Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Articulo 1
Caricato da
Sebastian VallejoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Articulo 1
Caricato da
Sebastian VallejoCopyright:
Formati disponibili
M ET ABOL I SM CL IN I CA L A N D E XP E RI ME N TAL 6 3 ( 2 0 14 ) 10 41 11
Available online at www.sciencedirect.com
Metabolism
www.metabolismjournal.com
Intestinal gluconeogenesis is crucial to maintain a
physiological fasting glycemia in the absence of hepatic
glucose production in mice
Armelle Penhoat a, b, c , Laetitia Fayard a, b, c , Anne Stefanutti a, b, c , Gilles Mithieux a, b, c ,
Fabienne Rajas a, b, c,
a
b
c
Institut National de la Sant et de la Recherche Mdicale, U855, Lyon 69372, France
University of Lyon, Lyon 69008, France
University Lyon 1, Villeurbanne 69622, France
A R T I C LE I N FO
Article history:
AB S T R A C T
Objective. Similar to the liver and kidneys, the intestine has been strongly suggested to be
Received 24 May 2013
a gluconeogenic organ. However, the precise contribution of the intestine to endogenous
Accepted 9 September 2013
glucose production (EGP) remains to be determined. To define the quantitative role of
intestinal gluconeogenesis during long-term fasting, we compared changes in blood glucose
Keywords:
during prolonged fasting in mice with a liver-deletion of the glucose-6 phosphatase catalytic
Endogenous glucose production
(G6PC) subunit (LKO) and in mice with a combined deletion of G6PC in both the liver and the
Glucose homeostasis
intestine (ILKO).
Knockout mice
Materials/Methods. The LKO and ILKO mice were studied after 6 h and 40 h of fasting by
measuring metabolic and hormonal plasmatic parameters, as well as the expression of
gluconeogenic enzymes in the liver, kidneys and intestine.
Results. After a transient hypoglycemic episode (approximately 60 mg/dL) because of
their incapacity to mobilize liver glycogen, the LKO mice progressively re-increased their
plasma glucose to reach a glycemia comparable to that of wild-type mice (90 mg/dL) from
30 h of fasting. This increase was associated with a rapid induction of renal and intestinal
gluconeogenic gene expression, driven by glucagon, glucocorticoids and acidosis. The ILKO
mice exhibited a similar induction of renal gluconeogenesis. However, these mice failed to
re-increase their glycemia and maintained a plasma glucose level of only 60 mg/dL
throughout the 48 h-fasting period.
Conclusions. These data indicate that intestinal glucose production is essential to
maintain glucose homeostasis in the absence of hepatic glucose production during fasting.
These data provide a definitive quantitative estimate of the capacity of intestinal
gluconeogenesis to sustain EGP during long-term fasting.
2014 Elsevier Inc. All rights reserved.
Abbreviations: EGP, endogenous glucose production; G6Pase, glucose-6 phosphatase; G6PC, glucose-6 phosphatase catalytic subunit;
LKO, liver knockout mice; ILKO, intestine and liver knockout mice; PEPCK-c, phosphoenolpyruvate carboxykinase cytosolic form; WT,
wild-type.
Corresponding author. Inserm U855/UCBL Universit Lyon 1 Laennec 7 Rue Guillaume Paradin 69372 Lyon cedex 08, France. Tel.: + 33 478
77 10 28; fax: + 33 478 77 87 62.
E-mail address: fabienne.rajas@univ-lyon1.fr (F. Rajas).
0026-0495/$ see front matter 2014 Elsevier Inc. All rights reserved.
http://dx.doi.org/10.1016/j.metabol.2013.09.005
M ET ABOL I SM CL IN I CA L A N D EX PE RI ME N TA L 6 3 ( 2 0 14 ) 10 41 1 1
1.
Introduction
Endogenous glucose production (EGP) is a crucial physiological function that is essential for the maintenance of a plasma
glucose concentration approximately 90100 mg/dL in the
absence of glucose supplied by food, i.e., between the periods
of meal assimilation and during fasting [13]. The liver,
kidneys and intestine are the three organs contributing to
EGP, as they are the only organs known to express the
catalytic subunit (G6PC) of the glucose-6 phosphatase (G6Pase)
enzyme, which catalyzes the last biochemical step common to
glycogenolysis and gluconeogenesis [4,5].
Although the liver has long been considered the major
contributor to EGP in the post-absorptive state, which includes
fasting, it is well-established that the kidney rapidly increases
its contribution to EGP upon fasting [see [2,6] for review]. We
demonstrated that the kidneys represent nearly 50% of the
EGP after 24 h of fasting in rats instead of approximately 15%
20% in the post-absorptive state (6 h of fasting) [7]. This
finding is consistent with the contribution of the kidneys to
EGP in humans, which represents approximately 5%20% of
the EGP in the post-absorptive state [8,9] and roughly 25%50%
during long-term fasting [8,10]. The intestinal gluconeogenesis is enhanced more progressively during fasting, at least at
the level of gluconeogenic gene expression [11]. However, we
have suggested that the gut would increase its contribution to
EGP from 5%10% in post-absorptive rats to approximately
20%25% after 48 h of fasting [12,13]. This suggests a model
where both intestinal and renal gluconeogenesis could
replace liver gluconeogenesis in the fasting rat [14,15]. In
humans, extrahepatic gluconeogenesis could compensate for
the absence of the liver during the anhepatic phase of liver
transplantation [16,17]. In this case, the kidneys were suggested to contribute to approximately 70% of the EGP with the
remaining 30% being attributed to the intestine [16].
However, the individual contribution of the intestine and
the kidneys in the EGP has yet to be clarified. While the role of
the kidneys seems undeniable, the participation of the
intestine in the EGP during fasting is uncertain, particularly
from a quantitative viewpoint. Therefore, to investigate this
point, we used a novel genetic approach in mice. We
previously showed that liver-specific G6PC knockout (KO)
mice are normoglycemic in the fed state and they resist
fasting. These mice first undergo a transient hypoglycemic
episode due to the absence of liver glycogenolysis [18] but
eventually reach normal fasting glycemia of wild-type mice,
i.e., 90100 mg/dL. This steady state is due to a rapid induction
of renal and intestinal gluconeogenesis [18]. To assess the
respective contribution of the kidneys and the intestine in the
maintenance of fasting plasma glucose during short- and
long-term fasting periods, we generated a mouse model with a
double KO of G6PC in both the liver and the intestine. If
intestinal glucose production is essential to maintain glucose
production during fasting, we hypothesized that the intestine/
liver-KO mice would not maintain their blood glucose at 90
100 mg/dL during long-term fasting. Our data unequivocally
demonstrate the key contribution of the gut in sustaining
plasma glucose during fasting by comparing how liver-KO and
intestine/liver-KO mice undergo fasting.
105
2.
Methods
2.1.
Generation of liver and intestine G6pc knockout mice
Transgenic B6.G6pclox/lox.SACreERT2/w (liver-specific deletion)
and B6.G6pclox/lox.VillCreERT2/w mice (intestine-specific deletion)
were crossed to generate a new mouse model (B6.G6pclox/lox.
SACreERT2/w.VillCreERT2/w mice) [19,20]. These new mice expressed
the inducible Cre-ERT2 recombinase under the control of the
serum albumin (SA) and villin (Vill) promoters. Additionally,
their G6pc exon 3 was flanked by two loxP sites. The mouse
genotypes were determined from tail genomic DNA by PCR with
specific primers [19,20]. The genomic DNA was extracted from
the tissues with a Direct PCR kit (Viagen, Los Angeles, CA,
USA). Male adult (78 week-old) B6.G6pc lox/lox.SA CreERT2/w.
VillCreERT2/w and B6.G6pclox/lox.SACreERT2/w mice were injected
intraperitoneally with 100 L tamoxifen (10 mg/mL, SigmaAldrich) once daily on five consecutive days to obtain the
intestine and liver G6pc KO (ILKO) and liver G6pc KO (LKO)
mice, respectively. The control C57BL/6 J (Charles River Laboratories, LArbresle, France) wild-type (WT) mice were treated
with the same tamoxifen injections. The number of animals
studied is indicated in the figure legends. All mice were housed
in the animal facility of Lyon 1 University (Animaleries Lyon Est
Conventionnelle et SPF) under controlled temperature (22 C)
conditions with a 12-h light/12-h dark cycle. The mice had free
access to water and to a standard rodent starch-enriched diet
(Safe, Augy, France). All procedures were performed in accordance with the principles and guidelines established by the
European Convention for the Protection of Laboratory Animals.
The animal care committee of the Lyon 1 University approved
all experiments. The mice were killed by cervical dislocation in
the post-absorptive state (6 h after food removal) or after 40 h of
fasting, at the age of 1213 weeks. The liver and kidneys were
rapidly removed and flash-frozen in liquid nitrogen. The
intestine (proximal jejunum) was rinsed and immediately
frozen in liquid nitrogen. The frozen tissues were kept at
80 C until use.
2.2.
Metabolic studies
Blood was drawn under isoflurane anesthesia from the retroorbital vein for the plasma metabolite and hormone determinations. The insulin, glucagon, corticosterone, epinephrine and norepinephrine concentrations were determined
with mouse ELISA kits from Crystal Chem (Downers Grove, IL,
USA), Yanaihara Institute (Shizuoka, Japan), Arbor Assays
(Ann Arbor, MI, USA) and Cusabio (Wuhan, China), respectively. The -hydroxybutyrate content was measured using
Optium -ketone test strips with Optium Xceed sensors
(Abbott Diabetes Care, Alameda, CA, USA). The lactate
concentrations were determined with bioMerieux (MarcylEtoile, France) colorimetric kits. The blood glucose was
determined with an Accu-Chek Go glucometer (Roche Diagnostics, Meylan, France) during the fasting experiments. The
hepatic glycogen and glucose-6 phosphate determinations
were carried out as described by Keppler and Decker [21]. The
hepatic triglycerides content was measured using a
106
M ET ABOL I SM CL IN I CA L A N D E XP E RI ME N TAL 6 3 ( 2 0 14 ) 10 41 11
bioMerieux kit after the methanol/chloroform extraction of
the lipids in the liver homogenates.
2.3.
Determination of enzymatic activities
The frozen tissues were reduced to powder at liquid nitrogen
temperature and homogenized in 10 mmol/L HEPES, pH 7.3,
and 0.25 mol/L sucrose (9 vol/g tissue) by ultrasonication. The
G6Pase activity was directly assayed in the homogenates for
10 min at 30 C at pH 7.3 in the presence of a saturating
glucose-6 phosphate concentration (20 mmol/L). The inorganic phosphate release was determined by complexometry [5].
The PEPCK-c activity was assessed using the decarboxylation
assay [22] in the supernatant of the homogenates obtained by
centrifugation for 1 h at 100,000 g. The decarboxylation assay
determines the formation of phosphoenol pyruvate by an
equilibrium displacement that generates oxaloacetate from
malate by malate dehydrogenase in a mixture containing
50 mmol/L Tris, pH 8.0, 0.75 mmol/L MnCl2, 1 mmol/L NAD+,
2.5 U malate dehydrogenase, 1 mmol/L GTP and 50100 L of
cytosolic tissue extract in a 1 mL final volume. The formation
of oxaloacetate was measured spectrophotometrically at
37 C by measuring the NADH formation.
2.4.
Gene expression analyses
The total RNAs were isolated from tissues with the TRIzol
reagent (Invitrogen, Carlsbad, CA, USA). The first strand cDNAs
were synthetized from 500 ng total RNA using M-MLV reverse
transcriptase RNAse H minus (Promega, France) and oligo(dT)
primers. The PCR experiments were completed with Master
SYBR Green Mixture (Roche Diagnostic). The mouse ribosomal
protein mL19 transcript (Rpl19) was used as a reference and the
results were expressed as a ratio compared to the expression of
mL19 in arbitrary units. The following specific primers were
used: 5-TTACCAAGACTCCCAGGACTG-3 (sense located in
exon 1) and 5-GAGCTGTTGCTGTAGTAGTCG-3 (antisense
located in exon 2) for mouse G6pc, 5-AGCCTTTGGTCAACAACTGG-3 (sense) and 5-TGCCTTCGGGGTTAGTTATG-3
(antisense) for mouse Pck1 encoding PEPCK-c and 5GGTGACCTGGATGAGAAGGA-3 (sense) and 5-TTCAGCTTGTGGATGTGCTC-3 (antisense) for Rpl19.
2.5.
Statistical analyses
The data are expressed as means SEMs. The statistical
analyses were performed using either a one-way ANOVA
followed by Tukey's post-hoc test or a two-way ANOVA
followed by Bonferronis test. The differences were considered
statistically significant at p < 0.05.
3.
Results
3.1.
Intestinal and liver glucose-6 phosphatase deletion
in mice
The G6Pase activity was disrupted specifically in the liver and
in the intestine by temporal and tissue-specific KO of the G6pc
gene based on a Cre/lox strategy, as described in the Methods.
The tissue-specificity of the G6pc exon 3 excision was
confirmed by PCR amplification from genomic DNA extracted
from the liver, small intestine and kidneys of the ILKO and
LKO mice (Fig. 1A). A 595-bp PCR fragment corresponding to
the G6pc exon 3-deleted allele was amplified from the genomic
DNA extracted from the liver and intestine of the ILKO mice
and a 1189-bp PCR fragment corresponding to the exon 3
floxed G6pc allele from the kidneys of ILKO mice. The same
amplification generated a 595-bp PCR fragment from only the
liver and a 1189-bp PCR fragment from the intestine and the
kidneys of the LKO mice. In wild-type mice, a 1029-bp PCR
fragment corresponding to the wild-type allele was amplified
from all gluconeogenic organs (Fig. 1A). Accordingly, the
hepatic G6Pase activity was undetectable five weeks after
gene deletion in both ILKO and LKO transgenic mice either in
the post-absorptive state (6 h of fasting) or in the 40 h-fasted
state (Fig. 1B). As previously published, a residual non-specific
intestinal G6Pase activity was still present in the ILKO mice
(Fig. 1C) [20]. These results confirmed the specific excision of
G6pc exon 3 in the liver and the intestine of the ILKO mice when
the gene deletion was induced in adult mice [19,20].
3.2.
Control of blood glucose in intestine/liver-specific
knockout mice
Both the ILKO and the LKO mice exhibited a normal viability
comparable to that of the wild-type mice. They exhibited a
growth rate similar to that of the wild-type mice (Table 1) and
their blood glucose was not significantly different from that of
the wild-type mice in the fed state (160.6 3.9 mg/dL, 149.3
6.5 mg/dL and 167.6 3.9 mg/dL for ILKO, LKO and wild-type
mice, respectively, expressed as means SEMs; n = 15; NS).
When undergoing fasting, the LKO mice exhibited a rapid but
transient drop in plasma glucose to approximately 60 mg/dL
at 6 h of fasting (Fig. 2). This was from their incapability to
mobilize their liver glycogen stores compared to the wild-type
mice (Table 1), as previously reported [18]. In contrast, the
plasma glucose decreased progressively in wild-type mice
undergoing fasting, to plateau at a value approximately
90 mg/dL after 24 h of fasting (Fig. 2). In agreement with
previous data [18], the plasma glucose of the fasted LKO mice
increased again after 6 h of fasting and eventually reached
that of the wild-type mice at 30 h of fasting (Fig. 2). This was
associated with a rapid induction of both G6PC and PEPCK-c
gene expression and enzyme activity in the intestine (Fig. 1C
and 1D) and in the kidneys (Fig. 3), representative of a robust
activation of extrahepatic gluconeogenesis. Similarly, the
intestinal expression of Pck1 mRNA was highly induced in
the ILKO mice (Fig. 1D). The hormonal and metabolic
mechanisms underlying the response to fasting of the LKO
compared to the wild-type mice were thoroughly analyzed in
a previous paper [18]. Thus, we focused our analysis on the
differences characterizing the ILKO compared to the LKO
mice. Interestingly, the early response of the ILKO mice to
fasting (6 h) was relatively comparable to the response of the
LKO mice. Indeed, both the ILKO and LKO mice displayed
the early drop in plasma glucose to 60 mg/dL (Fig. 2). However,
the ILKO and LKO mice displayed a different time course of
plasma glucose concentration upon prolonged fasting. The
107
M ET ABOL I SM CL IN I CA L A N D EX PE RI ME N TA L 6 3 ( 2 0 14 ) 10 41 1 1
LIVER
LKO
ILKO
G6Pase activity (U/g prot)
140
WT
1189 bp
1029 bp
595 bp
ILKO
LKO
WT
120
100
80
60
40
20
0
6h of fasting
40h of fasting
Pck1/Rpl19 mRNA
G6Pase activity (U/g prot)
20
10
40h of fasting
40
INTESTINE
*,$
30
6h of fasting
INTESTINE
50
2
1
0
40hh off fasting
f
Fig. 1 Intestinal- and liver-specific glucose-6 phosphatase deletion in mice. (A) Tissue-specific excision of G6pc exon 3.
Genomic DNA extracted from the liver, intestine and kidneys of ILKO, LKO and wild-type mice was amplified using specific
G6pc primers. Fragments of 1189, 1029 and 595-bp corresponded to the floxed G6pc allele, the wild-type allele and the exon
3-deleted G6pc allele, respectively. The expected sizes are shown on the left of the panel. (BC) The G6Pase activity in the liver
(B) and in the intestine (C) of 6 h- and 40 h-fasted ILKO (black bars), LKO (hatched bars) and wild-type (WT, white bars) mice. (D)
The levels of Pck1 mRNA expressed as a ratio relative to Rpl19 mRNA levels in the intestine of 40 h-fasted ILKO (black bars), LKO
(hatched bars) and wild-type (white bars) mice. The data were obtained five weeks after gene deletion and are expressed as
means SEMs (n = 5 mice per group). The values that are significantly different from the wild-type (*p < 0.05) and the LKO mice
(p < 0.05) are indicated. The values that differ significantly from 6 h of fasting are indicated ($p < 0.05).
ILKO mice were unable to re-increase their plasma glucose,
which plateaued approximately 60 mg/dL throughout the
48 h-fasting period (Fig. 2). This difference could be explained
by the high induction of intestinal G6Pase activity (an
approximate 170% increase) in the LKO mice between 6 h
and 40 h of fasting, while the ILKO mice do not express
intestinal G6Pase (Fig. 1C). It is noteworthy that both the ILKO
and LKO mice displayed the same liver metabolite contents at
6 h of fasting, with a high accumulation of glycogen and
triglycerides in the liver, which leads to hepatomegaly and
steatosis (Table 1). The ILKO and LKO mice also had
comparable plasma parameters (Table 2). As observed in the
LKO mice, the ILKO mice showed a high glucagon level, which
is associated with an increase in corticosterone in comparison
Table 1 Liver weight and liver metabolites in 6 h and 40 h-fasted mice.
6 h of fasting
ILKO
Body weight (g)
Liver weight (g)
Glycogen content (mg/g of liver)
G6P content (mol/g of liver)
TG content (mg/g tissue)
28.7
2.79
67.5
3.7
69.7
0.2
0.13*
5.0*
0.2*
5.5*
LKO
28.6
2.56
65.0
4.7
80.9
0.6
0.2*
2.6*
0.6*
21.1*
40 h of fasting
WT
27.9
1.15
28.6
1.0
17.2
0.6
0.03
3.0
0.1
5.3
ILKO
24.3
2.25
59.8
2.8
78.6
0.5
0.10*
5.3*
0.15*
7.3*
LKO
24.8
2.35
60.6
2.7
65.2
0.8
0.07*
4.8*
0.3*
4.4*
Values are expressed as means SEM (n = 6 mice per group).
Data were determined after 6 h and 40 h of fasting from ILKO, LKO and wild-type (WT) mice, 5 weeks after gene deletion.
Values significantly different from wild-type (*p < 0.05) are indicated.
WT
24
0.75
0.4
0.1
36.0
0.4
0.02
0.3
0.04
3.4
108
M ET ABOL I SM CL IN I CA L A N D E XP E RI ME N TAL 6 3 ( 2 0 14 ) 10 41 11
Blood glucose (mg/dL)
200
100
WT
LKO
$$
$$
50
ILKO
$$
0
12
18
24
30
36
42
48
Time of fasting (hours)
Fig. 2 Glycemia follow-up during long-term fasting. The
blood glucose was determined at different times of fasting in
ILKO (black squares), LKO (white circles) and wild-type (WT,
white squares) mice. The data were obtained five weeks after
the gene deletion and are expressed as means SEMs (n =
10 to 19 mice per group). The ILKO values significantly
different from the wild-type (**p < 0.01, *p < 0.05) and the
LKO (p < 0.01, p < 0.05) mice are indicated. The LKO values
that differ significantly from the wild-type ($$p < 0.01) mice
are indicated.
to the wild-type mice (Table 2). Moreover, no modification of
the stress hormones (epinephrine and norepinephrine) was
observed in the ILKO mice in comparison to the wild-type
mice. However, low blood glucose (60 mg/dL) was associated
with a concomitant increased availability of ketone bodies
(Table 2). In addition, the urinary pH of the ILKO, like the LKO
mice, was more acidic after 6 h of fasting in comparison to the
wild-type mice. This reflects a metabolic acidosis, which is
known to be involved in the activation of Pck1 gene expression
in the kidneys [18]. Interestingly, both the ILKO and LKO mice
showed an induction of renal gluconeogenic gene expression
in comparison to the wild-type mice (Fig. 3). Remarkably, there
was no difference in the liver metabolites or the plasma
parameters between the 40 h fasted-ILKO and the 40 h fastedLKO mice (Tables 1 and 2). Similarly, the induction of renal
gluconeogenic gene expression was comparable in ILKO and
LKO mice after 40 h of fasting (Fig. 3).
4.
Discussion
Although the liver is thus far considered the major site of
glucose production, we emphasize herein the quantitative
role of the intestine and the kidneys in maintaining glucose
homeostasis during prolonged fasting. On one hand, with the
capacity for both intestinal and renal gluconeogenesis, the
LKO mice were able to maintain a physiological glycemia after
30 h of fasting. However, the ILKO mice, with only the capacity
for renal gluconeogenesis, were able to maintain a glycemia
approximately 60 mg/dL throughout fasting.
We previously highlighted the key roles of increased
plasma glucagon and corticosterone in the induction of
renal and intestinal G6Pase gene expression and of metabolic
acidosis in the induction of renal PEPCK-c gene expression in
G6Pase
0
6h of fasting
200
ILKO
LKO
WT
150
40h of fasting
50
0
6h of fasting
0
6h of fasting
40h of fasting
100
100
Pck1/Rpl19 mRNA
250
G6Pase activity (U/g prot)
40h of fasting
PEPCK-c activity (U/g prot)
G6pc/Rpl19 mRNA
PEPCK-c
75
50
25
0
6h of fasting
40h of fasting
Fig. 3 Expression of the main gluconeogenic enzymes in the kidneys of ILKO, LKO and wild-type mice in the post-absorptive
state and during fasting. The levels of G6pc and Pck1 mRNA expressed as a ratio relative to Rpl19 mRNA levels (A and B) and
specific G6Pase and PEPCK-c activities (C and D) of ILKO (black bars), LKO (hatched bars) and wild-type (WT, white bars) mice.
The mice were killed after 6 h or 40 h of fasting. The data were obtained five weeks after the gene deletion and are expressed as
means SEM (n = 5 mice per group). The values significantly different from the wild-type (*p < 0.05) are indicated.
109
M ET ABOL I SM CL IN I CA L A N D EX PE RI ME N TA L 6 3 ( 2 0 14 ) 10 41 1 1
Table 2 Plasma parameters of 6 h-fasted and 40 h-fasted mice.
6 h of fasting
Insulin (ng/mL)
Glucagon (pg/mL)
Glucagon-to-insulin ratio
Corticosterone (ng/mL)
Lactate (mmol/L)
Ketone bodies (mmol/L)
Urinary pH
Epinephrine (ng/mL)
Norepinephrine (pg/mL)
40 h of fasting
ILKO
LKO
WT
ILKO
LKO
WT
0.37 0.05*
343.3 20.8*
1.15 0.10*
234.1 35.1*
6.5 0.3*
1.10 0.13*
5.0 0.1*
<0.2
9.5 1
0.26 0.04*
340.8 40.5*
1.36 0.15*
224.4 8.9*
4.7 0.5*
1.14 0.14*
4.9 0.1*
<0.2
9 1.5
0.78 0.04
66.7 9.
0.09 0.01
56.6 18.1
2.4 0.3
0.60 0.09
5.8 0.2
0.5 0.04
<6
0.07 0.02*
239.2 23.2
2.63 0.50
319.2 15.6
10.3 0.3*
1.95 0.48*
5.8 0.1
<0.2
7.1 0.4
0.06 0.02*
172.9 17.4
2.94 1.08
321.8 53.4
10.8 1.4*
2.15 0.42*
5.9 0.2
<0.2
12.2 1.3
0.26 0.09
166.7 9.8
0.77 0.19
407.8 52.5
7.1 0.3
3.53 0.29
5.9 0.2
<0.2
<6
Values are expressed as means SEM (n = 6 mice per group). Data were determined after 6 h and 40 h of fasting from ILKO, LKO, and wild-type
(WT) mice, 5 weeks after gene deletion.
Values significantly different from wild-type (*p < 0.05) are indicated.
both LKO and wild-type mice upon fasting [18]. However, we
indicated that this induction did not involve any stress
response in terms of catecholamine release, indicating that
a transient hypoglycemic episode (60 mg/dL) is not a stressful
situation in mice. No significant increase in plasma catecholamines was observed herein upon fasting, either in LKO or
ILKO mice. Moreover, the plasma glucose concentration of the
ILKO mice remained low through the 48 h-fasting period
without causing any stress response. This suggests again that
a plasma glucose concentration approximately 60 mg/dL,
even if long-lasting, is compatible with life in mice and may
be considered a low physiological range rather than a
pathophysiological range. This may be related to the concomitant increased availability of ketone bodies from the beginning of the fasting period in both LKO and ILKO mice (Table 2).
Ketone bodies are key alternative energy substrates under
conditions of low glucose availability, such as during fasting
[23]. Furthermore, we observed no difference between ILKO
and LKO mice regarding other key parameters that modulate
glucose fluxes (e.g., plasma insulin and/or glucagon, glucagonto-insulin ratio). Therefore, it appears that the molecular
mechanisms involved in the activation of renal gluconeogenic
genes in ILKO mice were mainly driven by glucagon,
glucocorticoids and acidosis. Hence, the data herein strongly
suggest that intestinal gluconeogenesis is a metabolic process
that allows LKO mice to achieve a normal fasting glycemia
(approximately 90 mg/dL) in the absence of hepatic glucose
production. Interestingly, using a novel genetic approach in
mice, these data are in complete agreement with previous
results on the role of the kidneys (approximately 70%) and the
gut (approximately 30%) in the EGP during the anhepatic
phase of liver transplantation in humans [16].
In addition to its role in the regulation of blood glucose
during long-term fasting, the glucose release by the intestine
could play a major role in energy homeostasis in the postabsorptive state, with a major influence on the control of body
weight and insulin sensitivity. Indeed, intestinal gluconeogenesis via the neural sensing of released glucose into the
portal vein and the transmission of this signal to the brain
plays a key role in the control of hunger and satiety. Hence,
the induction of intestinal gluconeogenesis has provided a
physiological explanation for the satiety effects induced by
protein-enriched diets [24,25]. In addition to its beneficial
effect on the control of food intake, protein-enriched food has
been suggested to improve glycemic control both in type 2
diabetic patients [26] and in rats [7]. The activation of
intestinal gluconeogenesis may also account for the rapid
improvement of insulin sensitivity occurring after gastric
bypass surgery [27,28]. Thus, these novel data emphasize that
intestinal gluconeogenesis must be regarded not only as a key
contributor of glucose during fasting but also as a crucial
signal in the central control of glucose and energy homeostasis, with possible applications in therapeutics for obesity and
diabetes [23].
A second and important inference from the present
study is that kidney gluconeogenesis is sufficient to sustain
a plasma glucose concentration in a low physiological range
during fasting, which is compatible with life without the
mobilization of any stress response by the sympathetic
nervous system. This corroborates previous data in fasting
rats [7] and fasting humans [10], which strongly suggested
that the kidneys may account for approximately 50% of the
total glucose production in the body during fasting. This
highlights the key role of renal glucose production during
the fasting state in rodents and humans. This capacity of
the kidneys to produce glucose is noteworthy in the context
of renal failure because patients with renal failure are prone
to hypoglycemic episodes [29]. Conversely, this finding
could also be considered in the context of diabetes. Indeed,
renal glucose production was increased in both type 1 and
type 2 diabetic patients, which could contribute to hyperglycemia [3032].
In conclusion, the strength of this study is that it
definitively establishes, from a novel genetic approach, the
key contribution of the intestine in the whole body glucose
production during fasting in mice. Our results also emphasize
the major role of the kidneys in EGP on a quantitative level.
This knowledge may have important implications in several
situations in human physiopathology (see above). Moreover,
the induction of intestinal glucose production after bypass
surgery in diabetic rats or mice leads to a rapid amelioration of
insulin resistance [27,28]. It is noteworthy that intestinal
gluconeogenesis might take place after bypass in obese
human [33,34]. In this sense, a weakness of this study is that
we did not determine the impact of the absence of intestinal
glucose production on insulin sensitivity in ILKO mice.
110
M ET ABOL I SM CL IN I CA L A N D E XP E RI ME N TAL 6 3 ( 2 0 14 ) 10 41 11
Another weakness is that we did not study the impact of
absent kidney gluconeogenesis on plasma glucose during
fasting. When available, a mice model with a kidney-specific
knockout of G6pc will most likely be useful to implement for
our understanding of the importance of the kidneys in whole
body glucose control.
Author contributions
A.P. performed the experiments and wrote the manuscript.
L.F. and A.S. participated to the acquisition of data. G.M.
conceived the protocols, interpreted the data and wrote the
manuscript. F.R. conducted the study, interpreted the data
and edited the manuscript. F.R. is the guarantor of this work.
Funding
This work was supported by research grants from the French
National Research Agency (ANR-11-BSV1-009) and the Association Francophone des Glycognoses. The authors thank
INSERM for funding their work and position (A.P.) and the
CNRS (A.S., G.M. and F.R.) for funding their positions.
Acknowledgments
The authors thank the members of Animalerie Lyon Est
Conventionnelle et SPF (University Lyon 1 Laennec, SFR Sant
Lyon Est) for animal care and the members of the CECIL
platform (University Lyon 1 Laennec, SFR Sant Lyon Est). The
authors also thank Prof. Pierre Chambon and Dr. Daniel
Metzger (Mouse Clinical Institute, Strasbourg, France) for
generously providing B6.SA-Cre-ERT2 transgenic mice and
Dr. Sylvie Robine (Paris, France) for generously providing
B6.villin-Cre-ERT2 transgenic mice. The authors are grateful to
Jennifer Vinera for help in editing the manuscript.
Conflict of interest
The authors declare there is no conflict of interest in relation
to this work.
REFERENCES
[1] Ashmore J, Weber G. The role of hepatic glucose-6-phosphatase in the regulation of carbohydrate metabolism. Vitam
Horm 1959;17:91132.
[2] Corssmit EP, Romijn JA, Sauerwein HP. Review article:
regulation of glucose production with special attention to
nonclassical regulatory mechanisms: a review. Metabolism
2001;50(7):74255.
[3] Nordlie RC. Glucose-6-phosphatase phosphotransferase:
roles and regulation in relation to gluconeogenesis. In:
Hanson RW, Mehlman MA, editors. New-York: John Wiley &
Sons; 1976.
[4] Mithieux G, Rajas F, Gautier-Stein A. A novel role for glucose-6
phosphatase in the small intestine in the control of glucose
homeostasis. J Biol Chem 2004;279:442314.
[5] Rajas F, Bruni N, Montano S, Zitoun C, Mithieux G. The
glucose-6 phosphatase gene is expressed in human and rat
small intestine: regulation of expression in fasted and
diabetic rats. Gastroenterology 1999;117(1):1329.
[6] Gerich JE, Meyer C, Woerle HJ, Stumvoll M. Renal gluconeogenesis. Its importance in human glucose homeostasis.
Diabetes Care 2001;24:38291.
[7] Pillot B, Soty M, Gautier-Stein A, Zitoun C, Mithieux G. Protein
feeding promotes redistribution of endogenous glucose
production to the kidney and potentiates its suppression by
insulin. Endocrinology 2009;150(2):61624.
[8] Ekberg K, Landau BR, Wajngot A, et al. Contributions by
kidney and liver to glucose production in the postabsorptive
state and after 60 h of fasting. Diabetes 1999;48:2928.
[9] Stumvoll M, Meyer C, Perriello G, Kreider M, Welle S, Gerich J.
Human kidney and liver gluconeogenesis: evidence for organ
substrate selectivity. Am J Physiol Endocrinol Metab
1998;274(5):E81726.
[10] Owen OE, Felig P, Morgan AP, Wahren J, Cahill GFJ. Liver and
kidney metabolism during prolonged starvation. J Clin Invest
1969;48:57483.
[11] Mithieux G, Bady I, Gautier A, Croset M, Rajas F, Zitoun C.
Induction of control genes in intestinal gluconeogenesis is
sequential during fasting and maximal in diabetes. Am J
Physiol Endocrinol Metab 2004;286:E3705.
[12] Croset M, Rajas F, Zitoun C, Hurot JM, Montano S, Mithieux G.
Rat small intestine is an insulin-sensitive gluconeogenic
organ. Diabetes 2001;50(4):7406.
[13] Mithieux G, Gautier-Stein A, Rajas F, Zitoun C. Contribution of
intestine and kidney to glucose fluxes in different nutritional
states in rat. Comp Biochem Physiol B 2006;143(2):195200.
[14] Minassian C, Mithieux G. Differential time course of liver and
kidney glucose-6 phosphatase activity during fasting in rats.
Comp Biochem Physiol B Biochem Mol Biol 1994;109(1):
99104.
[15] Minassian C, Zitoun C, Mithieux G. Differential time course of
liver and kidney glucose-6 phosphatase activity during longterm fasting in rat correlates with differential time course of
messenger RNA level. Mol Cell Biochem 1996;155(1):3741.
[16] Battezzati A, Caumo A, Martino F, et al. Nonhepatic glucose
production in humans. Am J Physiol Endocrinol Metab
2004;286(1):E12935.
[17] Joseph SE, Heaton N, Potter D, Pernet A, Umpleby MA, Amiel
SA. Renal glucose production compensates for the liver
during the anhepatic phase of liver transplantation. Diabetes
2000;49:4506.
[18] Mutel E, Gautier-Stein A, Abdul-Wahed A, et al. Control of
blood glucose in the absence of hepatic glucose production
during prolonged fasting in mice. Diabetes 2011;60(12):
312131.
[19] Mutel E, Abdul-Wahed A, Nirilanto Ramamonjisoa N, et al.
Targeted deletion of liver glucose-6 phosphatase mimics
glycogen storage disease type 1a including development of
multiple adenomas. J Hepatol 2011;54:52937.
[20] Penhoat A, Mutel E, Amigo-Correig M, et al. Protein-induced
satiety is abolished in the absence of intestinal gluconeogenesis. Physiology & Behavior 2011;105:8993.
[21] Keppler D, Decker K. Glycogen: determination with
amyloglucosidase. In: Methods of enzymatic analysis.
Bergmeyer HU, ed. Deerfield Beach, FL, Verlag-Chemie 1974:
11271131.
[22] Jomain-Baum M, Schramm VL. Kinetic mechanism of phosphoenolpyruvate carboxykinase (GTP) from rat liver cytosol.
Product inhibition, isotope exchange at equilibrium, and
partial reactions. J Biol Chem 1978;253(10):364859.
M ET ABOL I SM CL IN I CA L A N D EX PE RI ME N TA L 6 3 ( 2 0 14 ) 10 41 1 1
[23] Delaere F, Magnan C, Mithieux G. Hypothalamic integration
of portal glucose signals and control of food intake and
insulin sensitivity. Diabetes Metab 2010;36(4):25762.
[24] Duraffourd C, De Vadder F, Goncalves D, et al. Mu-opioid
receptors and dietary protein stimulate a gut-brain neural
circuitry limiting food intake. Cell 2012;150(2):37788.
[25] Mithieux G, Misery P, Magnan C, et al. Portal sensing of
intestinal gluconeogenesis is a mechanistic link in the
diminution of food intake induced by diet protein. Cell Metab
2005;2(5):3219.
[26] Gannon MC, Nuttall FQ. Effect of a high-protein, lowcarbohydrate diet on blood glucose control in people with
type 2 diabetes. Diabetes 2004;53(9):237582.
[27] Sun D, Wang K, Yan Z, et al. Duodenal-jejunal bypass surgery
up-regulates the expression of the hepatic insulin signaling
proteins and the key regulatory enzymes of intestinal
gluconeogenesis in diabetic Goto-Kakizaki rats. Obes Surg
2013;23(11):173442.
[28] Troy S, Soty M, Ribeiro L, et al. Intestinal gluconeogenesis
is a key factor for early metabolic changes after gastric bypass
but not after gastric lap-band in mice. Cell Metab 2008;8(3):
20111.
111
[29] Arem R. Hypoglycemia associated with renal failure. Endocrinol Metab Clin North Am 1989;18(1):10321.
[30] Meyer C, Stumvoll M, Nadkarni V, Dostou J, Mitrakou A,
Gerich J. Abnormal renal and hepatic glucose metabolism in
type 2 diabetes mellitus. J Clin Invest 1998;102:61924.
[31] Mithieux G. A synergy between incretin effect and intestinal
gluconeogenesis accounting for the rapid metabolic benefits
of gastric bypass surgery. Current Diabetes Reports 2012;12(2):
16771.
[32] Mitrakou APD, Vlachos L, D Mourikis, et al. Increased
renal glucose production in insulin dependent diabetes
(IDDM): contribution to systemic glucose appearance and
effect of insulin repletion (Abstract). Diabetes
1996;45(Suppl. 2):33A.
[33] Hayes MT, Foo J, Besic V, Tychinskaya Y, Stubbs RS. Is
intestinal gluconeogenesis a key factor in the early changes
in glucose homeostasis following gastric bypass? Obes Surg
2011;21(6):75962.
[34] Mithieux G. Comment about intestinal gluconeogenesis after
gastric bypass in human in relation with the paper by Hayes
et al., Obes. Surg. 2011. Obes Surg 2012;22(12):19202 [author
reply 19231924].
Potrebbero piacerti anche
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Banquet ServerDocumento4 pagineBanquet ServerMichal Kaczmarz100% (3)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Icds N AayDocumento8 pagineIcds N AayMeghan PaulNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Dishwasher Manual 9000568171Documento81 pagineDishwasher Manual 9000568171Matt WinneNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grain Preservation BiosystemDocumento429 pagineGrain Preservation BiosystemBufalo GennaroNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Tra Vinh 11Documento11 pagineTra Vinh 11Pluvi OphileNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Sarap BuhayDocumento21 pagineSarap BuhayMICHAEL STEPHEN GRACIASNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- When She Danced Martin Sherman PDFDocumento46 pagineWhen She Danced Martin Sherman PDFNina EararNessuna valutazione finora
- SushiDocumento6 pagineSushiMonil ChhedaNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Oaxaca: Contemporary Art Museum (Maco Pre-Hispanic Art Museum "Rufino TamayoDocumento3 pagineOaxaca: Contemporary Art Museum (Maco Pre-Hispanic Art Museum "Rufino TamayoSarahi LaraNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Imports and ExportsDocumento24 pagineImports and ExportsElumalai SrinivasanNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Study Guide Cookery NC 2Documento7 pagineStudy Guide Cookery NC 2FRANCIS D. SACRONessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Shilajit Soma of The AlchemistDocumento2 pagineShilajit Soma of The AlchemistalacrisviamNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- JjajangmyeonDocumento1 paginaJjajangmyeonMiguel VenturaNessuna valutazione finora
- Practical 01 06 J.a.N.gimhani BST17025Documento13 paginePractical 01 06 J.a.N.gimhani BST17025Dulanjali PereraNessuna valutazione finora
- Chilled Taho New Label - Modified 4 27 15Documento1 paginaChilled Taho New Label - Modified 4 27 15Glenn Cabance LelinaNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Gluten-Free Diet TipsheetDocumento2 pagineGluten-Free Diet Tipsheetapi-392216729100% (2)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- DPN Catalog 2012Documento24 pagineDPN Catalog 2012nezyayikNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
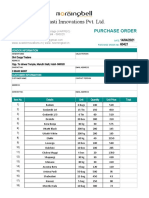
- Purchase Order Template 02 - TemplateLabDocumento3 paginePurchase Order Template 02 - TemplateLabMorning BellNessuna valutazione finora
- 3Rd Unit Test in T.L.E Agricultural Crop ProductionDocumento2 pagine3Rd Unit Test in T.L.E Agricultural Crop Productionlalaine reginaldoNessuna valutazione finora
- Final Case StudyDocumento18 pagineFinal Case Studyapi-487702467100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Go Go Bird MenuDocumento1 paginaGo Go Bird MenuFarley ElliottNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1091)
- Melamine in FoodsDocumento15 pagineMelamine in FoodsAnura Senarathna100% (4)
- Main MenuDocumento1 paginaMain MenuLeandro MachadoNessuna valutazione finora
- Pas 2022-2023 - Bahasa Inggris - XDocumento26 paginePas 2022-2023 - Bahasa Inggris - XasifaanrltNessuna valutazione finora
- OKRA Standards For UKDocumento8 pagineOKRA Standards For UKabc111007100% (2)
- Impact General Placement Test: Choose The Correct AnswerDocumento4 pagineImpact General Placement Test: Choose The Correct AnswerYakeline López100% (1)
- Forum Script - ObesityDocumento5 pagineForum Script - ObesityHUHUHUNessuna valutazione finora
- Industrial Visit ReportDocumento17 pagineIndustrial Visit ReportARPITA BAGH100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- As 2012707Documento20 pagineAs 2012707Sukitha KothalawalaNessuna valutazione finora
- Hasil Survei Tsunami 17 Juli 2006 Pangandaran-Cilacap 23-24 Juli 2006Documento26 pagineHasil Survei Tsunami 17 Juli 2006 Pangandaran-Cilacap 23-24 Juli 2006dodolipet69Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)