Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Alumin Posph Poison
Caricato da
azar103Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Alumin Posph Poison
Caricato da
azar103Copyright:
Formati disponibili
J Indian Acad Forensic Med, 32(4)
ISSN 0971-0973
Review paper
Aluminium Phosphide Poisoning: Management and Prevention
*Dr.S.Ranjan Bajpai
Abstract
Death by Aluminium phosphide (AlP) and organo-phosphide poisoning are the commonest forms of
poisoning in India. Aluminium phosphide is used as rodenticide and pesticide in grain storage facilities. It produces
phosphine gas, which results in mitochondrial poisoning. There is no known antidote for AIP poisoning. The effects
of AlP poisoning, mediated by phosphine and mechanism of action have not been established.The information
related to this poisoning is available in the literature and substantiated by practical experience. Liberated phosphine
cannot be detoxified but Magnesium sulphate has been reported to be effective. Another remedy can be rapid
absorption by coconut oil which might be helpful.
Treatment consists of gastric lavage with potassium permanganate solution, oral administration of charcoal
and sorbitol suspension, intravenous administration of sodium bicarbonate, magnesium sulphate and calcium
gluconate, and oral administration of sodium bicarbonate and coconut oil. Use of coconut oil for treatment in this
poisoning is suggested, although clinical trials and scientific approval is still awaited. Every suggestion, news
regarding new modality of treatment for this poisoning needs to be shared in the interest of saving precious human
lives. It is with this aim the present paper is written.
Key Words: Aluminium Phosphide, Phosphine, Rodenticide, Pesticide
ii.
Slurry of activated charcoal orally or
through nasogastric tube to adsorb
phosphine from the gastro intestinal tract.
iii.
Antacids, to reduce symptoms pertaining to
the stomach and to reduce the absorption of
phosphine through the stomach, H2
antagonists can also be used.
iv.
Medicated liquid paraffin or MgSO4 to
accelerate the excretion of Aluminium
phosphide and phosphine from the gastro
intestinal tract.
B. Reducing Cellular Toxicity of phosphine:
Phosphine produces atmosphere of hypoxia
and free radical stress by binding with cytochrome
oxidase and by inhibiting catalase. Magnesium ions
help in scavenging free radicals through GSH
recovery hence is effective as parenteral antioxidant
in this poisoning. Magnesium is anti-hypoxic and
anti-arrhythmic agent, hence due to all its beneficial
effects; it is effective in reducing the mortality in this
poisoning. The dose schedule observed to be
effective was 1 gm of MgSO4 i. v. stat followed by 1
gm after every 4 6 hours, with magnesium levels
remaining within safe limits (3 3.6 mEq.). Lower or
higher dosages have not been observed to be much
effective.
Liberated phosphine cannot be detoxified as
there is no specific antidote available. Magnesium
sulphate has been reported to be effective in reducing
mortality but some workers had found no significant
difference in dose related mortality rates in patients
treated with and without MgSO4. In a study
Introduction:
Agrochemical poisoning is a major public
health problem in developing countries particularly in
setting of low education and poor regulatory
frameworks. Aluminium phosphide is a solid
fumigant pesticide. It is marketed in India as tablets
of celphos and quickphos. Aluminium phosphide has
currently aroused interest with increasing number of
cases in the past three decades due to increased use in
agricultural and non-agricultural purpose; hence easy
availability has increased its misuse to commit
suicide.
Management:
Patients with Aluminium phosphide
poisoning are managed conservatively as no specific
antidote to the poison is known. The objective of the
treatment is to provide symptomatic and supportive
aid to the patients till phosphine is excreted through
the lungs and kidneys.
A. Reducing absorption of phosphine:
i.
Gastric lavage with KMnO4 (1:10000) or
with magnesium sulphate (MgSO4) to
oxidise the unabsorbed poison.
Corresponding Author:
*Assistant Professor
Department of Forensic Medicine
A. J. Institute of Medical Sciences
Mangalore (Karnataka)
Email: sr.bajpai@rediffmail.com
Mobile No.: +91 - 9425301920
352
J Indian Acad Forensic Med, 32(4)
ISSN 0971-0973
(Desired HCO3- = 25 mEq/L) half of the calculated
dose should be infused immediately and repeated
doses calculated in every 3 hours. If blood pH
improves with use sodium bicarbonate, it is
associated with good prognosis.
conducted by U.K.Singh et al. (1997), survival was
better in patients who presented within 4 hours and
i.v. MgSO4 was started and the authors believe that
MgSO4 therapy should be instituted early in all
patient(s) with Aluminium phosphide poisoning,
based on serum magnesium levels, considering the
high mortality of Aluminium phosphide and lack of
specific antidote.
Magnesium sulphate has been tried with
limited success for its general membrane stabilising
effect in cardiac cells.
Sushil Kumar et al. (1990) report that shock
and ECG changes in Aluminium phosphide poisoning
cases could be reverted in large percentage of cases
with larger doses of i.v. MgSO4, which raised the
serum Mg levels to about 5.2 mEq/lt.
Chugh et al. (1994) in a study on 155
patients of Aluminium phosphide poisoning studied
the efficacy of magnesium sulphate in relation to
dose of Aluminium phosphide ingested and
concluded that the effect on is mortality related to the
dose of pesticide consumed. They also observed that
MgSO4 reduced the mortality more or less equally,
irrespective of the dose of pesticide consumed.
Siwach et al. (1994) have also observed that
dose related mortality rates in patients treated with
and without MgSO4 are not significantly different.
They estimated serum Magnesium at six points
within first 24 hours and found no evidence of
hypomagnesemia at any stage, they also observed
that the chemical method of Mg++ estimation
(especially tital yellow) may give low values in
patients receiving calcium gluconate simultaneously
and tissue Mg++ reflects more accurately total Mg++
status of the body in comparison to serum level alone.
Magnesium estimation was done by them using
atomic absorption spectrophotometer which is the
more reliable method for Mg++ estimation.
Magnesium content of various organs in non
survivors and RBC Mg++ content along with serum
level were estimated. Hypomagnesemia was not
observed in any case. Magnesium content in the
organs was observed to be significantly higher than
control.
The authors also state that magnesium is
weak antiarrythmic agent and may be useful in
controlling few supra ventricular arrhythmia and
recommend use of more potent antiarrythmic agent
like Amiodarone and continued cardiac monitoring
for timely control ventricular arrythmias observed in
Aluminium phosphide poisoning.
Siwach also report (1997) that correction of
acidosis by slow infusion of sodium bicarbonate is
very helpful. If blood gas analysis is possible, total
base deficit may be calculated using the following
formula.
Base deficit = 0.4 x body wt. x desired HCO3measured HCO3- (mEq).
C. Steps to increase phosphine excretion:
Phosphine is stable and is excreted through
breath and urine. Adequate hydration, renal perfusion
with IV fluid and low dose dopamine (4 to 6 micro
gm/kg/min) enhances the excretion through urine.
Diuretic in presence of BP 70 80 mm Hg may be
useful.
Dialysis is indicated in cases with acute
renal failure if the patient is haemodynamically
stable. Supported measures in the treatment of
Aluminium phosphide poisoning include treatment of
hypoxia by oxygen inhalation or endotracheal
intubation or assisted ventilation along with
monitoring of blood gases. Treatment of shock with 3
to 4 liters of 0.9 % saline in first 8 to 12 hours, low
dose dopamine with dobutamine, hydrocortisone 200
to 400 mg I/V after 4 to 6 hours to reduce dose of
dopamine to check the capillary leakage in lung and
to potentiate the responsiveness of shock to
endogenous catacolamines. Hydrocortisone also
compensated for low levels of cortisone found in this
poisoning.
Prevention:
Since death is rapid and survival after
significant poisoning is rare, prevention is the logical
option. The most effective way for prevention is to
either ban or impose strict regulation on the sale of
aluminium phosphide tablets.
Cageing of tablets in smaller plastic with
holes and spikes so that they cant be swallowed as
such, is likely to reduce the incidence of Aluminium
phosphide poisoning.
Preventive measures have been classified by Chug et
al. under following headings:
I. Prophylaxis during and
fumigation at home and outside:
a.
b.
c.
d.
e.
f.
g.
353
after
Protect the copper containing parts before
fumigation.
Do not fumigate the grains when
temperature is below 50C.
Adequate washing facility should be
available at times during handling.
Eating, drinking, smoking should be
prohibited during and before washing after
handling.
During fumigation, operator must be given
efficient respiratory protection.
Complete the distribution of tablets within
limited time.
In warehouses, person should not sleep in
the room fumigated.
J Indian Acad Forensic Med, 32(4)
ISSN 0971-0973
4.
h.
Wear synthetic rubber gloves, boots, light
weight impervious clothes, apron, and
suitable eye protectives during fumigation
and at the time of opening the container.
i. Always open the container in air.
j. Do not inhale dust or fumes of fumigated
grains.
k. Use of phosphine detectors strips before
entering a fumigated area.
The optimum temperature for fumigation is
150C to 200C and humidity 63.7 %. When fumigated
grains is exposed to air for half an hour, the whole
phosphine gets dissipated rapidly and the cereals
become fit for consumption. Phosphine in humid air
is oxidised and becomes non-toxic.
5.
6.
7.
8.
9.
II. Education:
Farmers handling the fumigant must be
made aware of its lethal aspects. They should demand
the required amount of tablets. They should be
advised to bury the tablets in open fields after use.
They should keep their tablets away from the reach of
children and other family members.
10.
11.
III. Advice to Government Agencies:
State agencies should restrict the open sales
of this pesticide. The tablets should not be given to
young persons and children without proper
verification and confirmation. Dealers not following
the Government instructions should be punished. The
manufacturers should be advised to make small packs
of 2 3 tablets with suitable container. If possible the
pesticide should be banned.
12.
13.
14.
15.
References:
1.
2.
3.
Clinical Toxicology, Nov.2009,Vol.47,No.9, Pages
908-909, DOI- 10.3109/15563650903285657
Anger, Francois; Paysant, Francois and et al . Journal of
Analytical Toxicology,Vol.24,No.2,March 2000, Pages
90-92(3)
Human and Experimental Toxicology, Vol.24,No.4,
pages
215-218
(2005)
DOI10.1191/0960327105ht5130a
16.
17.
354
Shadnia Shahin, Rahini Mojgan, Pajournand
Abdokarim, Rasouli Hasein Mohd. Poison Center,
lohgman Hakim Hospital,Shaheed-Behesthti University
of Medical Sciences Research Centre, Tehran,Iran
Successful treatment of acute aluminium phosphide
poisoning: possible benefit of coconut oil.
Chugh SN, Jaggal KL, Malhotra KC. 1990. Steps to
reduce the mortality in Aluminium phosphide
poisoning. JAPI, 38 32.
Chugh SN. 1992. Aluminium phosphide poisoning
Present status and management. JAPI. 40; 401 405.
Chugh SN, Mittal S, Seth S, Chugh K. 1995. Lipid
peroxidation in acute aluminium phosphide poisoning.
JAPI. 43; 265 66.
Chugh SN, Prem Kumar, Aggrawal HK et al. 1994.
Efficacy of magnesium sulphate in Aluminium
phosphide poisoning Comparison of two different
dose schedules. JAPI. 42; 373 75.
Siwach SB, Pratap Singh, Sushil Ahlawat, Abha
Dua, Deepak Sharma. 1994. Serum and tissue
magnesium content in patients of acute Aluminium
phosphide poisoning and critical evaluation of high
dose magnesium sulphate therapy in reducing mortality.
JAPI. 42 (2); 107 10.
Avasthi R, Sharma R. 1994. Aluminium phosphide
poisoning and magnesium sulphate therapy. JAPI. 42;
670.
Singh UK, Chakraborty B, Prasad R. 1997.
Aluminium phosphide poisoning: A growing concern in
pediatric population. Indian Pediatrics. 34; 650 51.
Sepaha GC, Bharani AK, Jain SM et al. 1985. Acute
Aluminium phosphide poisoning. JIMA. 83; 378.
Iseri LT, Chugh P, Tobis J. 1983. Magnesium therapy
for intractable ventricular tachyarrhythmias in normal
magnesemic patients. West J. Med. 138; 823 826.
Sushil Kumar, Elhence GP, Mital HS, Mehrotra VS,
Khanna PN. 1990. Intravenous magnesium sulphate
therapy in aluminium phosphide poisoning. JAPI. 38
(1); 32.
Siwach SB. 1997. Recent trends in the management of
acute aluminium phosphide poisoning. Post Graduate
Medicine. 11; 411 413.
Sharma A. 1995. Oral Aluminium phosphide
poisoning. Indian Pediatrics. 32; 339 342.
Koley TP. 1998. Aluminium phosphide poisoning
Part I. Indian Journal of Clinical Practice. 9; 5.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Nidek GYC-1000 Photocoagulator - Technical TrainingDocumento85 pagineNidek GYC-1000 Photocoagulator - Technical TrainingAngela RoblesNessuna valutazione finora
- CXR ABC by DR ShamolDocumento139 pagineCXR ABC by DR Shamolazar103100% (3)
- Basic VibrationDocumento76 pagineBasic VibrationJack Adam100% (1)
- Marine Fenders International 2010 Catalog REDUCEDDocumento52 pagineMarine Fenders International 2010 Catalog REDUCEDMuralidhara Rao100% (2)
- CSB Case Study Hoeganaes Dec9 FinalDocumento31 pagineCSB Case Study Hoeganaes Dec9 FinalthelaceNessuna valutazione finora
- Chemistry Form 4 A+ NotesDocumento67 pagineChemistry Form 4 A+ NotesFebian Henry93% (15)
- ProjectDocumento15 pagineProjectAnil Singh Chauhan100% (1)
- COVID - English Final PDFDocumento2 pagineCOVID - English Final PDFazar103Nessuna valutazione finora
- TNSOP 6 Clinical GuidelinesDocumento14 pagineTNSOP 6 Clinical Guidelinesazar103Nessuna valutazione finora
- TNSOP 2 Sample Collection PDFDocumento4 pagineTNSOP 2 Sample Collection PDFazar103Nessuna valutazione finora
- TNSOP 4 Home Care PDFDocumento1 paginaTNSOP 4 Home Care PDFazar103Nessuna valutazione finora
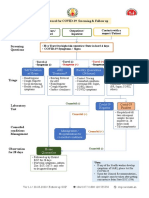
- Protocol For COVID 19 Screening and Followup PDFDocumento1 paginaProtocol For COVID 19 Screening and Followup PDFazar103Nessuna valutazione finora
- Contact Follow Up: Identify Contacts of Lab Confirmed COVID-19 Patients by District EOC (Use FORM 3A)Documento1 paginaContact Follow Up: Identify Contacts of Lab Confirmed COVID-19 Patients by District EOC (Use FORM 3A)azar103Nessuna valutazione finora
- Spartan 16 ManualDocumento579 pagineSpartan 16 ManualwuNessuna valutazione finora
- Assignment 4 Solution PDFDocumento6 pagineAssignment 4 Solution PDFAhmed AttallaNessuna valutazione finora
- Eh40 2005Documento74 pagineEh40 2005Adel SukerNessuna valutazione finora
- 2701 Downstream ProcessingDocumento16 pagine2701 Downstream Processingdadang71Nessuna valutazione finora
- Cato - Clinical Drug Trials and Tribulations PDFDocumento453 pagineCato - Clinical Drug Trials and Tribulations PDFcapranzoloNessuna valutazione finora
- HS-C0964SA3 / HS-C1264SA4 HS-C1865SA4 / HS-C2465SA1: FeaturesDocumento1 paginaHS-C0964SA3 / HS-C1264SA4 HS-C1865SA4 / HS-C2465SA1: FeaturesklseklseNessuna valutazione finora
- OCVProd Ref GuideDocumento127 pagineOCVProd Ref Guidejeff.triaxis100% (1)
- Catalyst 15 Magazine SCREENDocumento51 pagineCatalyst 15 Magazine SCREEN5DSX4zKSNessuna valutazione finora
- Galvafroid Data SheetDocumento13 pagineGalvafroid Data SheetAdam HughesNessuna valutazione finora
- AN 280 IC Carbohydrates Coffee HPAE PAD AN70231 ENDocumento12 pagineAN 280 IC Carbohydrates Coffee HPAE PAD AN70231 ENjoann bNessuna valutazione finora
- Constructing Ashby MapDocumento9 pagineConstructing Ashby MapIr FankovicNessuna valutazione finora
- Animikh Ray ResumeDocumento4 pagineAnimikh Ray ResumeAnimikh RayNessuna valutazione finora
- Cytotoxic Screening of Tropical Plants Using Brine Shrimp Lethality TestDocumento20 pagineCytotoxic Screening of Tropical Plants Using Brine Shrimp Lethality TestPrograma BRICNessuna valutazione finora
- Toxic Run ExportDocumento3 pagineToxic Run ExportOH CHEN XI MoeNessuna valutazione finora
- Demulsification Kinetics of W/O Emulsion in An A.C. Electric FieldDocumento7 pagineDemulsification Kinetics of W/O Emulsion in An A.C. Electric FieldajostosNessuna valutazione finora
- Chapters 3 and 4 Experimental ErrorDocumento55 pagineChapters 3 and 4 Experimental ErrorAman SharmaNessuna valutazione finora
- Gaussian BeamsDocumento58 pagineGaussian BeamsDaniel Humberto Martinez SNessuna valutazione finora
- Photobleaching of 5,10,15,20 Tetrakis (M Hydroxyphenyl) PorphyrinDocumento8 paginePhotobleaching of 5,10,15,20 Tetrakis (M Hydroxyphenyl) PorphyrinEsteban ArayaNessuna valutazione finora
- Magic Cleaner - FroniusDocumento4 pagineMagic Cleaner - FroniusKristy DavisNessuna valutazione finora
- Q3 - GRADE 8 - Lesson Guide - 2023-2024Documento4 pagineQ3 - GRADE 8 - Lesson Guide - 2023-2024Jasmine kNessuna valutazione finora
- C17H PDFDocumento40 pagineC17H PDFramau619Nessuna valutazione finora
- Cmo11l Quiz 2Documento6 pagineCmo11l Quiz 2Ryan GanabNessuna valutazione finora
- JEE Main 2023 31 January Shift 2Documento13 pagineJEE Main 2023 31 January Shift 2barnwalk367Nessuna valutazione finora