Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
New Oral Anticoagulants For Stroke Prevention in Atrial Fibrillation
Caricato da
mngalaxyTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
New Oral Anticoagulants For Stroke Prevention in Atrial Fibrillation
Caricato da
mngalaxyCopyright:
Formati disponibili
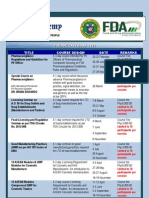
INFOGRAPHIC
INFOGRAPHIC
SLOW RISE OF NOACs
NEW ORAL ANTICOAGULANTS FOR STROKE
PREVENTION IN ATRIAL FIBRILLATION
Warfarin usage in 2015: 11,551,000
Prescription items dispensed in the community in England. Edoxaban was approved in 2015.
Rivaroxaban
Dabigatran
Apixaban
1,538,000
The National Institute for Health and Care Excellence recommends NOACs as an option for
non-valvular AF after a discussion about the risks and benefits compared with warfarin
1,000,000
European Society of Cardiology guidance recommends that
NOACs are broadly preferable to warfarin for non-valvular AF
Around 12,500 strokes are caused by atrial fibrillation (AF) in the UK each year,
and 7,100 of these are preventable with appropriate anticoagulation. Four new oral
anticoagulants (NOACs) are now available in the UK in addition to warfarin.
667,000
500,000
366,000
2012
2013
2014
2015
ANTICOAGULANT EFFECT OF NOACs
The coagulation cascade is a series of reactions involving coagulation factors that ultimately results in the formation of a blood clot. The
NOACs directly inhibit one specific coagulation factor in the cascade, whereas warfarin prevents the coagulation process by suppressing
the synthesis of several vitamin K-dependent coagulation factors.
INTRINSIC (CONTACT ACTIVATION) PATHWAY
EXTRINSIC (TISSUE FACTOR) PATHWAY
Activated by contact of the vessel wall with
lipoprotein particles or bacteria
Activated in response to tissue injury
Factors IX
Factors XI, XII
Factor VII
Factor X
Factor Xa
RIVAROXABAN
EDOXABAN
Thrombin (Factor IIa)
WARFARIN
Fibrinogen
(Factor I)
Usual dose: 110mg od. Bioavailability: 99%.
Peak plasma level: 7296 hrs. Half-life: 2060 hrs.
Renal excretion: <1%. Liver metabolism: yes.
Drug-drug and drug-food interactions: numerous.
THE PHARMACEUTICAL JOURNAL
VOL 297
NO 7893
1.60%
DABIGATRAN
Fibrin
(Factor Ia)
RATE OF PRIMARY
OUTCOME/YEAR:
1.18%
1.50%
THE NOACs
All NOACs are indicated for the prevention of stroke and systemic embolism in adults with nonvalvular AF who have one or more risk factors, such as
prior stroke or transient ischaemic attack; age 75 years; hypertension; diabetes mellitus and symptomatic heart failure. Unlike warfarin, the NOACs
have a predictable therapeutic response, rapid onset of action, few drug interactions and no requirement for regular coagulation monitoring.
DABIGATRAN ETEXILATE
(PRADAXA; BOEHRINGER INGELHEIM)
Usual dose: 20mg od with food. Bioavailability:
66% (without food), almost 100% (with food). Peak
plasma level: 24 hrs. Half-life: 59 hrs (young), 1113 hrs
(elderly). Renal excretion: 35%. Liver metabolism: yes.
Usual dose: 150mg bid. Bioavailability: 37%.
Peak plasma level: 2hrs. Half-life: 1217hrs.
Renal excretion: 80%. Liver metabolism: no.
Interactions: Use with strong inhibitors of both CYP3A4 and
P-gp, such as azole-antimycotics or HIV protease inhibitors, is
not recommended. Co-administration with dronedarone and
strong CYP3A4 inducers should be avoided.
Interactions: Use with strong P-gp inhibitors ketoconazole,
cyclosporine, itraconazole and dronedarone is contraindicated.
Use with P-gp inhibitor verapamil requires dose reduction.
Use with P-gp inducers should be avoided.
APIXABAN
(ELIQUIS; BRISTOL-MYERS SQUIBB-PFIZER)
EDOXABAN (LIXIANA; DAIICHI SANKYO UK)
Usual dose: 5mg bid. Bioavailability: 50%.
Peak plasma level: 14 hrs. Half-life: 12 hrs.
Renal excretion: 27%. Liver metabolism: yes.
Interactions: Use with strong inhibitors of CYP3A4 or
P-glycoprotein (P-gp) is not recommended. Use with
strong inducers of CYP3A4 and P-gp requires caution.
Usual dose: 60 mg od. Bioavailability: 62%. Peak
plasma level: 12 hrs. Half-life: 1014 hrs. Renal
excretion: 50%. Liver metabolism: minimal.
Interactions: Use with the P-gp inhibitors ciclosporin,
dronedarone, erythromycin or ketoconazole requires
dose reduction to 30mg once daily. Use with caution
concomitantly with P-gp inducers (e.g. rifampicin).
DECIDING WHICH NOAC
Several patient characteristics may be considered when deciding on which NOAC to recommend. Patient preference for once daily dosing may also
be taken into account. CAD: coronary artery disease, MI: myocardial infarction, ACS: acute coronary syndrome.
Sources: Slow rise of NOACs NHS Digital; European Heart Journal; NICE; Timeline New England Journal of Medicine;
The NOACs Europace; Summaries of product characteristics; Deciding which NOAC Arrhythmia & Electrophysiology Review.
Editorial adviser: Satinder Bhandal, consultant anticoagulation pharmacist, Buckinghamshire Hospitals Trust
Infographic: MAG
152
1.27%
2015
ENGAGE-AF is published in NEJM
showing edoxaban is noninferior to
warfarin with respect to the prevention
of stroke or systemic embolism and is
associated with significantly lower rates
of bleeding and death from cardiovascular
causes. GI bleeding increased with the
60mg dose of edoxaban.
RATE OF PRIMARY
OUTCOME/YEAR:
APIXABAN
WARFARIN
Prothrombin (Factor II)
2014
RIVAROXABAN (XARELTO; BAYER)
Tissue factor
Factor X
2013
ARISTOTLE trial is published in
NEJM showing apixaban is superior to
warfarin in preventing stroke or systemic
embolism in patients with AF and results
in lower mortality. Patients treated
with apixaban had significantly fewer
intracranial bleeds, but GI bleedings
were similar between both groups.
Idarucizumab (Praxbind), an
antidote to dabigatran
EDOXABAN
Edoxaban
2.4%
2.1%
APIXABAN
Warfarin
RATE OF PRIMARY
OUTCOME/YEAR:
Warfarin
1.69%
1.11%
2012
ROCKET AF trial is published in NEJM
showing rivaroxaban is non-inferior to
warfarin for the prevention of stroke or
systemic embolism, with no differences
in the risk of major bleeding, although
intracranial and fatal bleeding occurred
less frequently in the rivaroxaban group.
GI bleeding was greater with rivaroxaban.
RATE OF PRIMARY
OUTCOME/YEAR:
Warfarin
RE-LY trial is published in NEJM
showing that dabigatran 150mg
BID is superior to warfarin for
prevention of stroke and systemic
embolism, with no significant
differences in major bleeding,
although gastrointestinal (GI)
bleeding was higher.
2011
Rivaroxaban
2010
Dabigatran
APPROVAL IN EU
DRUG TRIALS &
RATE OF STROKE
OR SYSTEMIC
EMBOLISM
(PRIMARY
OUTCOME)
RIVAROXABAN
Apixaban
DABIGATRAN
Warfarin
2011
DAWN CONNELLY
2009
1,500,000
SEPTEMBER 2016
Cross-linked
Fibrin clot
PREVIOUS, OR HIGH RISK OF,
GI BLEED
HIGH ISCHAEMIC STROKE RISK, LOW
BLEEDING RISK
CAD, PREVIOUS MI OR HIGH RISK
FOR ACS/MI
SEPTEMBER 2016
RENAL
IMPAIRMENT
NO 7893
VOL 297
DIARRHOEA
DISORDERS
THE PHARMACEUTICAL JOURNAL
153
Potrebbero piacerti anche
- StrokeDocumento22 pagineStrokeAlex GasnasNessuna valutazione finora
- Heart FailureDocumento48 pagineHeart Failurecoollist33100% (1)
- Diuretic Treatment in Heart FailureDocumento12 pagineDiuretic Treatment in Heart FailureRoberto López Mata100% (1)
- Risala Fi Usul Ač-Fiqh by ShafiiDocumento393 pagineRisala Fi Usul Ač-Fiqh by ShafiiFahimNessuna valutazione finora
- Understanding Non-Hodgkins Lymphoma: Classification, Risk Factors, PresentationDocumento95 pagineUnderstanding Non-Hodgkins Lymphoma: Classification, Risk Factors, PresentationwihelminaNessuna valutazione finora
- Imaging Cardiac AmyloidosisDocumento16 pagineImaging Cardiac Amyloidosiskromatin9462Nessuna valutazione finora
- Fibrilación RevistaDocumento7 pagineFibrilación RevistaMishell Madisson Lino TolentinoNessuna valutazione finora
- Ecr 12 1 40Documento6 pagineEcr 12 1 40Ahmed MohammedNessuna valutazione finora
- Pos NoacDocumento40 paginePos NoacSanjeev Harry Budhooram100% (1)
- Stroke (Drug Research)Documento84 pagineStroke (Drug Research)Caren ChanNessuna valutazione finora
- Unanswered Questions During The Live EventDocumento9 pagineUnanswered Questions During The Live Eventyash_acharya007Nessuna valutazione finora
- Actualizacion Sobre El Uso de Los Nuevos Anticoagulantes OralesDocumento11 pagineActualizacion Sobre El Uso de Los Nuevos Anticoagulantes Oralesjdelta28Nessuna valutazione finora
- Noac Prescribing Tips For NoacsDocumento4 pagineNoac Prescribing Tips For NoacsBudiono WijayaNessuna valutazione finora
- Vorapaxar: General InformationDocumento21 pagineVorapaxar: General InformationIoana GhirvuNessuna valutazione finora
- VorapaxarDocumento21 pagineVorapaxarIoana GhirvuNessuna valutazione finora
- Management of Atrial Fibrillation CNA 2015Documento14 pagineManagement of Atrial Fibrillation CNA 2015isaNessuna valutazione finora
- EnalaprilDocumento32 pagineEnalaprilYeyenJaejoongNessuna valutazione finora
- ARNI Evidence and Perspectives in Cardiovascular DiseaseDocumento12 pagineARNI Evidence and Perspectives in Cardiovascular Diseasefazlur risyad laochiNessuna valutazione finora
- IvabradineDocumento4 pagineIvabradineLamy SNessuna valutazione finora
- Anticoag 2015november FullDocumento14 pagineAnticoag 2015november FullRosanna FiorilloNessuna valutazione finora
- Verapamil PDFDocumento13 pagineVerapamil PDFddandan_2Nessuna valutazione finora
- Apixaban in Patients With Atrial FibrillationDocumento12 pagineApixaban in Patients With Atrial FibrillationthedancingseaNessuna valutazione finora
- ASRA Guidelines on Neuraxial Blockade and AnticoagulantsDocumento66 pagineASRA Guidelines on Neuraxial Blockade and AnticoagulantsAshiyan IrfanNessuna valutazione finora
- Aspectos Prácticos Nuevos Anticoagulantes Am Jour Hem 2011Documento5 pagineAspectos Prácticos Nuevos Anticoagulantes Am Jour Hem 2011jose_esteban_pena_duranNessuna valutazione finora
- Cards JC - Association of Rivaroxaban Vs Apixaban With Major Ischemic or Hemorrhagic Events in Patients With Atrial FibrillationDocumento18 pagineCards JC - Association of Rivaroxaban Vs Apixaban With Major Ischemic or Hemorrhagic Events in Patients With Atrial Fibrillationapi-602288180Nessuna valutazione finora
- Atrial Fibrillation 2022Documento29 pagineAtrial Fibrillation 2022daniel mitikuNessuna valutazione finora
- HypertensionDocumento12 pagineHypertensionAhmedNessuna valutazione finora
- List of Anticoagulants GuideDocumento4 pagineList of Anticoagulants GuideMalem NganbaNessuna valutazione finora
- Case 1 & 2Documento4 pagineCase 1 & 2Adeel ShahidNessuna valutazione finora
- CPG3 Secondary Stroke PreventionDocumento10 pagineCPG3 Secondary Stroke Preventionmochamad rizaNessuna valutazione finora
- 309 Novel Anti-Platelet Agents and AnticoagulantsDocumento13 pagine309 Novel Anti-Platelet Agents and AnticoagulantsPhani NadellaNessuna valutazione finora
- Aliskiren, Enalapril, or Aliskiren and Enalapril in Heart FailureDocumento12 pagineAliskiren, Enalapril, or Aliskiren and Enalapril in Heart FailureRoberto López MataNessuna valutazione finora
- Amlodipine - Drug Information - UpToDateDocumento9 pagineAmlodipine - Drug Information - UpToDateBárbaraNessuna valutazione finora
- Antagonist Oral AnticoagulantsDocumento66 pagineAntagonist Oral Anticoagulantsbagheera316Nessuna valutazione finora
- 19BCPDocumento64 pagine19BCPNinna Isabel VictorioNessuna valutazione finora
- 21 9 1034Documento6 pagine21 9 1034Marcela MurafaNessuna valutazione finora
- Pharmacologic Treatment For Cardiac Failure: ACE InhibitorsDocumento36 paginePharmacologic Treatment For Cardiac Failure: ACE InhibitorsGleden UmayamNessuna valutazione finora
- Acitrom - The No.1 Oral AnticoagulantDocumento31 pagineAcitrom - The No.1 Oral AnticoagulantNishant SagarNessuna valutazione finora
- Neuraxial Blockade and AnticoagulantsDocumento69 pagineNeuraxial Blockade and Anticoagulantskamel6Nessuna valutazione finora
- Arixtra: (Fondaparinux Sodium) InjectionDocumento26 pagineArixtra: (Fondaparinux Sodium) InjectionTri Purma SariNessuna valutazione finora
- Arfarin: Arget UdienceDocumento4 pagineArfarin: Arget UdienceMano cempakaNessuna valutazione finora
- JAH3 11 E025723Documento36 pagineJAH3 11 E025723ResidenPatKlin Juli2022Nessuna valutazione finora
- Ran Ola ZineDocumento20 pagineRan Ola ZineHamza AlmaqtriNessuna valutazione finora
- QuinaprilDocumento30 pagineQuinaprilYeyenJaejoongNessuna valutazione finora
- Fondaparinux in Acute Coronary Syndromes CA5068 Admin OnlyDocumento9 pagineFondaparinux in Acute Coronary Syndromes CA5068 Admin OnlynaeamzNessuna valutazione finora
- 1000 - Johnson Venous ThrombDocumento33 pagine1000 - Johnson Venous ThrombAlejandro Kanito Alvarez SNessuna valutazione finora
- Clinical Review: Evidence Based Case ReportDocumento4 pagineClinical Review: Evidence Based Case ReportFranz Bruno Bailey RojasNessuna valutazione finora
- AWMSG advice on oral anticoagulation for NVAFDocumento10 pagineAWMSG advice on oral anticoagulation for NVAFAna MariaNessuna valutazione finora
- ClexaneDocumento19 pagineClexaneahmadNessuna valutazione finora
- Nigeria CME - Optimal - Care - For - Dvt-Pe - PatientsDocumento48 pagineNigeria CME - Optimal - Care - For - Dvt-Pe - PatientsStella CooKeyNessuna valutazione finora
- AtrijalnafibrilacijaDocumento2 pagineAtrijalnafibrilacijaGordana Blagić SavinNessuna valutazione finora
- Genetic Implications Pregnancy CategoryDocumento4 pagineGenetic Implications Pregnancy CategoryElizabeth LevitskyNessuna valutazione finora
- AnticoagulantsDocumento3 pagineAnticoagulantsKarthik SubramaniamNessuna valutazione finora
- Description: EnalaprilatDocumento17 pagineDescription: EnalaprilatYeyenJaejoongNessuna valutazione finora
- Cardio Lab MedsDocumento11 pagineCardio Lab MedsDianne Erika MeguinesNessuna valutazione finora
- PIIS1053077018310437Documento5 paginePIIS1053077018310437andi rahmatNessuna valutazione finora
- Contraindications To Thrombolytic Therapy: Aminocaproic AcidDocumento3 pagineContraindications To Thrombolytic Therapy: Aminocaproic AcidTia Siti RoilaNessuna valutazione finora
- Prehospital and Emergency Department Care of Atrial FibrillationDocumento8 paginePrehospital and Emergency Department Care of Atrial FibrillationindahkurNessuna valutazione finora
- Antiplatelet Therapy: New Antiplatelet Drugs in PerspectiveDocumento4 pagineAntiplatelet Therapy: New Antiplatelet Drugs in Perspectivegeo_mmsNessuna valutazione finora
- Celecoxib by RP-HPLCDocumento23 pagineCelecoxib by RP-HPLCNarongchai PongpanNessuna valutazione finora
- Pharmaceutical Sales Executive Consultant in Sarasota FL Resume Gail BoyerDocumento2 paginePharmaceutical Sales Executive Consultant in Sarasota FL Resume Gail BoyerGailBoyerNessuna valutazione finora
- Edoc - Pub db-4Documento4 pagineEdoc - Pub db-4info for businessNessuna valutazione finora
- Aloe Induced Toxicity Phytochemistry and Pharmacodynamics, Toxicokinetics and Case StudyDocumento7 pagineAloe Induced Toxicity Phytochemistry and Pharmacodynamics, Toxicokinetics and Case StudyVidyavardhini UshirNessuna valutazione finora
- Marketing Data - UncheckedDocumento30 pagineMarketing Data - UncheckedJasmeet SinghNessuna valutazione finora
- Clarithromycin - Drug Information - UpToDate PDFDocumento56 pagineClarithromycin - Drug Information - UpToDate PDFNaztasia 'ola' Flowerin BNessuna valutazione finora
- Iodine Clock Reaction LabDocumento3 pagineIodine Clock Reaction LabKar YanNessuna valutazione finora
- Fermentation Industries GuideDocumento11 pagineFermentation Industries GuidemichsantosNessuna valutazione finora
- Phytochemical Methods: Lecture Notes IDocumento8 paginePhytochemical Methods: Lecture Notes Irvraman3100% (2)
- Risk and Return Analysis of Pharmaceutical Industry in Capital MarketsDocumento13 pagineRisk and Return Analysis of Pharmaceutical Industry in Capital MarketssoumithrasasiNessuna valutazione finora
- 2022 - July - 25 - Drug Price Reference IndexDocumento45 pagine2022 - July - 25 - Drug Price Reference Indexkhara teanoNessuna valutazione finora
- Distortion of Generic and Patent Medicine in ConsuDocumento4 pagineDistortion of Generic and Patent Medicine in ConsulithasyamadlyNessuna valutazione finora
- OBAT YANG MENDEKATI EXPIRE DATE 2021Documento2 pagineOBAT YANG MENDEKATI EXPIRE DATE 2021vicki yugasworoNessuna valutazione finora
- 2012 Guide To Vermonts Prescribed Products Gift Ban and Disclosure LawDocumento40 pagine2012 Guide To Vermonts Prescribed Products Gift Ban and Disclosure LawIpey1986Nessuna valutazione finora
- Agen 53 BilastineDocumento19 pagineAgen 53 BilastineHyderNessuna valutazione finora
- Simple method to detect antibiotic resistance phenotypes in Pseudomonas aeruginosaDocumento15 pagineSimple method to detect antibiotic resistance phenotypes in Pseudomonas aeruginosaMari FereNessuna valutazione finora
- Antipsychotic Drugs - Wafa Bin ShamlanDocumento8 pagineAntipsychotic Drugs - Wafa Bin ShamlanSara AbdoNessuna valutazione finora
- FDA Academy Course Calendar 2013Documento4 pagineFDA Academy Course Calendar 2013Johnny ManahanNessuna valutazione finora
- Approved Price List of Medicine2007-08 (1) 07!09!07Documento10 pagineApproved Price List of Medicine2007-08 (1) 07!09!07Anonymous m65TTcfOTNessuna valutazione finora
- Coumadin WarfarinDocumento1 paginaCoumadin WarfarinSheri490100% (1)
- Prince ReportDocumento28 paginePrince ReportKevin RanpariaNessuna valutazione finora
- CelluliteDocumento8 pagineCelluliteAdityaNessuna valutazione finora
- Antibacterial Activity of Leaves of Lagerstroemia Speciosa (L) PersDocumento2 pagineAntibacterial Activity of Leaves of Lagerstroemia Speciosa (L) PersMark Nel NuñezNessuna valutazione finora
- Antiseptics&Disinfectants PDFDocumento33 pagineAntiseptics&Disinfectants PDFana_mondekarNessuna valutazione finora
- Benzo Thio PheneDocumento12 pagineBenzo Thio PhenevivekanandtNessuna valutazione finora
- HPTLC method for determination of plumbagin in Plumbago zeylanica Linn. rootDocumento5 pagineHPTLC method for determination of plumbagin in Plumbago zeylanica Linn. rootrajrudrapaaNessuna valutazione finora
- International Journal of Gynecology and ObstetricsDocumento5 pagineInternational Journal of Gynecology and ObstetricsLilian Rahma AnandaNessuna valutazione finora
- Seminar On Protein and Peptides Drug DeliveryDocumento37 pagineSeminar On Protein and Peptides Drug DeliverykeyurNessuna valutazione finora
- 13 Juli 21 SD BatubulanDocumento126 pagine13 Juli 21 SD Batubulanni ketut martiniNessuna valutazione finora
- Name of Sleeping Pill in Bangladesh - Google Search PDFDocumento1 paginaName of Sleeping Pill in Bangladesh - Google Search PDFPrati ShahanazNessuna valutazione finora