Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Limitations of Autograft and Allograft New Synthetic Solutions PDF
Caricato da
Santiago VázquezTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Limitations of Autograft and Allograft New Synthetic Solutions PDF
Caricato da
Santiago VázquezCopyright:
Formati disponibili
FEATURE ARTICLE
Limitations of Autograft and Allograft:
New Synthetic Solutions
Randal R. Betz, MD
Abstract
Autogenous cancellous bone is widely regarded as an
ideal construct for graft procedures, supplying osteoinductive growth factors, osteogenic cells, and a structural scaffold. However, procurement morbidity and constraints on obtainable quantities limit its use. Allograft is
the next best alternative at present; however, minor
immunogenic rejection and risk of disease transmission
Bone is the most common tissue for
transplant procedures, second only to
blood. More than 2.2 million bone
grafts worldwide and 450,000 in the
United States are performed each year.1
Autogenous bone has been the implant
of choice for most of these procedures;
in the United States, autogenous bone
was used in approximately 60% of bone
grafts in 1996, compared with 34%
allograft and 7% other materials.2
Autologous bone supplies the scaffold
(bone mineral and collagen) for osteoconduction, growth factors (noncollagenous bone matrix proteins) for
osteoinduction, and progenitor stem
cells for osteogenesis. The iliac crest is
chosen most frequently as the donor tissue site because of the quality and volume of bone available. However, procurement difficulties arise as a result of
lengthened surgery with a second
From Shriners Hospital for Children,
Philadelphia, Pa.
are unresolved issues. Although synthetic grafting materials eliminate these risks, these materials do not transfer
osteoinductive or osteogenic elements to the host site.
To offer the advantages of autograft and allograft, a
composite graft may be considered. Such a graft can
combine a synthetic scaffold with biologic elements to
stimulate cell infiltration and new bone formation.
operative incision, limited supply of
bone, and iatrogenic complications secondary to graft procurement.3
Allograft, the most common alternative to autograft, carries a finite risk of
transferring contaminants, toxins, or
infection from the donor. The processing of allograft tissue lowers this risk
but, unfortunately, can substantially
degrade the biologic and mechanical
properties initially present in the donated tissue. An ample supply is not
assured; processed and banked donor
bone is not always available at the time
of surgery.4,5
Great strides have been made with
synthetic alternatives over the past
decade. These materials may soon provide results comparable to or even superior to autograft (Table). Until recently,
synthetics had been viewed less favorably than autograft and allograft; only
10% of bone graft procedures worldwide have relied on synthetic materials,
including ceramics and polymers.1
Specific disadvantages encountered
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
with such materials in clinical settings
have included low or unpredictable
resorbability, difficulty in handling
(coral-derived hydroxyapatite [HA]),6
and poor clinical results with occasional inflammatory foreign body reaction
(degradable polymers).7,8 These complications can be surmounted with
newer, modified materials, such as specialty ceramics. One of the most
promising emerging surgical options
may be the use of a composite graft that
contains osteogenic cells and osteoinductive growth factors along with a
synthetic osteoconductive matrix.
Composite materials being tested in
preclinical and clinical trials may
demonstrate equivalent or superior
functionality to autograft and allograft.
GRAFT MATERIALS
Autograft
Using autologous bone graft bypasses potential complications of host rejection or disease transfer. The autograft
brings with it an osteoconductive
s561
www.orthobluejournal.com
ORTHOPEDICS
MAY 2002 VOL 25 NO 5/SUPPLEMENT
TABLE
Comparison of Bone Graft Materials
Graft
Autograft
Allograft
Properties
Osteogenic, osteoinductive,
osteoconductive
Osteoconductive, weakly
osteoinductive
Ceramics (TCP, Osteoconductive
hydroxyapatite)
Injectable cerOsteoconductive
amic cements
-TCP/BMA
Osteogenic, osteoinductive,
composite
osteoconductive
DBM
Osteoconductive, osteoinductive
Collagen
Good delivery vehicle for
other synthetic graft
materials
Advantages
No host rejection; no disease transmission;
retains viable osteoblasts
Greater availability of banked bone than
autograft; customized forms available;
no additional surgical procedure needed
Limitless availability; no additional surgical
procedure needed
Limitless supply, injectable, biocompatible,
some initial structural support
Limitless supply, biocompatible; can be
manipulated during placement
Ease of use; no additional surgical
procedure needed
Structure provides a favorable milieu to
bone regeneration
Disadvantages
Procurement morbidity, limited
availability; high cost
Immunogenic, disease transfer risk, not
osteogenic; variable clinical results;
expensive
Not osteogenic or osteoinductive, little
initial structural support
Not osteogenic or osteoinductive,
expensive, lack of placement control
Expense reflects R&D, commercialization costs
No structural support, not osteogenic
Minimal structural support, potentially
immunogenic
Abbreviations: -TCP5 -tricalcium phosphate, BMA5 bone marrow aspirate, DBM5 demineralized bone matrix, and R&D5 research and
development.
matrix of cartilage, minerals and matrix
proteins, osteoinductive proteins, and
osteogenic bone and marrow cells.9 As
a result, high success rates are achieved
with certain graft procedures (Table).
In spinal segment fusion, for example,
autogenous graft in posterior cervical
and lumbar procedures produces union
in > 90% of cases.10 Successful incorporation and union, however, depend
highly on the graft location and technique. For example, posterolateral lumbar fusion, the most common spinal
arthrodesis procedure, shows failure
(nonunion) in 5%-44% of surgeries in
which autografts are used.10
The theoretical potential of autograft does not always translate into successful outcomes in clinical practice.
Although bone harvested from the
patient's iliac crest or rib transfers
osteogenic precursor cells, its
osteogenic capability is rapidly depleted; most of the cellular (osteogenic)
components do not survive the transplant.10
Often, the supply of autogenous
bone is not sufficient given the patient's
overall physical condition or the indication for surgery. Autogenous bone
graft may not be feasible in the elderly,
in small pediatric patients, or in
patients with metastatic disease. The
treatment of spinal deformity in adults
or neuromuscular scoliosis in children
can require a relatively large autograft.11 This may be impractical if it
leads to iliac crest weakening to the
point of precluding its later use for fixation points in spinal instrumentation.
The volume of iliac crest is usually
inadequate in cases of congenital scoliosis and neurofibromatosis. In cases of
paralytic scoliosis and pelvic obliquity,
posterior spinal fusion commonly
involves additional instrumentation to
the pelvis, thus precluding harvest from
the posterior ilium.11,12 Additionally
compromised pulmonary function, as
is frequently seen in these patients,
would bar retrieval of bone from the
posterior rib cage.12,13 Atrophic osteoporotic pelvic bone, as accompanies
paralytic scoliosis or progressive scoliosis secondary to cerebral palsy, compounds the difficulty in retrieving bone
stock.14,15 Insufficient autogenous bone
in a graft procedure may be a cause of
subsequent failure to fuse.14 When
long, multisegmental spinal fusions or
revisions for fracture repair are
required, retrieving adequate bone subsequent to previous harvests may not
be possible.
When the quality and quantity of a
patient's bone stock make harvesting of
an autograft possible, the surgical procedure presents risks of significant
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
complications. These risks include hernia formation, blood loss, nerve injury,
postoperative infection, hematoma formation, and chronic pain at the donor
site.9,16 In a study of 214 children, the
incidence of perioperative complications was 2%. However, when interviewed, 24% of patients reported pain
at the donor site and 15% had complications that affected daily living activities.17 Seiler and Johnson18 identified
the reported risks of bone donor site
surgeries: arterial injury, ureteral
injury, herniation, chronic pain, nerve
injury, infection, fracture, pelvic instability, cosmetic defects, hematoma, and
tumor transplantation. Chronic pain
has been attributed to heterotopic bone
formation.19 Improved surgical techniques, such as limiting subcutaneous
dissection and providing layered tension-free incision closures, have been
suggested as a means of reducing some
complications.20
Allograft
Bone obtained from a donor is the
most frequently chosen substitute for
autogenous bone and is used to either
replace or extend its volume. Procedures
with allograft increased 14-fold between
1985 and 1996 and recently account for
approximately one-third of bone grafts
performed in the United States.2
s562
www.orthobluejournal.com
BETZ
The increased availability of
banked, donated bone tissue relative to
the supply of the patient's own bone has
made possible the manufacture and
fabrication of customized forms, such
as dowels, strips, and chips, made from
allograft tissue. Some of these
machine-structured allograft forms,
such as threaded bone dowels, can
serve dually as fixation devices and
delivery systems for bioactive agents.10
Including allograft as a bone filler
can provide early structural support
without procurement site morbidity
and is associated with a 60%-90%
overall success rate for large segmental
replacements (Table).21 The best allograft results may be obtained in the
adolescent patient undergoing scoliosis
correction and fusion.10 Dodd et al22
assessed results in 40 patients with
idiopathic scoliosis treated with grafts
obtained from either femoral head allograft or iliac crest autograft. Rates of
successful union were equivalent
(100%) for the 2 groups. The allograft
group demonstrated a low rate of infection, less blood loss at surgery, and
reduced postoperative pain.
The primary drawbacks of allograft
include highly variable, less satisfactory clinical results compared with autograft, especially for posterior lumbar
spinal fusion,23 and the finite risk of
disease transfer and immunogenic
reaction.24 These outcomes may be
attributed in part to the preservation,
storage, and sterilization procedures
for banked allograft to lower the risk of
disease transmission and rejection but
which eliminate osteogenic cells and
weaken osteoinductive potential.
Processing and radiation also degrade
structural integrity, reducing mechanical strength up to 50%.10,25 Allograft is
more slowly incorporated than autograft and may require more hardware
protection.23,25
Other drawbacks related to procurement are expense, donor-to-donor variation in quality, and limited availability. The cost of allogenic bone for a
spine deformity procedure requiring
6 bottles of cancellous chips (30 cc per
LIMITATIONS
bottle) is $2100. Families of potential
donors harbor a fear of gross disfigurement that substantially curbs donation
of bone relative to tenders of solid
organs; tissue banks, therefore, experience difficulty with procurement.5,26
Processing of allogenic bone
reduces, but does not fully eliminate,
the risk of disease transfer and
immunogenicity. Contaminants or
pathologies that may be transferred
include viral (especially human
immunodeficiency virus [HIV] and
hepatitis B and C) and bacterial infection, malignancy, systemic disorders
(rheumatoid arthritis, autoimmune disease), or toxins. In a study of 1146
femoral heads removed from patients
with osteoarthritis who elected hip
arthroplasty, 8% of the femoral heads
showed evidence of diseases that were
unreported and undiagnosed at the time
of hip surgery and were not pathologically associated with osteoarthritis,
including occult malignant tumors. All
1146 bone specimens would have been
deemed suitable for allograft by existing criteria apart from their analysis for
this study.27 Even so, the risk of disease
transmission with bone is low, even
lower than that of blood.2 Risk of HIV
in properly screened allograft is estimated to be 1 in 1.6 million, compared
with 1 in 450,000 in blood.
Nevertheless, at least 4 cases of HIV
transmission by fresh-frozen allograft
have been documented.23
The US Food and Drug
Administration (FDA) has recently
expressed concern that musculoskeletal
tissue can contain prions implicated in
degenerative neurologic disease, and
that these prions may not be inactivated
by approved processing techniques.28
The potential for any allograft to
trigger an immune response is attributed to the major histocompatibilitycomplex antigens expressed in cellular
material composing the allograft and,
to a lesser extent, proteoglycans in the
ground substance. In addition to HLA
class I antigens expressed by the stromal cells of the graft, HLA class II
antigens are expressed by the
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
OF
ALLOGRAFT
AND
AUTOGRAFT
parenchymal osteoblasts.29 Immunogenic responses delay, in a dose-dependent manner, the development of a new
blood supply to the graft site, which, in
turn, retards the rate of new bone
growth and limits the long-term extent
of incorporation and bone remodeling.23 The ability to promote an
immune response is a function of allograft processing; more aggressive processing has been associated with less
frequent and less intense immunologic
responses. Fresh allografts are no
longer used clinically for this reason.
Frozen allografts induce stronger
immune responses than frozen, freezedried allografts.23 In a multicenter
study of 84 patients receiving massive
frozen allografts, 49 (58%) patients
were sensitized to class I antigens and
46 (55%) were sensitized to class II
antigens.30 Friedlaender et al21 concur
that long-term clinical outcome of allografts is improved when class II antigens are closely matched between
donors and recipients, but they comment that biologic consequences of
immunologic events remain speculative. In their series of 33 patients with
large segmental deficits of long bones
repaired with massive frozen allograft,
23 of 29 (79%) patients available for
long-term follow-up exhibited satisfactory outcomes.21 While noting encouraging results in this study of
unmatched grafts, Friedlaender et al21
also acknowledge that an understanding of immunologic responses associated with bone allografts provides opportunities to improve the predictability of
clinical outcomes.
Allografts are processed by 2 primary means, freezing and demineralizing.
Both processes ensure the death of host
cells. As reviewed by Burwell,31 death
occurs primarily at the time of harvesting bone, although some peripheral
cells may survive depending on the
extent of the blood supply. Freezing,
freeze-drying, and demineralizing
processes are severe enough to kill any
remaining cells.
Allografts may be fresh-frozen or
freeze-dried after at least one washing
s563
www.orthobluejournal.com
ORTHOPEDICS
with an antibiotic solution. Fresh allografts are no longer used because they
engender inflammatory responses,23 but
freezing fresh allografts at 70C after
an antibiotic wash reduces the immunogenicity. Freeze-dried (lyophilized)
allografts are washed in antibiotic
twice, frozen at 70C, and dried to
5 weight-percent water. These freshfrozen allografts are more osteoinductive and stronger than freeze-dried
grafts. Human immunodeficiency virus
has been transmitted in fresh-frozen
allograft, but not in freeze-dried bone.23
Freeze-dried allograft is the least
immunogenic but has inferior osteoinductive and mechanical properties and
mechanical strength. Further sterilization of freeze-dried bone by ethylene
oxide or gamma irradiation may also
diminish osteoinductive properties.10
Rehydration of freeze-dried bone can
result in longitudinal microscopic and
macroscopic cracks, which may
account for decreased graft strength of
up to 50%.10,25 The shelf-life of freshfrozen bone stored at 20C is 1 year,10
at 70C, the shelf-life is 5 years23; the
shelf-life of freeze-dried bone is
indefinite.23
No amount of allograft processing
will fully eliminate the possibility of an
immune response or disease transfer.
The enhanced safety of processing is
offset by reductions in the biologic and
mechanical function of grafts with
more unpredictable outcomes than the
autograft gold standard.
BIOMATERIALS
Demineralized Bone Matrix
Demineralized bone matrix (DBM)
is an osteoconductive scaffold that is
produced by acid extraction of banked
allograft bone. It provides no structural
strength and contains noncollagenous
proteins, osteoinductive growth factors,
and type I collagen.32 Demineralized
bone matrix has greater osteoinductive
potential than allograft due to enhanced
bioavailability of growth factors secondary to the demineralization
process.10,24 The efficacy of DBM in
promoting new bone formation
MAY 2002 VOL 25 NO 5/SUPPLEMENT
depends on a number of factors, such
as processing solutions, demineralization time, temperature extremes, DBM
particle size, and method of terminal
sterilization.2
Since the early 1990s, DBM products have been widely used in orthopedic surgery.10 The first commercially
available preparation was Grafton gel
(Osteotech Inc, Eatontown, NJ), consisting of DBM with a glycerol carrier;
Grafton is also currently supplied as a
malleable putty and as flexible strips. A
moldable bone paste (Opteform,
Medtronic Sofamor Danek, Memphis,
Tenn), containing cortical bone chips,
and an injectable bone paste (Osteofil,
Medtronic Sofamor Danek), formed
from demineralized powder, are recent,
commercially marketed alternatives.
Although prospective clinical studies
are underway, available data suggest a
role for DBM as a bone graft extender
rather than as a bone graft
substitute.10,33
Collagen
Collagen is the most abundant protein in the extracellular bone matrix.
The structure of collagen is conducive
to mineral deposition, vascular
ingrowth, and growth-factor binding,
providing both a physical and chemical
milieu favorable to bone regeneration.8
However, it provides little or no initial
structural support and has potential
immunogenicity. So far, studies have
demonstrated its primary use as a
delivery system for other osteoconductive, osteoinductive, or osteogenic factors with mixed clinical results.24
A composite of collagen gel with
granules of a biphasic ceramic of HA
and tricalcium phosphate (TCP) was
studied in a posterior segmental canine
spinal fusion model.34 The addition of
collagen-ceramic composite to autograft was actually inferior to using a
smaller volume of autograft alone.
However, Zerwekh et al35 used the
same collagen-ceramic composite in a
canine anterior spinal fusion model and
found it to be an effective autograft
extender. A prospective, randomized
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
clinical trial comparing autograft with
a composite of TCP and autogenous
marrow in the treatment of long bone
fractures found no significant difference with regard to rates of union or
functional measures.36
SYNTHETIC OPTIONS
Ceramics
Advantages. Synthetic ceramics
offer potentially limitless availability.
Alone, synthetic ceramics impart no
osteogenic or osteoinductive properties. Synthetic implants do not require a
second operative site, and there is no
risk of disease transmission or
immunogenic response. The 3-dimensional (3-D) structure is the critical
determinant of the speed of incorporation and remodeling; a more porous,
lower density construct provides
greater surface area exposure for supply of nutrients, vascularization, and
bony ingrowth. The osteoconductive
scaffold provides an appropriate environment in which bone cells and bone
morphogenetic proteins (BMPs) can
adhere and proliferate. Historically, the
materials used have been hydroxyapatite (Ca10[PO4]6[OH]2), one of the calcium phosphate stoichiometries, or
combinations of the two. Initially, the
newly placed ceramic lacks compressive and tensile strength. Subsequent to
incorporation and healing, the area of
the implant attains mechanical strength
similar to cancellous bone.37
Success with specific formulations
for treatment of spinal misalignment or
fracture repair has been reported. In a
prospective study of posterior spinal
fusion in adolescents with idiopathic
scoliosis, 341 patients were randomized to either autograft or synthetic
porous ceramic blocks (macroporous biphasic calcium phosphate
[MBCP]).38 Overall results were comparable between the 2 groups at
18 months postoperatively except for
increased wound complications in the
autograft group. In a prospective study
of 106 patients with degenerative spine
or spondylolisthesis undergoing lumbar spinal fusion, MBCP granules were
s564
www.orthobluejournal.com
BETZ
used with autogenous bone marrow and
bone chips.39 Fusion was achieved in
100 of the 106 patients, suggesting that
MBCP provides a suitable alternative
to autografting.
Disadvantages. The main disadvantage of using pure ceramic as a bone
graft substitute is the minimal immediate structural support. However, purely
cancellous (as opposed to corticocancellous) autograft or allograft also
delivers little in the way of early structural support. A second disadvantage is
the absence of osteoinductive or
osteogenic properties. Both of these
disadvantages may be addressed in
future composites of biologic and synthetic elements. A third disadvantage is
the potential expense reflecting
research and development costs for
synthetics; this, however, is offset by
the reduction of procurement costs
associated with autograft and allograft.
Rapidly Resorbing Ceramics.
Tricalcium phosphate constructs generally contain approximately 39% calcium and 20% phosphorus by weight,
similar to natural bone.40 Such constructs have been used safely as synthetic bone void fillers in dentistry and
orthopedics for decades.41,42 The construct's calcium phosphaterich surface
layers seem to enhance bonding with
adjacent host bone. This stimulates
osteoclastic resorption and osteoblastic
new bone formation within the
resorbed implant.8
Slowly
Resorbing
Ceramics.
Hydroxyapatite exhibits brittleness and
resorbs slowly; implants of this material can become a focus of mechanical
stress. It is often modified and combined with other materials for
improved functionality and faster
resorption. A pediatric study assessed
results for 12 patients with severe scoliosis who underwent internal fixation
and fusion with HA/TCP alone or combined with autogenous cancellous
bone.43 Successful fusion was achieved
for all patients treated with HA/TCP
alone or combined with autograft,
based on clinical and radiologic examination at follow-up averaging
LIMITATIONS
15 months. Another study by Bucholz
et al44 used either interporous HA or
cancellous autograft to fill metaphyseal
defects in 40 patients with displaced
tibial plateau fractures.44 They found
no radiologic or clinical difference
between the 2 groups at follow-up.
Injectable
Ceramic
Cements.
Injectable calcium phosphate (Norian
SRS, Norian Corp, Cupertino, Calif)
represents a class of ceramics that combines some of the qualities of a cement
with those of a bone void filler. Norian
cement contains -TCP mixed with calcium carbonate and monocalcium phosphate monohydrate. In its initial liquid
state, it can be injected by syringe into a
fracture site or bone defect via closed or
open techniques; it then hardens in vivo
without generating significant heat. The
initial compressive strength of the hardened material is similar to that of cancellous bone. The calcium phosphate
implant undergoes long-term remodeling, and is ultimately completely
replaced by host tissue.8 Vascular channel invasion, osteoclastic activity, and
new bone formed in direct contact with
the implant become visible within a few
weeks of implantation, with minimal
foreign body reaction.24 Injectable calcium phosphate shows promise for
treating distal radius fractures and as an
adjunct to treating femoral neck fractures, vertebral body compression fractures, and reinforcement of pedicle
screw fixation.24
In a prospective, randomized study
of 40 patients with redisplaced distal
radial fractures, Kopylov et al45 compared treatment with injectable calcium
phosphate bone cement (and 2 weeks
of cast immobilization) with external
fixation for 5 weeks. Functional outcome was identical except for more
rapid recovery of grip strength and
wrist mobility in the injected group,
presumably due to the shorter immobilization time. Another prospective, randomized study compared conservative
treatment (traction, 6 weeks of cast
immobilization) with calcium phosphate bone cement injection (and
2 weeks of cast immobilization) in
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
OF
ALLOGRAFT
AND
AUTOGRAFT
110 patients with distal radius fractures.46 At the 1-year follow-up, the
union rate was only 58% in patients
treated by immobilization alone, compared with 82% in those injected with
cement before immobilization. Patients
treated with injectable cement experienced less pain and earlier restoration
of movement and grip strength. The
material has also been successfully
used to augment hip fracture treatment
(52 femoral neck fractures and
39 intertrochanteric fractures).47
A potential drawback of the liquid
injectable cement is accidental
extraosseous extrusion. Difficulties in
controlling final placement may result
in soft-tissue or intra-articular
deposits.46
Ultraporous -TCP. A highly porous
-TCP bone void filler that is composed of 90% interconnected void
space with a broad range of pore sizes
(1-1000 m) has been developed to
mimic the trabecular structure of natural cancellous bone (Vitoss, Orthovita,
Malvern, Pa). Small pores allow the
wicking of phagocytic cells for resorption and bone-forming cells, nutrients,
and growth factors for bone recovery
through capillary refill. The larger size
pores encourage vascularization and
bone ingrowth.48 This ceramic construct includes pore sizes within the
optimum range for osteoconductivity,
150-500 m, as cited by Gazdag et al.37
The -TCP particles have an average
diameter of 100 nm, small enough for
osteoclastic digestion in the remodeling
phase. The material can be manipulated
during placement, sculpted as blocks,
or packed as morsels; after it is packed
to conform to the shape of the bone
defect, its high porosity remains intact.
Like all ceramic scaffolds, -TCP does
not possess intrinsic osteogenic or
osteoinductive properties.
A canine study was undertaken to
determine the rate of new bone
ingrowth into defect sites repaired with
-TCP and to measure the rate of
resorption of the -TCP scaffold.49,50
Cylindrical metaphyseal defects measuring 10 X 25 mm in canine humeri
s565
www.orthobluejournal.com
ORTHOPEDICS
MAY 2002 VOL 25 NO 5/SUPPLEMENT
metals, such as porous tantalum) offer
the potential for absolute control of the
final structure, no immunogenicity, and
excellent biocompatibility.8
BIOLOGIC/SYNTHETIC
COMPOSITE GRAFTS
Rationale
A composite graft combines an
osteoconductive matrix with bioactive
agents that provide osteoinductive and
osteogenic properties, potentially replicating autograft functionality. The
osteoconductive substrate becomes a
delivery system for bioactive agents,10
requiring less chemotaxis and less
migration of osteoblast progenitor cells
to the graft site. The direct infusion of
progenitor cells should lead to more
rapid and consistent bone recovery.
When an osteoconductive scaffold is
seeded with bone marrow aspirate
(BMA) or BMP, for example, the composite graft may become both
osteogenic and osteoinductive, providing a competitive alternative to autograft.
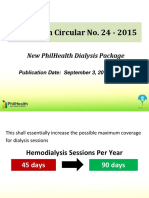
Figure: Radiograph of -tricalcium phosphate (-TCP) implants from 3-52 weeks.
were repaired with blocks of -TCP.
Specimens were examined up to 1 year
postimplantation, and bone ingrowth
and scaffold resorption were quantified
using standard histomorphometric
techniques. The -TCP scaffold
showed bone formation and resorption
as early as 3 weeks postimplantation.
By 6 weeks, the volume of new bone
formed throughout the implants
exceeded the volume of bone in areas
adjacent to the defects by approximately 20%. Bone density was in the normal range and the scaffold was almost
completely resorbed by the end of
12 weeks. By 24 weeks, the implant's
trabecular orientation and thickness
approximated that of adjacent bone.
The bone within the defects was virtually indistinguishable histologically
and radiographically from the surrounding bone at the 12-, 24-, and
52-week follow-ups (Figure).49,50
These findings were more encouraging than earlier histomorphometric
studies with traditional ceramics.51-53
Bruder et al52 found that a porous
ceramic composed of HA and conventional -TCP showed no change in its
structural geometry and essentially no
resorption over the first 16 weeks after
implantation. Delayed bone formation
was evident mostly at the periphery of
defects containing the ceramic
implants,51,52 in contrast to the pattern
of bone formation and resorption found
throughout the implants examined in
the canine ultraporous -TCP study
discussed in the previous paragraph.
The more uniform deposition of bone
in the ultraporous -TCP study may
have resulted from the greater interconnected microporosity of ultraporous
-TCP, which may accelerate remodeling by facilitating in-migration and
retention of osteogenic cells and
nutrients.
Nonbiologic Osteoconductive Substrates. Nonbiologic substrates (eg,
degradable polymers and fabricated
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
Potential Composites
Bone Marrow/Synthetic Composites.
Clinical experience with bone marrow
transplantation has established bone
marrow as a highly reliable source of
osteoblast progenitor cells.54 It is the
only source that does not require an
open surgical procedure or the additional time and cost of in vitro cell
growth.24 In addition, marrow cells
can be delivered percutaneously.55
Uncontrolled clinical studies suggest
that aspirated bone marrow autograft
may be of value in treating
nonunions,56,57 but no prospective trials
have studied isolated marrow grafts.58
Studies have looked at composites
of bone marrow and synthetics for bone
grafting with generally positive results.
In athymic mice, HA loaded with
human bone marrow cells placed subcutaneously showed an early bone
response.59 In rabbits, coralline HA
plus bone marrow was found to be an
unacceptable combination to achieve
lumbar spinal fusion.60 Solchaga et al61
s566
www.orthobluejournal.com
BETZ
attribute variable results with bone
marrow to the interindividual variability of rabbit specimens. In sheep, a
composite of a ceramic mixture of calcium phosphates and collagen mixed
with bone marrow achieved spinal
fusions of similar mechanical properties to autogenous corticocancellous
bone after 6 months.62 Hydroxyapatite
with bone marrow was comparable to
autograft in repairing 3-cm gaps in the
tibia of sheep,63 but composites of
resorbable calcium phosphates and
bone marrow were inadequate alternatives for autografts in the same model,
although the stimulatory effect of bone
marrow was noted.64
Some of these materials have been
investigated clinically. A composite of
a ceramic mixture of calcium phosphates and collagen mixed with bone
marrow and autogenous bone chips
available from the spine was used to
fuse lumbar vertebrae in a series of
106 patients, most (95/106) with
degenerative spine etiologies. After a
minimum follow-up period of 2 years,
100 of 106 patients achieved spinal
fusion. As degenerating spines are difficult to obtain arthrodesis, these
results were considered especially
encouraging.39
Ultraporous -TCP/BMA Composite.
The newer ultraporous version of TCP, Vitoss synthetic cancellous bone
void filler, may be well suited for use
with BMA in a composite graft. The
broad pore size range and interconnected
microporosity endow the scaffold with
favorable wicking and hydrophilic properties, encourage tissue ingrowth, and
allow percolation of body fluids that
facilitates the delivery of nutrients and
physical dissolution of the scaffold.
These attributes encourage retention of
both seeded marrow cells and growth
factors, as well as potentially greater
penetration of bone-forming cells,
phagocytic cells, growth factors, and
nutrients from adjacent bone.65
Osteoinductive Growth Factors and
Synthetic Composites. Bone morphogenetic proteins consist of a family of
at least 15 structurally related osteoin-
LIMITATIONS
ductive growth factors first identified in
1976 as the active osteoinductive fraction of DBM and characterized via
molecular cloning in 1988.32 Of the
BMPs, recombinant human bone morphogenetic protein-2 (rhBMP-2)
(Genetics Institute, Cambridge, Mass)
is closest to clinical application.
Osteoinductive growth factors other
than BMPs include transforming
growth factor (TGF), platelet-derived
growth factor (PDGF), insulin-like
growth factor (IGF), and fibroblast
growth factor (FGF).32 The role of
these other growth factors in fracture
repair is not yet fully defined.66
Histologic analyses of tissue
obtained from dental studies have confirmed new bone growing into defects
repaired with composites of absorbable
collagen sponge (ACS) and rhBMP-2.67
The safety and feasibility of the composite to augment local osseous defects
and preserve alveolar ridges after
extractions were shown in a 24-month
trial of 12 patients in 2 centers, although
some implant volume was lost from
week 4 to week 8.68 Biopsies taken
3 years posttreatment in a 12-patient
study showed normal bone formation in
extraction sites and alveolar ridges augmented with rhBMP-2/ACS.69
Feasibility studies and prospective
clinical trials have also begun to investigate orthopedic applications of
BMPs. BMP-7, also called recombinant human osteogenic protein-1
(rhOP-1), was used in a prospective,
randomized clinical trial of tibial
nonunions initiated in 1994.70
Multicenter clinical trials have begun
in the United States and abroad, and an
interim report on the use of rhBMP2/ACS in open tibial fractures became
available in 1999.71
In a prospective, randomized,
double-blind 24-patient trial, 5 of the
6 patients receiving rhOP-1 in a collagen carrier demonstrated new bone formation from 6 weeks onward in a critically sized fibular defect.72 In a 2-year
prospective, randomized, controlled
trial, 14 patients with lumbar degenerative disk disease received threaded
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
OF
ALLOGRAFT
AND
AUTOGRAFT
interbody fusion cages filled with
either rhBMP-2/collagen sponge or
autograft.73 At 6, 12, and 24 months,
fusions occurred in all 11 of the
rhBMP-2 patients compared to only
2 of 3 autograft patients. In addition,
patients in the rhBMP-2 group had
shorter hospital stays, most likely due
to the iliac crest procurement in the
autograft group. Because previous animal studies had shown that bone would
not spontaneously grow through collagen-filled cages alone, bone formation
was attributed to the presence of
rhBMP-2.
In a prospective, randomized, controlled, partially blinded, multicenter
24-month trial, 122 patients with
124 tibial nonunions were treated with
rhOP-1 in collagen or with autograft.74
Judging by clinical criteria 9 months
after surgery, 81% of nonunions treated
with rhOP-1/collagen fused versus
85% of nonunions treated with autograft (P= .52); by radiographic criteria,
corresponding rates of fusion were
75% and 84%, respectively (P= .22).
These initial results were continued
after 2 years with no difference in outcomes (P= .94). The incidence of
donor site pain was 20% in patients
receiving autogenous bone.
Luque compared the use of rhBMP2/biphasic-ceramic block composite
with autograft. During posterior transverse process spinal fusion in
7 patients, the BMP/ceramic composite
was implanted unilaterally, and the contralateral side was implanted with autograft. Preliminary results are similar
between the 2 groups.10 The implantation of rhBMP-2/ceramic bilaterally,
which would eliminate the need for
autograft, is being examined in the second phase of this study. Another
ongoing study will involve 45 patients undergoing anterior cervical
diskectomy and fusion with autograft.10
An rhBMP-2/collagen sponge construct
in various concentrations will be placed
to fill the iliac crest procurement defect
site. The future role of BMPs in orthopedic surgery should be better defined
by the results of these studies.
s567
www.orthobluejournal.com
ORTHOPEDICS
Growth factor enhancements can
now be prepared intraoperatively from
patients' blood. Proteins involved in
healing and reparative processes are
initially delivered to injury sites via
platelets and white blood cells, where
they are localized and concentrated by
clotting. One surgical aid, Autogenous
Growth Factors (Interpore Cross,
Irvine, Calif), collects and processes
the platelet- and leukocyte-rich buffy
coat at the time of need to form a gel
that stabilizes bone and graft fragments
and assists in their fixation. The gel
serves a dual function: it delivers and
localizes higher levels of proteins needed for repair and constrains graft elements to achieve incorporation. The
use of this type of gel to deliver exogenous osteoinductive growth factors also
appears attractive.75 A method has been
developed to separate platelet-rich
plasma
from
patients'
blood
(Symphony,
DePuy
AcroMed,
Raynham, Mass), which can then be
used to enhance allograft.
BMP/Polyglycolic Acid Polymer
Composites. Two of the broader categories of polymeric membranes that
have been investigated for use in bone
grafting procedures are polytetrafluoroethylene (PTFE) and the degradable poly--hydroxy acids (PHAs),
polylactic acid (PLA), and polyglycolic acid (PGA). Periodontal applications
of PTFE and rhBMP were reported and
reviewed in 199576; the combination of
PHAs and BMP were reviewed in
199677 with a more general and current
review of polymers and BMP following in 1999.78
Although degradable polymers have
little osteoconductive potential and are
associated with adverse foreign body
reactions,24 they are potentially versatile as growth factor delivery vehicles
with customized degradation rates and
3-D structure. Research in this area
remains active.
The addition of bovine-derived
BMP to both PTFE and degradable
membranes did not increase the rate of
healing of critical-sized defects in the
mandibles of rats, but rhBMP-2 accel-
MAY 2002 VOL 25 NO 5/SUPPLEMENT
erated healing when used with
PLA/PGA membranes.79 A porous
biodegradable copolymer, poly(D,L
[lactide-glycide]) (PLGA) was evaluated as a carrier for rhBMP-2 using a
canine posterior segmental spinal
fusion model.80 The rhBMP-2/PLGA
composite was compared with autogenous cancellous bone and with PLGA
alone. Union score and mechanical
testing showed no difference between
autogenous cancellous bone and
rhBMP-2/PLGA; both were superior to
PLGA alone.
BMA/BMP/Polyglycolic Acid Polymer Composite. Lane et al81 argues that
studies examining the use of either
osteoconductive matrices or osteogenic
BMA alone, or even in combination,
will be inferior to studies that include
an osteoinductive stimulant such as
BMP. A rat defect model showed the
apparent synergistic effect of osteoinductive rhBMP-2 combined with bone
marrow and a polylactic-glycolic acid
carrier, with results superior to that of
autogenous cancellous bone.
ADVANCEMENTS
The early concept of gene therapy
was described as the treatment of congenital diseases by transferring copies
of healthy DNA into cells with defective genes. The broader view now
includes the treatment and prevention
of congenital and acquired diseases by
transferring nucleic acid material
(DNA or RNA). This transfer can be
accomplished by direct (in vivo) application of DNA or RNA in vectors (generally, bacterial viruses are used) or by
an indirect (ex vivo) means whereby
nucleic acids are incorporated into cultured host cells out of the body and
then put back into the body.82
The use of gene therapy to repair
bone defects may have advantages over
the injection of an exogenous bolus of
osteoinductive BMPs. For example, the
use of a cellular delivery vehicle containing modified genetic material may
be more physiologic than an osteoconductive matrix, both in terms of timing
and concentration.
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
Several genes applicable to bone
repair have been successfully transferred. The gene coding for the expression of TGF-1 has been transferred
directly into the nucleus pulposus of
vertebral disks of rabbits, resulting in a
doubling of the synthesis of proteoglycans relative to control disks.83 Genes
from bovine intervertebral endplates
have been transferred indirectly, thus
suggesting novel ways of synthesizing
pharmacotherapies in situ.84 In addition, potential clinical treatments to
achieve spinal arthrodesis have been
attempted by transferring genes that
express the osteoinductive proteins
LMP-1 and BMP-2. A mixture of bone
marrow cells transfected with the
cDNA for an osteoinductive protein,
LMP-1, and devitalized bone matrix
has been used to fuse vertebrae in nude
rats,85 and an adenovirus containing the
gene for BMP-2 has been injected percutaneously along the spine at the lumbosacral junction in nude mice to produce ectopic new bone formation.
SUMMARY
Bone grafting is one of the most
common orthopedic procedures.86
Although autograft and banked allograft are used most frequently, synthetic composite bone substitutes that combine an osteoconductive matrix with
osteoinductive growth factors and
osteogenic cells may ultimately replace
them.
REFERENCES
1. Lewandrowski K, Gresser JD, Wise DL,
Trantolo DJ. Bioresorbable bone graft substitutes
of different osteoconductivities: a histologic evaluation of osteointegration of poly(propylene glycol-co-fumaric acid)-based cement implants in
rats. Biomaterials. 2000; 21:757-764.
2. Boyce T, Edwards J, Scarborough N.
Allograft bone: the influence of processing on
safety and performance. Orthop Clin North Am.
1999; 30:571-581.
3. Hu RW, Bohlman HH. Fracture at the iliac
bone graft harvest site after fusion of the spine.
Clin Orthop. 1994; 309:208-213.
4. Broom MJ, Banta JV, Renshaw TS. Spinal
fusion augmented by Luque-rod segmental
instrumentation for neuromuscular scoliosis. J
Bone Joint Surg Am. 1989; 71:32-44.
5. Henman P, Finlayson D. Ordering allograft by weight: suggestions for the efficient use
of frozen bone-graft for impaction grafting. J
s568
www.orthobluejournal.com
BETZ
Arthroplasty. 2000; 15:368-371.
6. Bucholz RW. Development and clinical
use of coral-derived hydroxyapatite bone graft
substitutes. In: Urist MR, O'Connor BT, Burwell
RG, eds. Bone Grafts, Derivatives and
Substitutes. Oxford: Butterworth-Heinemann
Ltd; 1994:260-270.
7. Bostman O, Pihlajamaki H. Clinical biocompatibility of biodegradable orthopaedic
implants for internal fixation: a review.
Biomaterials. 2000; 21:2615-2621.
8. Cornell CN. Osteoconductive materials
and their role as substitutes for autogenous bone
grafts. Orthop Clin North Am. 1999; 30:591-598.
9. Arrington ED, Smith WJ, Chambers HG,
Bucknell AL, Davino NA. Complications of iliac
crest bone graft harvesting. Clin Orthop. 1996;
329:300-309.
10. Sandhu HS, Grewal HS, Parvataneni H.
Bone grafting for spinal fusion. Orthop Clin
North Am. 1999; 30:685-698.
11. Gau YL, Lonstein JE, Winter RB, Koop S,
Denis F. Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis
and pelvic obliquity: a review of 68 patients. J
Spinal Disord. 1991; 4:399-410.
12. Bridwell KH, O'Brien MF, Lenke LG,
Baldus C, Blanke K. Posterior spinal fusion supplemented with only allograft bone in paralytic
scoliosis. Does it work? Spine. 1994; 19:26582666.
13. Yazici M, Asher MA. Freeze-dried allograft for posterior spinal fusion in patients with
neuromuscular spinal deformities. Spine. 1997;
22:1467-1471.
14. McCarthy RE, Peek RD, Morrissy RT,
Hough AJ Jr. Allograft bone in spinal fusion for
paralytic scoliosis. J Bone Joint Surg Am. 1986;
68:370-375.
15. Montgomery DM, Aronson DD, Lee CL,
LaMont RL. Posterior spinal fusion: allograft
versus autograft bone. J Spinal Disord. 1990;
3:370-375.
16. Summers BN, Eisenstein SM. Donor site
pain from the ilium: a complication of lumbar
spine fusion. J Bone Joint Surg Br. 1989; 71:677680.
17. Skaggs DL, Samuelson MA, Hale JM,
Kay RM, Tolo VT. Complications of posterior
iliac crest bone grafting in spine surgery in children. Spine. 2000; 25:2400-2402.
18. Seiler JG, Johnson J. Iliac crest autogenous bone grafting: donor site complications. J
South Orthop Assoc. 2000; 9:91-97.
19. Ross N, Tacconi L, Miles JB. Heterotopic
bone formation causing recurrent donor site pain
following iliac crest bone harvesting. Br J
Neurosurg. 2000; 14:476-479.
20. Banwart JC, Asher MA, Hassanein RS.
Iliac crest bone graft harvest donor site morbidity: a statistical evaluation. Spine. 1995; 20:10551060.
21. Friedlaender GE, Strong DM, Tomford
WW, Mankin HJ. Long-term follow-up of
patients with osteochondral allografts. A correlation between immunologic responses and clinical
outcome. Orthop Clin North Am. 1999; 30:583588.
22. Dodd CAF, Fergusson CM, Freedman L,
Houghton GR, Thomas D. Allograft versus autograft bone in scoliosis surgery. J Bone Joint Surg
Br. 1988; 70:431-434.
LIMITATIONS
23. Ehrler DM, Vaccaro AR. The use of allograft bone in lumbar spine surgery. Clin Orthop.
2000; 371:38-45.
24. Fleming JE Jr, Cornell CN, Muschler GF.
Bone cells and matrices in orthopedic tissue
engineering. Orthop Clin North Am. 2000;
31:357-374.
25. Pelker
RR,
Friedlaender
GE.
Biomechanical aspects of bone autografts and
allografts. Orthop Clin North Am. 1987; 18:235239.
26. Carter G. Harvesting and implanting allograft bone. AORN J. 1999; 70:660-670.
27. Palmer SH, Gibbons CL, Athanasou NA.
The pathology of bone allograft. J Bone Joint
Surg Br. 1999; 81:333-335.
28. Masiello SA, Epstein JA. Letter to
Regeneration Technologies, Inc. Pooling of
tissue from multiple donors during processing
prohibited. Rockville, MD: Food and Drug
Administration, 2001.
29. Horowitz MC, Friedlaender GE. The
immune response to bone grafts. In: Friedlaender
GE, Goldberg VM, eds. Bone and Cartilage
Allografts. Biology and Clinical Applications.
Rosemont, Ill: The Academy of Orthopaedic
Surgeons; 1991:85-101.
30. Strong DM, Friedlaender GE, Tomford
WW, et al. Immunologic responses in human
recipients of osseous and osteochondral allografts. Clin Orthop. 1996; 326:107-114.
31. Burwell RG. The fate of bone grafts. In:
Apley AG, ed. Recent Advances in Orthopedics.
London: J & A Churchill Ltd; 1969:115-207.
32. Ludwig SC, Boden SD. Osteoinductive
bone graft substitutes for spinal fusion: a basic
science summary. Orthop Clin North Am. 1999;
30:635-645.
33. Sassard WR, Eidman DK, Gray PM Jr, et
al. Augmenting local bone with Grafton demineralized bone matrix for posterolateral lumbar spine
fusion: avoiding second site autologous bone harvest. Orthopedics. 2000; 23:1059-1065.
34. Muschler GF, Negami S, Hyodo A,
Gaisser D, Easley K, Kambic H. Evaluation of
collagen ceramic composite graft materials in a
spinal fusion model. Clin Orthop. 1996;
328:250-260.
35. Zerwekh JE, Kourosh S, Scheinberg R, et
al. Fibrillar collagen-biphasic calcium phosphate
composite as a bone graft substitute for spinal
fusion. J Orthop Res. 1992; 10:562-572.
36. Chapman MW, Bucholz R, Cornell C.
Treatment of acute fractures with a collagen-calcium phosphate graft material: a randomized
clinical trial. J Bone Joint Surg Am. 1997;
79:495-502.
37. Gazdag AR, Lane JM, Glaser D, Forster
RA. Alternatives to autogenous bone graft: efficacy and indications. J Am Acad Orthop Surg.
1995; 3:1-8.
38. Ransford AO, Morley T, Edgar MA, et al.
Synthetic porous ceramic compared with autograft in scoliosis surgery. A prospective, randomised study of 341 patients [published erratum
appears in J Bone Joint Surg Br. 1998; 80:562]. J
Bone Joint Surg Br. 1998; 80:13-18.
39. Cavagna R, Daculsi G, Bouler JM.
Macroporous calcium phosphate ceramic: a
prospective study of 106 cases in lumbar spinal
fusion. J Long Term Eff Med Implants. 1999;
9:403-412.
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
OF
ALLOGRAFT
AND
AUTOGRAFT
40. LeGeros RZ. Calcium Phosphates in Oral
Biology and Medicine. Basel, Switzerland: S
Karger AG; 1991.
41. McAndrew MP, Gorman PW, Lange TA.
Tricalcium phosphate as a bone graft substitute in
trauma: preliminary report. J Orthop Trauma.
1988; 2:333-339.
42. Doursounian L, Cazeau C, Touzard R-C.
Use of tricalcium phosphate ceramics in tibial
plateau fracture repair: results of 15 cases
reviewed at 38 months. Available at:
http://bhd.online.fr/framesus.htm.
Accessed
December 15. 1999.
43. Passuti N, Daculsi G, Rogez JM, Martin
S, Bainvel JV. Macroporous calcium phosphate
ceramic performance in human spine fusion. Clin
Orthop. 1989; 248:169-176.
44. Bucholz RW, Carlton A, Holmes R.
Interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Clin Orthop.
1989; 240:53-62.
45. Kopylov P, Runnqvist K, Jonsson K,
Aspenberg P. Norian SRS versus external fixation in redisplaced distal radial fractures. A randomized study in 40 patients. Acta Orthop
Scand. 1999; 70:1-5.
46. Sanchez-Sotelo J, Munuera L, Madero R.
Treatment of fractures of the distal radius with a
remodellable bone cement: a prospective, randomised study using Norian SRS. J Bone Joint
Surg Br. 2000; 82:856-863.
47. Goodman SB, Bauer TW, Carter D, et al.
Norian SRS cement augmentation in hip fracture
treatment. Laboratory and initial clinical results.
Clin Orthop. 1998; 348:42-50.
48. Erbe EM. Attributes of Vitoss synthetic
cancellous bone void filler, an ultraporous betatricalcium phosphate scaffold [abstract].
Presented at: International Workshop on Bone
Substitutes (AO Foundation - Association for the
Study of Internal Fixation); October 8-10. 2000.
Davos, Switzerland. Available at: http://www.aoasif.ch/events/other/wbs/abstracts/a5.pdf.
Accessed April 27, 2001.
49. Erbe E. Attributes of Vitoss synthetic cancellous bone void filler, an ultraporous beta-tricalcium phosphate scaffold [abstract]. In press.
50. Erbe E. Chemistry and resorption characteristics of a synthetic cancellous bone void filler,
an ultraporous beta-tricalcium phosphate scaffold [abstract]. Presented at: World Spine I. First
Interdisciplinary World Congress on Spinal
Surgery; August 28-September 1, 2000; Berlin,
Germany.
51. Kon E, Muraglia A, Corsi A, et al.
Autologous bone marrow stromal cells loaded
onto porous hydroxyapatite ceramic accelerate
bone repair in critical-size defects of sheep long
bones. J Biomed Mater Res. 2000;49:328-337.
52. Bruder SP, Kraus KH, Goldberg VM,
Kadiyala S. The effect of implants loaded with
autologous mesenchymal stem cells on the healing of canine segmental bone defects. J Bone
Joint Surg Am. 1998; 80:985-996.
53. Johnson KD, Frierson KE, Keller TS, et
al. Porous ceramics as bone graft substitutes in
long bone defects: a biomechanical, histological,
and radiographic analysis. J Orthop Res. 1996;
14:351-369.
54. Muschler GF, Boehm C, Easley K.
Aspiration to obtain osteoblast progenitor cells
from human bone marrow: the influence of aspi-
s569
www.orthobluejournal.com
ORTHOPEDICS
ration volume. J Bone Joint Surg Am. 1997;
79:1699-1709.
55. Perry CR. Bone repair techniques, bone
graft, and bone graft substitutes. Clin Orthop.
1999; 360:71-86.
56. Garg NK, Gaur S. Percutaneous autogenous bone-marrow grafting in congenital tibial
pseudarthrosis. J Bone Joint Surg Br. 1995;
77:830-831.
57. Healey JH, Zimmerman PA, McDonnell
JM, Lane JM. Percutaneous bone marrow grafting of delayed union and nonunion in cancer
patients. Clin Orthop. 1990; 256:280-285.
58. Bauer TW, Muschler GF. Bone graft materials: an overview of the basic science. Clin
Orthop. 2000; 371:10-27.
59. Bareille R, Lafage-Proust MH, Faucheux
C, et al. Various evaluation techniques of newly
formed bone in porous hydroxyapatite loaded
with human bone marrow cells implanted in an
extra-osseous site. Biomaterials. 2000; 21:13451352.
60. Boden SD, Martin GJJ, Morone M, Ugbo
JL, Titus L, Hutton WC. The use of coralline
hydroxyapatite with bone marrow, autogenous
bone graft, or osteoinductive bone protein extract
for posterolateral lumbar spine fusion. Spine.
1999; 24:320-327.
61. Solchaga LA, Johnstone B, Yoo JU,
Goldberg VM, Caplan AI. High variability in rabbit bone marrow-derived mesenchymal cell
preparations. Cell Transplant. 1999; 8:511-519.
62. Walsh WR, Harrison J, Loefler A, et al.
Mechanical and histologic evaluation of
Collagraft(r) in an ovine lumbar fusion model.
Clin Orthop Relat Res. 2000; 375:258-266.
63. Wippermann B, Donow C, Schratt HE,
den Boer FC, Blokhuis T, Patka P. The influence
of hydroxyapatite granules on the healing of a
segmental defect filled with autologous bone
marrow. Ann Chir Gynaecol. 1999; 88:194-197.
64. Blokhuis TJ, Wippermann BW, den Boer
FC, et al. Resorbable calcium phosphate particles
as a carrier material for bone marrow in an ovine
segmental defect. J Biomed Mater Res. 2000;
51:369-375.
65. Erbe EM, Marx JG, Clineff TD,
Bellincampi LD. Potential of an ultraporous btricalcium phosphate synthetic cancellous bone
void filler and bone marrow aspirate composite
MAY 2002 VOL 25 NO 5/SUPPLEMENT
graft. Eur Spine J. 2001; 10(suppl2):S141-S146.
66. Lane JM, Tomin E, Bostrom MPG.
Biosynthetic bone grafting. Clin Orthop Related
Res. 1999; (367S):S107-S117.
67. Boyne PJ, Marx RE, Nevins M, et al. A
feasibility study evaluating rhBMP-2/absorbable
collagen sponge for maxillary sinus floor augmentation. Int J Periodontics Restorative Dent.
1997; 17:11-25.
68. Howell TH, Fiorellini J, Jones A, et al. A
feasibility study evaluating rhBMP-2/absorbable
collagen sponge device for local alveolar ridge
preservation or augmentation. Int J Periodontics
Restorative Dent. 1997; 17:124-139.
69. Cochran DL, Jones AA, Lilly LC,
Fiorellini JP, Howell H. Evaluation of recombinant human bone morphogenetic protein-2 in
oral applications including the use of endosseous
implants: 3-year results of a pilot study in
humans. J Periodontol. 2000; 71:1241-1257.
70. Wolfe MW, Cook SD. Use of osteoinductive implants in the treatment of bone defects.
Med Prog Technol. 1994; 20:155-168.
71. Riedel GE, Valentin-Opran A. Clinical
evaluation of rhBMP-2/ACS in orthopedic trauma: a progress report. Orthopedics. 1999;
22:663-665.
72. Geesink RG, Hoefnagels NH, Bulstra SK.
Osteogenic activity of OP-1 bone morphogenetic
protein (BMP-7) in a human fibular defect. J
Bone Joint Surg Br. 1999; 81:710-718.
73. Boden SD, Zdeblick TA, Sandhu HS,
Heim SE. The use of rhBMP-2 in interbody
fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine.
2000; 25:376-381.
74. Friedlaender GE, Perry CR, Cole JD, et al.
Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J
Bone Joint Surg Am. 2001; 83(pt2;suppl1):S151S158.
75. Interpore Cross. Autologous Growth
Factors (AGFTM) technology for enhanced bone
repair.
A vailable
at:
http
://www.interporecross.com/agf.html. Accessed
October 2, 2000.
76. Sigurdsson TJ, Tatakis DN, Lee MB,
Wikesj UME. Periodontal re generative potential
of space-providing expanded polytetrafluoroethylene membranes and recombinant human bone
SLACK, Incorporated, 6900 Grove Rd, Thorofare, NJ 08086-9477.
No reproduction, distribution or posting without express permission of SLACK Incorporated.
morphogenetic proteins. J Periodontol. 1995;
66:511-521.
77. Hollinger JO, Leong K. Poly(a-hydroxy
acids): carriers for bone morphogenetic proteins.
Biomaterials. 1996; 17:187-194.
78. Hollinger JO, Winn SR. Tissue engineering of bone in the craniofacial complex. Ann N Y
Acad Sci. 1999; 875:379-385.
79. Zellin G, Hedner E, Linde A. Bone regeneration by a combination of osteopromotive
membranes with different BMP preparations: a
review. Connect Tissue Res. 1996; 35:279-284.
80. Muschler GF, Hyodo A, Manning T,
Kambic H, Easley K. Evaluation of human bone
morphogenetic protein 2 in a canine spinal fusion
model. Clin Orthop Relat Res. 1994; 308:229240.
81. Lane JM, Yasko AW, Tomin E, et al. Bone
marrow and recombinant human bone morphogenetic protein-2 in osseous repair. Clin Orthop
Relat Res. 1999: 216-227.
82. Nishida K, Gilbertson LG, Evans CH,
Kang JD. Potential applications of gene therapy
to the treatment of spinal disorders. Spine. 2000;
25:1308-1314.
83. Nishida K, Kang JD, Gilbertson LG, et al.
Modulation of the biologic activity of the rabbit
intervertebral disc by gene therapy: an in vivo
study of adenovirus-mediated transfer of the
human transforming growth factor b1 encoding
gene. Spine. 1999; 24:2419-2425.
84. Wehling P, Schulitz KP, Robbins PD,
Evans CH, Reinecke JA. Transfer of genes to
chondrocytic cells of the lumbar spine. Proposal
for a treatment strategy of spinal disorders by
local gene therapy. Spine. 1997; 22:1092-1097.
85. Boden SD, Titus L, Hair G, et al. Lumbar
spine fusion by local gene therapy with a cDNA
encoding a novel osteoinductive protein (LMP1). Spine. 1998; 23:2486-2492.
86. Van Heest A, Swiontowski M. Bone-graft
substitutes. Lancet. 1999; 353(suppl1):28-29.
s570
www.orthobluejournal.com
Potrebbero piacerti anche
- Limitations of Autograft and Allograft: New Synthetic SolutionsDocumento10 pagineLimitations of Autograft and Allograft: New Synthetic SolutionsJeremy BellNessuna valutazione finora
- Xenograf Versus AllograftDocumento14 pagineXenograf Versus AllograftLab NanobiomaterialesNessuna valutazione finora
- Baldwin 2019Documento24 pagineBaldwin 2019Javier Alonso Jara CánovasNessuna valutazione finora
- NIH Public Access: Bone Tissue Engineering: Recent Advances and ChallengesDocumento59 pagineNIH Public Access: Bone Tissue Engineering: Recent Advances and ChallengesCarlosNessuna valutazione finora
- Rogers2012 Autogenous Bone Graft Basic Science and ReviewDocumento5 pagineRogers2012 Autogenous Bone Graft Basic Science and ReviewKlausNessuna valutazione finora
- Bone Graft Literature ReviewDocumento4 pagineBone Graft Literature Reviewea7gjrm5100% (1)
- Wallace, Maxillary Sinus AugmentationDocumento16 pagineWallace, Maxillary Sinus AugmentationChin-lungHsiehNessuna valutazione finora
- Conf 4.1docxDocumento9 pagineConf 4.1docxhaminatrafNessuna valutazione finora
- Bone Graft AssingmentDocumento4 pagineBone Graft AssingmentNyein Chan AungNessuna valutazione finora
- SCAFFOLDS COMBINED WITH STEM CELLS AND GROWTH FACTORS IN RECONSTRUCTION OF LARGE BONE DEFECTS. Rodolfo Capanna, Pietro de BiaseDocumento7 pagineSCAFFOLDS COMBINED WITH STEM CELLS AND GROWTH FACTORS IN RECONSTRUCTION OF LARGE BONE DEFECTS. Rodolfo Capanna, Pietro de BiaseNuno Craveiro LopesNessuna valutazione finora
- Bone Grafting: Classification by OriginDocumento4 pagineBone Grafting: Classification by OriginHerlangga Fadhillah AkbarNessuna valutazione finora
- Bone GraftDocumento18 pagineBone GraftSchuyler PereiraNessuna valutazione finora
- 5 SmartBone 2019 Paper Tibial Plateu FracturesDocumento11 pagine5 SmartBone 2019 Paper Tibial Plateu FracturesachmadaNessuna valutazione finora
- Bone Grafting and Bone Graft SubstitutesDocumento12 pagineBone Grafting and Bone Graft Substitutesaiakoby100% (1)
- Autogenous Bone GraftDocumento10 pagineAutogenous Bone Graftprogramari maxiloNessuna valutazione finora
- Autogenous Bone Harvest For Implant ReconstructionDocumento12 pagineAutogenous Bone Harvest For Implant Reconstructioncmfvaldesr7Nessuna valutazione finora
- 2 R Comparacion Materiales y Resultados Revision 2017Documento11 pagine2 R Comparacion Materiales y Resultados Revision 2017feli.riam24Nessuna valutazione finora
- RadiusDocumento11 pagineRadiusOana AlexandraNessuna valutazione finora
- Opciones Reconstructivas en Tibia JAAOS 2021Documento9 pagineOpciones Reconstructivas en Tibia JAAOS 2021Sebastian CardonaNessuna valutazione finora
- ImplantsDocumento7 pagineImplantsAna MacoveiNessuna valutazione finora
- Journal Orthopaedic Research - 2018 - Wojda - Parathyroid Hormone For Bone RegenerationDocumento9 pagineJournal Orthopaedic Research - 2018 - Wojda - Parathyroid Hormone For Bone RegenerationGali Alfaro ZagalNessuna valutazione finora
- 6 IntroductionDocumento6 pagine6 IntroductionDrsaumyaNessuna valutazione finora
- Pi Is 1010518215004084Documento8 paginePi Is 1010518215004084Ceza CezaaNessuna valutazione finora
- A Literature Based Comparison of Bone Augmentation.1Documento6 pagineA Literature Based Comparison of Bone Augmentation.1drzana78Nessuna valutazione finora
- Dhammi 2015Documento3 pagineDhammi 2015Lisa AdeliaNessuna valutazione finora
- Aaid Joi D 17 00053Documento11 pagineAaid Joi D 17 00053Yun De LinNessuna valutazione finora
- 2020 2.279 机器人的准确性和安全性 股骨头坏死的辅助钻孔减压Documento8 pagine2020 2.279 机器人的准确性和安全性 股骨头坏死的辅助钻孔减压du jiafeiNessuna valutazione finora
- Trampuz 2003Documento20 pagineTrampuz 2003collin samuelNessuna valutazione finora
- Bone Grafts, Bone Substitutes and OrthobiologicsDocumento11 pagineBone Grafts, Bone Substitutes and Orthobiologicshaqqulmauludiyah_ict_ismkiNessuna valutazione finora
- Albrektsson Foreign Body ReactionDocumento11 pagineAlbrektsson Foreign Body ReactionjeremyvoNessuna valutazione finora
- 2021 Salim OngunDocumento9 pagine2021 Salim Ongun謎超人Nessuna valutazione finora
- Cohen 2019Documento12 pagineCohen 2019Jarvin Miguel Buitrago GalindezNessuna valutazione finora
- Chapter VIDocumento17 pagineChapter VIsteigmannNessuna valutazione finora
- Bone Graft CervicalDocumento7 pagineBone Graft CervicalCarlos JohnsonNessuna valutazione finora
- Bone Graft Harvesting From Distant Sites Concepts and TechniquesDocumento16 pagineBone Graft Harvesting From Distant Sites Concepts and TechniquesGenesis Centeno100% (3)
- A Concept For The Treatment of Various Dental Bone Defects.Documento6 pagineA Concept For The Treatment of Various Dental Bone Defects.Jaime FrancoNessuna valutazione finora
- Horizontal Ridge Augmentation Using GBR With A Native Collagen Membrane and 1:1 Ratio of Particulate Xenograft and Autologous Bone: A 3 Year After Final Loading Prospective Clinical StudyDocumento9 pagineHorizontal Ridge Augmentation Using GBR With A Native Collagen Membrane and 1:1 Ratio of Particulate Xenograft and Autologous Bone: A 3 Year After Final Loading Prospective Clinical StudyYodel SrnthNessuna valutazione finora
- Bonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonDocumento19 pagineBonegraftingforimplant Surgery: Ladi Doonquah,, Pierre-John Holmes,, Laxman Kumar Ranganathan,, Hughette RobertsonJason LeeNessuna valutazione finora
- Patel 2019Documento8 paginePatel 2019Aahil SumairNessuna valutazione finora
- Peri-Implant Mucositis and Peri-Implantitis: A Current Understanding of Their Diagnoses and Clinical ImplicationsDocumento8 paginePeri-Implant Mucositis and Peri-Implantitis: A Current Understanding of Their Diagnoses and Clinical Implicationsjabp1691Nessuna valutazione finora
- Bone-Graft Substitutes:: Facts, Fictions & ApplicationsDocumento0 pagineBone-Graft Substitutes:: Facts, Fictions & ApplicationsdlopitaaNessuna valutazione finora
- PEAK Success or Failure of Dental Implants A Literature Review With Treatment ConsiderationsDocumento10 paginePEAK Success or Failure of Dental Implants A Literature Review With Treatment ConsiderationsJani MehulNessuna valutazione finora
- Autogenous Bone GraftDocumento17 pagineAutogenous Bone GraftIan CostaNessuna valutazione finora
- Bone Graft AlternativesDocumento6 pagineBone Graft Alternativesyudha anantha khaerul putraNessuna valutazione finora
- Bone and Connective TissueDocumento20 pagineBone and Connective TissueKarka PalmaNessuna valutazione finora
- Types of Bone Graft Materials Jumping Gap (Distance)Documento5 pagineTypes of Bone Graft Materials Jumping Gap (Distance)Mazen T. ShembeshNessuna valutazione finora
- Assignment-3: Recent Advances and Evidence Based Practice in Musculoskeletal PhysiotherapyDocumento7 pagineAssignment-3: Recent Advances and Evidence Based Practice in Musculoskeletal PhysiotherapyIshitaNessuna valutazione finora
- Masquelet InjuryDocumento8 pagineMasquelet Injurydrets70Nessuna valutazione finora
- Injertos Oseos OnlayDocumento7 pagineInjertos Oseos OnlayJuLi Solorzano QuinteroNessuna valutazione finora
- Recent advances in dental implant imaging and placement techniquesDocumento3 pagineRecent advances in dental implant imaging and placement techniquesvinayak shuklaNessuna valutazione finora
- UntitledDocumento15 pagineUntitledinaNessuna valutazione finora
- Vertebroplasty AbstactDocumento25 pagineVertebroplasty AbstactAshok KumarNessuna valutazione finora
- Long-Term Effects of Vertical Bone Augmentation: A Systematic ReviewDocumento15 pagineLong-Term Effects of Vertical Bone Augmentation: A Systematic ReviewShafira Nur Amalia ZulvaNessuna valutazione finora
- GRAFT ALVEOLAR DEFECTS BEFORE IMPLANT PLACEMENTDocumento10 pagineGRAFT ALVEOLAR DEFECTS BEFORE IMPLANT PLACEMENTAhmed BastawissiNessuna valutazione finora
- Bone Grafts and Substitutes in DentistryDocumento27 pagineBone Grafts and Substitutes in Dentistry林金鋒Nessuna valutazione finora
- Causes and Warning Signs of Dental Implant FailureDocumento139 pagineCauses and Warning Signs of Dental Implant FailureDrIbrahimShaikhNessuna valutazione finora
- Cervical Total Disc Replacement: Long-Term OutcomesDocumento12 pagineCervical Total Disc Replacement: Long-Term OutcomesKyle RobinNessuna valutazione finora
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentDa EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNessuna valutazione finora
- Mesenchymal Stem Cells and Skeletal RegenerationDa EverandMesenchymal Stem Cells and Skeletal RegenerationNessuna valutazione finora
- Emergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant ProfessorDocumento45 pagineEmergency Psychiatry Other Than Suicide: Dr. Pooja Singh, MD Assistant Professorpooja singhNessuna valutazione finora
- Temporomandibular Joint DisorderDocumento9 pagineTemporomandibular Joint DisorderTannels100% (1)
- Full Mouth Reconstruction - by John UtamaDocumento11 pagineFull Mouth Reconstruction - by John Utamajutama8289Nessuna valutazione finora
- Birštonas Toursim Manual 2022Documento64 pagineBirštonas Toursim Manual 2022Visit BirštonasNessuna valutazione finora
- Music Therapy Research PaperDocumento7 pagineMusic Therapy Research Paperapi-300510538Nessuna valutazione finora
- OPD Schedule (02.08.2023)Documento5 pagineOPD Schedule (02.08.2023)Private MineNessuna valutazione finora
- ParacetamolDocumento1 paginaParacetamolcen janber cabrillos100% (1)
- CPC PowerpointDocumento36 pagineCPC Powerpointapi-277377339Nessuna valutazione finora
- J Jacc 2023 04 019dDocumento12 pagineJ Jacc 2023 04 019dCristi AlexandruNessuna valutazione finora
- Intro CBTDocumento12 pagineIntro CBTAria LevinsNessuna valutazione finora
- Case StudyDocumento6 pagineCase StudyAmitNessuna valutazione finora
- Pathophysiology of A Anxiety Disorder PDFDocumento7 paginePathophysiology of A Anxiety Disorder PDFpragna novaNessuna valutazione finora
- Nursing Care Plan Deficiency of Fluid VolumeDocumento12 pagineNursing Care Plan Deficiency of Fluid VolumefitrawatiarifuddinNessuna valutazione finora
- Endocrine MCQDocumento11 pagineEndocrine MCQiman14100% (3)
- ABG Quiz by GroupDocumento13 pagineABG Quiz by Grouplourd nabNessuna valutazione finora
- 09 SterilizationDocumento34 pagine09 Sterilizationitung2350% (2)
- 250 Medical Office Procedures R 2014Documento6 pagine250 Medical Office Procedures R 2014api-250674550Nessuna valutazione finora
- MYOPIA REDUCTION... A View from the InsideDocumento6 pagineMYOPIA REDUCTION... A View from the InsidePierre RodulfoNessuna valutazione finora
- CrohnsDocumento19 pagineCrohnsLauren LevyNessuna valutazione finora
- Peptic UlcerDocumento4 paginePeptic UlcerEris Abdul AzizNessuna valutazione finora
- Formulasi Tablet VaginalDocumento9 pagineFormulasi Tablet VaginalnatinlalaNessuna valutazione finora
- Morris Fishbein - How the AMA Enemy Fought American Health InnovationsDocumento9 pagineMorris Fishbein - How the AMA Enemy Fought American Health InnovationsuncoveringconsciousNessuna valutazione finora
- 09 Dialysis DataDocumento11 pagine09 Dialysis DataThinkingPinoyNessuna valutazione finora
- MMPI-2 Validity ScalesDocumento7 pagineMMPI-2 Validity ScalesEspíritu Ciudadano50% (2)
- Body Condition Scoring As A Tool For Dairy Herd Management PDFDocumento5 pagineBody Condition Scoring As A Tool For Dairy Herd Management PDFfrankyNessuna valutazione finora
- Atrial FibrillationDocumento14 pagineAtrial FibrillationNur Atiqah ZainalNessuna valutazione finora
- Prepare Sponge and CakesDocumento30 paginePrepare Sponge and Cakesmarilyn rosilNessuna valutazione finora
- Innovations in Medical ElectronicsDocumento10 pagineInnovations in Medical Electronicsapi-3837905100% (5)
- Legal Medicine Review PDFDocumento10 pagineLegal Medicine Review PDFGhie TangonanNessuna valutazione finora
- Casestudy Pott's DiseaseDocumento36 pagineCasestudy Pott's DiseaseyasiraNessuna valutazione finora