Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Protozoans E Histolytica
Caricato da
JayricDepalobosCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Protozoans E Histolytica
Caricato da
JayricDepalobosCopyright:
Formati disponibili
[PROTOZOANS BY DR DOMANTAY] Aug.
19-20, 2014
[PROTOZOANS BY DR DOMANTAY] Aug. 19-20, 2014
Parasitic infections are either due to
a:
o Unicellular protozoan
o Multicellular metazoan
Protozoan parasites are parasites provided
with:
1. Nucleus
2. Cytoplasm
3. Outer limiting membrane
4. Organelles
*Organelles of locomotory
apparatus
a)
b)
c)
Feeding
Locomotion
Osmoregulation
Reproduction
Infective stages: CYSTS which are resistant to
environmental changes
o
abscess (extra intestinal dse)
E. histolytica Trophozoite
Many require a wet environment for:
1.
2.
3.
4.
Cilia: short processes found on the
surface
Flagella: longer, whip-like appendages
Pseudopodia: false feet
cause
colitis
and
liver
Other modes of transmission include:
o Venereal transmission (STD)
o Direct colonic inoculation
Cyst undergoes nuclear followed by
cytoplasmic division to form 8 trophozoites.
Excystation (release of trophozoites) then
occurs in the small or large bowel. The
trophozoites have the ability to colonize and
invade the large bowel.
E. histolytica trophozoites multiply by binary
fission.
They undergo encystation producing
uninucleate cysts, which undergo two
successive nuclear divisions to form the
characteristic quadrinucleate cysts (found in
stool).
able to thrive/survive even in the harshest
conditions
Vegetative stages: TROPHOZOITES
All protozoa fall under kingdom Protista
Major protozoan organisms causing disease in
man belong to:
o Phylum Sarcomastigophora
o Phylum Ciliophora
o Phylum Apicomplexa
o Phylum Microspora
Life cycle (two stages)
1. infective cyst
2. invasive trophozoite
Infection occurs when cysts are ingested from
fecally contaminated material
INTESTINAL AMEBAE: Entamoeba histolytica
E. histolytica is currently classified within
o
Subphylum Sarcodina
o
Superclass Rhizopoda
o
Class Lobosea
o
Order Amoebida
o
Genus Entamoebidae
o
Family Entamoeba
There are two generally distinct but
morphologically identical species, E. histolytica
and E. dispar
o E. histolytica = cause invasive
intestinal and extraintestinal dse
(histolytic)
o E. dispar = harmless commensal
Parasite Biology
E. histolytica is a pseudopod-forming nonflagellated protozoan parasite. It is the most
invasive of the parasites in the Entamoeba
family, and the only member of the family to
Pathogenesis & Clinical Manifestations
Signs & Symptoms
Majority of cases are asymptomatic infections
with cysts being passed out in the stools
1. Amebic colitis
presents as gradual onset of abdominal pain &
diarrhea with or without blood and mucus in
the stools.
Fever occurs only in 1/3 of patients (not
common).
[PROTOZOANS BY DR DOMANTAY] Aug. 19-20, 2014
2.
Ameboma presents as a mass-like lesion with
abdominal pain and a history of dysentery.
Name one differential diagnosis: carcinoma
Amebic liver abscess (ALA)
most common extra-intestinal form of
amebiasis.
cardinal manifestations of ALA are: (1) fever;
and
(2) right upper quadrant (RUQ) pain.
liver is tender & hepatomegaly is present in
50% of cases.
Chronic disease is found in older patients and it
involves wasting
Pathology
1. Trophozoite invasion is facilitated by the
expression of virulence factors:
a. Gal/GalNac lectin: mediates adherence
of trophozoite to host cells/ mucosa
b. Amebapores: form pores or holes in the
host membrane (lysed)
c. Cysteine proteinases: cytopathic for
host tissues, and they act by:
i. Thinning of mucin layer - allows
trophozoite to enter
submucosa
ii. Shortening of villi - indicates
malabsorption syndrome
iii. Breakdown of extracellular
matrix - aids in ability of
trophozoite to penetrate
Trophozoites attach to mucosal cells facilitated
by lectin.
They lyse cells through amebapores and
stimulate release of IL-8 which attracts and
activates neutrophils. (inflam.)
2. The trophozoites finally erode through the
lamina propria and extend laterally producing
the characteristic flask-shaped ulcer.
3.
The most common sides of amebic ulcer are
Cecum
Ascending colon
Sigmoid
E. Histolytica is the only protozoan that has an
extrainstestinal infection causing Amebic Liver Abscess
(ALA). How do trophozoites reach the liver?
4.
From the primary site in the colon, E.
histolytica trophozoites reach the liver through
a. portal vein = trophozoite penetrate the
submucosa (rich in blood vessels) thus
having a hematogenous route leading
to the Portal Vein then Liver.
b. may also occur through direct extension
(hepatic flexure of the ascending colon)
5.
Amebic Liver Absces (ALA):
Once in the liver, the trophozoites lyse
both inflammatory and liver cells
The abscess becomes filled with
necrotic, proteinaceous debris.
The aspirate is described as anchovysauce like. It is odorless and
bacteriologically sterile, although
secondary bacterial invasion may
occur.
If present, trophozoites are found at
the edge of the abscess.
*(middle of abscess only contain
necrotic cells)
Complications of E. HISTOLYTICA if left untreated:
1. Amebic Colitis
-it may cause perforations and secondary
bacterial peritonitis because colon is not
sterile.
2. Amebic Liver Abscess
-it can rupture to the pericardium, pleura or
into the peritoneal cavity.
3. Secondary Amebic Meningoencephalitis
-affects the meninges of the brain
-found in immunocompromised patients
causing abnormal mental state.
IMMUNITY TO E. HISTOLYTICA
Natural / Innate Immunity (non-specific)
Mucin from intestine prevents attachment
Complement-mediated killing in the
Systemic Circulation
Acquired Immunity
Cell mediated responses (T-cell)
Activated T-cell kills by:
a Directly lysing trophozoites in a
contact-dependent process
b Producing cytokines which attracts
macrophages and other effector
cells.
c Provides helper effect for B-cell
Antibody production
DIFFERENTIAL DIAGNOSIS
1. Amebic Colitis should be differentiated from:
[PROTOZOANS BY DR DOMANTAY] Aug. 19-20, 2014
Bacillary Dysentery of Shigella, Salmonella,
Campylobacter, Yersinia and Enteroinvasive E.
Coli
Inflammatory Bowel Disease- 2 entities:
o Crohns Disease
o Ulcerative Colitis.
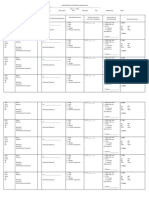
Difference between Bacillary and Amebic
BACILLARY
DYSENTERY
Bacterial
Maybe Epidemic
Acute Onset
Prodromal Fever and
malaise common
Vomiting Common
Patient is prostrate or
weak
Watery, Bloody
diarrhea
Odorless stool
Stool microscopy:
numerous bacilli, pus
cells macrophages, red
cells, no CharcotLeyden Crystals
Abdominal cramps
common and severe
Tenesmus* common
Natural history:
spontaneous recovery
in a few days, weeks or
more. No relapse
AMEBIC DYSENTERY
Parasitic
Seldom Epidemic
Gradual Onset
No Prodromal Features
No Vomiting
Patient usually
ambulant or
asyptomatic
Bloody Diarrhea
Fishy odor stool
Stool microscopy: few
bacilli, red cells,
trophozoites with
ingested RBC, Charcotleyden crystals
Mild abdominal cramps
Tenesmus* uncommon
Natural history:
Lasts for weeks;
dysentery returns after
remission; infection
persists for years.
Dysentery:
*Tenesmus= feeling of incomplete defecation
2. ALA should be differentiated from:
Pyogenic Liver abscess (pus formation by S.
aureus)
Tuberculosis of the Liver
Hepatic Carcinoma
3. Genital Amebiasis should be differentiated from:
Carcinoma
Tuberculosis
Chancroid (H. ducreii)
Lymphogranuloma Venereum (STD by
Chlamydia trachomatis
LABORATORY DIAGNOSIS
STANDARD METHOD: Fecalysis
Dont rule out with just 1 negative result
Minimum of 3 stool specimens collected at
different days because trophozoite/cyst release
is intermittent (released in batches)
DFS (Direct Fecal Smear)
- Use either: Saline, Iodine, Methylene Blue
-enhances visibility of organisms under the
microscope
-Charcot Leyden Crystals may be seen but rarely
(usual in asthma patient)
Concentration Techniques
-demonstrates cyst stage of protozoans
-techniques:
a) Zinc sulfate floatation- kills trophozoites
b) FECT- Formalin Ether Concentration Test
c) MIFC- Merthiolate Iodine Formalin
Concentration Test
Stool Culture
-Medium: Robinsons and Inokis
-usually done for research studies
E. histolytica vs E. dispar Laboratory Differentiation
o
PCR = determine genetic make-up
o
ELISA
o
Isoenzyme Analysis
SEROLOGY (for ALA)
Usually for ALA (detecting trophozoite in the liver is
hard)
Detects Antibody in Serum to positive infection
a) IHAT- Indirect Hemagglutination Test
Can direct past Antibody as long as 10 yrs*
b) CIE- Counter Immunioelectrophoresis
c) AGD- Agar Gel Diffusion
d) IFAT- Indirect Fluorescent Antibody Test
e) ELISA- Enzyme-linked Immunosorbent Assay
RADIOGRAPHIC STUDIES (for ALA)
UTZ
CT Scan
MRI
TREATMENT
2 Objectives:
a) Cure the invasive disease: Trophozoite
b) Eliminate the passage of the cyst (prevent further
infection)
1.
Invasive Amoebiasis Treatment:
o Metronidazole = DRUG OF CHOICE
o Other 5-nitroimidazole derivatives are also effective:
Tinidazole
Secnidazole
o
For asymptomatic cyst passers:
Diloxanide Furoate = DRUG of CHOICE
may also be given after a course of
metronidazole for invasive amebiasis
2.
ALA Treatement:
o
Percutaneous Drainage of Liver Abscess is indicated
for patients who do not respond to IV metronidazole.
EPIDEMIOLOGY
Distribution and Determinants of the Disease
Distribution:
At present, the epidemiology of E. histolytica is not certain
because of its similarities with E. dispar
E. Histolytica infects 50 million people worldwide
And about 100,000 infection ends fatally (ex.
Meningioencephalitis)
[PROTOZOANS BY DR DOMANTAY] Aug. 19-20, 2014
2nd to Malaria in terms of mortality caused by protozoans.
Increased cases of Amebiasis infection has been reported
from:
Indian subcontinent, Indonesia, Subsaharan &
Tropical Africa, Central & South America, Philippines
Determinants: Who are at risk of severe infection?
Children and neonates
Pregnant Women
Post-partum Patients
Those taking corticosteroids
Those with malignancy
Those with malnutrition
High risk groups in developed counties include
Recent travelers and immigrants
Inmates of mental institutions
Asexually active male homosexuals
Life Cycle of Entamoeba histolytica:
Cysts
and
trophozoites
are
passed
in
feces .
Cysts are typically
found
in
formed
stool,
whereas
trophozoites
are
typically found
in diarrheal stool.
Infection
by Entamoeba
histolytica occurs by
ingestion
of
mature
cysts
in
fecally
contaminated food, water, or hands. Excystation
occurs in the small intestine and trophozoites
are
released, which migrate to the large intestine. The trophozoites multiply by binary fission and produce
cysts , and both stages are passed in the feces . Because of the protection conferred by their walls,
[PROTOZOANS BY DR DOMANTAY] Aug. 19-20, 2014
the cysts can survive days to weeks in the external environment and are responsible for transmission.
Trophozoites passed in the stool are rapidly destroyed once outside the body, and if ingested would not
survive exposure to the gastric environment. In many cases, the trophozoites remain confined to the
intestinal lumen ( : noninvasive infection) of individuals who are asymptomatic carriers, passing cysts in
their stool. In some patients the trophozoites invade the intestinal mucosa ( : intestinal disease), or,
through the bloodstream, extraintestinal sites such as the liver, brain, and lungs ( : extraintestinal
disease), with resultant pathologic manifestations. It has been established that the invasive and
noninvasive forms represent two separate species, respectively E. histolytica and E. dispar. These two
species are morphologically indistinguishable unless E. histolytica is observed with ingested red blood cells
(erythrophagocystosis). Transmission can also occur through exposure to fecal matter during sexual
contact (in which case not only cysts, but also trophozoites could prove infective).
Note takers:
Marco Paulo Naoe
Geas-Ann Kho
Mary Anne Kua
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Sample Child Dedication ProgramDocumento1 paginaSample Child Dedication ProgramJayricDepalobos100% (2)
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Documento3 pagine"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNessuna valutazione finora
- Gilliam Autism Rating Scale (GARS-2) : Probability of Autism Is Unlikely, Possibly, Very LikelyDocumento3 pagineGilliam Autism Rating Scale (GARS-2) : Probability of Autism Is Unlikely, Possibly, Very LikelyKeishla MojicaNessuna valutazione finora
- Clinical Pastoral OrientationDocumento3 pagineClinical Pastoral OrientationJayricDepalobos100% (1)
- Biology Answers PDFDocumento30 pagineBiology Answers PDFأسيل الشلةNessuna valutazione finora
- The LightDocumento2 pagineThe LightJayricDepalobosNessuna valutazione finora
- Shipping Confirmation 1264941Documento1 paginaShipping Confirmation 1264941JayricDepalobosNessuna valutazione finora
- FWD: Schedule Change AdvisoryDocumento2 pagineFWD: Schedule Change AdvisoryJayricDepalobosNessuna valutazione finora
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 pagineConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNessuna valutazione finora
- FWD: Schedule Change AdvisoryDocumento2 pagineFWD: Schedule Change AdvisoryJayricDepalobosNessuna valutazione finora
- Bill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341Documento1 paginaBill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341JayricDepalobosNessuna valutazione finora
- Computer ModuleDocumento8 pagineComputer ModuleJayricDepalobosNessuna valutazione finora
- The Church Must Stand TogetherDocumento7 pagineThe Church Must Stand TogetherJayricDepalobosNessuna valutazione finora
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 pagineConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNessuna valutazione finora
- Medical Ward 1 Service 2 CensusDocumento13 pagineMedical Ward 1 Service 2 CensusJayricDepalobosNessuna valutazione finora
- WWW SlidDocumento1 paginaWWW SlidJayricDepalobosNessuna valutazione finora
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 pagineConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNessuna valutazione finora
- Medical Ward 1 Service 2 CensusDocumento13 pagineMedical Ward 1 Service 2 CensusJayricDepalobosNessuna valutazione finora
- Psalm 23 SermonDocumento5 paginePsalm 23 SermonJayricDepalobosNessuna valutazione finora
- Chapter 01 ChoicesDocumento9 pagineChapter 01 ChoicesJayricDepalobosNessuna valutazione finora
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocumento2 pagineWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNessuna valutazione finora
- YHH Strategic Plan 2016-2017Documento5 pagineYHH Strategic Plan 2016-2017JayricDepalobosNessuna valutazione finora
- Census TemplateDocumento3 pagineCensus TemplateJayricDepalobosNessuna valutazione finora
- Acquaintance Party ParticipantsDocumento1 paginaAcquaintance Party ParticipantsJayricDepalobosNessuna valutazione finora
- General Anesthesia in Caesarean SectionDocumento7 pagineGeneral Anesthesia in Caesarean SectionJayricDepalobosNessuna valutazione finora
- CAA Concert ProgramDocumento2 pagineCAA Concert ProgramJayricDepalobosNessuna valutazione finora
- Teen Parenting Brochure AssignmentDocumento1 paginaTeen Parenting Brochure AssignmentJayricDepalobosNessuna valutazione finora
- Pneumonia Antibiotics PDFDocumento1 paginaPneumonia Antibiotics PDFRudy KurniawanNessuna valutazione finora
- Peer Evaluation For Group 5Documento1 paginaPeer Evaluation For Group 5JayricDepalobosNessuna valutazione finora
- Thalassemia: Presentor: Don Jayric DepalobosDocumento19 pagineThalassemia: Presentor: Don Jayric DepalobosJayricDepalobosNessuna valutazione finora
- Tally Sheeth Per 10 HouseholdsDocumento14 pagineTally Sheeth Per 10 HouseholdsJayricDepalobosNessuna valutazione finora
- Tally Sheeth Per 10 HouseholdsDocumento14 pagineTally Sheeth Per 10 HouseholdsJayricDepalobosNessuna valutazione finora
- InnovativeTherapies Leukemia LymphomaDocumento0 pagineInnovativeTherapies Leukemia LymphomaTanja PopovićNessuna valutazione finora
- HybridizationDocumento19 pagineHybridizationSamer EhabNessuna valutazione finora
- Principles of Keyline DesignDocumento2 paginePrinciples of Keyline Designinfo1381Nessuna valutazione finora
- Mitosis Internet LessonDocumento3 pagineMitosis Internet LessonGLENMAR VINEGASNessuna valutazione finora
- Bacteriological Analytical Manual Chapter 21A Examination of Canned FoodsDocumento26 pagineBacteriological Analytical Manual Chapter 21A Examination of Canned FoodsFrancis Dave FloresNessuna valutazione finora
- Lecture 8 Colloids Electrokinetic PhenomenonDocumento33 pagineLecture 8 Colloids Electrokinetic PhenomenonJunaid Parker0% (1)
- Various Irrigation Solution in EndodonticDocumento70 pagineVarious Irrigation Solution in EndodontickalvinamyNessuna valutazione finora
- Neurons Rhombomere Hindbrain Amphibians Reflex Electrical SynapsesDocumento11 pagineNeurons Rhombomere Hindbrain Amphibians Reflex Electrical SynapsesNagy DóraNessuna valutazione finora
- Amino Acid For NeonateDocumento13 pagineAmino Acid For NeonateHerti PutriNessuna valutazione finora
- Grade 7 Science Cells in Its EnvironmentDocumento14 pagineGrade 7 Science Cells in Its Environmentapi-235404570100% (1)
- Cold Agglutinin Disease: PathogenesisDocumento2 pagineCold Agglutinin Disease: PathogenesisMichelle San Miguel FeguroNessuna valutazione finora
- Mammaprint in IndonesiaDocumento52 pagineMammaprint in IndonesiaYuliaji Narendra PutraNessuna valutazione finora
- Chapter Three Thermal Comfort and Health FS2023-24Documento27 pagineChapter Three Thermal Comfort and Health FS2023-24hssan AliNessuna valutazione finora
- Etymology: Meros Meaning "Part". The Term Was Coined in 1833 by Jöns Jacob Berzelius, Although HisDocumento12 pagineEtymology: Meros Meaning "Part". The Term Was Coined in 1833 by Jöns Jacob Berzelius, Although HisZoya KapoorNessuna valutazione finora
- Workup For ProteinuriaDocumento17 pagineWorkup For ProteinuriaSantiago ChávezNessuna valutazione finora
- 1 s2.0 S2213576613000808 MainDocumento2 pagine1 s2.0 S2213576613000808 MainUmi AndikaNessuna valutazione finora
- Creature IDs - Official ARK - Survival Evolved WikiDocumento19 pagineCreature IDs - Official ARK - Survival Evolved WikikirosandiskNessuna valutazione finora
- (1227) Validation of Microbial Recovery From Pharmacopeial Articles Usp39Documento5 pagine(1227) Validation of Microbial Recovery From Pharmacopeial Articles Usp39fadjarNessuna valutazione finora
- Alternative Culture Media For Bacterial Growth Using Different Formulation Ofprotein Sources PDFDocumento4 pagineAlternative Culture Media For Bacterial Growth Using Different Formulation Ofprotein Sources PDFSesi AgustinNessuna valutazione finora
- LecturasDocumento3 pagineLecturasJoseph DuffyNessuna valutazione finora
- Furan Acid On Fish OilDocumento12 pagineFuran Acid On Fish OilmisaelNessuna valutazione finora
- A Literature Review of The Epidemiology of Sepsis in Latin AmericaDocumento9 pagineA Literature Review of The Epidemiology of Sepsis in Latin AmericasmileybutterflyNessuna valutazione finora
- Matrix Pain ReliefDocumento167 pagineMatrix Pain ReliefSatinder Bhalla100% (5)
- Suturing TechniquesDocumento6 pagineSuturing TechniquesAldo TanNessuna valutazione finora
- Banana - WikipediaDocumento33 pagineBanana - WikipediaBryan Paul BautistaNessuna valutazione finora
- Daniel Timms ThesisDocumento274 pagineDaniel Timms ThesisIbrahim Basar AkaNessuna valutazione finora
- Hubungan Faktor Biotik Dan Abiotik Terhadap Keanekaragaman Makrobentos Di Hutan Mangrove Kabupaten Lombok BaratDocumento10 pagineHubungan Faktor Biotik Dan Abiotik Terhadap Keanekaragaman Makrobentos Di Hutan Mangrove Kabupaten Lombok BaratHadijahNessuna valutazione finora
- Animals With 5 Legs - Google SearchDocumento1 paginaAnimals With 5 Legs - Google SearchBen BerardNessuna valutazione finora