Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
1901 St. Louis First Modern Medical Disaster
Caricato da
namename99999Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
1901 St. Louis First Modern Medical Disaster
Caricato da
namename99999Copyright:
Formati disponibili
The 1901 St Louis Incident: The First Modern Medical Disaster
Ross E. DeHovitz
Pediatrics 2014;133;964; originally published online May 26, 2014;
DOI: 10.1542/peds.2013-2817
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/133/6/964.full.html
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright 2014 by the American Academy
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from pediatrics.aappublications.org at HAM-TMC Library on June 17, 2014
a,b
AUTHOR: Ross E. DeHovitz, MD
a
Palo Alto Medical Foundation, Palo Alto, California; and bDepartment of
Pediatrics, Stanford University School of Medicine, Stanford, California
Address correspondence to Ross E. DeHovitz, MD, Palo Alto Medical Foundation,
795 El Camino Real, Palo Alto, CA 94301. E-mail: dehovir@pamf.org
Accepted for publication Nov 6, 2013
KEY WORDS
antitoxin, diphtheria, tetanus
doi:10.1542/peds.2013-2817
The 1901 St Louis Incident: The First Modern
Medical Disaster
On October 19, 1901, Dr R.C. Harris, a
St Louis physician, attended to a young
girl named Bessie Baker who was suffering from advanced diphtheria. As was
his routine, he injected diphtheria antitoxin into the child and, as a preventive,
her 2 younger siblings and concluded that
she would soon be entirely well. But 4
days later he was called back to the
Bakers home to a terrifying discovery:
There I found that the little girl was
suffering from tetanus (lockjaw). I could
do nothing for her. The poison was
injected so thoroughly into her system
that she was beyond medical aid.1
Bessie died of tetanus the following
day, as did her 2 siblings within the
week. So began one of the worst safety
disasters in the history of American
public health, in which, by the time it
was over, some 13 children had died of
tetanus from contaminated antisera.
Diphtheria was a scourge throughout
the 19th century. It primarily affected
children, and it killed through the release of an exotoxin that creates
a pseudomembrane inside the throat of
affected patients. When death occurred,
which it did in 10% to 40% of patients, it
did so primarily through asphyxiation.
In 1884, Friedrich Loefer, a scientist in
Berlin, discovered how to culture diphtheria in the laboratory and he grew it
in guinea pigs. Loefers colleagues in
964
Germany and Paris developed experiments proving that a diphtheria toxin
when injected into guinea pigs, and
later dogs and horses, produced a substance in their blood that could be used
to treat diphtheria in another species.2
In September 1894, Emile Roux in Paris
announced that his horse antiserum
had cut diphtheria mortality from 56%
to 24% in his Paris hospital. There was
great interest in bringing this new
treatment to America. Consequently,
the rst horse antitoxin factory was
established in New York and produced
its rst doses in January 1895 (Supplemental Figure 1).2
The Health Commission in St Louis,
Missouri, decided to bring this technology to the people of their city as
well. They established a factory/farm
in late 1894, with the rst doses becoming available in September 1895.
Amand Ravold, a local physician and
trained bacteriologist, was hired by
the city to direct this project.
Dr Ravold studied in Paris as a pupil of
Louis Pasteur in the developing science of bacteriology. Antitoxin was
becoming available to the city from
private rms, but the health commissioner wanted the city to establish its
own supply of antitoxin to be able to
offer it free to the poor.
By 1901, 6 years after its introduction in
the St Louis area, the use of antitoxin for
the treatment of diphtheria had become
very successful. It became the standard
treatment of presumptive pharyngeal
diphtheria. It was in this environment that
the seeds of a tragedy began to take form.
On September 30, 1901, Dr Ravold bled
a horse named Jim and acquired 2
asks of serum. Jim had been an
ambulance horse, and he was turned
over to the stables in 1898 for antitoxin
production (Supplemental Figure 5).
On October 2nd, Jim became ill with
tetanus and was killed. The antiserum
obtained on September 30th was ordered to be destroyed.
On October 26, 1901, the health department was notied by a physician
that he had under observation 2 cases
of tetanus after the use of diphtheria
antiserum. Veronica ONeill Keenan was
the rst case reported. Bessie and May
Baker died shortly thereafter. Jacob
Senturia, like the others, had initially
responded to the diphtheria antiserum, but then 6 days later his physician found the patient suffering
from trismus sardonicus: There was
a rigid spine, rigid neck and the patient rested on his occiput and heels
and he was cyanotic.3 Jacob died on
October 30th.
DEHOVITZ
Downloaded from pediatrics.aappublications.org at HAM-TMC Library on June 17, 2014
MONTHLY FEATURE
Over the next few days, as more children died, the health department
recalled the existing bottles of antitoxin and began an investigation. By
November 7th, the 13th death had
been reported (Supplemental Figures 2
and 4).
The incident was reported nationwide,
and the public became fearful. In
Chicago, the diphtheria case fatality
rate increased by one-third. In the
Journal of the American Medical Association, an editorial was published
with the title Unjustiable Distrust of
Diphtheria Antitoxin. The editorial
warned of signicantly more deaths
unless physicians demand [from the
manufacturers] a guaranteed purity
of antitoxin and are thus enabled to
speak with the condence of denite
knowledge and so inspire the anxious
parent with their own condence.4
Back in St Louis, the Tetanus Court of
Inquiry began on December 17th. Dr
Ravold had insisted that he and Henry
Taylor, the colored janitor as the
newspapers referred to him, had disposed of the September 30th serum
after the horse died. But Taylors story
began to change after he was closeted with the Chief of Detectives by
order of Mayor Wells.5 After this prolonged interrogation, Taylor was
promptly placed back on the stand
where he stated that he did release
some of the serum dated September
30th (Supplemental Figure 3). He released it, he stated, because he
thought it was safe and because the
August 24th serum was exhausted.5
On February 13, 1902, the commission
issued their verdict stating that the 13
children died of tetanus-contaminated
vials dated September 30th. Second,
the commission found that Henry
Taylor, the janitor, bottled the serum
but was not fully aware of its poisonous nature. Conversely, Dr Ravold
was aware of the dangerous nature of
the September 30th serum but was
negligent in ensuring that it was
destroyed. Last, both Dr Ravold and
Taylor were to be dismissed from the
Health Department (Supplemental
Figure 6).5
Dr Ravold responded to the verdict
stating that the Board had wrongly
dismissed Taylor: Taylor, a man of 65,
honest and faithful, was not supposed
to be competent to look after the professional affairs of the ofce. He was
simply a good servant and this discharge will leave him in hard times.5
After the incident, the city ceased all
antitoxin production. Yet, it was largely
because of the St Louis incident, and
a similar incident in Camden, New
Jersey, where there were 9 deaths,
that Congress would pass the Biologics
Control Act in the spring of 1902.
Among the arguments made was
a statement that individual states were
powerless to protect themselves
against impure and impotent materials6 because most of them consumed biologics made out of state.
The act took effect on July 1, 1902, and
subjected any company making antitoxin or vaccines to inspections and
regulations. Many companies went out
of business under this increased
scrutiny. But the result of this legislation, and legislation a few years
later that created the Food and Drug
Administration, was to increase the
safety and public condence in these
lifesaving new therapies.6
There would be other medical disasters over the course of the 20th
century. But this 1901 incident was
arguably the rst ever using a modern medical therapy. Antitoxin, now
cleared from suspicion, continued to
drive down the death rate of this
terrifying disease until a vaccine using a formalin-inactivated toxin or
toxoid became available in 1922.7
Dr Ravold went on to have a distinguished career as a bacteriologist, and
he was elected president of the St
Louis Medical Society. When he died at
age 83 in 1942, his obituary made no
mention of the diphtheria antitoxin
incident of 1901.
After Henry Taylor was red from the
St Louis Health Department, he found
work as a waiter and caterer. He died
on June 6, 1907, from chronic nephritis
and cancer. The physician who signed
his death certicate was Dr Ravold.
REFERENCES
1. Interview with Dr. R. C. Harris. St Louis Post
Dispatch. October 30, 1901: 1
2. Allen A. Vaccine, the Controversial Story of
the Worlds Greatest Lifesaver. New York, NY:
W.W. Norton and Company; 2007:123124
3. Golland M. Report of coroners inquest, Jacob
Senturia, October 30, 1901
4. Unjustiable distrust of diphtheria antitoxin.
J Am Med Assoc. 1901;37:13961397
5. St Louis Republic. December 27, 1901, February 13, 1902
6. Willrich M. Pox: An American History. New
York, NY: Penguin Press; 2011:200
7. Colgrove J. State of Immunity. Berkeley, CA:
University of California Press; 2006:109112
FINANCIAL DISCLOSURE: The author has indicated he has no nancial relationships relevant to this article to disclose.
FUNDING: No external funding.
POTENTIAL CONFLICT OF INTEREST: The author has indicated he has no potential conicts of interest to disclose.
PEDIATRICS Volume 133, Number 6, June 2014
Downloaded from pediatrics.aappublications.org at HAM-TMC Library on June 17, 2014
965
The 1901 St Louis Incident: The First Modern Medical Disaster
Ross E. DeHovitz
Pediatrics 2014;133;964; originally published online May 26, 2014;
DOI: 10.1542/peds.2013-2817
Updated Information &
Services
including high resolution figures, can be found at:
http://pediatrics.aappublications.org/content/133/6/964.full.ht
ml
Supplementary Material
Supplementary material can be found at:
http://pediatrics.aappublications.org/content/suppl/2014/05/2
0/peds.2013-2817.DCSupplemental.html
Permissions & Licensing
Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
http://pediatrics.aappublications.org/site/misc/Permissions.xh
tml
Reprints
Information about ordering reprints can be found online:
http://pediatrics.aappublications.org/site/misc/reprints.xhtml
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
Grove Village, Illinois, 60007. Copyright 2014 by the American Academy of Pediatrics. All
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from pediatrics.aappublications.org at HAM-TMC Library on June 17, 2014
Potrebbero piacerti anche
- Da Silva - On Matter Beyond The Equation of ValueDocumento11 pagineDa Silva - On Matter Beyond The Equation of Valuenamename99999Nessuna valutazione finora
- 0 McKittrick - Dear ScienceDocumento198 pagine0 McKittrick - Dear Sciencenamename99999Nessuna valutazione finora
- 0 James Concerning Violence Fanon Black CyborgDocumento15 pagine0 James Concerning Violence Fanon Black Cyborgnamename99999Nessuna valutazione finora
- Flowers On Mt. Tam by Bola SeteDocumento5 pagineFlowers On Mt. Tam by Bola Setenamename99999Nessuna valutazione finora
- Stark - On Esposito - Network of ObserversDocumento11 pagineStark - On Esposito - Network of Observersnamename99999Nessuna valutazione finora
- OnlineHebrewTutorialEnglish PDF LNK PDFDocumento36 pagineOnlineHebrewTutorialEnglish PDF LNK PDFnamename99999Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Smith CV IptecDocumento6 pagineSmith CV Iptecapi-447191360Nessuna valutazione finora
- Lesson Plan ScenarioDocumento2 pagineLesson Plan Scenarioapi-247663890Nessuna valutazione finora
- Cost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaDocumento10 pagineCost Break Down For Kaluthra Kalu, Mahrgama Nine Puppies and DeltaAdopt a Dog in Sri LankaNessuna valutazione finora
- Microbiology Last Moment RevisionDocumento16 pagineMicrobiology Last Moment RevisionDeepak MainiNessuna valutazione finora
- 3 HIV Vidas Duo UltraDocumento7 pagine3 HIV Vidas Duo UltraAndri HaryonoNessuna valutazione finora
- Coagulase TestDocumento3 pagineCoagulase TestVanandiNessuna valutazione finora
- EYE Emergency Manual An Illustrated Guide: Second EditionDocumento56 pagineEYE Emergency Manual An Illustrated Guide: Second Editionmanleyj5305Nessuna valutazione finora
- DIAGNOSTICS (Student Copy)Documento59 pagineDIAGNOSTICS (Student Copy)Abigail Mayled LausNessuna valutazione finora
- BDDocumento10 pagineBDtorajasaNessuna valutazione finora
- Non-Priority: This Is Not A Boarding CardDocumento2 pagineNon-Priority: This Is Not A Boarding CardHa My PhamNessuna valutazione finora
- Daily Shouko #543Documento15 pagineDaily Shouko #543Joshua TercenoNessuna valutazione finora
- RockerDocumento2 pagineRockerwan hseNessuna valutazione finora
- FCM National-Rabies-Control-ProgramDocumento15 pagineFCM National-Rabies-Control-ProgramMaikka IlaganNessuna valutazione finora
- NICU Standing Orders KFAFHDocumento36 pagineNICU Standing Orders KFAFHallysonviernes100% (1)
- ENT Deferential Diagnosis MEDADDocumento22 pagineENT Deferential Diagnosis MEDADReham AshourNessuna valutazione finora
- Pharma QuestionsDocumento5 paginePharma QuestionsLey BeltranNessuna valutazione finora
- Biliary AtresiaDocumento9 pagineBiliary AtresiaPrabhakar KumarNessuna valutazione finora
- Communicable Disease: List of Communicable DiseasesDocumento13 pagineCommunicable Disease: List of Communicable DiseasesjasmineNessuna valutazione finora
- Generic Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Documento4 pagineGeneric Name: Quinupristin/Dalfopristin - Injection (Kwin-ue-PRIS-tin/DAL-foe-PRIS-tin)Jrose CuerpoNessuna valutazione finora
- Cap Guidelines 2010Documento42 pagineCap Guidelines 2010Marion Andrea PoblacionNessuna valutazione finora
- Who Guidelines Blood Donor Selection 2012Documento126 pagineWho Guidelines Blood Donor Selection 2012Dananjaya Junior100% (1)
- Catalogue Lsi 2010 UKDocumento72 pagineCatalogue Lsi 2010 UKNesak1980Nessuna valutazione finora
- Concepts Theory EpidemiologyDocumento48 pagineConcepts Theory EpidemiologyStephanie Wong100% (1)
- Infection Control Risk Assessment Tool 1208Documento7 pagineInfection Control Risk Assessment Tool 1208Ama AhyarNessuna valutazione finora
- The Microbiology of Wounds: Neal R. Chamberlain, PH.D., Department of Microbiology/Immunology KcomDocumento31 pagineThe Microbiology of Wounds: Neal R. Chamberlain, PH.D., Department of Microbiology/Immunology KcomFhaliesha Zakur100% (1)
- Australia Visa PDFDocumento6 pagineAustralia Visa PDFminjiew50% (2)
- Self-Amplifying RNA Vaccines For Infectious DiseasesDocumento13 pagineSelf-Amplifying RNA Vaccines For Infectious DiseasesRicardo SousaNessuna valutazione finora
- Babesia MicrotiDocumento9 pagineBabesia MicrotiFrancene Ac-DaNessuna valutazione finora
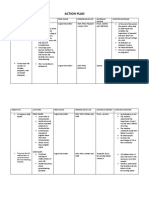
- Action PlanDocumento4 pagineAction PlanJosette Mae Atanacio67% (3)