Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Cell Injury and Adaptation
Caricato da
أحمدالشحاتTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Cell Injury and Adaptation
Caricato da
أحمدالشحاتCopyright:
Formati disponibili
Cell Injury and Adaptation
Dr. Sayed Abdel Raheem
Cell injury
Dr. Sayed Abdel Raheem
Cell injury
Causes of cell injury
1- Hypoxia:
- It is the most common cause of cell injury
- It is the lack of oxygen content of tissue with inability of cells to synthesize
ATP from aerobic oxidation
- Hypoxia is due to either:
- Ischemia: as in cases of atherosclerosis, thrombosis and embolism
- Cardiopulmonary failure
- Decreased oxygen carrying capacity of blood: as in cases of anemia
2- Infection:
- Due to bacteria, viruses, parasites and fungi
- Mechanism: either
- Direct effect of organisms on cells
- Production of toxins
- Host immune response
3- Immunologic reaction:
Such as in
- Hypersensitivity reaction
- Auto-immune diseases
4- Chemical causes:
- Drugs
- Poisons
- Pollution
- Occupational disease: asbestosis, silicosis, carbon monoxide poisoning
- Social lifestyle: alcohol intake, I.V drug abuse
5- Physical causes:
- Trauma
- Burns
- Radiation
- Forest bite
Dr. Sayed Abdel Raheem
Cell injury
6- Nutritional causes:
- Inadequate calorie intake: marasmus, kwashiorkor, and anorexia
nervosa
- Excess calorie intake: obesity
- Vitamin deficiency: vit. A, B, D, E, K
- Hypervitaminosis
7- Congenital disorders:
-Inborn errors of metabolism
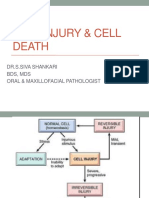
Cellular changes during cell injury
a- Cellular response to injury:
- Adaptation
- Reversible cell injury
- Irreversible cell injury and death (necrosis and apoptosis)
b- Cellular response to injury depends on:
i - The type of injury
ii- Duration including pattern of injury
iii- Severity and intensity of injury
iv- Type of injured cell
v- Metabolic state of cells
vi- Ability of cells to adapt
c- Critical intracellular systems susceptible to injury:
i- DNA
ii- Cell membrane
iii- ATP production
iv- Protein synthesis
Dr. Sayed Abdel Raheem
Cell injury
Cell Injury
1- Reversible Cell Injury:
Cloudy swelling
Hydropic degeneration
Fatty changes
2- Irreversible Cell Injury:
Necrosis
Apoptosis
Mechanism of reversible cell injury
i- Decreased ATP production: by oxidative phosphorylation
ii- Decreased Na pump via cell membrane resulting in:
- Influx of Na and water
- Efflux of K
- Swelling of endoplasmic reticulum
- Swelling of cell (hydropic swelling)
Dr. Sayed Abdel Raheem
Cell injury
iii- Switch to glycolysis resulting in:
- Depletion of cytoplasmic glycogen
- Increased lactic acid production
- Decreased intracellular PH
iv- Decreased protein synthesis: due to detachment of ribosomes from
rough endoplasmic reticulum
Mechanism of irreversible cell injury
i- Severe membrane damage:
- Membrane damage results in massive intracellular influx of calcium
- Efflux of intracellular proteins and enzymes into circulation
ii- Marked mitochondrial dysfunction:
- Mitochondrial swelling
- Damage of oxidative phosphorylation pathway with lack of ATP production
Dr. Sayed Abdel Raheem
Cell injury
iii- Rupture of lysosomes:
- Release of lysosomal enzymes into cytoplasm
- Activation of acid hydrolases followed by autolysis
The hallmark of irreversible injury is membrane damage
The end result of irreversible injury is cell death
Nuclear changes:
- Pyknosis: condensation of nuclear chromatin
- Karyorrhexis: nuclear fragmentation
- Karyolysis: dissolution of nucleus
Dr. Sayed Abdel Raheem
Cell injury
Pyknosis: shrinkage, Hyperchromasia: increased nuclear staining,
Karyorrhexis: nuclear fragmentation
Necrosis
Definition: localized tissue death in living body
Types:
i- Coagulative necrosis:
- Most common type
- Most often due to ischemia
- Due to denaturation and coagulation of proteins within cytoplasm
- Microscopically, there is loss of cellular details with preservation of
cellular outlines (City of ghosts)
- Common in most organs, including heart, liver, spleen, and kidney
ii- Liquefactive necrosis:
- Cellular destruction by hydrolytic enzymes
- Due to autolysis (release of proteolytic enzymes by injured cells) and
heterolysis (release of proteolytic enzymes from inflammatory cells)
- Occurs in abscess and brain infarcts
8
Dr. Sayed Abdel Raheem
Cell injury
Kidney, infarction, gross and microscopic
Lung infarction
Cerebral infarct
Dr. Sayed Abdel Raheem
A- Normal myocardium
Cell injury
B- Myocardium with coagulation necrosis
iii- Caseous necrosis:
- Combination of coagulation and liquefaction necrosis
- Grossly, soft, friable, yellowish and cheese-like
- Characteristic for granulomatous diseases like tuberculosis
iv- Fat necrosis:
- Caused by action of lipases on fatty tissue as in acute hemorrhagic
pancreatitis or trauma to fatty organs like breast
v- Fibrinoid necrosis:
- Necrotic connective tissue resembling fibrin
- Microscopically, has eosinophilic homogenous appearance
- It occurs in acute immnuologic injury as in hypersensitivity type II&III,
and rheumatic myocarditis
vi- Gangrenous necrosis:
- Gangrene means necrosis followed by putrefaction
- Dry gangrene, microscopic pattern is coagulative necrosis
- Wet gangrene, microscopic pattern is liquefactive necrosis
10
Dr. Sayed Abdel Raheem
Cell injury
Caseous necrosis, TB
Fat necrosis, enzymatic, omentum in acute pancreatitis
11
Dr. Sayed Abdel Raheem
Cell injury
Fibrinoid necrosis
Dry gangrene, big toe
Apoptosis
Definition:
- It is a programmed cell death without inflammatory response
- Only affects single cell or small groups of cells
Morphological changes:
- Cell shrinks in size and has dense eosinophilic cytoplasm
- Nuclear chromatin condensation followed by fragmentation
- Formation of cytoplasmic blebs
- Breakdown of cell into fragments (apoptotic bodies)
- Phagocytosis of apoptotic bodies by adjacent cells or macrophages
- Lack of inflammatory response
Regulator genes of apoptosis:
- bcl-2 (inhibits apoptosis by:
- Prevents release of cytochrome C from mitochondria
- Binding pro-apoptosis protease activating factor
- p 53 (stimulates apoptosis) by:
- Elevated by DNA injury and inhibition of cell cycle
- If DNA repair is impossible, p53 stimulates apoptosis
12
Dr. Sayed Abdel Raheem
Cell injury
Physiologic examples of apoptosis:
-Removal of cells during Embryogenesis
- Endometrial shedding during menstrual cycle
- Thymus after puberty
- Post Inflammatory Clean-up
Pathological examples of apoptosis:
- CD8+ T cell-mediated killing of virally infected cells (Councilman
bodies in Viral hepatitis)
- Cystic fibrosis, duct obstruction and atrophy of pancreatic cells
- Tumor cells
- Toxic effect on cells, e.g., chemicals, pathogens
13
Dr. Sayed Abdel Raheem
Cell injury
Skin apoptosis (arrow)
Apoptosis of epidermal cells. The apoptotic cells with intensely eosinophilic
cytoplasm and small, dense nuclei
14
Dr. Sayed Abdel Raheem
Cell injury
Cellular adaptive responses to injury
Atrophy
Definition:
Decrease of size of cell or organ after its full development
Causes:
- Immobilization, decrease of workload or disuse of an organ
- Ischemia, as in atherosclerosis
- Lack of hormonal or neural stimulation such as breast and uterus after
menopause and in paralysis
- Malnutrition
- Aging
Microscopically, small shrunken cells with lipofuscin granules
E/M, decrease intracellular components and autophagosomes
15
Dr. Sayed Abdel Raheem
Cell injury
Kidneys, normal (left) and ischemic atrophy (right) - gross, cut surfaces
16
Dr. Sayed Abdel Raheem
Cell injury
Hypertrophy
Definition:
Increase of size of an organ due to increase of size of its cells
Causes:
- Increase mechanical demand:
- Physiologic: striated muscles of athletes and weight lifters
- Pathologic: left ventricle of heart in hypertension
- Increased endocrine stimulation:
- Gravid uterus
- Lactating breast
Hypertrophy is mediated by growth factors, cytokines, increased
expression of genes, and increased protein synthesis
Hypertrophy and hyperplasia often occurs together
Benign prostatic hyperplasia
Heart, very thick ventricular wall
17
Dr. Sayed Abdel Raheem
Cell injury
Hyperplasia
Definition:
Increase of an organ due to increase of number of its cells
Causes:
- Physiologic causes:
- Compensatory, such as after partial hepatectomy
- Hormonal such as breast after puberty
- Antigenic stimulation such as lymphoid tissue in inflammation
- Pathologic causes :
- Endometrial hyperplasia
- Prostatic hyperplasia
Hyperplasia is mediated by growth factors, cytokines, and increased
expression of proto- oncogenes, increased DNA synthesis, and cell division
Benign prostatic hyperplasia, lining epithelium showing papillary
projections
18
Dr. Sayed Abdel Raheem
Cell injury
Metaplasia
Definition:
Reversible change of one cell type to another cell type in response to
irritation to tolerate environmental stresses
Examples:
- Epithelial metaplasia:
- Bronchial epithelium replaced by stratified squamous epithelium due to
irritation and smoking
- Urinary bladder epithelium replaced by stratified squamous epithelium
due to bilharziasis and urinary stones
- Gall bladder epithelium replaced by stratified squamous epithelium due
to gall bladder stones
- Mesenchymal metaplasia:
- Muscle tissue undergoes chondroid and osseous metaplasia in myositis
ossificans
Under persistent stress, metaplasia can progress to dysplasia and
eventually result in cancer
19
Dr. Sayed Abdel Raheem
Cell injury
Lung, squamous metaplasia
Barrett esophagus
Dysplasia
Definition:
Abnormal proliferation of cells characterized by variation of size, shape and
arrangement
Examples:
- Cervical intraepithelial neoplasia (CIN):
- It occurs in cervix of uterus due to chronic irritation
- It is graded as:
- CIN grade I: affects inner 1/3 of epithelial lining
- CIN grade II: affects inner 2/3 of epithelial lining
- CIN grade III: affects whole thickness of epithelial lining
Other examples of dysplasia, as actinic keratosis of skin and oral
leukoplakia
Dysplasia is not a cancer but may progress to cancer (pre- neoplastic)
severe dysplasia (dysplasia grade III) is considered as carcinoma in situ
20
Dr. Sayed Abdel Raheem
Cell injury
Normal epithelium
Severe dysplasia
Intracellular accumulations
Lipids:
- Triglycerides: such as fatty change of liver
- Cholesterol and LDL: such as atherosclerosis and xanthomas
Fatty change
Definition:
It is a form of reversible cell injury characterized by accumulation of fat in
non-fatty tissue
Sites:
Liver, kidney, heart, muscles
21
Dr. Sayed Abdel Raheem
Cell injury
Fatty change of liver
Causes:
1- Excess intake of fat and carbohydrates
2- Specific liver diseases such as viral hepatitis
3- Starvation
4- Diabetes mellitus
5- Deficiency of lipotropic factors as cholin and methionine
Gross:
The liver is enlarged, yellow, soft, and greasy, due to accumulation of fat
in the hepatocytes
Microscopic:
Hepatocytes contain large vacuoles with compressed nucleus atone side
22
Dr. Sayed Abdel Raheem
Cell injury
Fatty liver
fatty change (steatosis)
23
Dr. Sayed Abdel Raheem
Cell injury
Proteins:
- Russel bodies:
Intracytoplasmic accumulation of immunoglobulines in cases of
Rhinoscleroma
- Councilman bodies: in cases of viral hepatitis
- Proximal renal tubular epithelium in protienuria
Glycogen:
- In cases of glycogen storage disease
Exogenous pigments:
- Anthracosis: deposition of carbon particles in interstitial tissue of lung
due to inhalation of carbon particles
- Tattooing
- Ingestion of lead resulting in gingival lead line
Russel bodies
Councilman Bodies, in viral hepatitis
24
Dr. Sayed Abdel Raheem
Cell injury
Anthracosis of the lung
Endogenous pigments:
Lipofuscin:
Peri -nuclear yellow-brown pigment deposition in cases of brown atrophy
of the heart
Melanin:
Black-brown pigment deposition in skin in cases of navi and melanoma
Hemosidrin:
Golden-yellow-brown pigment, such as in cases of hemorrhage, heart
failure cells in cases of CVC of lung
Bilirubin:
Such as in jaundice and kernicterus (deposition of bilirubin in basal
ganglia) of newborn
25
Dr. Sayed Abdel Raheem
Cell injury
Lipofuscin granules in cardiac myocyte: A, light microscopy (deposits
indicated by arrows), and B, electron microscopy (note the perinuclear,
intralysosomal location)
Hemosiderin granules in liver cells, A, H&E section showing goldenbrown, finely granular pigment. B, Prussian blue reaction, specific for iron
26
Dr. Sayed Abdel Raheem
Cell injury
Liver: green yellow discoloration
Intracellular of bilirubin
Hyaline change
Definition:
Non-specific term used to describe any intra- or extracellular alteration that
has homogenous pink and structurless on H&E stains
Examples of intracellular hyaline:
- Russel bodies in rhinoscleroma
- Mallory bodies in liver in cases of alcholism
- Renal tubules in cases of protienuria
Examples of extracellular hyaline:
- Arteriolar wall in cases of hyaline arteriolosclerosis
- Amyloidosis
- Hyaline membrane disease of newborn
- Corpora amylacea in benign prostatic hyperplasia
27
Dr. Sayed Abdel Raheem
Cell injury
Hyalinosis of blood vessels of spleen
Pathological calcification
Definition:
Abnormal deposition of calcium salts in areas other than bone and teeth
A- Dystrophic calcification:
Definition:
It is abnormal deposition of calcium phosphates in necrotic and dead tissue
Examples:
- Psammoma bodies: laminated calcified bodies in cases of meningiomas,
papillary carcinoma of thyroid and ovary
- Traumatic fat necrosis of beast
- Enzymatic fat necrosis in cases of acute hemorrhagic pancreatitis
- Atherosclerotic plaques
- Monkberg medial calcific sclerosis
28
Dr. Sayed Abdel Raheem
Cell injury
Dystrophic calcification: calcium deposits in degenerated valve leaflet
Chronic pancreatitis, main duct is dilated and filled with calcified material
29
Dr. Sayed Abdel Raheem
Cell injury
B-Metastatic calcification:
Definition:
Precipitation of calcium salts in normal tissues due to hypercalcaemia
Causes:
- Hyperparathyroidism
- Parathyroid adenoma
- Renal failure
- Para- neoplastic syndrome
- Vitamin D intoxication
- Milk- alkalie syndrome
- Sarcoidosis
- Paget disease
- Multiple myeloma
Location of calcification in interstitial tissue of stomach, kidneys, lungs and
blood vessels
Calcification, metastatic, kidney
30
Dr. Sayed Abdel Raheem
Cell injury
Amyloidosis
Definition:
It is a group of diseases characterized by deposition of proteinaceous
material in extracellular spaces with pressure atrophy of these cells
Stains of amyloidal material:
a- H&E stains: appears homogenous pink and structureless
b- Congo red stain: appears orange red
c. Apple green birefringence under polarized light
Composition of Amyloid:
1. 90% non-branching fibrillary protein
2. 10% non fibrillary pentagonal substance called Amyloid P (AP)
component
3. Glycosaminoglycans (heparin sulfate)
Systemic Types of Amyloidosis
1. Primary amyloidosis:
Type of amyloid: AL (amyloid light chain)
Plasma cell disorders (multiple myeloma, B-cell lymphomas
Amyloid deposited in git, heart, tongue, larynx, bladder and peripheral
nerves
2. Secondary (Reactive) amyloidosis:
Type of amyloid: AA (amyloid associated protein)
Inflammation and neoplasia
Rheumatoid arthritis , system lupus erythematosus,TB,osteomyelitis,
Crohn, s disease, cancer
Amyloid deposited in liver, kidneys, spleen, lymph nodes and adrenals
3. Familial Mediterranean fever:
Type of amyloid: AA
Fibrillary protein: serum amyloid A (SAA)
Autosomal recessive disease
Recurrent inflammation, fever, and polyneuropathies
4. Hemodialysis-associated amyloidosis:
Type of amyloid: beta 2 microglobulin
31
Dr. Sayed Abdel Raheem
Cell injury
Fibrillary protein microglobulin
Affects 70% of patients on haemodialysis
Amyloid deposited in joints, synovium, and tendon sheath
Localized Types of Amyloid
1. Senile cerebral amyloidosis (Alzheimer disease)
Type of amyloid: beta 2 amyloid protein
Fibrillary protein: amyloid precursor protein (I3APP)
Found in Alzhiemer plaques and in cerebral vessels
The gene for APP is located on chromosome 21
2. Senile cardiac amyloidosis
Type of amyloid: TTR (transthyretin)
Fibrillary protein: transthyretin
Men> 70 years old
May cause cardiomyopathy, heart failure, and arrythmias
3. Endocrine type
Medullary carcinoma of the thyroid (procalcitonin)
Adult-onset diabetes (amylin)
Pancreatic islet cell tumors (amylin)
Clinical Features
1. Distribution of disease in systemic forms
a. Kidney
. Most commonly involved organ
. Nephrotic syndrome
. Progressive renal failure
b. Heart
. Restrictive cardiomyopathy
. Low voltage EKG
. Cardiac arrhythmias and CHF
c. Hepatospleenomegaly
32
Dr. Sayed Abdel Raheem
Cell injury
d. Gastrointestinal tract
. Tongue enlargement
. Malabsorption
2. Diagnosis: biopsy of the rectal mucosa, gingival, or the abdominal fat
pad
3. Prognosis: the prognosis of systemic amyloidosis is poor
Kidney, amyloidosis
Thyroid, medullary carcinoma
Cerebral amyloid
apple green birefringence
33
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Avian Medicine and Surgery in Practice Companion and Aviary BirdsDocumento384 pagineAvian Medicine and Surgery in Practice Companion and Aviary BirdsDrogaria Econômica0% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Thoughts and AdviceDocumento92 pagineThoughts and AdviceRohit SharmaNessuna valutazione finora
- Differential Diagnosis of Glomerular DiseasesDocumento2 pagineDifferential Diagnosis of Glomerular DiseasesMaryam Fadah100% (1)
- Orthostatic HypotensionDocumento9 pagineOrthostatic HypotensionأحمدالشحاتNessuna valutazione finora
- MRCP Material Drive PDFDocumento2 pagineMRCP Material Drive PDFأحمدالشحات100% (1)
- Chapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Documento3 pagineChapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD100% (5)
- Amyloidosis: Marwa Bawab - SP 10Documento51 pagineAmyloidosis: Marwa Bawab - SP 10Marrouch Ba100% (1)
- MCQ Bacteriology 31Documento9 pagineMCQ Bacteriology 31أحمدالشحات100% (1)
- Anatomopathological Session: Case 4 - A 79-Year-Old Man With Congestive Heart Failure Due To Restrictive CardiomyopathyDocumento10 pagineAnatomopathological Session: Case 4 - A 79-Year-Old Man With Congestive Heart Failure Due To Restrictive CardiomyopathyNovie AstiniNessuna valutazione finora
- 6 - Immune Deficiency Diseases 2Documento8 pagine6 - Immune Deficiency Diseases 2Belle Galao GepteNessuna valutazione finora
- OphthslDocumento1 paginaOphthslأحمدالشحاتNessuna valutazione finora
- اشهر اسئله لدكتور دينا شكرىDocumento6 pagineاشهر اسئله لدكتور دينا شكرىأحمدالشحاتNessuna valutazione finora
- Set 3c271ab3Documento12 pagineSet 3c271ab3أحمدالشحاتNessuna valutazione finora
- Amiloidosis JAMA 2020Documento11 pagineAmiloidosis JAMA 2020Matías Jesús Flamm ZamoranoNessuna valutazione finora
- MCI FMGE Previous Year Solved Question Paper 2005 MarchDocumento0 pagineMCI FMGE Previous Year Solved Question Paper 2005 MarchSharat Chandra0% (1)
- Aortic Valve Disease, Transcatheter Aortic Valve Replacement, and The Heart Failure Patient A State-Of-The-Art ReviewDocumento14 pagineAortic Valve Disease, Transcatheter Aortic Valve Replacement, and The Heart Failure Patient A State-Of-The-Art ReviewCarlos Alberto Holguin PalaciosNessuna valutazione finora
- Atlas de Marcadores Tumorales - DakoDocumento120 pagineAtlas de Marcadores Tumorales - Dakodavlab76Nessuna valutazione finora
- Internal Medicine Orals E&a Academia (Exclusive)Documento209 pagineInternal Medicine Orals E&a Academia (Exclusive)Shreya SinghNessuna valutazione finora
- MRP 2017Documento175 pagineMRP 2017vk100% (1)
- Cell Injury & Cell DeathDocumento61 pagineCell Injury & Cell DeathshivarocksNessuna valutazione finora
- 2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryDocumento24 pagine2022 AHA/ACC/HFSA Guideline For The Management of Heart Failure: Executive SummaryAna RuizNessuna valutazione finora
- 1.inflammation & Repair: Cardinal Signs of InflammationDocumento47 pagine1.inflammation & Repair: Cardinal Signs of Inflammationsharu4291Nessuna valutazione finora
- ASNC AND EANM Amyloidosis Practice Points WEBDocumento12 pagineASNC AND EANM Amyloidosis Practice Points WEBElena FlorentinaNessuna valutazione finora
- EULAR Recommendations For The Management of Familial Mediterranean FeverDocumento8 pagineEULAR Recommendations For The Management of Familial Mediterranean FeverTurboNessuna valutazione finora
- Enfermedad Renal y Desordenes HematologicasDocumento11 pagineEnfermedad Renal y Desordenes HematologicasIris GzlzNessuna valutazione finora
- Quick Review PDFDocumento154 pagineQuick Review PDFDr PenCaster100% (1)
- AMYLOIDOSISDocumento22 pagineAMYLOIDOSISMohan ChoudharyNessuna valutazione finora
- 612 FullDocumento5 pagine612 FullthiagoNessuna valutazione finora
- Biomarkers in AmyloidosisDocumento11 pagineBiomarkers in AmyloidosisMathew McCarthyNessuna valutazione finora
- Journal Reading Clinicopathological Study of Lichen Amyloidosis - Kartika Mega Utami BouwDocumento4 pagineJournal Reading Clinicopathological Study of Lichen Amyloidosis - Kartika Mega Utami BouwmarinNessuna valutazione finora
- Review Articles: Medical ProgressDocumento12 pagineReview Articles: Medical ProgressmoiNessuna valutazione finora
- Path Anat Part 1Documento184 paginePath Anat Part 1Javier Saad100% (1)
- Pathology SWT 13.11. 2023Documento19 paginePathology SWT 13.11. 2023Teena VajiNessuna valutazione finora
- AmyloidosisDocumento5 pagineAmyloidosisVenkata Subramanyam RNessuna valutazione finora
- Morpho KrokDocumento106 pagineMorpho KrokPrashant SinghNessuna valutazione finora