Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Renal Physiology
Caricato da
JayricDepalobosCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Renal Physiology
Caricato da
JayricDepalobosCopyright:
Formati disponibili
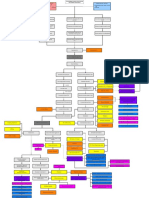
[RENAL PHYSIOLOGY 2ND HOUR] February 8, 2014
Classification scheme for Acute Kidney
Injury* (RIFLE criteria)
___
Risk
Injury
Failure
Loss
ESKD
GFR Criteria
Increased SCreat x
1.5 or GFR decrease
>25%
Increased SCreat x
or GFR decrease
>50%
Increased SCreat x 3
or GFR decrease
75% or SCrea
>4mg/dl
Urine
Output
Criteria
UO
<5ml/kg/h x
6hr
UO
<5ml/kg/h x
12hr
UO
<3ml/kg/h x
24hrs oliguria
Anuria x
12hrs
Persistent ARF complete loss of
kidney function >4 weeks
End Stage Kidney Disease
(>3months)
*Significance of RIFLE criteria: to know if the
clinical course of the patient is improving or not
based on the serum creatinine and urine output.
Urine
output will not make the doctor wait for a
couple of days before he can act on the patients
condition. For example, if by 6 hours the patient is
producing less than 5ml/kg/h, the doctor can analyze if
the kidney injury is progressing to a more severe form.
He may hydrate the patient, give diuretics, give an
anti-inflammatory drug, and give steroids depending
on his assessment. Every 6 hours the patient should be
reassessed. If management is not aggressive, this may
lead to progression to the point of dialysis.
ACUTE KIDNEY INJURY (AKI)
A. ETIOLOGY
Pre renal - before glomerulus/kidney
(Vasomotor nephropathy)
Ischemic - blood supply to kidney has been
compromised
Hypovolemia secondary to bleeding
GI electrolye losses in diarrhea
Burns or renal salt wasting stab wound, MVA
injury
Hypotension
Shock
Hypoxia
Heart Failure
Sepsis
Intestinal obstruction
Hepatorenal syndrome due to antigen antibody
reactions
Toxic drugs:
Aminoglycosides (gentamicin, amikacin,
neomycin)
Wasp stings
Bee stings
Toxins:
Plant toxins
*weight losing drugs such as Bangkok pills
contain aristolochic acid Renal failure, renal
insufficiency
Snake bites
Rhabdomyolysis
Blackwater fever in falciform malariae
Radiocontrast agents
Renal
(Intrinsic to kidney)
Glomerulonephritis
Post infectious (post streptococcal, post viral)
SystemicLupus Erythematosus
Henoch-Schonlein Purpura (HSP)
Membranoproliferative glomerulonehritis (MPGN)
ANCA GN
Anti-neutrophil cytoplasmic autoantibodes (ANCA)
assoc. w/ necrotizing & crescentic GN
Anti-Glomerular Basement Membrane disease
Vascular: renal artery stenosis affecting blood
supply to kidneys
Hemolytic-uremic syndrome (HUS)
Renal vein thrombosis
Renal artery thrombosis
Acute tubulointerstitial nephritis allergy to drugs
causing sloughing off of tubular membrane
Infectious
Epstein-Barr virus (EBV)
Leptospirosis (hepatorenal syndrome)
Drugs including herbal preparations
Acute pyelonephritis
Tumor infiltration
Post renal - after glomerulus/kidney
[RENAL PHYSIOLOGY 2ND HOUR] February 8, 2014
Structural (identify where obstruction is to see the
cause):
Posterior urethral valve
Ureteric obstruction
Neurogenic bladder
8) Prevent fluid overload (give diuretics or
doing RRT)
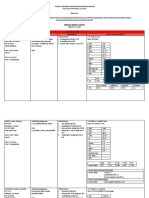
Modern criteria for the initiation of RRT
in the ICU
Oliguria (UO < 200ml w/in next 12 hrs)
Crystalluria acid crystals in the tubules
Tumor lysis syndrome (seen in patients receiving
chemotherapy)
Melamine
*Illegally added to food products (ex. milk) &
may cause renal & urinary problems)
*Resin used in porcelain used as milk substitute
*Renal stones, renal failure
Calculi
Blood clot
B. MANAGING AKI
Treatment or removal of the cause to address
treatment
Maintenance of physiological homeostasis while
recovery takes place
1) Nutritional support (30-35 kcal/kg/day) as
mixture of CHO and lipids, & CHON at 12g/kg (most patients have poor appetite so
IV solutions may be given)
2) Hyperkalemia must be promptly treated
(Use hyper-K regimen: nebulize the patient
Kayexylate may be given, calcium gluconateemergency management)
a) Insulin and dextrose (D5050)
*Insulin shifts K into cell
b) Sodium bicarbonate given if metabolic
acidosis is present (orally/intravenously)
c) Calcium gluconate
*Replaces Ca and help entry of K back into
the cell
d) RRT (Renal replacement therapy w/ 2
modalities: Peritoneal & Hemodialysis)
3) Metabolic acidosis (due to failure to
conserve HCO3)
4) Anemia (due to disruption of EPO production
in renal interstitial cell)
5) Renal doses of drugs
6) Stress ulcer prophylaxis
*Preserve the viability of GI mucosa so that
you can give H2 receptor antagonists &
potent pump inhibitors (PPI)
7) Prevent infection and iatrogenic causes of
infection
UO >0.5cc/kg w/in the next 6 hrs based on RIFLE
criteria
*Consider dialysis, unresponsive to fluid therapy
BUN > 80mg/dl
Normal: 20mg/dl
4x elevated BUN: consider diuretic therapy
Serum creatinine > 3mg/dL (initiate dialysis)
Normal: 1 mg/dl
75% increase: consider renal replacement
Serum K > 6.5mmol/L or rapidly rising
Arrhythmias experienced - you give bicarbonate,
Insulin, glucose, etc and yet it cannot be
corrected
Pulmonary edema unresponsive to diuretics
Uncompensated metabolic acidosis (pH<7.1)
HCO3 8 or 9
Temperature > 40 C
-Disruption of central regulator of temperature
Uremic complications (encephalopathy,
myopathy, neuropathy/pericarditis)
Overdose w/ a dialyzable toxin
Nephrotic syndrome: (3 cornerstones for
nephrosis:)
1. Proteinuria
*Urine spillage: > 2 g/day of CHON in children
> 3 g/day in adult
2. Generalized edema (ascites, periorbital
edema, bipedal edema, scrotal edema)
3. Hypoalbuminemia
Corticosteroids such as Prednisone are given
(e.g dose: 2mg/kg/day to a pediatric patient)
Some adverse effects of steroid therapy include
cushingoid appearance (bufallo hump), Hirsutism,
HTN, behavioral changes, steroid psychosis
Nephrotic
syndrome may be
precipitated by a
viral infection
(patients would
usually manifest with
cough and colds)
should be treated
first.
[RENAL PHYSIOLOGY 2ND HOUR] February 8, 2014
Obstructive Uropathy
-Renal cortex remains intact while renal medulla
has expanded and the presence of a pelvic
constriction of a ureter.
-Post renal obstruction that can eventually lead to
renal failure.
Intravenous pyelogram will show the
obstruction in the renal pelvis, dye cannot
be seen draining down into the urinary
bladder. Constriction is released via surgery
or a stent may be inserted prior to surgery
so that the urine drains out of the renal
pelvis relieving the patient from
obstruction.
Vesicoureteral Reflux (VUR)
-
Procedure that can show defect is known as
Vesico cystourethrogram (VCUG) a catheter is
inserted into the patient and dye is infused, the
dye goes to the urinary bladder, allow the patient
to void and it goes up towards the ureters.
Other post renal causes:
Duplication Anomalies
-Double ureters in one kidney
Weigert-Meyer rule
Upper pole of the kidney is drained by the
ectopic ureter w/c inserts inferomedially at
the urinary bladder (below the normal ureter)
Lower pole of the kidney is drained by normal
ureter
Upper pole hydroureteronephrosis
Ureterocele or ectopic ureter
Lower moiety reflux
Congenital CNS disorders
Voiding disturbances such as in a patient with
Kidney of newborns usually affected
Abnormal flow of urine from bladder to upper
urinary tract
A form of postrenal cause of AKI
Problem: abnormal anatomic insertion of ureter
to urinary bladder; thus, urine goes back to the
ureter
VUR grades:
Grade 1: urine reflux only into ureter w/o
any distension
Grade 2: urine reflux into ureter & renal
pelvis, still w/o any dilation
Grade 3: moderate dilation of ureter & renal
pelvis
Grade 4: dilation of renal pelvis & calyces w/
moderate ureteral tortousity
Grade 5: gross dilation of renal pelvis &
calyces & blunting of fornices
*Grades 1-3 are prone to UTI, treated with
antibiotic and urinary prophylaxis
*Grades 4 & 5 are operable: correct the insertion
of the ureter to the urinary bladder. Some degree
of renal failure may occur unless corrected by
surgery. Renal scarring will be present affecting
renal function, decreased number of nephrons
neurogenic bladder where in catheter is inserted
intermittently to drain the urine or else urine
refluxes to the kidney that leads renal function
compromise.
Dysplasias may cause pseudo obstructive
nephropathies
Myelodysplasia
Vertebral column anomalies that affect
primarily the lumbar and sacral segment of
the spinal cord
Urogenic bladder: no control of voiding
patterns
II. CHRONIC RENAL FAILURE
Results from irreversible loss of large
numbers of functioning nephrons
In AKI, there is still hope of reversibility
Serious clinical symptoms often do not occur
until the number of functional nephrons falls to
at least 70% below normal
There are patients who are asymptomatic until
only 30% of their renal function remains
Patients may have a history of
Glumerulonephritis, obstructive nephropathies,
Anemia (subtle signs)
Treatment is more of supportive, preserving the
function of the remaining nephrons
Dialysis is indicated
Causes
1.
Metabolic disorders
Diabetes mellitus most common cause
[RENAL PHYSIOLOGY 2ND HOUR] February 8, 2014
2.
3.
4.
5.
6.
7.
(*usual focus of researches, some new drugs
made cause hepatotoxicity)
Amyloidosis deposition of amyloids in the
kidneys
Renal vascular disorders
Atherosclerosis - cholesterol plaque deposition
Nephroclerosis - hypertension
Immunologic disorders
Glomerulonephritis
Polyarteritis nodosa
Lupus Erythromatosus increasing in number
Infections
Pyelonephritis
Tuberculosis
Primary tubular disorders
Nephrotoxins (analgesics & heavy metals)
Urinary tract obstruction
Renal calculi
Hypertophy of the prostate
Urethral constriction
Congenital disorders
Polycystic disease
Congenital absence of kidney tissue (renal
hypoplasia)
person must be placed on dialysis (temporary
treatment) a bridge to the treatment of
transplantation(true treatment) w/ a functional
kidney to survive
Renal Replacement Therapy (2 modalities)
Peritoneal Dialysis
Uses a fluid system that is compatible w/
peritoneal fluid
Peritoneum acts as the glomerulus w/c
serves as a semi permeable membrane
Peritoneal catheter inserted in posterior cul
de sac
Exchange of solutes in peritoneum, drain
fluid after 4-6 hrs
Done every day; usually 4x a day
History taking is very important (such as
NSAIDs taken, recurrent UTI)
5 Stages of Chronic Kidney Disease (CKD)
-IRREVERIBLE renal damage staging
Stage
Creatinine
clearance
Conditions
/associated
90 or more
ml/min/1.73 m2
with risks of
developing CKD
(lupus, nephrotic
syndrome)
II
60-89 ml/min/1.73
m2 (mild)
30-59 ml/min/1.73
m2 (moderate)
15-29 ml/min/1.73
m2 (severe) S/S of
III
IV
S/s present:
encephalopathy,
uremia, HTN,
hypercalemia,
<15 ml/min/1.73 m2
(end stage)
Dialysis is indicated usually in stages IV and V
End Stage Renal Disease
Progressive deterioration of renal function and
further loss of nephrons to a point at w/c the
emodialysis
Dialyzer serves as glomerulus
[RENAL PHYSIOLOGY 2ND HOUR] February 8, 2014
Optimum prescription for dialysis should be
done 3x/week but in the Philippines,
patients usually have it 2x/ week. (45 times
allotted by Philhealth)
Kidney transplant
-Insertion is in the iliac (sa may singit)
-
Native kidney is not removed or remains due to
higher infection risks, the new kidney is attached
Wrap ups
Clearance: In a steady state condition, the
serum level if an endogeneous marker s
correlated w/ the reciprocal of the level of GFR,
making it possible to estimate GFR w/o urine
collection
AKI in the Elderly
GFR declines w/ aging (> 65 years)
Age related decline in GFR is part of normal
aging
Decreased GFR in the elderly is an independent
predictor of adverse outcomes such as death
and cardiovascular disease
Decreased GFR in elderly requires adjustment in
drug dosages as in CKD
40 years old up will have a decline in glomeruli
every year
Upon reaching 70-80 years of age, 40%
functioning nephrons remain
Age related diseases occur, adjustment of drugs
because of decreased
Increased incidence of Adult Respiratory
Distress Syndromes, Spesis, Trauma
Mortality rate increases
Independent Risk Factors for AKI in the Elderly
Hypovolemia
Hypotension
Hypoxia
Sepsis
Be wary of renal function alongside with
associated co-morbidities (such as diarrhea and
diabetes) making them vulnerable to Kidney
injury.
Modification of Diet in Renal Disease
(MDRD)
Modification of diet in renal disease equation
This equation uses the serum creatinine value
in combination w/ age, sex, and race to
estimate GFR, and therefore avoids several of
the limitations to the use of serum creatinine
value alone
NOTETAKERS:
BANIZAL, Sigrid/CHOMAPOY,
Becky/CLAUDIO, Dennis
Potrebbero piacerti anche
- Registrable and Non-Registrable Adverse ClaimsDocumento18 pagineRegistrable and Non-Registrable Adverse ClaimsJacob Castro100% (1)
- HepatosplenomegalyDocumento52 pagineHepatosplenomegalySundar NatarajanNessuna valutazione finora
- CVS ExaminationDocumento72 pagineCVS ExaminationPrashanthBhatNessuna valutazione finora
- Ishemic Heart Disease-y-II-2011 (Student Version)Documento51 pagineIshemic Heart Disease-y-II-2011 (Student Version)kays30002403Nessuna valutazione finora
- Assessment or Acute Renal Failure SymptomsDocumento6 pagineAssessment or Acute Renal Failure SymptomsRifa Aprillia CahyaniNessuna valutazione finora
- Dyspnea and HypoxiaDocumento9 pagineDyspnea and Hypoxiadtimtiman100% (3)
- EKGDocumento31 pagineEKGJay JiangNessuna valutazione finora
- Ekg Normal Dan Acs Sudin TimurDocumento59 pagineEkg Normal Dan Acs Sudin TimurArum MaharaniNessuna valutazione finora
- CardiologyDocumento6 pagineCardiologyFrancis FransNessuna valutazione finora
- ... 4 Finals Cardiovascular PhysiologyDocumento8 pagine... 4 Finals Cardiovascular PhysiologyELIZABETH GRACE AMADORNessuna valutazione finora
- 555LDocumento8 pagine555LVictor Mamani VargasNessuna valutazione finora
- ECG Interpretations DR RPDocumento109 pagineECG Interpretations DR RPArnis Putri RosyaniNessuna valutazione finora
- Sample Child Dedication ProgramDocumento1 paginaSample Child Dedication ProgramJayricDepalobos100% (2)
- Common Histories and Red Flags Presentation Noninteractive VersionDocumento21 pagineCommon Histories and Red Flags Presentation Noninteractive VersionesmarNessuna valutazione finora
- Coronary Artery DiseaseDocumento7 pagineCoronary Artery Diseasejmar767Nessuna valutazione finora
- Ks Module 12Documento29 pagineKs Module 12jerinthomasrajanNessuna valutazione finora
- Diseases of GallbladderDocumento85 pagineDiseases of GallbladderFatima Marwa Teo MaghinayNessuna valutazione finora
- Polycystic Kidneys, A Simple Guide To The Condition, Treatment And Related DiseasesDa EverandPolycystic Kidneys, A Simple Guide To The Condition, Treatment And Related DiseasesNessuna valutazione finora
- Abdominal ExamDocumento7 pagineAbdominal Examjoshy221196Nessuna valutazione finora
- Jugular Venous Pulse: Madras Medical MissionDocumento53 pagineJugular Venous Pulse: Madras Medical MissionJoshua JayakaranNessuna valutazione finora
- Pain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Documento3 paginePain 2. Pallor Poikylothermia Parasthesia Pulselessness Factor V Leiden (Activated Protein C Resistance)Ryan TurnerNessuna valutazione finora
- Congestive Heart FailureDocumento86 pagineCongestive Heart FailureNabeel ShahzadNessuna valutazione finora
- Hyperosmolar Non Ketotic ComaDocumento23 pagineHyperosmolar Non Ketotic Comaprakash gunaNessuna valutazione finora
- Islamic Architecture PDFDocumento59 pagineIslamic Architecture PDFHarshi Garg100% (3)
- Bill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341Documento1 paginaBill To: Ship To:: 191 Sheree BLVD, Exton, PA 19341JayricDepalobosNessuna valutazione finora
- Wallenberg Syndrome: Publication DetailsDocumento9 pagineWallenberg Syndrome: Publication DetailsHuang Jen Liang100% (1)
- What's in A Birthday?: I. We Can Be Mixed Blessings To OthersDocumento2 pagineWhat's in A Birthday?: I. We Can Be Mixed Blessings To OthersJayricDepalobosNessuna valutazione finora
- Q. List Different Functions of The Kidney: (A) Homeostatic FunctionDocumento42 pagineQ. List Different Functions of The Kidney: (A) Homeostatic Functionramadan100% (4)
- JVP Examination For GPDocumento43 pagineJVP Examination For GPNovenZefanyaNessuna valutazione finora
- Eva Braun Life With Hitler PDFDocumento2 pagineEva Braun Life With Hitler PDFPamela0% (1)
- Diabetic Nephropathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDa EverandDiabetic Nephropathy, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNessuna valutazione finora
- Developing The Tourism Sector in The Sultanate of OmanDocumento18 pagineDeveloping The Tourism Sector in The Sultanate of OmanSalma Al-NamaniNessuna valutazione finora
- A Simple Guide to Gallstones and Gallbldder DiseasessDa EverandA Simple Guide to Gallstones and Gallbldder DiseasessNessuna valutazione finora
- Clinical Pastoral OrientationDocumento3 pagineClinical Pastoral OrientationJayricDepalobos100% (1)
- Cases Torts 7-29-17 DigestDocumento1 paginaCases Torts 7-29-17 Digestczabina fatima delicaNessuna valutazione finora
- "Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."Documento3 pagine"Better Is The Day of Death": Feasting: For That Is The End of All Men and The Living Will Lay It To His Heart."JayricDepalobosNessuna valutazione finora
- Epilepsy and Seizure DisordersDocumento38 pagineEpilepsy and Seizure DisordersMalueth AnguiNessuna valutazione finora
- Approach To HematuriaDocumento45 pagineApproach To HematuriaArun GeorgeNessuna valutazione finora
- HUA 3G Capacity OptimizationDocumento39 pagineHUA 3G Capacity Optimizationismail_hw91% (11)
- Neurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Documento10 pagineNeurologic Emergencies Stroke & Tia: Devin R. Harris, MD MHSC CCFP (Em)Samantha Lui100% (2)
- Abdominal TB: A.Kirit Junior Resident Surgery AiimsDocumento29 pagineAbdominal TB: A.Kirit Junior Resident Surgery Aiimsranjan kumar100% (1)
- MBA Advantage LRDocumento304 pagineMBA Advantage LRAdam WittNessuna valutazione finora
- Heart Failure RevisionDocumento4 pagineHeart Failure RevisionBlanaid MargaretNessuna valutazione finora
- Cardiac Examination Inspection, Palpation & Percussion : Dr. Rajesh Bhat UDocumento38 pagineCardiac Examination Inspection, Palpation & Percussion : Dr. Rajesh Bhat URanjith RavellaNessuna valutazione finora
- Renal Physiology IDocumento16 pagineRenal Physiology IJubilee Christiene AngNessuna valutazione finora
- An Overview Of: Acute Kidney Injury (Aki: Hasan BasriDocumento22 pagineAn Overview Of: Acute Kidney Injury (Aki: Hasan BasriDz PutraNessuna valutazione finora
- Virus MnemonicDocumento2 pagineVirus MnemonicTatum CheneyNessuna valutazione finora
- VQ - O2 GradientDocumento27 pagineVQ - O2 GradientIkbal NurNessuna valutazione finora
- Arrhythmias + Pharmacology: Mechanism of ArrhythmiaDocumento10 pagineArrhythmias + Pharmacology: Mechanism of ArrhythmiaJuliana Ching Joo LimNessuna valutazione finora
- Kidney AnatomyDocumento2 pagineKidney Anatomyameerabest100% (1)
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocumento4 pagineRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniNessuna valutazione finora
- Anatomy of StomachDocumento4 pagineAnatomy of StomachIntan Putri Maisarah100% (1)
- Renal Laboratory TestsDocumento2 pagineRenal Laboratory TestsRitz CelsoNessuna valutazione finora
- GastrointestinalDocumento104 pagineGastrointestinalNugroho AnisNessuna valutazione finora
- Peripheral Vascular System ExaminationDocumento2 paginePeripheral Vascular System ExaminationKay Bristol100% (1)
- Cardio Physiology FullDocumento11 pagineCardio Physiology FullSara Lee Wei LiNessuna valutazione finora
- Tubular Functions of KidneyDocumento161 pagineTubular Functions of KidneyPhysiology by Dr RaghuveerNessuna valutazione finora
- Newsletter v5n2Documento92 pagineNewsletter v5n2Transverse Myelitis AssociationNessuna valutazione finora
- Nonalcoholic Fatty Liver Disease (NAFLD) : Where Are We Today?Documento32 pagineNonalcoholic Fatty Liver Disease (NAFLD) : Where Are We Today?Saad MotawéaNessuna valutazione finora
- Notes in Physiology 2nd PDFDocumento37 pagineNotes in Physiology 2nd PDFDany SamuelNessuna valutazione finora
- Meds For HypertensionDocumento3 pagineMeds For HypertensionZonicsNessuna valutazione finora
- DKA Draft 1 AM - Drawio 2Documento1 paginaDKA Draft 1 AM - Drawio 2Dud AccNessuna valutazione finora
- 20 - Toronto Notes 2011 - Ophthamology PDFDocumento46 pagine20 - Toronto Notes 2011 - Ophthamology PDFSisterzzShopDua0% (1)
- Obstetrics Cases by Caroline de CostaDocumento9 pagineObstetrics Cases by Caroline de CostaJeffrey HingNessuna valutazione finora
- Cme Fluid and Electrolytes 2902016Documento37 pagineCme Fluid and Electrolytes 2902016Mohd Faie Ramli0% (1)
- CH 11 Heart NotesDocumento2 pagineCH 11 Heart Notesummnicole0% (1)
- Pancreatic CancerDocumento25 paginePancreatic CancerAatir JavaidNessuna valutazione finora
- ASCITESDocumento25 pagineASCITESGanesh BabuNessuna valutazione finora
- AnaemiaDocumento83 pagineAnaemiaMohammad_Islam87100% (2)
- Department of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaDocumento39 pagineDepartment of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaAvanti ShendurjaneNessuna valutazione finora
- Behavioral FinalsDocumento28 pagineBehavioral FinalsKofiBNessuna valutazione finora
- Cardiac Arrhythmia: Prepared By: Charina Gail O. Baloy, RPH, Msc. (C.)Documento44 pagineCardiac Arrhythmia: Prepared By: Charina Gail O. Baloy, RPH, Msc. (C.)Chinenye Akwue100% (1)
- PP Drug Classes and IndicationsDocumento67 paginePP Drug Classes and IndicationspninthemakinNessuna valutazione finora
- FWD: Schedule Change AdvisoryDocumento2 pagineFWD: Schedule Change AdvisoryJayricDepalobosNessuna valutazione finora
- Shipping Confirmation 1264941Documento1 paginaShipping Confirmation 1264941JayricDepalobosNessuna valutazione finora
- The LightDocumento2 pagineThe LightJayricDepalobosNessuna valutazione finora
- Conjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisDocumento13 pagineConjunctivitis (Inclusion) Vs Acute Bacterial ConjunctivitisJayricDepalobosNessuna valutazione finora
- Chapter 01 ChoicesDocumento9 pagineChapter 01 ChoicesJayricDepalobosNessuna valutazione finora
- Medical Ward 1 Service 2 CensusDocumento13 pagineMedical Ward 1 Service 2 CensusJayricDepalobosNessuna valutazione finora
- YHH Strategic Plan 2016-2017Documento5 pagineYHH Strategic Plan 2016-2017JayricDepalobosNessuna valutazione finora
- Acquaintance Party ParticipantsDocumento1 paginaAcquaintance Party ParticipantsJayricDepalobosNessuna valutazione finora
- CAA Concert ProgramDocumento2 pagineCAA Concert ProgramJayricDepalobosNessuna valutazione finora
- Thalassemia: Presentor: Don Jayric DepalobosDocumento19 pagineThalassemia: Presentor: Don Jayric DepalobosJayricDepalobosNessuna valutazione finora
- Teen Parenting Brochure AssignmentDocumento1 paginaTeen Parenting Brochure AssignmentJayricDepalobosNessuna valutazione finora
- Peer Evaluation For Group 5Documento1 paginaPeer Evaluation For Group 5JayricDepalobosNessuna valutazione finora
- Acute Gastroenteritis: By: Madhavi Pandya Priyanka NandiDocumento16 pagineAcute Gastroenteritis: By: Madhavi Pandya Priyanka NandiJayricDepalobosNessuna valutazione finora
- Parasitology 18 Lung FlukesDocumento25 pagineParasitology 18 Lung FlukesJayricDepalobosNessuna valutazione finora
- Female BW - 3800 BL - 55 AS - 8,9 PA - 40Documento3 pagineFemale BW - 3800 BL - 55 AS - 8,9 PA - 40JayricDepalobosNessuna valutazione finora
- Microbiology Lecture Series Luz Gregoria Lazo-Velasco, MDDocumento105 pagineMicrobiology Lecture Series Luz Gregoria Lazo-Velasco, MDJayricDepalobos100% (1)
- Basic Physical Examination in ENT PDFDocumento44 pagineBasic Physical Examination in ENT PDFJayricDepalobosNessuna valutazione finora
- Department of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017Documento1 paginaDepartment of Community & Family Medicine Md-Dcfmc-046-O1: CBHP June 01, 2017JayricDepalobosNessuna valutazione finora
- AKSINDO (Mr. Ferlian), 11 - 13 Mar 2016 (NY)Documento2 pagineAKSINDO (Mr. Ferlian), 11 - 13 Mar 2016 (NY)Sunarto HadiatmajaNessuna valutazione finora
- Low Steam Cane - Almoiz Industries Road To SuccessDocumento9 pagineLow Steam Cane - Almoiz Industries Road To SuccessArif ShafiNessuna valutazione finora
- VB Knowledge Buying A Home Flashcards QuizletDocumento1 paginaVB Knowledge Buying A Home Flashcards QuizletSavaya CrattyNessuna valutazione finora
- Fume Cup BrochureDocumento2 pagineFume Cup Brochuremfisol2000Nessuna valutazione finora
- ERF 2019 0128 H160 Noise CertificationDocumento10 pagineERF 2019 0128 H160 Noise CertificationHelimanualNessuna valutazione finora
- Fiche 2 ConnexionsDocumento2 pagineFiche 2 ConnexionsMaria Marinela Rusu50% (2)
- Business Communication and Behavioural StudiesDocumento10 pagineBusiness Communication and Behavioural StudiesBhujangam NaiduNessuna valutazione finora
- The Fat Cat Called PatDocumento12 pagineThe Fat Cat Called PatAlex ArroNessuna valutazione finora
- Chapter 1: Introduction Aviation Industry: Mini Project On Vistara AirlinesDocumento84 pagineChapter 1: Introduction Aviation Industry: Mini Project On Vistara Airlinesselvaraj rapakaNessuna valutazione finora
- The Mystery of The Secret RoomDocumento3 pagineThe Mystery of The Secret RoomNur Farhana100% (2)
- Emilio Aguinaldo: The First Philippine Republic The Malolos CongressDocumento3 pagineEmilio Aguinaldo: The First Philippine Republic The Malolos CongressLIEZLE ANN EROYNessuna valutazione finora
- Eliminate Zombie Nouns and Minimize Passive Voice: Plain LanguageDocumento2 pagineEliminate Zombie Nouns and Minimize Passive Voice: Plain LanguagePădure IonuțNessuna valutazione finora
- SOAL ASSEMEN PAKET A BAHASA INGGRIS NewDocumento3 pagineSOAL ASSEMEN PAKET A BAHASA INGGRIS Newmtsn4 clpNessuna valutazione finora
- A Study of Absenteeism of Workers in Nutrine Confectionery Company LTD ChittoorDocumento69 pagineA Study of Absenteeism of Workers in Nutrine Confectionery Company LTD ChittoorShoaib MohammedNessuna valutazione finora
- Manusia LemahDocumento8 pagineManusia LemahKhoirul MubinNessuna valutazione finora
- The Watchmen Novel AnalysisDocumento10 pagineThe Watchmen Novel AnalysisFreddy GachecheNessuna valutazione finora
- Brochure For New HiresDocumento11 pagineBrochure For New HiresroseNessuna valutazione finora
- ROSEN Group - Challenging Pipeline DiagnosticsDocumento42 pagineROSEN Group - Challenging Pipeline DiagnosticsFuad0% (1)
- Kumpulan Soal UPDocumento16 pagineKumpulan Soal UPTriono SusantoNessuna valutazione finora
- Online Book Store System: Bachelor of Computer EngineeringDocumento31 pagineOnline Book Store System: Bachelor of Computer Engineeringkalpesh mayekarNessuna valutazione finora
- Heredity and Variation IDocumento21 pagineHeredity and Variation Ismbdy tbhhhNessuna valutazione finora
- Amma Vun - Bala AshtagamDocumento4 pagineAmma Vun - Bala AshtagamSHIV RAMNessuna valutazione finora