutazione finora
- Identify CVD Risk in the Office with Framingham & Non-Fasting TestsDocumento28 pagineIdentify CVD Risk in the Office with Framingham & Non-Fasting TestsJuwanto Wakimin100% (1)
- Emergency Department Evaluation Back PainDocumento29 pagineEmergency Department Evaluation Back PainRodolfo GorveñaNessuna valutazione finora
- Anemia in ChildrenDocumento9 pagineAnemia in ChildrenVillegas Sepúlveda AbrahamNessuna valutazione finora
- Goodpasture Syndrome: Lung and Kidney Autoimmune DiseaseDocumento6 pagineGoodpasture Syndrome: Lung and Kidney Autoimmune DiseaseAman singhNessuna valutazione finora
- AkiDocumento42 pagineAkimarauder_popNessuna valutazione finora
- Blood Conservation Methods in Anaesthesia and SurgeryDocumento113 pagineBlood Conservation Methods in Anaesthesia and SurgeryAgya PrempehNessuna valutazione finora
- What Is LeukemiaDocumento11 pagineWhat Is LeukemiaNazneen RagasaNessuna valutazione finora
- Febrile Neutropenia: Nontapak ThiangpakDocumento53 pagineFebrile Neutropenia: Nontapak ThiangpakRapid MedicineNessuna valutazione finora
- 17 ManuscriptDocumento10 pagine17 ManuscriptBaru Chandrasekhar RaoNessuna valutazione finora
- Pathophysiology 2Documento92 paginePathophysiology 2Princess AgarwalNessuna valutazione finora
- Kwashiorkor AND Marasmus: Group 6Documento18 pagineKwashiorkor AND Marasmus: Group 6Christian De GuzmanNessuna valutazione finora
- Types of Leukemia ExplainedDocumento4 pagineTypes of Leukemia ExplainedwizardebmNessuna valutazione finora
- Acute Myeloid Leukemia (Drug Study)Documento3 pagineAcute Myeloid Leukemia (Drug Study)Krisianne Mae Lorenzo FranciscoNessuna valutazione finora
- Plasminogen ActivatorDocumento3 paginePlasminogen ActivatorteocriNessuna valutazione finora
- Acute Lymphoblastic Leukemia (ALL)Documento14 pagineAcute Lymphoblastic Leukemia (ALL)Med PhuongNessuna valutazione finora
- Leukaemia and Lymphoma Whats The DifferenceDocumento7 pagineLeukaemia and Lymphoma Whats The Differencepaul_calburean7899Nessuna valutazione finora
- Acute Myeloid LekumiaDocumento34 pagineAcute Myeloid LekumiaBhuwan ThapaNessuna valutazione finora
- Nur 111 Session 6 Sas 1Documento12 pagineNur 111 Session 6 Sas 1Zzimply Tri Sha UmaliNessuna valutazione finora
- 13-Cis-Retinoic Acid: It's Therapeutic Implications and Adverse EffectsDocumento8 pagine13-Cis-Retinoic Acid: It's Therapeutic Implications and Adverse EffectsBoston Science Publishing100% (1)
- Systemic Lupus Erythematosus 2012Documento564 pagineSystemic Lupus Erythematosus 2012Dan MunteanuNessuna valutazione finora
- Presentasi CKDDocumento21 paginePresentasi CKDNubli LohNessuna valutazione finora
- Leukemia PDFDocumento63 pagineLeukemia PDFErfan Syahid AzhariNessuna valutazione finora
- Immunopharmacology: Dr. Hamad AlshabiDocumento8 pagineImmunopharmacology: Dr. Hamad AlshabiHamad Alshabi100% (1)
- Haematology - Blood Films.Documento6 pagineHaematology - Blood Films.kkkssbbNessuna valutazione finora
- Normal Lab ValuesDocumento1 paginaNormal Lab Valueshurt_y100% (1)
- Adrenal DisordersDocumento29 pagineAdrenal DisordersSuliman Garalleh100% (1)
- Conventional Versus Video Laryngoscopy For.24Documento9 pagineConventional Versus Video Laryngoscopy For.24Isabella HosanaNessuna valutazione finora
- Nej Mo A 1607991Documento11 pagineNej Mo A 1607991Isabella HosanaNessuna valutazione finora
- ReferencesDocumento1 paginaReferencesIsabella HosanaNessuna valutazione finora
- InformedConsent ClinicalstudiesDocumento10 pagineInformedConsent ClinicalstudiestisconNessuna valutazione finora
- Transcatheter Aortic Valve Replacement With EarlyDocumento2 pagineTranscatheter Aortic Valve Replacement With EarlyIsabella HosanaNessuna valutazione finora
- Pi 3 GammaDocumento11 paginePi 3 GammaIsabella HosanaNessuna valutazione finora
- Anticipated Difficult Airway The Role Of.75Documento2 pagineAnticipated Difficult Airway The Role Of.75Isabella HosanaNessuna valutazione finora
- Laureola LornaDocumento3 pagineLaureola LornaIsabella HosanaNessuna valutazione finora
- Christmas Sponsorship2Documento2 pagineChristmas Sponsorship2Isabella HosanaNessuna valutazione finora
- Mechanisms of Disease in Devt of RaDocumento9 pagineMechanisms of Disease in Devt of RaIsabella HosanaNessuna valutazione finora
- Problem of Choice Current Biologic Agents and Future Prospects in RaDocumento10 pagineProblem of Choice Current Biologic Agents and Future Prospects in RaIsabella HosanaNessuna valutazione finora
- WNT SignalDocumento4 pagineWNT SignalIsabella HosanaNessuna valutazione finora
- Pi 3 GammaDocumento11 paginePi 3 GammaIsabella HosanaNessuna valutazione finora
- Mechanisms of Disease in Devt of RaDocumento9 pagineMechanisms of Disease in Devt of RaIsabella HosanaNessuna valutazione finora
- Cns InfectionsDocumento7 pagineCns InfectionsIsabella HosanaNessuna valutazione finora
- Targetng Intracellular Signaling PathwaysDocumento3 pagineTargetng Intracellular Signaling PathwaysIsabella HosanaNessuna valutazione finora
- Autoimmunity Reviews: ReviewDocumento18 pagineAutoimmunity Reviews: ReviewIsabella HosanaNessuna valutazione finora
- Problem of Choice Current Biologic Agents and Future Prospects in RaDocumento10 pagineProblem of Choice Current Biologic Agents and Future Prospects in RaIsabella HosanaNessuna valutazione finora
- Emerging Cell and Cytokine TargetsDocumento12 pagineEmerging Cell and Cytokine TargetsIsabella HosanaNessuna valutazione finora
- Pathogenesis of Ra From NatureDocumento9 paginePathogenesis of Ra From NatureIsabella HosanaNessuna valutazione finora
- Cns InfectionsDocumento7 pagineCns InfectionsIsabella HosanaNessuna valutazione finora
- Septic Shock - Ongoing Management After Resuscitation in Children - UpToDateDocumento23 pagineSeptic Shock - Ongoing Management After Resuscitation in Children - UpToDateIsabella HosanaNessuna valutazione finora
- Risk of Infection in Children With Fever and Non-chemotherapy-Induced Neutropenia - UpToDateDocumento10 pagineRisk of Infection in Children With Fever and Non-chemotherapy-Induced Neutropenia - UpToDateIsabella HosanaNessuna valutazione finora
- Physiology and Classification of Shock in Children - UpToDateDocumento10 paginePhysiology and Classification of Shock in Children - UpToDateIsabella HosanaNessuna valutazione finora
- Jurnal Tirosin Kinase 4Documento13 pagineJurnal Tirosin Kinase 4Maya SariNessuna valutazione finora
- Chronic Myeloid LeukemiaDocumento12 pagineChronic Myeloid Leukemiaapi-408858450Nessuna valutazione finora
- Haematological Malignancies: Classification, Clinical Features and ManagementDocumento54 pagineHaematological Malignancies: Classification, Clinical Features and ManagementSaifSeddikiNessuna valutazione finora
- How I Treat Mixed-Phenotype Acute LeukemiaDocumento9 pagineHow I Treat Mixed-Phenotype Acute LeukemiaFachitah AndrianicNessuna valutazione finora
- What Was The Human Genome Project?Documento12 pagineWhat Was The Human Genome Project?tonxasNessuna valutazione finora
- Xpert BCR-ABL Ultra: Delivering Confidence With Fast and Accurate Chronic Myeloid Leukemia Molecular Monitoring ResultsDocumento4 pagineXpert BCR-ABL Ultra: Delivering Confidence With Fast and Accurate Chronic Myeloid Leukemia Molecular Monitoring ResultsAndrianRakhmatsyahNessuna valutazione finora
- Medicine 8 - AnswersDocumento111 pagineMedicine 8 - Answersgazelle-xNessuna valutazione finora
- ChemotherapyDocumento16 pagineChemotherapyNandhini SaranathanNessuna valutazione finora
- ДокументDocumento72 pagineДокументDianna ArzumanovaNessuna valutazione finora
- Aj. Chulaporn-Bosutinib-Search Engine and Study EndpointsDocumento5 pagineAj. Chulaporn-Bosutinib-Search Engine and Study EndpointsCalm Phurit SenachaiNessuna valutazione finora
- Digital PCR Application - Leukemia enDocumento10 pagineDigital PCR Application - Leukemia enMohammed H. KeshtaNessuna valutazione finora
- Vox Sanguin Juli 2021Documento124 pagineVox Sanguin Juli 2021rsdarsono labNessuna valutazione finora
- Seminar: Florent Malard, Mohamad MohtyDocumento17 pagineSeminar: Florent Malard, Mohamad MohtyStephania SandovalNessuna valutazione finora
- BCR-ABL Medula OsseaDocumento4 pagineBCR-ABL Medula Osseanathaliasantosx3Nessuna valutazione finora
- 10.1038@s41588 018 0315 5Documento20 pagine10.1038@s41588 018 0315 5Omar FernándezNessuna valutazione finora
- Biology Project CancerDocumento20 pagineBiology Project CancerJay PrakashNessuna valutazione finora
- Directory of Service (DOS) - Effective From 1st April 2012Documento74 pagineDirectory of Service (DOS) - Effective From 1st April 2012kgnmatinNessuna valutazione finora
- Acute Lymphoblastic Leukemia in The Older Adult: Ibrahim Aldoss, MD Stephen J. Forman, MD and Vinod Pullarkat, MDDocumento10 pagineAcute Lymphoblastic Leukemia in The Older Adult: Ibrahim Aldoss, MD Stephen J. Forman, MD and Vinod Pullarkat, MDHugo HectorNessuna valutazione finora
- Understanding Acute Leukemia: Signs, Symptoms and TreatmentDocumento46 pagineUnderstanding Acute Leukemia: Signs, Symptoms and TreatmentMaica LectanaNessuna valutazione finora
- Mechanisms of Resistance To Imatinib and Second-GenerationDocumento10 pagineMechanisms of Resistance To Imatinib and Second-GenerationRiyadh Z. MawloodNessuna valutazione finora
- Chronic Myelogenous Leukemia: The PH ChromosomeDocumento1 paginaChronic Myelogenous Leukemia: The PH ChromosomeJolaine ValloNessuna valutazione finora
- 3讲义hematologyDocumento96 pagine3讲义hematologychongyu888xiongNessuna valutazione finora
- Chronic Myeloid LeukemiaDocumento15 pagineChronic Myeloid Leukemiabonitaeffendi100% (1)