Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Acute Renal Failure
Caricato da
GerardLumCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Acute Renal Failure
Caricato da
GerardLumCopyright:
Formati disponibili
jslum.
com | Medicine
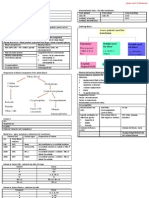
Acute Renal Failure (Acute Kidney Injury) (ARF)
Definition Complications of ARF
Clinical syndrome Oliguria
Rapid ↓ in Renal Excretory Function (occurring over hours → days) Hyperkalaemia
Oliguria ( <400ml/day) Pulmonary Edema
Anuria Metabolic Acidosis
↑ Serum Creatinine (SCr) Uremic symptoms
↑ Blood Urea Nitrogen (BUN)
Management
Importance Fluid Management
Occurs in 5% of all Hospital Admissions Pre-Renal Renal Post-Renal
Hospital Morbidity & Mortality (common cause) (30-70%) (with Volume deficit) (without Volume deficit)
Severity of underlying illness Fluid Replacement, Fluid Restriction Remove Obstruction
Complications of ARF Correction of Na+, K+ restriction
Intravascular Volume Fluid Intake =
Iatrogenic cases (50%) Contraction Output + 50ml
Sepsis • Blood Transfusion IV Frusemide
Fluid, Electrolyte imbalance • Normal Saline,
Drug Hartmann solution
Nephrotoxicity Control BP
Reversible if diagnosed & treated promptly (many cases) Hyperkalaemia
If patient survives, renal function returns to Normal or Near Normal Mild ( <6.5 mmol/L) Moderate → Severe ( >6.5 mmol/L)
(ECG – Bradycardia peaked T waves to
Diagnostic Evaluation idioventricular rhythm)
Establish Diagnosis Fluid Therapy IV Calcium Gluconate (10%)
Serum Biochemistry IV Insulin + Glucose
Symptoms & Signs Salbutamol
Elucidation of Cause Haemodialysis, Haemofiltration (if Anuric)
Clinical assessment – Presenting symptoms, Drug History, Hospital course, PE Pulmonary Edema
Urine Examination Sit up, Give ↑ flow O2 mask
Blood Tests Venous Vasodilator – Morphine IV/ IV Nitrate
Renal Imaging Loop Diuretic – Frusemide IV
Renal Biopsy Haemodialysis, Haemofiltration (if no response)
Continuous +ve airway pressure ventilation therapy
Metabolic Acidosi s
pH < 7.1 or with HCO3 >10mmol/L
Mild – Fluid Therapy
Supportive Treatment
Uraemic signs & symptoms
• Pericarditis
Urine Evaluation • Uraemic Encephalopathy
Dipstick Urinalysis Urine Microscopy Urine Biochemical Indices • Bleeding
Proteinuria Examination of Distinguish from • GI Complications
Haemoglobin sediment of Pre-renal ARF Hyperkalaemia
Leucocytes centrifuged speciment Intrinsic/ Renal ARF Fluid overload
Cells Urine Osmolality Acidosis
Casts ( > 350mosm/kg in Pre-Renal) SCr > 600 umol/L
Crystals Fractional Excretion of Na+ Urea > 30 mmol/L
Pyuria ( <1% in Pre-Renal) Dialysis
Peritoneal Dialysis
Haemodialysis
Ultrasound
Continuous Renal Re placement Therapy (CRRT )
Outcome & Long Term Prognosis
Mortality rate – 50%
Causes of Death
Sepsis
Cardiovascular causes
Pulmonary dysfunction
Mortality & Cause
Pre-Renal - 7%
Normal Acute Obstruction Toxin related - 30%
Following Trauma, Major Surgery - 50-70%
Renal Biopsy Mortality rates ↑
After excluding Pre-Renal, Post-Re nal causes of ARF Older patients
Cause of Intrinsic/ Renal ARF is unclear Multiple Organ Failure (MOF)
Useful when Clinical assessment, Urinalysis, Laboratory investigations Sepsis
suggest a diagnosis other than Ischaemic or Nephrotoxic Inj ury Patients who survive ARF episode, mostly recover sufficient renal function
Anti-glomerular basement membrane disease Never recover renal function (5-10%)
Glomerulonephritis (RPGN ) Long term dialysis
Vasculitis Transplantation
Allergic Interstitial Nephritis
jslum.com | Medicine
Acute Renal Failure
Pre-Renal (Volume Responsive) (55%) Renal (Intrinsic) (40%) Post-Renal (5-10%)
Hypovolaemia Acute Tubular Necrosi s Obstruction
Vomiting, Diarrhoea (Necrosis of Tubular Epithelial Cells) Between External Urethral meatus & Bladder neck
Haemorrhage Ischaemia Toxins Bilateral Ureteric Obstruction
Burns As for Prerenal ARF Exogenous (Drugs) Unilateral Ureteric Obstruction
Aminoglycosides (one fun ctioning Kidney)
↓ Effective Circulating Volume Amphotericin B
Cardiac Failure Radiographic contrast Bladder Neck Obstruction (most common)
Septic Shock Endogenous
Cirrhosis Rhabdomyolysis Early Stage of Obstruction (hours → days)
Anaphylaxis Haemolysis Continued glomerular filtration
Gradual distension
Drugs Interstitial Nephritis • Proximal Ureter
ACE Inhibitors Allergic Infection Infiltration • Renal Pelvis
Diuretics Antibiotics Bacterial Lymphoma • Renal Calyces
Penicillins Leptosprosis Leukaemia ↑ Tubular Hydrostatic Pressure
Sulfonamides Viral Sarcoidosis
NSAIDs Hantavirus Later Stage of Obstruction
Alveolar Vasoconstriction occurs
Diseases of Glomeruli/ Renal Microvasculature ↓ GFR
Glomerulonephritis, Vasculitis, HUS, DIVC,
Toxaemia of Pregnancy, Accelerated Hypertension
Intratubular Deposition & Obstruction
Myeloma proteins, Uric Acid
Pathogenesis Pathogenesis (Acute Tubular Ne crosis) Pathogenesis
Hypovolaemia Renal Hypoperfusion Obstruction
(↓ Effec tive Circulating Volume) ↓ ↓
↓ Tubular Ischaemia Back-Pressure
Systemic Arterial Pressure ↓ (Proximal Tubule) ↓
↓ (Thick Ascending Limb LOH) Inhibit Filtration
Renal Hypoperfusion ↓ ↓
↓ Cellular Apoptosis Inflammation Swelling, Pressure ↑
GFR ↓ (Necrosis) ↓ ↓
↓ ↓ Capillary Compress Blood Vessel
Prerenal Azotemia Back Leak Disruption of Normal sludging ↓
(Renal Parenchyma Not Damaged) Of Epithelial Integrity Ischaemia
Glomerular ↓ ↓
Filtrate Cell Sloughing Acute Kidney Injury
↓
Luminal Obstruction
↓
Acute Kidney Injury
(Acute Tubular Necrosis)
Pathogenesis
Myoglobin, Aminoglycoside
Haemoglobin antibiotic
↙ ↘ ↓
Inhibit NO Promote Accumulate in
↓ Intrarenal Renal Tubular
Multiple Intrarenal Oxidative Epithelial cells
Myeloma Vasoconstriction Stress ↓
↓ ↓ Cause
Immunoglobulin Ischaemia Oxidative
light chain Stress
↓
Directly Injury to
toxic to Tubular
Tubular Epithelial
Epithelial Cells
Cell ↓
↑ Tubular
Anticancer obstruction,
Drugs compromise
tubular
transport of
solute
Type of ARF
Pre-Renal Intrarenal Post-Renal
BUN:Creatini ne > 20:1 10:1 – 20:1 10:1 – 20:1
FENa (Fractional Excretion of Sodium) < 1% > 1% > 1%
Urine Specific Gravity > 1.020 1.010 – 1.020 1.010 – 1.020
Ultrasound Normal Normal Hydronephrosis
Urine Osmolality 350-600 < 300 Normal
Potrebbero piacerti anche
- Vesico Ureteral RefluxDocumento1 paginaVesico Ureteral RefluxGerardLumNessuna valutazione finora
- Urinary Tract Infections in ChildrenDocumento1 paginaUrinary Tract Infections in ChildrenGerardLumNessuna valutazione finora
- Urinary Tract InfectionDocumento4 pagineUrinary Tract InfectionGerardLum100% (2)
- Sexually Transmitted DiseasesDocumento6 pagineSexually Transmitted DiseasesGerardLum100% (3)
- Prostate GlandsDocumento3 pagineProstate GlandsDragan PetrovicNessuna valutazione finora
- Thyroid PhysiologyDocumento2 pagineThyroid PhysiologyGerardLum100% (2)
- ThrombophiliaDocumento3 pagineThrombophiliaGerardLum100% (1)
- Skeletal Muscle RelaxantsDocumento1 paginaSkeletal Muscle RelaxantsGerardLum100% (2)
- ThalassaemiaDocumento4 pagineThalassaemiaGerardLum100% (4)
- Soft Tissue TumoursDocumento8 pagineSoft Tissue TumoursGerardLum100% (2)
- Soft Tissue InfectionsDocumento3 pagineSoft Tissue InfectionsGerardLum100% (1)
- Renal Function in Disease StateDocumento2 pagineRenal Function in Disease Statedamai140390Nessuna valutazione finora
- Pathophysiology of Calcium, Phosphate HomeostasisDocumento5 paginePathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Posterior Pituitary SyndromeDocumento1 paginaPosterior Pituitary SyndromeGerardLumNessuna valutazione finora
- Renal Excretion of DrugsDocumento3 pagineRenal Excretion of DrugsGerardLum100% (3)
- Paediatrics OrthopaedicsDocumento5 paginePaediatrics OrthopaedicsGerardLumNessuna valutazione finora
- Principles of Blood TransfusionDocumento2 paginePrinciples of Blood TransfusionGerardLum100% (3)
- Pituitary Gland PathologyDocumento4 paginePituitary Gland PathologyGerardLumNessuna valutazione finora
- Pathogenesis Chronic Complications DiabetesDocumento5 paginePathogenesis Chronic Complications DiabetesGerardLum100% (1)
- Pathophysiology of Nerve InjuryDocumento2 paginePathophysiology of Nerve InjuryGerardLum100% (1)
- Pathology of Thyroid DiseasesDocumento5 paginePathology of Thyroid DiseasesGerardLum100% (2)
- Pituitary DysfunctionDocumento2 paginePituitary DysfunctionGerardLum0% (1)
- Pathology of TestesDocumento4 paginePathology of TestesGerardLum100% (1)
- Pathogenesis Bleeding DisordersDocumento4 paginePathogenesis Bleeding DisordersGerardLumNessuna valutazione finora
- Pathology of DiabetesDocumento4 paginePathology of DiabetesGerardLum100% (4)
- Obstructive UropathyDocumento3 pagineObstructive UropathyGerardLum100% (1)
- Pathology GlomerulonephritisDocumento4 paginePathology GlomerulonephritisGerardLum100% (2)
- Nsaids DrugsDocumento2 pagineNsaids DrugsIrene Zae MwandotoNessuna valutazione finora
- Overview of AnaemiaDocumento2 pagineOverview of AnaemiaGerardLumNessuna valutazione finora
- Nocturnal EnuresisDocumento1 paginaNocturnal EnuresisGerardLumNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- English Week3 PDFDocumento4 pagineEnglish Week3 PDFLucky GeminaNessuna valutazione finora
- Department of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Documento8 pagineDepartment of Education: Weekly Home Learning Plan Grade Ii Fourth Quarter Week 8Evelyn DEL ROSARIONessuna valutazione finora
- Timely characters and creatorsDocumento4 pagineTimely characters and creatorsnschober3Nessuna valutazione finora
- Application of ISO/IEC 17020:2012 For The Accreditation of Inspection BodiesDocumento14 pagineApplication of ISO/IEC 17020:2012 For The Accreditation of Inspection BodiesWilson VargasNessuna valutazione finora
- 2019 May Chronicle AICFDocumento27 pagine2019 May Chronicle AICFRam KrishnaNessuna valutazione finora
- Unit 1 - Introduction To BankingDocumento17 pagineUnit 1 - Introduction To Bankingc08Nessuna valutazione finora
- Distinguish Between Tax and FeeDocumento2 pagineDistinguish Between Tax and FeeRishi Agarwal100% (1)
- Childrens Ideas Science0Documento7 pagineChildrens Ideas Science0Kurtis HarperNessuna valutazione finora
- Health Education and Health PromotionDocumento4 pagineHealth Education and Health PromotionRamela Mae SalvatierraNessuna valutazione finora
- Chapter 2Documento22 pagineChapter 2Okorie Chinedu PNessuna valutazione finora
- Ecole Polytechnique Federale de LausanneDocumento44 pagineEcole Polytechnique Federale de LausanneSyed Yahya HussainNessuna valutazione finora
- Clean Agent ComparisonDocumento9 pagineClean Agent ComparisonJohn ANessuna valutazione finora
- Guide to Fair Value Measurement under IFRS 13Documento3 pagineGuide to Fair Value Measurement under IFRS 13Annie JuliaNessuna valutazione finora
- ME6404 Thermal EngineeringDocumento18 pagineME6404 Thermal EngineeringAnonymous mRBbdopMKfNessuna valutazione finora
- Kahveci: OzkanDocumento2 pagineKahveci: OzkanVictor SmithNessuna valutazione finora
- The Teacher and The Community School Culture and Organizational LeadershipDocumento10 pagineThe Teacher and The Community School Culture and Organizational LeadershipChefandrew FranciaNessuna valutazione finora
- Wacker Neuson RTDocumento120 pagineWacker Neuson RTJANUSZ2017100% (4)
- Symmetry (Planes Of)Documento37 pagineSymmetry (Planes Of)carolinethami13Nessuna valutazione finora
- Supreme Court rules stabilization fees not trust fundsDocumento8 pagineSupreme Court rules stabilization fees not trust fundsNadzlah BandilaNessuna valutazione finora
- BPO UNIT - 5 Types of Securities Mode of Creating Charge Bank Guarantees Basel NormsDocumento61 pagineBPO UNIT - 5 Types of Securities Mode of Creating Charge Bank Guarantees Basel NormsDishank JohriNessuna valutazione finora
- Microsoft Word 2000 IntroductionDocumento72 pagineMicrosoft Word 2000 IntroductionYsmech SalazarNessuna valutazione finora
- Gi 007 Gerund InfinitiveDocumento2 pagineGi 007 Gerund Infinitiveprince husainNessuna valutazione finora
- Injection Timing (5L) : InspectionDocumento2 pagineInjection Timing (5L) : InspectionaliNessuna valutazione finora
- Job Description Support Worker Level 1Documento4 pagineJob Description Support Worker Level 1Damilola IsahNessuna valutazione finora
- Ground Water Resources of Chennai DistrictDocumento29 pagineGround Water Resources of Chennai Districtgireesh NivethanNessuna valutazione finora
- Give Five Examples Each of Nature Having Reflection Symmetry and Radial Symmetry Reflection Symmetry Radial Symmetry Butterfly StarfishDocumento12 pagineGive Five Examples Each of Nature Having Reflection Symmetry and Radial Symmetry Reflection Symmetry Radial Symmetry Butterfly StarfishANNA MARY GINTORONessuna valutazione finora
- Emerson Park Master Plan 2015 DraftDocumento93 pagineEmerson Park Master Plan 2015 DraftRyan DeffenbaughNessuna valutazione finora
- Environment ManagerDocumento234 pagineEnvironment ManagerAbhishek kumarNessuna valutazione finora
- Vidura College Marketing AnalysisDocumento24 pagineVidura College Marketing Analysiskingcoconut kingcoconutNessuna valutazione finora
- ASTM D256-10 - Standard Test Methods For Determining The Izod Pendulum Impact Resistance of PlasticsDocumento20 pagineASTM D256-10 - Standard Test Methods For Determining The Izod Pendulum Impact Resistance of PlasticsEng. Emílio DechenNessuna valutazione finora