Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Accommodative Changes With Orthokeratology
Caricato da
Gema FelipeTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Accommodative Changes With Orthokeratology
Caricato da
Gema FelipeCopyright:
Formati disponibili
Accommodative changes produced in
response to overnight orthokeratology
Gema Felipe-Marquez, Mara NombelaPalomo, Isabel Cacho & Amelia NietoBona
Graefe's Archive for Clinical and
Experimental Ophthalmology
Incorporating German Journal of
Ophthalmology
ISSN 0721-832X
Graefes Arch Clin Exp Ophthalmol
DOI 10.1007/s00417-014-2865-2
1 23
Your article is protected by copyright and
all rights are held exclusively by SpringerVerlag Berlin Heidelberg. This e-offprint is
for personal use only and shall not be selfarchived in electronic repositories. If you wish
to self-archive your article, please use the
accepted manuscript version for posting on
your own website. You may further deposit
the accepted manuscript version in any
repository, provided it is only made publicly
available 12 months after official publication
or later and provided acknowledgement is
given to the original source of publication
and a link is inserted to the published article
on Springer's website. The link must be
accompanied by the following text: "The final
publication is available at link.springer.com.
1 23
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
DOI 10.1007/s00417-014-2865-2
MISCELLANEOUS
Accommodative changes produced in response
to overnight orthokeratology
Gema Felipe-Marquez & Mara Nombela-Palomo &
Isabel Cacho & Amelia Nieto-Bona
Received: 22 May 2014 / Revised: 6 October 2014 / Accepted: 10 November 2014
# Springer-Verlag Berlin Heidelberg 2014
Abstract
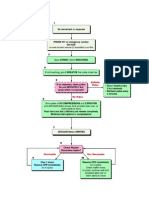
Background To evaluate short-term (3 months) and long-term
(3 years) accommodative changes produced by overnight
orthokeratology (OK).
Methods A prospective, longitudinal study on young adult
subjects with low to moderate myopia was carried out. A total
of 93 patients took part in the study. Out of these, 72 were
enrolled into the short-term follow-up: 21 were on a control
group, 26 on a Paragon CRT contact lenses group, and 25 on a
Seefree contact lenses group. The other 21 patients were old
CRT wearers on long-term follow-up. Accommodative function was assessed by means of negative and positive relative
accommodation (NRA / PRA), monocular accommodative
amplitude (MAA), accommodative lag, and monocular accommodative facility (MAF). These values were compared
among the three short-term groups at the follow-up visit. The
long- and short-term follow-up data was compared among the
CRT groups.
Results Subjective accommodative results did not suffer any
statistically significant changes in any of the accommodative
tests for any of the short-term groups when compared to
G. Felipe-Marquez : M. Nombela-Palomo
Department of Optics II (Optometry & Vision) Faculty of Optics &
Optometry, Complutense University of Madrid, Madrid, Spain
I. Cacho
Instituto Balear de Oftalmologa, Palma, Balearic Islands, Spain
A. Nieto-Bona
Contactology and Optometry Research Group (GICO), Department
of Optics II (Optometry & Vision) Faculty of Optics & Optometry,
Complutense University of Madrid, Madrid, Spain
G. Felipe-Marquez (*)
Department of Optics II, Faculty of Optometry, Universidad
Complutense de Madrid, Arcos de Jalon 118, 28037 Madrid, Spain
e-mail: gemafelipe@gmail.com
baseline. There were no statistically significant differences
between the three short-term groups at the follow-up visit.
When comparing the short- and long-term groups, only the
NRA showed a significant difference (p=0.0006) among all
the accommodation tests.
Conclusions OK does not induce changes in the ocular accommodative function for either short-term or long-term
periods.
Keywords Orthokeratology . Accommodative function .
Accommodative amplitude . Myopia . Contact lenses
Introduction
Myopic patients are always seeking options for eliminating
the use of their spectacles. The most common alternatives to
spectacles nowadays are contact lenses and refractive surgery.
Switching from spectacles to contact lenses affects the accommodation demands on myopic subjects [13]. These accommodation changes could range from negligible to large
enough to create major problems. The importance of a good
accommodative function for daily tasks has been a subject of
interest among clinicians, and changes in this function have
been studied along different ages and in different population
groups [16]. In 1949, Alpern [1] showed by means of a
theorical calculation that myopes have to accommodate more
to see the same object at the same distance when wearing
contact lenses than wearing spectacles. These changes have
been examined in clinical studies that show an increase in
accommodation required by myopes when they switch from
spectacles to contact lenses [2], which does not depend on
whether they use rigid or soft contact lenses [3]. There is also a
recent study [4] that analyzes the accommodative and binocular function in subjects wearing spectacles and soft contact
lenses. In contrast with the previous studies, they do not find
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
significant differences in accommodative amplitude. However, the accommodative lag and negative relative accommodation are higher when wearing contact lenses. When the alternative to glasses is refractive surgery, it is known that some
patients complain of near-vision problems during the early
postoperative days. A clinical trial [5] observes that laser insitu keratomileusis produces a non-significant effect on accommodation. Another study [6] found that amplitude and
facility of accommodation decreases in early postoperative
photorefractive keratectomy days, and increases back
3 months after surgery for patients under the age of 30 when
compared to preoperative values.
Another alternative to using spectacles is orthokeratology.
Corneal refractive therapy or overnight orthokeratology (OK)
is a non-surgical and reversible technique designed to temporarily correct refraction errors. Oxygen-permeable contact
lenses are used during sleep to reshape the cornea. Patients
then remove them in the morning to obtain a good visual
acuity without correction throughout the day. Advances in
lens material and technology have led to more predictable
corneal reshaping, and the results of several studies [714],
showing how it can slow the progression of the myopia, have
increased the use of the OK treatment. While there has been an
increase in orthokeratology research during the last decade,
studies concerning accommodative function pre- and postorthokeratology are limited. Only two publications [15, 16]
seem to study this function. McLeods research [15] concluded that after 3 months of OK treatment, no differences could
be found in either amplitude of accommodation or in negative
and positive relative accommodation in children. The other
publication was a pilot study by Brand [16], which found no
change in the accommodative lag but a significant improvement in accommodative facility after 3 months of OK. However, this study was limited by a very reduced and heterogeneous patients sample and, for this reason, the author considered the need for a larger study.
There are thus few studies that have analyzed the accommodative changes after OK, and the ones that are available
have a limited or heterogeneous patient sample, thus requiring
more investigation. This research aims to study the effect of
OK on accommodative function through clinical observation
in adults undergoing OK, measuring negative and positive
relative accommodation, accommodative amplitude, accommodative response, and accommodative facility. Our hypothesis is that accommodation function is not affected after the
OK treatment.
Material and methods
We designed a prospective, longitudinal, single-center study.
The study was approved by the Carlos III Hospitals Ethics
Committee, Madrid, Spain and adhered to the tenets of the
Declaration of Helsinki. Two follow-up periods were carried
out in the present study. Short-term follow-up analyzed accommodative changes over a 3-month follow-up period in
patients undergoing overnight OK treatment with two different types of OK lenses, in contrast to a control group not
having OK treatment. Long-term follow-up compared the
accommodative function over a 3-month follow-up period
versus a 3-year follow-up period on Paragon CRT (corneal
refractive therapy) contact lenses wearers.
The participants were informed of the studys protocol and
objectives. They had to meet some inclusion criteria and show
an interest in the treatment. They were recruited through the
following webpage: http://www.ucm.es/accion-social. This
page was accessible to all students and staff from the
Complutense University of Madrid, which comprises a
population of aproximately 47,000 subjects.
Our primary outcome measure was the accommodative
amplitude for having the best repeatability among other
methods [17, 18] when determined by the minus-lens method.
Also, for being the measure that, according to the Granmo
7.12 post-hoc power analysis program, needs the highest
subject number to become significant out of all the accommodative tests measured in this study. We calculated our sample
group from the mean, standard deviation, and coefficient of
repeatability. Accepting an alpha risk of 0.05 and a beta risk of
0.2 in a two-sided test, 21 subjects were needed for the first
group and 21 for the second to obtain a statistically significant
difference equal to or greater than 1 unit. The common standard deviation for our study age group was assumed to be 1.72
[18], and the correlation coefficient between the initial and
final measurement as 0.8. A drop-out rate of 10 % had been
anticipated.
Inclusion/exclusion criteria
Patients ranged from 18 to 30 years of age, and they had an
ocular refraction range of 0.50 to 5.00 DS of myopia for the
sphere and 0.25 to 1.25 DC for the cylinder. They had a
monocular best-corrected visual acuity (BCVA) of at least
0.04 logarithm of the minimum angle of resolution (logMAR).
The baseline refractive state of each participant was measured
by the manifest refraction obtained from a phoropter at the
outset of the study. Subjects were required to attend follow-up
visits at the established times. Old gas-permeable contact lens
wearers were excluded from the study, and hydrophilic lens
wearers were instructed to stop wearing their contact lenses
4 weeks before the start of the study. Subjects were also
excluded if they were pregnant or planning to become pregnant over the next 3 months. Additionally, patients that had
any systemic or eye disease, history of eye surgery, or evidence of keratoconus or corneal irregularity were also excluded. Finally, any patients that were participating in any another
clinical trial were also excluded.
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
Study population
A total of 161 people contacted the research team, and they
were given oral/written detailed information about the study.
Out of these, 68 subjects were not enrolled in the final study;
46 of them refused to participate because of personal reasons,
11 did not meet the inclusion criteria and 11 discontinued the
study due to the following: three CRT and two Seefree had
poor uncorrected visual acuity improvement, one CRT and
one Seefree had grade 2 staining (Efron grading scale), three
Seefree were unable to keep follow-up appointment, and one
CRT changed residence.
A total of 93 subjects participated in the study, of which 72
took part in the short-term follow-up: 21 took part in the
control group, and were evaluated with their conventional
correction at baseline and after 3 months, and 51 subjects
were enrolled into the treatment group and were started on
corneal refractive therapy using OK lenses (26 with CRT
lenses and 25 with Seefree lenses). They were evaluated at
baseline and 3 months after starting the treatment. Apart from
these evaluation visits, they also attended all the standard
visits for OK lens fitting. The 21 subjects from the long-term
group were participants in a previously finished CRT study
[19, 20], and had been wearing CRT lenses for at least 3 years.
Patients in this group only attended the follow-up visit. These
patients and those from the CRT-short-term follow-up group
were matched according to age, and to refractive and
keratometric values (p>0.05) previous to the OK.
Study protocol and clinical procedures
The study followed a controlled protocol. All measurements
were performed in the same office. The same clinical procedures were conducted in the same order by the same clinician
for all patients: corneal topography, visual acuity, refraction,
accommodative measurements, and slit-lamp examination. At
baseline, visual acuity and accommodative measurements
were taken with pretreatment optical correction. At the
follow-up visit, uncorrected visual acuity (UCVA), subjective
refraction, and subjective accommodative measurements were
determined without optical correction for OK groups and with
correction for the control group.
The powers of the corneal meridians were performed with
Atlas 9000 topographer (Carl Zeiss, Jena, Germany). Highcontrast visual acuity was assessed using ETDRS logMAR
charts. Subjective accommodative procedures were evaluated
in the next order. Relative accommodation was measured
using a phoropter, with the subject viewing a horizontal 20/
30 letter test line at 40 cm. The clinician introduced minus (to
stimulate positive relative accommodation, PRA) or plus (to
stimulate negative relative accommodation, NRA) spherical
lenses in 0.25 D steps binocularly until the patient reported
first sustained blur [21]. Negative relative accommodation
(NRA) was measured before positive (PRA) as suggested by
Scheiman & Wick [22]. The monocular accommodative amplitude (MAA) was determined by the minus-lens method,
which has been shown to have the best repeatability [18]. The
subject viewed a horizontal 20/30 letter test line at 33 cm, and
the clinician introduced minus lenses in 0.25 D increments
until the target first became blurred. To compensate for
minification the working distance adjustment used was kept
at 2.50 D [21]. Accommodative lag was measured by dynamic
retinoscopy (MEM, monocular estimate method). The clinician interposes plus or minus lenses (with motion or against
motion, respectively) in front of one eye at a time, until
neutralizing the reflex found in the horizontal meridian, with
the subject viewing a 20/30 letter test line. The monocular
accommodative facility (MAF) was conducted using 2.00 D
flippers, with a 20/30 test target at 40 cm. The patient was
asked to view the letters, and say now as soon as the letters
appeared clear. The refocus with +2.00 and 2.00 D was
repeated during a period of 60 s, and the cycles per minute
were recorded.
Contact lenses and adaptation
Two lens designs were used for the OK treatment. These were
the HDS 100 Paragon CRT design (Paragon Vision Sciences;
Interlenco, Madrid, Spain) and Seefree design made of Boston XO2 material (Conptica, Barcelona, Spain). Both lenses
belong to the double reverse-geometry generation of advanced
orthokeratology lenses.
The following adaptation procedure for the lenses was
implemented by a single contact lens practitioner according
to the manufacturers protocol: (1) the specifications for the
lenses were determined by the calculation rule provided by the
manufacturer (CRT lenses) or from the calculation mode
offered by the Oculus Easygraph (Oculus Optikgeraete
GMBH; Oculus; Conptica, Barcelona, Spain) (Seefree
lenses), (2) adequate fit was assessed using fluorescein, and
(3) a satisfactory fit was confirmed by the typical bulls eye
pattern that was observed by corneal topography after an
overnight trial.
New OK wearers were instructed to sleep a minimum of
8 h with their OK contact lenses every night, and to clean
them on a daily basis. All participants used MeniCare Plus
all-in-one multi-purpose lens solution with a weekly protein remover (Menicon Progent) (Menicon Co., Ltd, Nagoya, Japan), and applied unidose preservative-free lubricant eye drops (Moisture drops Avizor, Madrid, Spain)
every night to the OK lenses before inserting them into the
eye. They were examined on the morning of the very next
day, 1 week, and 1 month after adaptation, and attended
any extra visit needed if they had any problem with their
contact lenses.
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
Data analysis
Data were analyzed using STATGRAPHICS Centurion XVI,
version 16.1.17. Monocular clinical procedures were measured
in both eyes, but statistical analysis was performed only on the
data obtained from the right eyes, after ensuring that there was
no statistically significant difference between the means of the
two eyes. In the overall sample, all variables exhibited a Gaussian distribution according to the KolmogorovSmirnov test.
The baseline and follow-up data for short-term groups were
compared using a paired-sample t test. Analyses among groups
(CRT, Seefree, and control group) were performed using oneway analysis of variance (ANOVA). Results from the longterm follow-up (3-month versus 3-year period of CRT) were
compared using an unpaired-sample t test. The pre- and posttreatment and intergroup comparison were considered statistically significant for p<0.05.
Results
The final study sample was therefore comprised of 21 subjects
for the control group, 26 new CRT wearers, 25 new Seefree
wearers, and 21 old CRT wearers. None of the OK lens
wearers who finished the treatment experienced adverse responses related to the lens wear, and no abnormalities of the
eyes were found under slit-lamp microscopy. Table 1 shows
the baseline mean values and standard deviations for gender,
age, BCVA, and refractive and keratometric measurements for
the right eyes of each group.
groups. The sphere reductions recorded at 3 months were
2.231.06 D and 2.090.95 D for the CRT and Seefree
groups respectively. No statistically significant changes were
detected for the refractive cylinder of each group. The mean
post-treatment residual refractive errors for the CRT and for
the Seefree groups were 0.010.35 D (range 0.87 to +0.50
D) and 0.010.34 D (range 0.50 to +0.50 D) respectively,
and the mean uncorrected visual acuity values were 0.08
0.08 and 0.010.09 logMAR for the CRT and Seefree
groups, c respectively. The uncorrected visual acuity improved in a statistically significant manner from baseline to
3 months in both OK groups (p<0.00). The central cornea was
statistically significantly flattened (p<0.00) for both the steeper and flatter meridians after the 3-month treatment in both of
the OK groups. The changes recorded at 3 months were 1.22
0.53 D and 1.200.52 D for the flatter meridian of the CRT
and Seefree groups respectively, and 1.170.62 D and 1.03
0.61 D for the steeper meridian respectively. The control
group did not show any statistically significant differences in
these measurements for the same period of time.
Table 2 shows the means and standard deviations of
the accommodative values at baseline and changes after
the 3-month treatment in NRA, PRA, MAA, lag and
MAF for control, CRT, and Seefree group. The p-value
column shows no differences over the 3-month treatment
for any of the above-mentioned accommodative parameters for all groups. The last column compares changes
over the 3 months among the three groups with ANOVA
test, showing no significant differences for any of the
parameters.
Long-term follow-up
Short-term follow-up
The mean sphere magnitude and sphere equivalent (SE) decreased significantly from baseline to 3 months for all OK
Table 1
We studied the long-term effects that CRT lens wear has over
a 3-month and 3-year follow-up period for the abovementioned accommodative values. The mean residual
Refractive and corneal variables previous to the OK treatment
Control (n=21)
mSD
CRT 3 months (n=26)
Seefree (n=25)
CRT 3 years (n=21)
Male/female (%)
Male/female (n)
Age (years)
BCVA (LogMAR)
Sphere (D)
57 % / 43 %
12 / 9
24.84.0
0.080.06
2.231.09
46 % / 54 %
12 / 14
24.23.4
0.060.06
2.161.06
40 % / 60 %
10 / 15
25.83.5
0.120.05
2.071.00
43 % / 57 %
9 / 12
24.93.5
0.060.06
1.900.99
Cylinder (D)
SE (D)
Sim Kflat (D)
Sim Ksteep (D)
0.200.26
2.331.07
43.201.59
44.031.68
0.180.30
2.251.07
43.211.40
43.941.46
0.160.28
2.151.00
43.511.26
44.141.42
0.220.34
2.051.05
43.191.50
43.921.56
n number of subjects, m mean, SD standard deviation, BCVA best-corrected visual acuity, SE sphere equivalent, Sim Kflat, Sim Ksteep simulated
keratometry readings along flatter and steeper meridians
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
Table 2 Short-term follow-up.
Accommodative values at
baseline and 3 months, and
changes over 3 months
Baseline
mSD
NRA (D)
Control
CRT
Seefree
PRA (D)
Control
CRT
Seefree
MAA (D)
Control
CRT
Seefree
Lag (D)
Control
CRT
A positive change over time
corresponded with an increased
result after 3 months, and a
negative change with a decreased
result
m mean, SD standard deviation
Seefree
MAF (cpm)
Control
CRT
Seefree
1
0.25
0.27
0.65
1.650.71
1.700.99
1.710.78
1.960.88
1.990.88
1.910.93
0.310.79
0.290.92
0.200.70
0.08
0.09
0.26
0.90
9.661.92
9.992.02
9.392.27
9.322.02
9.481.60
8.991.75
0.341.10
0.512.10
0.411.18
0.19
0.18
0.15
0.93
0.620.27
0.440.34
0.570.33
0.370.35
0.030.36
0.060.50
0.76
0.48
0.72
0.470.49
0.530.34
0.050.59
0.70
11.073.87
9.804.92
11.554.55
10.454.30
10.974.19
11.004.43
0.632.80
1.174.81
0.553.9
0.33
0.18
0.55
Table 3 Long-term follow-up. Accommodative values for 3 months
and 3 years with CRT
Lag (D)
MAF (cpm)
1.580.50
1.990.88
9.481.60
2.230.72
1.950.77
8.661.31
0.370.35
10.974.19
0.350.41
11.685.28
m mean, SD standard deviation
* p<0.01
ANOVA
00.39
0.150.70
0.160.60
Orthokeratology is an effective and reversible treatment
that gives the patient freedom from optical correction to
NRA (D)
PRA (D)
MAA (D)
Paired t-test
p-value
1.940.54
1.580.50
1.430.45
Discussion
3 years
Change over time
1.940.48
1.730.66
1.590.56
refractive error for the 3-year follow-up group was 00.38 D
(range :0.75 to +1.00 D) and the mean uncorrected visual
acuity value was 0.110.07 logMAR. Table 3 shows the
means and standard deviations of these values for the two
follow-up groups. The p-value column only shows a statistically significant difference for the NRA value (p<0.01). The
other accommodative parameters did not show any statistically significant difference between the two groups.
3 months
mSD
3 months
p-value
0.0006*
0.89
0.08
0.84
0.61
0.21
carry out activities of daily living while being awake.
This treatment has been widely studied [713, 2325],
but to date there are only two references that have
studied the accommodative function in OK treatment
[15, 16]. However, both McLeod [15] and Brand [16]
considered the need for further investigation to reach
concluding results. McLeod recognized that the minuslens method would have been a better option to measure amplitude of accommodation, rather than using the
push-up technique, and Brand considered his sample to
be very reduced and heterogeneous. The current study
has been carried out with the aim of analyzing the
changes in accommodation induced over time by OK
treatment in adults.
Short-term follow-up
The theoretical calculations about the influence of contact
lenses on accommodation [1, 2] showed that when axial
myopic subjects switch from spectacles to contact lenses, a
greater accommodative effort is required. The change of accommodative requirement is directly related to the degree of
myopia. Robertson et al. [2] analyzed accommodative requirements using schematic eyes with 5, 7, 10 and 15 D; these
myopic values are higher than the ones we found in this
current study. Robertson et al. [2] supported their theoretical
calculations with a clinical study, measuring the near-point of
accommodation. They found that the near-point of
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
accommodation was closer to the eye when the myopia was
corrected with spectacles than when wearing contact lenses,
and they found a much greater difference than had been
anticipated from theoretical calculations. Carney and Woo
[3], in agreement with Robertson et al., also concluded that
an increased accommodation is required for myopic subjects
when they wear contact lenses, but that it does not depend on
whether they are rigid or soft contact lenses. The results of the
current study do not show differences between groups in any
of the accommodative measurements, and thus the accommodative function is not affected by the wearing of CRT or
Seefree lenses. According to the current studys results and
those from Carney and Woo [3], ocular accommodation is not
disturbed by either the type (soft/rigid), nor the contact lenss
brand (CRT/Seefree). However, we did not find a difference
between the control group and the OK wearers, which contrasts with Carney and Woos finding. A more recent study [4]
does not show changes in accommodation when myopes
switch from spectacles to soft contact lenses, contrasting with
these previous studies [2, 3]. Jimenez et al. [4] considered that
the differences between their results and the previous studies
could be explained by the different sample sizes or refractive
errors, among others. Our mean refraction was about 2.25 D,
Jimnez et al.s 2.50 D and previous studies approximately
4.25 D. If we only bear in mind the theory, a lower refraction
would not show statistically significant differences, while a
higher power could. A change in a high refraction could be
due to the distance of the accommodative plane. We should
not forget that the OK needs time to be completed and stabilized. This present study allowed a 3-month follow-up period
from the baseline visit, which should be enough time for the
visual system to adapt to the new situation. We are unaware of
whether there are accommodative changes over the first days
of contact lens wear, because we did not take measurements
during those days. Besides, the reversibility of the OK effect
varies per individual, and thus the regression is not linear and
not always predictable. It is possible that different habits of
accommodation are learned while fitting OK lenses from the
beginning of the OK treatment. This could be the reason for
which several patients reported near-vision difficulties after
PRK or LASIK treatment [5, 6]. This way, Karimian et al. [6]
found that both AA and FA decreased over the early days of
post-PRK treatment, but increased or went back to the original
level after 3 months from surgery. We must take into account
that the accommodative change is drastic after surgery, and
that the visual system needs time to get used to the new
corneal shape and for the accommodative function to become
stable.
When we compared the changes over time, we did not find
any statistical differences either for the study groups, or for
any of the accommodative tests. In fact, all results show
normal mean accommodative values, according to the normative values for young adults [22]. Although occasional values
of the clinical tests were out of normal ranges, none of them
could be classified into any of the accommodative or binocular disorders [26], and thus all subjects had normal accommodative function at both baseline and follow-up visits. However, the outcomes may be different when measured from populations with abnormal accommodative or binocular vision
function. Statistical analysis revealed no significant differences in NRA/PRA over the 3-month follow-up, agreeing
with McLeods [15] data from children. Jimnez et al.s [4]
NRA values were significantly higher (p<0.01) with soft
contact lenses than with spectacles over time. They also found
lower PRA values (p=0.07) and higher values of accommodative lag (p<0.01), and therefore suggested that their accommodative results could indicate the presence of an accommodative insufficiency with contact lens wear. Our lack of differences for the NRA, PRA, and accommodative lag values
over time contrasts with those from Jimnez et al. [4], and
could be explained by the different focal points when using
soft contact lenses, spectacles, or OK lenses. Brand [16] and
McLeod [15] also found no changes in the accommodative
response after a 3-month follow-up period, despite the fact
that McLeod [15] used a different measuring technique, the
fused cross-cylinder method. Our lack of changes on the
amplitude of accommodation induced by the OK agrees with
McLeods study, although they used the push-up technique
and recognized that the minus-lens method would have been a
better option. Our accommodative facility results disagree
with those from Brand [16], who found a significant improvement after OK in this test. However, he did not measure the
number of cycles per minute but only graded the accommodative facility into a pass or a fail, and we are therefore not
able to compare these results.
Post-hoc power analysis was carried out on the measurements close to reaching significance: PRA in both control and
CRT groups, with paired t-test p-values of 0.08 and 0.09
respectively (Table 2). According to this analysis, a required
sample size of eight subjects per group for a paired t-test
would be needed to reach clinical significance. Since our
groups comprised a much larger final amount of subjects (21
subjects for the control group, 26 new CRT wearers, and 25
new Seefree wearers) the analysis confirms that our results
were not clinically significant.
There is previous literature studying the relationship between the eyes aberrations and the accommodative function
[2732]. However, there are no studies on this relationship
when OK lenses are fitted. Tarrant et al. [33] hypothesized,
analyzing the Zernike defocus, that a reduction in accommodative lag is the result of the increase in spherical aberration
produced by OK. Our lag results varied among groups: the
control and CRT groups suffered a slight decrease of the lag
value, while for the Seefree group this value suffered a slight
increase, although none of them were significant. On the other
hand, Gifford et al. [34] considered the accommodation as an
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
active process to neutralize the ocular spherical aberration
due to the differences between corneal and ocular spherical aberrations. The lack of significant changes in any of
our accommodative measurements does not agree with
these previous hypotheses. A possible explanation for this
difference could lie with the time of reassessment: Tarrant
et al. reassessed 4 weeks after the beginning of the OK
treatment, Gifford et al. after 1 week, and the present
study after 3 months. It could be that these different
periods of time between the baseline and follow-up visits
would result in different adaptations of the ocular system.
Another explanation could be that the OK treatment generates little change in the internal optics when the eye
readapts to the new corneal shape, while the accommodative capability does not suffer changes over time. There is
a recently published study [35] that discusses the effect of
OK on anterior chamber depth, posterior radius of corneal
curvature, and axial length over 1 year. However, its
results do not agree with those from other previous studies [3641]. Bearing in mind that accommodation relies
on the combined action of ciliary muscle and ocular lens
system, a future study would be interesting that apart from
our accommodative parameters, pre and post-OK treatment would control the central corneal thickness, anterior
chamber depth, pupil diameter, crystalline lens thickness,
and radii of curvature of the anterior and posterior surfaces of the lens by means of long scan depth optical
coherence tomography [42, 43], in
Conclusions
The present study includes the largest sample size to date on
the changes in accommodative function with OK in an adult
population. The accommodative function is not altered by OK
treatment for either a short or a long period of OK treatment.
The NRA is the only accommodative function that has a
significantly different value between the long- and shortterm groups at the follow-up visit, which could be explained
by possible changes of the interaction between the accommodative and vergence systems.
Acknowledgments The authors want to thank Interlenco (Madrid,
Spain), Conptica (Barcelona, Spain), and Avizor (Madrid, Spain) laboratories for their support.
Conflict of interest The authors declare no financial or proprietary
interests in any of the materials or methods mentioned.
No sources of public or private financial support declared.
Presentation at a conference None
Clinical trial registration number if required None
References
1. Alpern M (1949) Accommodation and convergence with contact
lenses. Am J Optom Arch Am Acad Optom 26:379387
2. Robertson DM, Ogle KN, Dyer JA (1967) Influence of contact lenses
on accommodation. Theoretic considerations and clinical study. Am J
Ophthalmol 64:860871
3. Carney LG, Woo GC (1977) Comparison of accommodation with
rigid and flexible contact lenses. Am J Optom Physiol Optic 54:595
597
4. Jimenez R, Martinez-Almeida L, Salas C, Ortiz C (2011) Contact
lenses vs spectacles in myopes: is there any difference in accommodative and binocular function? Graefes Arch Clin Exp Ophthalmol
249:925935. doi:10.1007/s00417-010-1570-z
5. Liu L, Yuan J, Li J, Li X, Wang Y (2008) Effect of laser in situ
keratomileusis on accommodation. J Huazhong Univ Sci Technol
Med Sci 28:596598. doi:10.1007/s11596-008-0524-8
6. Karimian F, Baradaran-Rafii A, Bagheri A, Eslani M, Bayat H,
Aramesh S, Yaseri M, Amin-Shokravi A (2010) Accommodative
changes after photorefractive keratectomy in myopic eyes. Optom
Vis Sci 87:833838. doi:10.1097/OPX.0b013e3181f6fccc
7. Koffler BH, Sears JJ (2013) Myopia control in children through
refractive therapy gas permeable contact lenses: is it for real? Am J
Ophthalmol 156(6):1076.e11081.e1. doi:10.1016/j.ajo.2013.04.
039
8. Cheung SW, Cho P (2013) Validity of axial length measurements for
monitoring myopic progression in orthokeratology. Invest
Ophthalmol Vis Sci 54:16131615. doi:10.1167/iovs. 12-10434
9. Cho P, Cheung SW (2012) Retardation of myopia in Orthokeratology
(ROMIO) study: a 2-year randomized clinical trial. Invest
Ophthalmol Vis Sci 53:70777085. doi:10.1167/iovs. 12-10565
10. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, GutierrezOrtega R (2012) Myopia control with orthokeratology contact lenses
in Spain: refractive and biometric changes. Invest Ophthalmol Vis
Sci 53:50605065. doi:10.1167/iovs. 11-8005
11. Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T (2012)
Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest
Ophthalmol Vis Sci 53:39133919. doi:10.1167/iovs. 11-8453
12. Kakita T, Hiraoka T, Oshika T (2011) Influence of overnight
orthokeratology on axial elongation in childhood myopia. Invest
Ophthalmol Vis Sci 52:21702174. doi:10.1167/iovs. 10-5485
13. Walline JJ, Jones LA, Sinnott LT (2009) Corneal reshaping and
myopia progression. Br J Ophthalmol 93:11811185. doi:10.1136/
bjo.2008.151365
14. Cho P, Cheung SW, Edwards M (2005) The longitudinal
orthokeratology research in children (LORIC) in Hong Kong: a pilot
study on refractive changes and myopic control. Curr Eye Res 30:
7180. doi:10.1080/02713680590907256
15. McLeod ADL (2006) Effects of overnight orthokeratology on phoria,
vergence, and accommodation in children. New England College of
Optometry, pp. xi, 125 p
16. Brand P (2013) The effect of orthokeratology on accommodative and
convergence function: a clinic based pilot study. Optom Vis Perform
1:162167
17. Antona Pealba B (2010) Fiabilidad intraexaminador y concordancia
de pruebas clnicas de evaluacin de la visin binocular Optica II
(Optometra y visin). Universidad Complutense de Madrid, Madrid.
Spain, pp. 251. Thesis. http://eprints.ucm.es/10149/1/T30728.pdf
18. Antona B, Barra F, Barrio A, Gonzalez E, Sanchez I (2009)
Repeatability intraexaminer and agreement in amplitude of accommodation measurements. Graefes Arch Clin Exp Ophthalmol 247:
121127. doi:10.1007/s00417-008-0938-9
19. Nieto-Bona A, Gonzalez-Mesa A, Nieto-Bona MP, Villa-Collar C,
Lorente-Velazquez A (2011) Short-term effects of overnight
Author's personal copy
Graefes Arch Clin Exp Ophthalmol
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
orthokeratology on corneal cell morphology and corneal thickness.
Cornea 30:646654. doi:10.1097/ICO.0b013e31820009bc
Nieto-Bona A, Gonzalez-Mesa A, Nieto-Bona MP, Villa-Collar C,
Lorente-Velazquez A (2011) Long-term changes in corneal morphology induced by overnight orthokeratology. Curr Eye Res 36:895
904. doi:10.3109/02713683.2011.593723
Palomo-Alvarez C, Puell MC (2008) Accommodative function in
school children with reading difficulties. Graefes Arch Clin Exp
Ophthalmol 246:17691774. doi:10.1007/s00417-008-0921-5
Scheiman MM, Wick B (2008) Clinical management of binocular
vision : heterophoric, accommodative and eye movement disorders.
Lippincott Williams & Wilkins, Philadelphia
Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, GutierrezOrtega R (2014) Short-term changes in ocular biometry and refraction after discontinuation of long-term orthokeratology. Eye Contact
Lens 40:8490. doi:10.1097/icl.0000000000000014
Santolaria E, Cervino A, Queiros A, Brautaset R, Gonzalez-Meijome
JM (2013) Subjective satisfaction in long-term orthokeratology patients. Eye Contact Lens 39:388393. doi:10.1097/ICL.
0b013e3182a27777
Swarbrick HA (2006) Orthokeratology review and update. Clin Exp
Optom 89:124143. doi:10.1111/j.1444-0938.2006.00044.x
Cacho-Martinez P, Garcia-Munoz A, Ruiz-Cantero MT (2014) Is
there any evidence for the validity of diagnostic criteria used for
accommodative and nonstrabismic binocular dysfunctions? J
Optom 7:221. doi:10.1016/j.optom.2013.01.004
Ninomiya S, Fujikado T, Kuroda T, Maeda N, Tano Y, Oshika T,
Hirohara Y, Mihashi T (2002) Changes of ocular aberration with
accommodation. Am J Ophthalmol 134:924926
Hazel CA, Cox MJ, Strang NC (2003) Wavefront aberration and its
relationship to the accommodative stimulusresponse function in
myopic subjects. Optom Vis Sci 80:151158
Cheng H, Barnett JK, Vilupuru AS, Marsack JD, Kasthurirangan S,
Applegate RA, Roorda A (2004) A population study on changes in
wave aberrations with accommodation. J Vis 4:272280. doi:10.
1167/4.4.3
Iida Y, Shimizu K, Ito M, Suzuki M (2008) Influence of age on ocular
wavefront aberration changes with accommodation. J Refract Surg
24:696701
Yuan Y, Shao Y, Tao A, Shen M, Wang J, Shi G, Chen Q, Zhu D,
Lian Y, Qu J, Zhang Y, Lu F (2013) Ocular anterior segment
biometry and high-order wavefront aberrations during accommodation. Invest Ophthalmol Vis Sci 54:70287037. doi:10.1167/
iovs. 13-11893
Hiraoka T, Miyata K, Nakamura Y, Ogata M, Okamoto F, Oshika T
(2014) Influence of cycloplegia with topical cyclopentolate on
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
higher-order aberrations in myopic children. Eye (Lond). doi:10.
1038/eye.2014.34
Tarrant J, Liu Y, Wildsoet CF (2009) Orthokeratology can decrease
the accommodative lag in myopes. ARVO Meet Abstr 50:4294
Gifford P, Li M, Lu H, Miu J, Panjaya M, Swarbrick HA (2013)
Corneal versus ocular aberrations after overnight orthokeratology.
Optom Vis Sci 90:439447. doi:10.1097/OPX.0b013e31828ec594
Gonzalez-Mesa A, Villa-Collar C, Lorente-Velazquez A, Nieto-Bona
A (2013) Anterior segment changes produced in response to longterm overnight orthokeratology. Curr Eye Res 38:862870. doi:10.
3109/02713683.2013.790977
Owens H, Garner LF, Craig JP, Gamble G (2004) Posterior corneal
changes with orthokeratology. Optom Vis Sci 81:421426
Stillitano IG, Chalita MR, Schor P, Maidana E, Lui MM, Lipener C,
Hofling-Lima AL (2007) Corneal changes and wavefront analysis
after orthokeratology fitting test. Am J Ophthalmol 144:378386.
doi:10.1016/j.ajo.2007.05.030
Tsukiyama J, Miyamoto Y, Higaki S, Fukuda M, Shimomura Y
(2008) Changes in the anterior and posterior radii of the corneal
curvature and anterior chamber depth by orthokeratology. Eye
Contact Lens 34:1720. doi:10.1097/ICL.0b013e3180515299
Chen D, Lam AK, Cho P (2010) Posterior corneal curvature change
and recovery after 6 months of overnight orthokeratology treatment.
Ophthalmic Physiol Opt 30:274280. doi:10.1111/j.1475-1313.
2010.00710.x
Queiros A, Villa-Collar C, Gutierrez AR, Jorge J, Ribeiro-Queiros
MS, Peixoto-de-Matos SC, Gonzalez-Meijome JM (2011) Anterior
and posterior corneal elevation after orthokeratology and standard
and customized LASIK surgery. Eye Contact Lens 37:354358. doi:
10.1097/ICL.0b013e318232e32d
Yoon JH, Swarbrick HA (2013) Posterior corneal shape changes in
myopic overnight orthokeratology. Optom Vis Sci 90:196204. doi:
10.1097/OPX.0b013e31828121eb
Yuan Y, Chen F, Shen M, Lu F, Wang J (2012) Repeated measurements of the anterior segment during accommodation using long scan
depth optical coherence tomography. Eye Contact Lens 38:102108.
doi:10.1097/ICL.0b013e318243e795
Zhu D, Shao Y, Leng L, Xu Z, Wang J, Lu F, Shen M (2014)
Automatic biometry of the anterior segment during accommodation
imaged by optical coherence tomography. Eye Contact Lens. doi:10.
1097/ICL.0000000000000043
Garca A, Cacho P, Lara F (2002) Evaluating relative accommodations in general binocular dysfunctions. Optom Vis Sci 79:779787
Aldaba M, Vilaseca M, Arjona M, Pujol J (2013) Age-related changes in accommodation measured with a double-pass system.
Ophthalmic Physiol Opt 33:508515. doi:10.1111/opo.12038
Potrebbero piacerti anche
- Contact Lenses Vs Spectacles in Myopes: Is There Any Difference in Accommodative and Binocular Function?Documento12 pagineContact Lenses Vs Spectacles in Myopes: Is There Any Difference in Accommodative and Binocular Function?mau tauNessuna valutazione finora
- The Actions and Uses of Ophthalmic Drugs: A Textbook for Students and PractitionersDa EverandThe Actions and Uses of Ophthalmic Drugs: A Textbook for Students and PractitionersNessuna valutazione finora
- Single-Step Transepithelial PHDocumento9 pagineSingle-Step Transepithelial PHlenniNessuna valutazione finora
- Lower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor FracturesDocumento5 pagineLower Eyelid Complications Associated With Transconjunctival Versus Subciliary Approaches To Orbital Floor Fracturesstoia_sebiNessuna valutazione finora
- Accommodative and Binocular Vision Dysfunction in A Portuguese Clinical PopulationDocumento7 pagineAccommodative and Binocular Vision Dysfunction in A Portuguese Clinical PopulationpoppyNessuna valutazione finora
- Efficacy and Safety of A Soft Contact Lens To Control MyopiaprogressionDocumento8 pagineEfficacy and Safety of A Soft Contact Lens To Control MyopiaprogressionAmandaNessuna valutazione finora
- GlaucomaDocumento37 pagineGlaucomaxuelun1Nessuna valutazione finora
- 1 s2.0 S2452232516302165 MainDocumento9 pagine1 s2.0 S2452232516302165 MainIndah Nur LathifahNessuna valutazione finora
- Effects of 1064-nm Nd-YAG Long-Pulse Laser On Polidocanol MicrofoamDocumento8 pagineEffects of 1064-nm Nd-YAG Long-Pulse Laser On Polidocanol MicrofoamrachiddellarNessuna valutazione finora
- Axial Length StudyDocumento8 pagineAxial Length StudyMαρία ΚολέδαNessuna valutazione finora
- Assisted Cataract Surgery Versus Standard UltrasoundDocumento3 pagineAssisted Cataract Surgery Versus Standard UltrasoundNanda Tata NataNessuna valutazione finora
- Consensus On The Management of Astigmatism in Cataract SurgeryDocumento14 pagineConsensus On The Management of Astigmatism in Cataract Surgerymelon segerNessuna valutazione finora
- Efikasi TX Gukoma 2016Documento37 pagineEfikasi TX Gukoma 2016Al-Harits OctaNessuna valutazione finora
- Ebn RugayDocumento6 pagineEbn RugayJeffrey Barcelon TanglaoNessuna valutazione finora
- Ascrs 2Documento7 pagineAscrs 2leokapilNessuna valutazione finora
- Seizure: Kristina Malmgren, Anna EdelvikDocumento8 pagineSeizure: Kristina Malmgren, Anna EdelvikRidho ArendoNessuna valutazione finora
- Clinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusDocumento10 pagineClinical Study: Two-Year Accelerated Corneal Cross-Linking Outcome in Patients With Progressive KeratoconusPunam RazputriNessuna valutazione finora
- Current Advances in Ophthalmic TechnologyDa EverandCurrent Advances in Ophthalmic TechnologyParul IchhpujaniNessuna valutazione finora
- Low-Level Red-Light Therapy As A Novel Modality For Myopia Control in Children: A Systematic ReviewDocumento14 pagineLow-Level Red-Light Therapy As A Novel Modality For Myopia Control in Children: A Systematic ReviewArlinNessuna valutazione finora
- VitrectomiaDocumento11 pagineVitrectomiaSebastianCruzTroncosoNessuna valutazione finora
- Research ArticleDocumento7 pagineResearch ArticlePhei Qing TjangNessuna valutazione finora
- Rmo 97 40Documento15 pagineRmo 97 40JoseNessuna valutazione finora
- Literature Review PterygiumDocumento7 pagineLiterature Review Pterygiumafmzzaadfjygyf100% (1)
- Scheimpflug Corneal Densitometry Changes After TrabeculectomyDocumento7 pagineScheimpflug Corneal Densitometry Changes After TrabeculectomyFernando MartínezNessuna valutazione finora
- Myopia Control During Orthokeratology Lens Wear in Children Using A Novel Study DesignDocumento11 pagineMyopia Control During Orthokeratology Lens Wear in Children Using A Novel Study DesignLisa WidiasmokoNessuna valutazione finora
- The Open Ophthalmology Journal: Editorial: Update On Glaucoma Diagnosis and ManagementDocumento2 pagineThe Open Ophthalmology Journal: Editorial: Update On Glaucoma Diagnosis and ManagementNur Rakhma AkmaliaNessuna valutazione finora
- Dry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-AnalysisDocumento7 pagineDry Eye and Corneal Sensitivity After Small Incision Lenticule Extraction and Femtosecond Laser-Assisted in Situ Keratomileusis: A Meta-Analysismohamad safiiNessuna valutazione finora
- Articulo en InglesDocumento20 pagineArticulo en InglesJavier VivarNessuna valutazione finora
- Effect of Repeated Low-Level Red-Light Therapy For Myopia Control in Children A Multicenter Randomized Controlled TrialDocumento11 pagineEffect of Repeated Low-Level Red-Light Therapy For Myopia Control in Children A Multicenter Randomized Controlled TrialYekiita QuinteroNessuna valutazione finora
- Critical Appraisal Nyimas Irina SilvaniDocumento6 pagineCritical Appraisal Nyimas Irina SilvaniNyimas Irina SilvaniNessuna valutazione finora
- CRST1111 Cs Mini ZabriskieDocumento2 pagineCRST1111 Cs Mini ZabriskieTyasBanggaPribadieNessuna valutazione finora
- High Myopiaypartial Reduction Ortho-K: A 2-Year Randomized StudyDocumento10 pagineHigh Myopiaypartial Reduction Ortho-K: A 2-Year Randomized StudykarakuraNessuna valutazione finora
- Jurnal Mata 5Documento6 pagineJurnal Mata 5Dahru KinanggaNessuna valutazione finora
- Prostaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerDocumento4 pagineProstaglandin Release During Femtosecond Laser-Assisted Cataract Surgery: Main InducerAyen AlingNessuna valutazione finora
- Contact Lens and Anterior Eye: Rute J. Macedo-de-Araújo, Eef Van Der Worp, José M. González-Méijome TDocumento9 pagineContact Lens and Anterior Eye: Rute J. Macedo-de-Araújo, Eef Van Der Worp, José M. González-Méijome TJorge Silva VereauNessuna valutazione finora
- Compliance With Soft Contact Lens Replacement Schedules and Associated Contact Lens-Related Ocular Complications: The UCLA Contact Lens StudyDocumento10 pagineCompliance With Soft Contact Lens Replacement Schedules and Associated Contact Lens-Related Ocular Complications: The UCLA Contact Lens StudyMirza RisqaNessuna valutazione finora
- Pi Is 0161642022006698Documento7 paginePi Is 0161642022006698TRẦN NGỌC LAM THANHNessuna valutazione finora
- Presentation 1Documento24 paginePresentation 1-Yohanes Firmansyah-Nessuna valutazione finora
- Jurnal Mata 1Documento8 pagineJurnal Mata 1Anonymous sFBiKFJ3Nessuna valutazione finora
- Refractive TheoryrDocumento3 pagineRefractive TheoryrgotcanNessuna valutazione finora
- 16 Nigwekar Etal.Documento4 pagine16 Nigwekar Etal.editorijmrhsNessuna valutazione finora
- Corticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Documento8 pagineCorticosteroids For Bacterial Keratitis - The Steroids For Corneal Ulcers Trial (SCUT)Bela Bagus SetiawanNessuna valutazione finora
- The Effectiveness of Laser Vitreolysis For Vitreous Floaters in Posterior Vitreous DetachmentDocumento7 pagineThe Effectiveness of Laser Vitreolysis For Vitreous Floaters in Posterior Vitreous Detachmentmistic0Nessuna valutazione finora
- The Ahmed Shunt Versus The Baerveldt Shunt For Refractory Glaucoma: A Meta-AnalysisDocumento7 pagineThe Ahmed Shunt Versus The Baerveldt Shunt For Refractory Glaucoma: A Meta-AnalysisYusri YudhaNessuna valutazione finora
- Closed-Chamber Techniques For Iridodialysis Repair BMC 2018Documento6 pagineClosed-Chamber Techniques For Iridodialysis Repair BMC 2018Alexandre IshizakiNessuna valutazione finora
- Monovision Lasik in Emmetropic Presbyopic PatientsDocumento7 pagineMonovision Lasik in Emmetropic Presbyopic PatientsIvana Ester Sinta UliNessuna valutazione finora
- Pharmacological Treatments of Presbyopia: A Review of Modern PerspectivesDocumento4 paginePharmacological Treatments of Presbyopia: A Review of Modern PerspectivesPrisciLia Ade SyahnaNessuna valutazione finora
- DEFOCUS - Photonics-2023Documento8 pagineDEFOCUS - Photonics-2023Rafael IribarrenNessuna valutazione finora
- Emily Covington Critical Review RelaxofonDocumento6 pagineEmily Covington Critical Review Relaxofonapi-254759511Nessuna valutazione finora
- tmpC73A TMPDocumento8 paginetmpC73A TMPFrontiersNessuna valutazione finora
- Comparison of The Effect of Cycloplegia On Astigmatism Measurement in A Pediatric Amblyopic PopulationDocumento6 pagineComparison of The Effect of Cycloplegia On Astigmatism Measurement in A Pediatric Amblyopic PopulationSyaiful UlumNessuna valutazione finora
- Early Protraccion Class IIIDocumento13 pagineEarly Protraccion Class IIISandra CarranzaNessuna valutazione finora
- Glaukoma TripleDocumento5 pagineGlaukoma TripleR.m. IrsanNessuna valutazione finora
- Simultaneous Double Eyelid Blepharoplasty and Ptosis CorrectionDocumento8 pagineSimultaneous Double Eyelid Blepharoplasty and Ptosis CorrectionshininghmNessuna valutazione finora
- Patients' Attitudes and Beliefs To Presbyopia and Its CorrectionDocumento6 paginePatients' Attitudes and Beliefs To Presbyopia and Its CorrectionPutri kartiniNessuna valutazione finora
- File 712 20230127155855Documento9 pagineFile 712 20230127155855Nakarit SangsirinawinNessuna valutazione finora
- Boston XODocumento5 pagineBoston XOjuan diego RuizNessuna valutazione finora
- 2012 Cer Hiraoka Long-Term Effect of Orthokeratology 5yDocumento7 pagine2012 Cer Hiraoka Long-Term Effect of Orthokeratology 5yIgnacio AlvarezNessuna valutazione finora
- A Comparison of Laser Photocoagulation With Cryotherapy For Threshold Retinopathy of Prematurity at 10 Years Part 2. Refractive OutcomeDocumento6 pagineA Comparison of Laser Photocoagulation With Cryotherapy For Threshold Retinopathy of Prematurity at 10 Years Part 2. Refractive OutcomeSalma HamdyNessuna valutazione finora
- 2021 Article 2180Documento8 pagine2021 Article 2180Nabilla Mitha TalitaNessuna valutazione finora
- PneumoniaDocumento20 paginePneumoniaKartika RezkyNessuna valutazione finora
- Patient DatasheetDocumento28 paginePatient DatasheetMohit RajNessuna valutazione finora
- Npi NH PDFDocumento24 pagineNpi NH PDFsatyagraha84Nessuna valutazione finora
- How To Control Hypertension (High Blood Pressure) - Nutrition StudiesDocumento3 pagineHow To Control Hypertension (High Blood Pressure) - Nutrition StudiesMatevž BrojanNessuna valutazione finora
- Facial Fat Grafting: Why, Where, How, and How MuchDocumento20 pagineFacial Fat Grafting: Why, Where, How, and How MuchMade SetiadjiNessuna valutazione finora
- Dorothea Orem-Self Care TheoryDocumento10 pagineDorothea Orem-Self Care TheoryNikhil MohanNessuna valutazione finora
- Cholesterol PresentationDocumento28 pagineCholesterol Presentationapi-240098169Nessuna valutazione finora
- Types of NeurotransmittersDocumento1 paginaTypes of NeurotransmittersAileen AblanNessuna valutazione finora
- Data Sheet Data Sheet: Gelafusal GelafusalDocumento2 pagineData Sheet Data Sheet: Gelafusal Gelafusalfahri azwarNessuna valutazione finora
- Cabello 2012Documento7 pagineCabello 2012Vannia BautistaNessuna valutazione finora
- Basic Life SupportDocumento6 pagineBasic Life SupportRyan Mathew ScottNessuna valutazione finora
- Therapy ManualDocumento52 pagineTherapy ManualcrisNessuna valutazione finora
- Autocoid PharmacologyDocumento29 pagineAutocoid PharmacologyLyadelou Fortu100% (1)
- Manual C28 Plus enDocumento28 pagineManual C28 Plus enSveto SlNessuna valutazione finora
- Immune Thrombocytopenia (Second Option)Documento16 pagineImmune Thrombocytopenia (Second Option)Fein MalricNessuna valutazione finora
- PHD Thesis Ram Dheeraj Business Admin PDFDocumento292 paginePHD Thesis Ram Dheeraj Business Admin PDFplaycharles89Nessuna valutazione finora
- Trastorno de Ansiedad Artículo en Ingles: CursoDocumento11 pagineTrastorno de Ansiedad Artículo en Ingles: CursocamilaNessuna valutazione finora
- Family Nursing Care Plan SeizuresDocumento3 pagineFamily Nursing Care Plan SeizuresClaire AlcantaraNessuna valutazione finora
- Anti Aging and LongevityDocumento37 pagineAnti Aging and LongevityrehanfasihNessuna valutazione finora
- Wastewater Treatment Plant Operator I (WWTPOI)Documento2 pagineWastewater Treatment Plant Operator I (WWTPOI)Rahmi ArslanNessuna valutazione finora
- The Arthritis Step by Step Strategy PDF EBook DownloadDocumento7 pagineThe Arthritis Step by Step Strategy PDF EBook Downloadowenmathias880% (2)
- Pelvic Inflammatory DiseaseDocumento34 paginePelvic Inflammatory DiseaseOhunakin AfolabiNessuna valutazione finora
- Applying Theories, Perspectives, and Practice Models To Integrated HealthDocumento78 pagineApplying Theories, Perspectives, and Practice Models To Integrated HealthMd Farid AhmedNessuna valutazione finora
- Symptoms of Sexual DisordersDocumento5 pagineSymptoms of Sexual DisordersJham ⎝⏠⏝⏠⎠ CapulongNessuna valutazione finora
- PRICELIST OGB JKN Update 08.04.22Documento7 paginePRICELIST OGB JKN Update 08.04.22Imro FitrianiNessuna valutazione finora
- Youstina Khalaf Exam 26-5Documento6 pagineYoustina Khalaf Exam 26-5M Usman KhanNessuna valutazione finora
- Respiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoDocumento8 pagineRespiratory Physiology: Control of The Upper Airway: Richard L. Horner University of TorontoDopamina PsicoactivaNessuna valutazione finora
- VOLUX 尖沙咀 chung parr hall 鍾伯豪醫生 PDFDocumento8 pagineVOLUX 尖沙咀 chung parr hall 鍾伯豪醫生 PDFAnonymous YT4f4ejNtH100% (1)
- Abnormal Psychology Chapter 13Documento84 pagineAbnormal Psychology Chapter 13Summer LeeNessuna valutazione finora
- Pediatric LeukemiasDocumento42 paginePediatric LeukemiasslyfoxkittyNessuna valutazione finora