Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
81 179 1 SM
Caricato da
concozTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
81 179 1 SM
Caricato da
concozCopyright:
Formati disponibili
Paediatrica Indonesiana
VOLUME 56
January 2016
Number 1
Case Report
Clinical and molecular analysis of Noonan syndrome
in Indonesia: a case report
Iffa Mutmainah1,2, Willy M. Nillesen2, Farmaditya E. P. Mundhofir1, Tri I. Winarni1,
Ineke van der Burgt2, Helger G. Yntema2, Sultana M. H. Faradz1
oonan syndrome (NS; OMIM#163950) is
a relatively common autosomal dominant
disorder with a worldwide prevalence of
approximately 1:1,000 to 1:2,500. The
syndrome is characterized by distinctive facial features,
congenital heart defects (CHD), and short stature.
Distinctive facial features consist of a broad and high
forehead, hypertelorism, downslanting palpebral
fissures, a high arched palate, low set and posteriorly
rotated ears with a thick helix, and a short neck
with excess nuchal skin and low posterior hairline.
Additional relatively frequent features include chest
deformities, cryptorchidism in males, mild intellectual
disability, and bleeding diathesis.1,2
In 2001, missense mutations in the PTPN11
gene were reported in about 50% of NS cases. This
gene encodes the tyrosine protein phosphatase nonreceptor SHP2, which is involved in ERK activation
via RAS-MAPK pathway.3 Later, several other genes
involved in the RAS-MAPK pathway were found
to be mutated in NS individuals without PTPN11
mutations, including KRAS, SOS1, RAF1, NRAS,
BRAF, MAP2K1, and RIT1, as well as mutations in
SHOC2 and CBL causing an NS-like disorder (
Noonan syndrome-like disorder with loose anagen hair/
NSLH and Noonan syndrome-like disorder with or
without juvenile myelomonocytic leukemia/NSLL,
respectively).2,4,5 The involvement of two other genes,
A2ML1 and RRAS is still unclear.6,7
62 Paediatr Indones, Vol. 56, No. 1, January 2016
Despite the relatively high frequency of NS in
the general population, no Indonesian patients have
been reported. Here, we report the first Indonesian
case with a confirmed molecular diagnosis of NS.
Keywords: Noonan syndrome, Turner syndrome,
PTPN11 gene, molecular analysis
The Case
fifteen-year-old girl was suspected to have
Turner syndrome and was referred by her
pediatric endocrinologist to the Center for
Biomedical Research (CEBIOR), Semarang,
Central Java, Indonesia, for a cytogenetic analysis. She
was short compared to the average height of her peers.
On physical examination, her height was 137 cm (<3rd
From the Division of Human Genetics, Center for Biomedical Research
(CEBIOR), Diponegoro University Medical School, Semarang, Indonesia1,
and the Department of Human Genetics, Radboud University Medical
Center, Nijmegen, The Netherlands2
Reprint requests to: Sultana M. H. Faradz, Center for Biomedical
Research (CEBIOR), Diponegoro University Medical School, Jl. Prof.
Soedarto SH no.1, Tembalang, Semarang, Indonesia. Telp. +62-248454714; Fax. +62-24-8454714; Email: sultanafaradz@gmail.com.
Iffa Mutmainah et al: Clinical and molecular analysis of Noonan syndrome
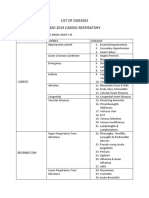
Figure 1. The posterior view of an Indonesian patient with Noonan syndrome shows a low posterior
hairline and a webbed neck.
centile) and her weight was 39 kg (<5th centile). She
had a normal head circumference (54 cm). Facial
dysmorphisms included a high forehead and depressed
nasal bridge. In addition, she had a webbed neck, a low
posterior hairline, and clinodactyly of both 5th toes.
The parents consented only to showing a picture of the
back of the patient (Figure 1). The result of growth
hormone (GH) testing was within the normal range,
as were thyroid function tests. Chromosomal analysis
showed a normal female karyotype (46, XX), even after
reculture and counting more cells in order to exclude
mosaicism for Turner syndrome. Further history-taking
by the pediatrician and medical geneticists revealed
that she had a congenital heart defect. At the age of
10 years, echocardiography showed mild pulmonary
regurgitation, tricuspid regurgitation, and trivial
mitral regurgitation. Follow-up echocardiography
showed normal heart valves, an intact interatrial and
interventricular septum, and good systolic function.
Bone age radiography at the age of ten years was
consistent with that of a 7-year-old girl. Moreover, she
had normal menstrual cycles and breast development.
No other family members had the same phenotype.
Based on the clinical and additional investigations,
NS was suspected.
Molecular analysis of the PTPN11 gene was
performed in the Genome Diagnostics Laboratory of
the Radboud University Medical Center in Nijmegen,
The Netherlands. The DNA was extracted from
peripheral blood lymphocytes using a salting-out
method. All exons and flanking splice sites of the
PTPN11 gene were sequenced on a 3730 automated
sequencer (Applied Biosystems, Foster City, CA).
Primer sequences and PCR conditions are available
upon request. A missense mutation in exon 3 was
identified: c.317A>C, p.(Asp106Ala) (based
on GenBank Accession Number NM_002834.3,
nomenclature according to the Human Genome
Variation Society (HGVS) guidelines.8 Segregation
analysis in both parents revealed that the mutation
was de novo in the child (Figure 2).
Figure 2. Electropherograms of the patient-parents trio. (A): patient, (B): father, and (C): mother. The mutation was absent in both parents, confirming de novo occurrence. The position of the c.317A>C mutation is
indicated by the arrow. The M represents the heterozygous A/C.
Paediatr Indones, Vol. 56, No. 1, January 2016 63
Iffa Mutmainah et al: Clinical and molecular analysis of Noonan syndrome
Discussion
In our patient with a clinical suspicion of NS, a de novo
missense mutation in the PTPN11 gene was detected.
This mutation [c.317A>C; p(Asp106Ala)] was first
reported in 2002 by Tartaglia et al. in two sporadic
cases and in one family.9 Our patient had a webbed
neck, low posterior hairline, a congenital heart defect,
and short stature, all of which are consistent with
the NS features. The patient also showed the typical
dysmorphic facial features, as previously described.10
In the worldwide population, NS is relatively
common. The incidence was estimated to be
approximately 1:1,000 to 1:2,500.1 In 2013, the
Indonesian population was estimated to consist of
almost 250 million people.11 Therefore, between
100,000-250,000 NS cases should be present in
Indonesia. Nevertheless, to our knowledge, no NS
cases from Indonesia have been reported in either
national or international literature. We would not
expect NS to be less prevalent in Indonesia than in
other parts of the world, since most mutations occur
de novo. Furthermore, the heart defect is generally not
lethal in NS, so it is also unlikely that most NS patients
in Indonesia die at a young age, before they are
recognized as NS patients. The most likely explanation
for the lack of reporting on NS in Indonesia is that
the clinical features are not observed to be peculiar
so NS cases are often not recognized. A clinical and
molecular diagnosis of NS is important, however,
because parents should be informed as to the etiology
of the condition in their child, the risk of recurrence
in future pregnancies, and treatment options.
Noonan syndrome shares many phenotypic
similarities with Turner syndrome (TS), the most well
known chromosomal aberration in females. However,
differentiation between NS and TS can be determined
by chromosomal analysis. Turner syndrome is the
most prevalence complete or mosaic monosomy X in
females, while NS is a single gene mutation affecting
both females and males.12 Furthermore, to aid the
diagnostic process, several scoring systems have
been developed. The most commonly used method
was developed by van der Burgt et al. in 1994 (Table
1). A clinical diagnosis of NS can be made when the
typical facial dysmorphology plus another major sign
are present, or two minor signs or suggestive facial
dysmorphology plus two major signs are present, or
64 Paediatr Indones, Vol. 56, No. 1, January 2016
Table 1. Clinical features of our patient compared to those
in published cases of NS
Clinical features*
Facial
A: Typical dysmorphology
B: Suggestive dysmorphology
Cardiac
A: PVS, HCM, and/or ECG typical of NS
B: Other defects
Height
A: <3rd percentile
B: <10th percentile
Chest wall
A: Pectus carinatum/excavatum
B: Broad thorax
Family history
A: First-degree relative with definite NS
B: First-degree relative with suggestive NS
Other
A: ID, cryptorchidism, and lymphatic
dysplasia
B: One of ID, cryptorchidism, or lymphatic
dysplasia
Our patient
+
+
+
NA
* Adapted from van der Burgt (2007),1
A: major sign, B:
minor sign, NA: not available, PVS: pulmonary valve stenosis, HCM:
hypertrophiccCardiomyopathy, ECG: electrocardiogram, ID: intellectual
disability.
three minor signs are present.1
Facial features change with age and become less
noticeable in adulthood. Thus, some adults may be
recognized as having NS after their child has been
diagnosed with NS. While birth length and weight are
usually normal in NS patients, feeding difficulties in
the neonatal period often occur and may cause failure
to thrive. This condition can resolve spontaneously
later in infancy. During childhood, the mean height
is within the lower end of the normal range. With
delayed puberty and reduced or absent pubertal
growth spurt, the mean height falls below the normal
range. A growth catch-up may present in the late
teen years.2,13
More than 70% of NS patients have a broad spectrum of CHDs. The two most common defects are pulmonary valve stenosis (PVS), with or without dysplastic
valve, and hypertrophic cardiomyopathy (HCM). The
presence of PVS is most commonly associated with a
mutation in PTPN11, whereas HCM is associated with
a mutation in RAF1 and RIT1.2,4 Other relatively frequent features are unilateral or bilateral cryptorchidism
in males, skeletal abnormalities particularly superior
pectus carinatum and inferior pectus excavatum, as
Iffa Mutmainah et al: Clinical and molecular analysis of Noonan syndrome
well as bleeding diathesis.1,2 Management guidelines
for NS, including an NS growth chart were released
in 2010.14 Administration of GH showed short-term
growth acceleration, but outcomes of long-term treatment remain inconclusive.15 Therefore, the policy to
offer GH treatment to NS patients differs among countries.16 Regular cardiac evaluations are recommended
during GH treatment.17 Furthermore, as NS is a genetic
and multisystem disorder, a multidisciplinary team approach to patient care is essential for better quality of
life in NS individuals.
In conclusion, we report the first Indonesian
NS case with molecular confirmation. Establishing
a molecular diagnosis is not only important for
confirmation of the diagnosis, but also for genetic
counseling to patients and their families. Since most
of the mutations occur de novo, the recurrence risk for
future offspring is very low, less than 1%.However, when
one of the parents appears to have NS, the recurrence
risk is 50%.18 The publication of this Indonesian NS
case is important to raise awareness for this relatively
common disease, as it has likely been underestimated
in the Indonesian population. Establishing a clinical
diagnosis, and when possible a molecular confirmation,
is important for patients and their families.
Acknowledgments
This study was partially supported by merit scholarship from
Ministry of National Education and Culture, Republic of
Indonesia in collaboration with Radboud University Medical
Center in Nijmegen, The Netherlands. The authors wish to
thank the laboratory staff at the Department of Human Genetics,
Radboud UMC in Nijmegen, The Netherlands and CEBIOR,
Diponegoro University Medical School, Semarang, Central
Java, Indonesia.
Conflict of interest
None declared.
References
1. van der Burgt I. Noonan syndrome. Orphanet J Rare Dis.
2007;2:1-6.
2. Roberts AE, Allanson JE, Tartaglia M, Gelb BD. Noonan
syndrome. Lancet. 2013;381:333-42.
3. Tartaglia M, Mehler EL, Goldberg R, Zampino G, Brunner
HG, Kremer H, et al. Mutations in PTPN11, encoding the
protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet. 2001;29:4658.
4. Nava C, Hanna N, Michot C, Pereira S, Pouvreau N, Niihori
T, et al. Cardio-facio-cutaneous and Noonan syndromes due
to mutations in RAS/MAPK signalling pathway: genotypephenotype relationships and overlap with Costello syndrome.
J Med Genet. 2007;44:763-71.
5. Aoki Y, Niihori T, Banjo T, Okamoto N, Mizuno S, Kurosawa
K, et al. Gain-of-function mutations in RIT1 cause Noonan
syndrome, a RAS/MAPK pathway syndrome. Am J Hum
Genet. 2013;93:173-80.
6. Vissers LE, Bonneti M, Paardekooper Overman J, Nillesen
WM, Frints SG, de Ligt J, et al.
Heterozygous germline mutations in A2ML1 are associated with a disorder clinically
related to Noonan syndrome. Eur J Hum Genet. 2015;23:31724.
7. Chen PC, Yin J, Yu HW, Yuan T, Fernandez M, Yung CK,
et al. Next-generation sequencing identifies rare variants
associated with Noonan syndrome. Proc Natl Acad Sci U S
A. 2014;111:11473-8.
8. Gray KA, Yates B, Seal RL, Wright MW, Bruford EA.
genenames.org: the HGNC resources in 2015. Nucleic Acids
Res. 2015 Jan; 43 (Database issue): D1079-85. doi: 10.1093/
nar/gku1071. PMID: 25361968.
9. Tartaglia M, Kalidas K, Shaw A, Song X, Musat DL, van
der Burgt I, et al. PTPN11 mutations in Noonan syndrome:
molecular spectrum, genotype-phenotype correlation, and
phenotypic heterogeneity. Am J Hum Genet. 2002;70:155563.
10. Bhambhani V, Muenke M. Noonan syndrome. Am Fam
Physician. 2014;89:37-43.
11. Statistic Indonesia (Badan Pusat Statistik). [created 2014
April 07; cited 2014 Aug 21]. Available from: http://www.
bps.go.id/linkTabelStatis/view/id/1274.
12. Romano
AA, Allanson JE, Dahlgren J, Gelb BD, Hall B, Pierpont ME, et al. Noonan syndrome: clinical features, diagnosis,
and management guidelines. Pediatrics. 2010;126:746-59.
13. Padidela R, Camacho-Hbner C, Attie KM, Savage MO.
Abnormal growth in Noonan syndrome: genetic and
endocrine features and optimal treatment. Horm Res.
2008;70:129-36.
14. DYSCERNE-Noonan syndrome guideline development
group. Management of noonan syndrome: a clinical guideline.
University of Manchester. 2010; [cited 2014 Oct 10].
Available from: https://kr.ihc.com/ext/Dcmnt?ncid=52109
Paediatr Indones, Vol. 56, No. 1, January 2016 65
Iffa Mutmainah et al: Clinical and molecular analysis of Noonan syndrome
6050&tfrm=default.
15. Binder G. Noonan syndrome, the Ras-MAPK signalling
pathway and short stature. Horm Res. 2009;71:6470.
16. Raynal P. Growth hormone and Noonan syndrome: update
in dysfunctional signalling aspects and in therapy for short
stature. Horm Stud. 2014;2:1.
17. Noordam C. Growth hormone and the heart in Noonan
66 Paediatr Indones, Vol. 56, No. 1, January 2016
syndrome. Horm Res. 2009;72:49-51.
18. Allanson JE, Roberts AE. Noonan Syndrome. 2001 Nov
15 [Updated 2011 Aug 4]. In: Pagon RA, Adam MP,
Ardinger HH, et al., editors. GeneReviews [Internet].
Seattle (WA): University of Washington, Seattle; 19932016. Available from: http://www.ncbi.nlm.nih.gov/books/
NBK1124/.
Potrebbero piacerti anche
- J 1440-1754 2010 01970-JenniDocumento7 pagineJ 1440-1754 2010 01970-JenniasnsmomNessuna valutazione finora
- Nefrotico 2018 PDFDocumento14 pagineNefrotico 2018 PDFRoxanne RadulovicNessuna valutazione finora
- A Descriptive Study of NPHS1 and NPHS2 Mutations in ChildrenDocumento14 pagineA Descriptive Study of NPHS1 and NPHS2 Mutations in ChildrenCalvin Tanuwijaya Stick BolaNessuna valutazione finora
- External Ear Anomalies and Hearing Impairment in NoonanDocumento17 pagineExternal Ear Anomalies and Hearing Impairment in NoonanPrinksezza LatinnaNessuna valutazione finora
- Adult LeucodystrophyDocumento12 pagineAdult LeucodystrophylauraalvisNessuna valutazione finora
- Congenital Nephrotic Syndrome: A Cases Report: Case Report Open AccessDocumento4 pagineCongenital Nephrotic Syndrome: A Cases Report: Case Report Open AccessAzaliRiccoNessuna valutazione finora
- Sindrome de NoonamDocumento19 pagineSindrome de NoonamLicMarinaGarayNessuna valutazione finora
- Presentation Clinical Spectrum and Chromosomal Abnormalities of Children With Turner 1251Documento6 paginePresentation Clinical Spectrum and Chromosomal Abnormalities of Children With Turner 1251Mai SomaaNessuna valutazione finora
- Discussion: Aspiration DisplayedDocumento4 pagineDiscussion: Aspiration DisplayedmartinNessuna valutazione finora
- Failure To ThriveDocumento3 pagineFailure To ThrivefernandoNessuna valutazione finora
- 15 Follow-Up of Sonographically Detected Soft Markers For Fetal AneuploidyDocumento5 pagine15 Follow-Up of Sonographically Detected Soft Markers For Fetal AneuploidyDiego Bedón AscurraNessuna valutazione finora
- Congenital Toxoplasmosis Associated With Severe Intracerebral Calcification and West SyndromeDocumento3 pagineCongenital Toxoplasmosis Associated With Severe Intracerebral Calcification and West SyndromeDevina Rossita HapsariNessuna valutazione finora
- JURNALDocumento4 pagineJURNALrahastuti drgNessuna valutazione finora
- Noonan Syndrome and Clinically Related Disorders (2011)Documento25 pagineNoonan Syndrome and Clinically Related Disorders (2011)ramonaNessuna valutazione finora
- Down SyndromeDocumento74 pagineDown Syndromeanumeha sharma100% (2)
- Santos Et Al 2011. Hearing Loss and Airway Problems in Children With MucopolysaccharidosesDocumento7 pagineSantos Et Al 2011. Hearing Loss and Airway Problems in Children With MucopolysaccharidosesBoNessuna valutazione finora
- Dysembryoplastic Neuroepithelial Tumors in Childhood: Long-Term Outcome and Prognostic FeaturesDocumento7 pagineDysembryoplastic Neuroepithelial Tumors in Childhood: Long-Term Outcome and Prognostic Featureslucasher35Nessuna valutazione finora
- Diagnostic Exome Sequencing in Persons With Severe Intellectual DisabilityDocumento9 pagineDiagnostic Exome Sequencing in Persons With Severe Intellectual DisabilityMiaNessuna valutazione finora
- Ref 15Documento9 pagineRef 15Tiago BaraNessuna valutazione finora
- Neuroradiological Findings of Trisomy 13 in A Rare Long-Term SurvivorDocumento3 pagineNeuroradiological Findings of Trisomy 13 in A Rare Long-Term Survivorchristian roblesNessuna valutazione finora
- Cerebral Toxoplasmosis in Aids PatientDocumento15 pagineCerebral Toxoplasmosis in Aids PatientnoniclaraNessuna valutazione finora
- Niebuhr, E.: The Cri Du Chat SyndromeDocumento2 pagineNiebuhr, E.: The Cri Du Chat SyndromeThonieroce Apryle Jey MorelosNessuna valutazione finora
- FTPDocumento2 pagineFTPDesta FransiscaNessuna valutazione finora
- ResumenDocumento5 pagineResumenPaulette BuñayNessuna valutazione finora
- Neurodevelopment Down and Heart DefctsDocumento8 pagineNeurodevelopment Down and Heart DefctsJeancarlosTerapiaFisicaNessuna valutazione finora
- Case Discussion SLEDocumento4 pagineCase Discussion SLERanjeetha SivaNessuna valutazione finora
- Reyes - Unit 2 (Part 2)Documento4 pagineReyes - Unit 2 (Part 2)Justine Ericca ReyesNessuna valutazione finora
- Ucm 439476Documento1 paginaUcm 439476Fadel BilondatuNessuna valutazione finora
- How Far Should We Explore Hypospadias? Next-Generation Sequencing Applied To A Large Cohort of Hypospadiac PatientsDocumento9 pagineHow Far Should We Explore Hypospadias? Next-Generation Sequencing Applied To A Large Cohort of Hypospadiac Patientsddd gdhNessuna valutazione finora
- Clinical Diseases With Chromosomal AbnormalitiesDocumento52 pagineClinical Diseases With Chromosomal AbnormalitiesAzifah ZakariaNessuna valutazione finora
- Gender Gap in Deep Brain Stimulation For Parkinson 'S DiseaseDocumento10 pagineGender Gap in Deep Brain Stimulation For Parkinson 'S Diseasemawara khanNessuna valutazione finora
- Thrasivoulos: Cardiomyopathy in Children: Importance of Aetiology in PrognosisDocumento2 pagineThrasivoulos: Cardiomyopathy in Children: Importance of Aetiology in PrognosisDede MarizalNessuna valutazione finora
- Triple X Syndrome With A Rare Finding: Cleft Palate: Case ReportDocumento3 pagineTriple X Syndrome With A Rare Finding: Cleft Palate: Case ReportDewi JayantiNessuna valutazione finora
- Klinefelter Early DiagnosedDocumento7 pagineKlinefelter Early DiagnosedPratita Jati PermatasariNessuna valutazione finora
- Paediatrica Indonesiana: Case ReportDocumento9 paginePaediatrica Indonesiana: Case ReportEHbsd WardNessuna valutazione finora
- Progressive Increase of The Mutated Mitochondria1 DNA Fraction in Kearns-Sayre SyndromeDocumento6 pagineProgressive Increase of The Mutated Mitochondria1 DNA Fraction in Kearns-Sayre SyndromeGréta BotyánszkiNessuna valutazione finora
- Case Report Turner Syndrome Michael Final PrintDocumento35 pagineCase Report Turner Syndrome Michael Final PrintMichael MettafortunaNessuna valutazione finora
- Ultrasonido Doppler Temprano AMSDocumento7 pagineUltrasonido Doppler Temprano AMSKaren Marbelly OrozcoNessuna valutazione finora
- Journal Noonan SyndromeDocumento7 pagineJournal Noonan SyndromeSheilla GiustiNessuna valutazione finora
- Infectious Dan Autoantibody Associated EncephalitisDocumento13 pagineInfectious Dan Autoantibody Associated EncephalitisAyudiah ParamitaNessuna valutazione finora
- Down Syndrome REG Last EditDocumento60 pagineDown Syndrome REG Last EditJane NeduNessuna valutazione finora
- Neural Tube DefectsDocumento12 pagineNeural Tube Defectsdaniel_1592Nessuna valutazione finora
- Geller 2015Documento14 pagineGeller 2015Michelle BaldacciNessuna valutazione finora
- Case Report FinalDocumento14 pagineCase Report FinalAaron Lemuel OngNessuna valutazione finora
- Jurnal PEIDocumento4 pagineJurnal PEIMadonna Frozen100% (1)
- Cornelia de Lange Syndrome - A Recognizable Fetal PhenotypeDocumento5 pagineCornelia de Lange Syndrome - A Recognizable Fetal PhenotypeTien Chen TuNessuna valutazione finora
- A Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsDocumento9 pagineA Cohort Study To Assess The New WHO Japanese Encephalitis Surveillance StandardsarmankoassracunNessuna valutazione finora
- Grunt2010 Cerebral Sinus Venous Thrombosis in Swiss ChildrenDocumento6 pagineGrunt2010 Cerebral Sinus Venous Thrombosis in Swiss ChildrenModou NianeNessuna valutazione finora
- 456 FullDocumento4 pagine456 FullDino GoncalvesNessuna valutazione finora
- Develop Med Child Neuro - 2022 - Houwen Van Opstal - Long Term Outcomes For Females With Early Onset DystrophinopathyDocumento12 pagineDevelop Med Child Neuro - 2022 - Houwen Van Opstal - Long Term Outcomes For Females With Early Onset DystrophinopathyJessica CampoNessuna valutazione finora
- Angelman SyndromeDocumento4 pagineAngelman SyndromeRowena DigalNessuna valutazione finora
- Uncommon Disorders Masquerading As Acute Flaccid Paralysis in ChildrenDocumento7 pagineUncommon Disorders Masquerading As Acute Flaccid Paralysis in ChildrenAnonymous G20oAbl6p8Nessuna valutazione finora
- Congenital Hypotonia Is There An AlgorithmDocumento4 pagineCongenital Hypotonia Is There An AlgorithmEvelyn HerreraNessuna valutazione finora
- Actualización en El Manejo Del Síndrome de Turner en Niñas y Adolescentes. Revisión de La Literatura e Incorporación de Recomendaciones de Las Nuevas Guías ClínicasDocumento8 pagineActualización en El Manejo Del Síndrome de Turner en Niñas y Adolescentes. Revisión de La Literatura e Incorporación de Recomendaciones de Las Nuevas Guías ClínicasLopez Alvarado JheisonNessuna valutazione finora
- Thanatoporic Dysplasia FIXDocumento7 pagineThanatoporic Dysplasia FIXYudha GanesaNessuna valutazione finora
- Diagnosis and Management of Down Syndrome: Guest Editor: Bhim S. PandhiDocumento8 pagineDiagnosis and Management of Down Syndrome: Guest Editor: Bhim S. PandhiRidwan Balatif - Co-AsstNessuna valutazione finora
- Gallicchio 2003Documento6 pagineGallicchio 2003Cristina Georgiana SerbanNessuna valutazione finora
- Henoch Schonlein Purpura (IgA Vasculitis)Documento15 pagineHenoch Schonlein Purpura (IgA Vasculitis)Emily Eresuma100% (1)
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDa EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNessuna valutazione finora
- Delirium: Acute Brain Dysfunction in the Critically IllDa EverandDelirium: Acute Brain Dysfunction in the Critically IllChristopher G. HughesNessuna valutazione finora
- Antihyperglycemic Agents Comparison Chart PDFDocumento9 pagineAntihyperglycemic Agents Comparison Chart PDFconcoz100% (1)
- Antihyperglycemic Agents Comparison Chart PDFDocumento9 pagineAntihyperglycemic Agents Comparison Chart PDFconcoz100% (1)
- Soal MCQ 3 Nov 2014Documento17 pagineSoal MCQ 3 Nov 2014Funnie AdeliaNessuna valutazione finora
- Initiation and Use of Propranolol For Infantile Hemangioma: Report of A Consensus ConferenceDocumento15 pagineInitiation and Use of Propranolol For Infantile Hemangioma: Report of A Consensus ConferenceNur Melani Sari WardaniNessuna valutazione finora
- 7 - Sorasak Respiratory Care HFMDDocumento6 pagine7 - Sorasak Respiratory Care HFMDconcozNessuna valutazione finora
- BPAC Introduction FinalDocumento38 pagineBPAC Introduction FinalconcozNessuna valutazione finora
- 55 3 11 PDFDocumento9 pagine55 3 11 PDFshasyaNessuna valutazione finora
- WarezDocumento124 pagineWarezconcozNessuna valutazione finora
- Tetralogy of FallotDocumento28 pagineTetralogy of FallotconcozNessuna valutazione finora
- CD008635 AbstractDocumento4 pagineCD008635 AbstractconcozNessuna valutazione finora
- Disturbances of PigmentationDocumento118 pagineDisturbances of PigmentationconcozNessuna valutazione finora
- 2012 Health Effects and Cell Phone Base StationsDocumento11 pagine2012 Health Effects and Cell Phone Base StationsconcozNessuna valutazione finora
- Thione Whitening SlidesDocumento6 pagineThione Whitening SlidesconcozNessuna valutazione finora
- Newborn Umbilical Cord Care - An Evidence Based Quality ImprovemenDocumento45 pagineNewborn Umbilical Cord Care - An Evidence Based Quality ImprovemenNuridha FauziyahNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 2013 KCCS Diploma Course PDFDocumento16 pagine2013 KCCS Diploma Course PDFconcozNessuna valutazione finora
- 460 523 1 PBDocumento6 pagine460 523 1 PBconcozNessuna valutazione finora
- Obstetrics 4Documento5 pagineObstetrics 4concozNessuna valutazione finora
- Preventif Pada PreeklampsiDocumento12 paginePreventif Pada PreeklampsiconcozNessuna valutazione finora
- Nausea and Vomiting in Pregnancy: MedicineDocumento8 pagineNausea and Vomiting in Pregnancy: Medicineapi-315854829Nessuna valutazione finora
- 460 523 1 PBDocumento6 pagine460 523 1 PBconcozNessuna valutazione finora
- Css Tetralogy of Fallot DoddyDocumento14 pagineCss Tetralogy of Fallot DoddyIman SrchmnNessuna valutazione finora
- WarezDocumento124 pagineWarezconcozNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Kejang Demam'Documento11 pagineKejang Demam'concozNessuna valutazione finora
- Kejang Demam'Documento11 pagineKejang Demam'concozNessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Ophthalmia NeonatorumDocumento2 pagineOphthalmia NeonatorumconcozNessuna valutazione finora
- Funduscopy of Retinal PathologiesDocumento4 pagineFunduscopy of Retinal PathologiesAvinindita Nura LestariNessuna valutazione finora
- M.Ch. CVSDocumento43 pagineM.Ch. CVSRithikaNessuna valutazione finora
- List of Diseases Imo 2019 Cardio-RespiratoryDocumento2 pagineList of Diseases Imo 2019 Cardio-RespiratoryDimas Adjie Yuda MahendraNessuna valutazione finora
- Seeley's Essentials of Anatomy & Physiology (10thDocumento4 pagineSeeley's Essentials of Anatomy & Physiology (10thZiaNessuna valutazione finora
- UrosepsisDocumento35 pagineUrosepsisdrasas690Nessuna valutazione finora
- Acute Kidney InjuryDocumento17 pagineAcute Kidney InjuryCha-cha UzumakiNessuna valutazione finora
- Lung AbscessDocumento10 pagineLung AbscessCherlotte TbNessuna valutazione finora
- Ncma217 Week 9Documento11 pagineNcma217 Week 9Polly ArcheronNessuna valutazione finora
- D Pharmacy 1st Year B Pharm First Sem - Anatomy & Physiology Notes - Solved Question PaperDocumento28 pagineD Pharmacy 1st Year B Pharm First Sem - Anatomy & Physiology Notes - Solved Question Papersham100% (2)
- Heart Disease in PregnancyDocumento87 pagineHeart Disease in PregnancyMonisha ArulalanNessuna valutazione finora
- Student Handbook: Metabolism System Stage 2Documento22 pagineStudent Handbook: Metabolism System Stage 2Awais_123Nessuna valutazione finora
- Wacp 2020 Recalls: Ucth April/Oct 2020Documento49 pagineWacp 2020 Recalls: Ucth April/Oct 2020Walter EgbaraNessuna valutazione finora
- Obstetrics - MCQ - 3rd - BHMS - (Old, New, 2015)Documento25 pagineObstetrics - MCQ - 3rd - BHMS - (Old, New, 2015)Anil kadamNessuna valutazione finora
- Cardiovascular DiseaseDocumento3 pagineCardiovascular Diseasearif wicaksonoNessuna valutazione finora
- Carotid Sinus MassageDocumento3 pagineCarotid Sinus MassageSandeep m rNessuna valutazione finora
- Lecture 33 - Biomarkers: Learning ObjectivesDocumento37 pagineLecture 33 - Biomarkers: Learning ObjectivesAustin KellyNessuna valutazione finora
- PNLE - Renal ExamDocumento22 paginePNLE - Renal ExamRay Mays100% (1)
- Diagnosis and Treatment of Avian Renal Disease: Christal Pollock, DVM, DABVP-AvianDocumento22 pagineDiagnosis and Treatment of Avian Renal Disease: Christal Pollock, DVM, DABVP-AvianjudithNessuna valutazione finora
- HipertiroidDocumento31 pagineHipertiroidEdo Pramana PutraNessuna valutazione finora
- Nursing JournalDocumento10 pagineNursing JournalRenee Dwi Permata MessakaraengNessuna valutazione finora
- Medical Examination Form For Police ApplicantsDocumento2 pagineMedical Examination Form For Police ApplicantsElite Mission HospitalNessuna valutazione finora
- Sensory DisturbancesDocumento155 pagineSensory DisturbancesCharles Okoh100% (1)
- Robbins Chapter 11Documento5 pagineRobbins Chapter 11Luming LiNessuna valutazione finora
- MCQs On Inborn Errors of MetabolismDocumento6 pagineMCQs On Inborn Errors of MetabolismNOOR100% (2)
- Tests Module 2Documento59 pagineTests Module 2Haruna Bzaki100% (1)
- PediatricDocumento55 paginePediatricJade Q Osit100% (6)
- KDIGO GD Membranous NephropathyDocumento1 paginaKDIGO GD Membranous NephropathyF AudreyNessuna valutazione finora
- Radiology MCQSDocumento23 pagineRadiology MCQSHabib Mughal67% (3)
- Coronary Artery DiseaseDocumento38 pagineCoronary Artery Diseaseshaitabligan100% (2)
- Granulomatosis With PolyangiitisDocumento9 pagineGranulomatosis With PolyangiitisGean RamosNessuna valutazione finora