Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
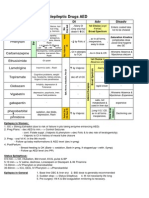
Anticholinergic Drugs
Caricato da
AmikyDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Anticholinergic Drugs
Caricato da
AmikyCopyright:
Formati disponibili
-
CHOLINERGIC AGONISTS
Agonist INITIATES A CHOLINERGIC RESPONSE
A. Direct Acting
1. Acetylcholine
2. Bethanecol
3. Carbachol
4. Pilocarpine
Oral: treatment of decreased salivation accompanying
4.
Pyridostigmine and ambenonium
Chronic management of MG
Duration of action are intermediate (3-6, 4-8 hours)
5.
Tacrine, donzepezil, rivastigmine, galantamine
Alzheimers delay progression
Adverse effect: GI distress
head and neck irradiation
B. Indirect Acting (ACETYLCHOLINESTERASE INHIBITOR);
Reversible
1.
Edrophonium
Used in diagnosis of MG: which is an autoimmune
disease caused by antibodies to the nicotinic receptor
-
at NMJs
There is degradation resulting in fewer receptors
available for interaction with neurotransmitters
IV: rapid increase in muscle strength: may provoke
cholinergic crisis:
o Atropine is the antidote
Used in differentiating cholinergic and myasthenic
crisis: both are marked by severe muscle weakness
Symptomatic MG treatment
Adverse effects: generalized cholinergic stimulation
C. Indirect Acting: Anticholinesterases (Irreversible)
1. Echothiopate
Open angle glaucoma
D. Organophosphate toxicity
Manifested as muscarinic and nicotinic s/sx
Nicotinic effects:
o Hypertension
o Tachycardia
o Pallor
o Mydriasis (dilation)
Management:
o Pralidoxime reactivate inhibited AChE
o Atropine prevent muscarinic effects
o Diazepam
o General supportive measures
and difficulty breathing
o Myasthenic crisis: worsening of condition
Respiratory distress
Dysphagia
Dysarthria
Ptosis, diplopia
Prominent muscle weakness
Management:
Intubation, NGT
ABGs, Serum electrolytes,
I/O, daily weight
CPPT, suctioning
Avoid sedatives and
tranquilizers aggravate
hypoxia and hypercapnea
further respi and cardiac
CHOLINERGIC ANTAGONISTS
depression
Cholinergic crisis: overdose of
parasympatholytics, anticholinergic drugs)
anticholinesterase drugs
A.
2.
3.
Physostigmine
Increase intestinal and bladder motility
Ophthalmic: miosis and spasms of accommodation
Used in overdose of anticholinergics: atropine,
TCA,phenothiazines
Neostigmine
Also known as: cholinergic blockers,
Antimuscarinic Agents
Selectively blocks muscarinic receptors: action of
-
1.
sympathetic stimulation are unopposed
Inhibits all muscarinic functions
Atropine
2.
Persistent dilation of the pupil, unresponsiveness to
light, cyclopegia (inability to focus for near vision)
o Tx: narrow angle glaucoma
o Phenylephrine is favored over atropine
Reduced GI motility, but Hcl production is not
Used in enuresis among children
Produces xerostomia
Antidote for cholinergic agonists
Side effects:
o Dry mouth
o Blurred vision
o Sandy eyes
o Tachycardia
o Urinary retention
o Constipation
CNS effects:
o Restlessness
o Confusion
o Delirum
o Hallucination
Physostigmine overcome atropine toxicity
Ipratropium and tiotropium
Bronchodilators
Tiotropium: once daily vs. ipra (4x)
Inhalation
4.
Tropicamide and cyclopentolate
Ophthalmic solution of mydriasis and cyclopegia
5.
Benztropne and trihexyphenidyl
Adjuncts to antiparkinsonian agents
B.
C.
Darifenacin, fesoterodine, oxybutynin, solifenacin,
tolterodine, and trospium chloride
Treat overactive urinary bladder disease
Ganglionic Blockers
1. Nicotine
2. Mecamylamine
Neuromuscular Blockers
Interfere with transmission of Efferent impulses to
skeletal muscles; muscle relaxant adjuvants
1.
o
-
Nonpolarizing Agents
Mechanism of action:
excitatory)
High doses: complete blockade, no direct
electrical stimulation
Action: FIRST TO LAST AFFECTED:
o Face and eyes muscles small rapidly
contracting
o Fingers
o Limbs
o Neck and trunk
o ICS
o Diaphragm
Reversal: recovery
Mode: IV only, terminated by redistribution not
metabolized
AE: generally safe with minimal SE
Drug interactions:
o Halothane decrease the effect
o Calcium channel blockers and
aminoglycoside antibiotics: increase the
a.
and blocking short term memory
More effective prophylactially
Adjunct in anesthetic procedures
3.
Low doses: Prevent binding of Ach inhibits
muscular contraction (remember that ACh is
Scopolamine
Anti-motion sickness drug
May produce euphoria abuse
Indications: limited to prevention of motion sickness
-
6.
effect
Cistracurium
i. Spontaeously degrades in plasma
ii. Dose need not be reduced in renal
iii.
failure
Used in MOSF metabolism is
independent of renal and hepatic
b.
c.
d.
e.
2.
function
Pancuronium vagolytic (increase HR)
Rocuronium
Tubocurarine
Vecoronium
Polarizing Agents
a. Succinylcholine
i. Common SE: post-op muscle pain
ii. Hyperkalemia and increased IOP and
iv.
intragastric pressure may occur
May trigger malignant hyperthermia
1. Cool patient
2. Administer dantrolene
Indicated if rapid intubation is necessary,
v.
esp if patient has gastric contents
Rapid onset, brief duration, usually given
iii.
continuous infusion
ADRENERGIC AGONISTS
A.
Catecholamines:
1. Epinephrine
2. Norepinephrine
3. Isoproterenol
4. Dopamine
5.
Characteristics of catecholamines:
1.
2.
3.
B.
1.
2.
3.
High potency
Rapid inactivation (IV, never PO)
Do not penetrate CNS
Noncatecholamines
Have longer half-lives
Phenylepinephrine
Ephedrine
Amphetamine
Potrebbero piacerti anche
- Cholinergics and AnticholinergicsDocumento5 pagineCholinergics and AnticholinergicscatislandbigredNessuna valutazione finora
- Electrolyte ImbalanceDocumento3 pagineElectrolyte ImbalancemewilkinNessuna valutazione finora
- Ninja - Anti-HTN PDFDocumento6 pagineNinja - Anti-HTN PDFErica Hyeyeon Lee100% (2)
- Basic Principles of PharmacologyDocumento13 pagineBasic Principles of Pharmacologyemmanuel100% (1)
- Mishba +pharmacology + Tapan ShahDocumento232 pagineMishba +pharmacology + Tapan ShahRaushan BlakeNessuna valutazione finora
- Hmg-Coa Reductase Inhibitors (Statins) : Side Effects, Contraindications, InteractionsDocumento6 pagineHmg-Coa Reductase Inhibitors (Statins) : Side Effects, Contraindications, Interactionswaste78Nessuna valutazione finora
- Bmed Concept MapDocumento2 pagineBmed Concept Mapapi-247954649Nessuna valutazione finora
- Electrolyte Mnemonic QuizletDocumento3 pagineElectrolyte Mnemonic QuizletA.h.Murad100% (2)
- Pharmacology CNS DrugsDocumento15 paginePharmacology CNS DrugsM Youssif Elkady100% (1)
- Cardiovascular Pharmacology OutlineDocumento11 pagineCardiovascular Pharmacology OutlineLhay de OcampoNessuna valutazione finora
- OB Drug ChartsDocumento2 pagineOB Drug ChartsNursingSchoolNotesNessuna valutazione finora
- H Hemolysis E Elevated L Liver Function L Low P Platelet B Breast U Uterus B Bowel B Bladder L Lochia E Episiotomy H HemorrageDocumento7 pagineH Hemolysis E Elevated L Liver Function L Low P Platelet B Breast U Uterus B Bowel B Bladder L Lochia E Episiotomy H HemorrageAlexNessuna valutazione finora
- Antianginal DrugsDocumento3 pagineAntianginal DrugsyukariNessuna valutazione finora
- DRUGS Flash CardsDocumento9 pagineDRUGS Flash Cardsdrp2011Nessuna valutazione finora
- Pharmacology FirecrackerDocumento37 paginePharmacology FirecrackerRehan Usman100% (1)
- Comprehensive Pharmacology Study NotesDocumento123 pagineComprehensive Pharmacology Study NotesEdil M Jama100% (1)
- Drug ChartDocumento8 pagineDrug Chartstudentalwaysstudy100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- Ninja - Cholinergic Drugs PDFDocumento4 pagineNinja - Cholinergic Drugs PDFErica Hyeyeon Lee100% (2)
- Template Drug Card1Documento1 paginaTemplate Drug Card1Kay TaylorNessuna valutazione finora
- Anti-Arrhythmic Agents For Pharmacy PDFDocumento41 pagineAnti-Arrhythmic Agents For Pharmacy PDFKelvinTMaikanaNessuna valutazione finora
- NSAIDS and SteroidsDocumento2 pagineNSAIDS and Steroidsmed testNessuna valutazione finora
- Cardiovascular Drugs XL ChartDocumento4 pagineCardiovascular Drugs XL Chartcdp158767% (3)
- Receptor Pharmacology Cheat Sheet (4f6203b546fa5)Documento5 pagineReceptor Pharmacology Cheat Sheet (4f6203b546fa5)sinthreckNessuna valutazione finora
- Grapefruit Juice and Drug Interactions - 0717Documento2 pagineGrapefruit Juice and Drug Interactions - 0717Asri YaniNessuna valutazione finora
- Pathophysiology of Endocrine SystemDocumento64 paginePathophysiology of Endocrine SystemTess MohamedNessuna valutazione finora
- Pharmacology Notes (Chapter 20 and 21)Documento2 paginePharmacology Notes (Chapter 20 and 21)graycorypNessuna valutazione finora
- Antiepileptic Drugs AED: D' DI Disadv SE AdvDocumento1 paginaAntiepileptic Drugs AED: D' DI Disadv SE Advrayooona88Nessuna valutazione finora
- Autonomic DrugsDocumento107 pagineAutonomic DrugsMaria Mercedes LeivaNessuna valutazione finora
- O Insert Picture Here From Slide: Heart Failure Heart FailureDocumento4 pagineO Insert Picture Here From Slide: Heart Failure Heart FailureAlec Xavier MirandaNessuna valutazione finora
- Endocrine DisordersDocumento5 pagineEndocrine DisordersBilly Ray VillanuevaNessuna valutazione finora
- Ninja - Autacoids PDFDocumento3 pagineNinja - Autacoids PDFErica Hyeyeon LeeNessuna valutazione finora
- Agents Causing Coma or SeizuresDocumento3 pagineAgents Causing Coma or SeizuresShaira Aquino VerzosaNessuna valutazione finora
- ENDOCRINE NURSING-FINAL HDDocumento15 pagineENDOCRINE NURSING-FINAL HDJayvee Novenario Casaljay100% (1)
- Electrolytes ImbalancesDocumento4 pagineElectrolytes ImbalancesPeter John Ruiz100% (1)
- Opioids PDFDocumento2 pagineOpioids PDFErica Hyeyeon LeeNessuna valutazione finora
- Onco PharmacologyDocumento9 pagineOnco Pharmacologyarn0ld21Nessuna valutazione finora
- Cholinergics and Cholinergic BlockersDocumento5 pagineCholinergics and Cholinergic Blockersapi-3739910100% (3)
- NERVOUS MnemonicsDocumento4 pagineNERVOUS MnemonicsHimNessuna valutazione finora
- Cholinergic Drug MnemonicsDocumento1 paginaCholinergic Drug Mnemonicssunshine151100% (1)
- Common Drug Stems Cheat Sheet: Drug Stem Drug Class And/or Stem Explanation ExamplesDocumento2 pagineCommon Drug Stems Cheat Sheet: Drug Stem Drug Class And/or Stem Explanation ExamplesjthsNessuna valutazione finora
- Diabetes Treatment: PancreatitisDocumento2 pagineDiabetes Treatment: PancreatitisSafiya JamesNessuna valutazione finora
- CholestyramineDocumento1 paginaCholestyramineKatie McPeekNessuna valutazione finora
- FAELDONEA - B. Concept MapDocumento1 paginaFAELDONEA - B. Concept MapPatricia Jean FaeldoneaNessuna valutazione finora
- Musculoskeletal PharmacologyDocumento18 pagineMusculoskeletal PharmacologyBLEEMAGE100% (2)
- Nursing Pharmacology Inflammation Study GuideDocumento11 pagineNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Ninja - Anemias PDFDocumento1 paginaNinja - Anemias PDFErica Hyeyeon LeeNessuna valutazione finora
- Cardiac Drugs HypertensionDocumento5 pagineCardiac Drugs HypertensionEciOwnsMeNessuna valutazione finora
- LasixDocumento1 paginaLasixKatie McPeek100% (2)
- Hormones and Related DrugsDocumento42 pagineHormones and Related DrugsRamya PrabhuNessuna valutazione finora
- PharmacologyDocumento35 paginePharmacologyJan Michael ArtiagaNessuna valutazione finora
- Endocrine DisordersDocumento27 pagineEndocrine Disordersasdfgrttt100% (4)
- Fluids and ElectrolytesDocumento9 pagineFluids and ElectrolytesAlvin Jay DacilloNessuna valutazione finora
- EndocrineDocumento2 pagineEndocrineUnclePorkchopNessuna valutazione finora
- Summary of Adrenergic DrugsDocumento3 pagineSummary of Adrenergic DrugsrabduljabarrNessuna valutazione finora
- Dysrhythmias Cheat SheetDocumento2 pagineDysrhythmias Cheat SheetKandice ChandlerNessuna valutazione finora
- Ninja - Antihyperlipidemics PDFDocumento3 pagineNinja - Antihyperlipidemics PDFErica Hyeyeon Lee100% (1)
- Anticholinergic: Anticholinergics: Generic and Brand NamesDocumento6 pagineAnticholinergic: Anticholinergics: Generic and Brand NamesSaffery Gly LayuganNessuna valutazione finora
- Dr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityDocumento41 pagineDr. Jagan Associate Professor of Pharmacology HOD - para Clinical Department Texila American UniversityredderdatNessuna valutazione finora
- 7 - Cholinomimetic DrugsDocumento50 pagine7 - Cholinomimetic DrugslalitrajindoliaNessuna valutazione finora
- Corelation of The Changes Between The Iridocorneal - Angle and Other Paramet E Rs at The Neovascular GlaucomaDocumento25 pagineCorelation of The Changes Between The Iridocorneal - Angle and Other Paramet E Rs at The Neovascular GlaucomaAJVAZI100% (1)
- hdf492 Portfolio PresentationDocumento14 paginehdf492 Portfolio Presentationapi-403412647Nessuna valutazione finora
- Heart PDFDocumento48 pagineHeart PDFdr.chetan2385Nessuna valutazione finora
- CSR Activities - Hygiene and SanitationDocumento14 pagineCSR Activities - Hygiene and SanitationFinplus IndiaNessuna valutazione finora
- Child Safety PDFDocumento240 pagineChild Safety PDFVaibhav AgarwalNessuna valutazione finora
- Soal Bahasa Inggris SBMPTN 2003Documento3 pagineSoal Bahasa Inggris SBMPTN 2003soe_barn64Nessuna valutazione finora
- Syllabus FOR: AIAPGET 2023Documento5 pagineSyllabus FOR: AIAPGET 2023Rahul KirkNessuna valutazione finora
- Microbiology at A GlanceDocumento126 pagineMicrobiology at A GlanceMuhammad UsmanNessuna valutazione finora
- How To Use Akpi Seed For Hips, Butts and Breasts EnlargementDocumento5 pagineHow To Use Akpi Seed For Hips, Butts and Breasts EnlargementLinda PrideNessuna valutazione finora
- Clinical Neuroscience Psychopathology and The Brain 2Nd Edition Full ChapterDocumento41 pagineClinical Neuroscience Psychopathology and The Brain 2Nd Edition Full Chapterwilliam.kellar832100% (20)
- Philippine Navy Naval Installation Command Naval Installation and Facilities-National Capital RegionDocumento9 paginePhilippine Navy Naval Installation Command Naval Installation and Facilities-National Capital RegionDuchesne San JoseNessuna valutazione finora
- Desain GTSL SangryDocumento53 pagineDesain GTSL SangrySanggry Mutiara PardedeNessuna valutazione finora
- TDSB GR 9-12 Student Census, 2022Documento31 pagineTDSB GR 9-12 Student Census, 2022True NorthNessuna valutazione finora
- Technology and Its Negativity: English For Academic and Professional Purposes Performance Task 2: Position PaperDocumento2 pagineTechnology and Its Negativity: English For Academic and Professional Purposes Performance Task 2: Position PaperAlliah MatozaNessuna valutazione finora
- Estethic DentistreDocumento639 pagineEstethic DentistreAdrian Venegas Melo100% (1)
- BIO210 Infomation 7Documento5 pagineBIO210 Infomation 7Rex BrazilNessuna valutazione finora
- Critical Movie Review Template # 1: General InstructionsDocumento3 pagineCritical Movie Review Template # 1: General InstructionsNicole MilanNessuna valutazione finora
- Google Forms Survey Sample H.S.B SBA 2023Documento8 pagineGoogle Forms Survey Sample H.S.B SBA 2023Brianna ChuramanNessuna valutazione finora
- Health 7: Learner'S Instructional MaterialDocumento14 pagineHealth 7: Learner'S Instructional MaterialGeneNessuna valutazione finora
- COMSECXDocumento5 pagineCOMSECXJoseph CruzNessuna valutazione finora
- Rpms Evaluation For School Head (Mov'S / Mfo'S)Documento5 pagineRpms Evaluation For School Head (Mov'S / Mfo'S)Laiza Niña Gimenez LariegoNessuna valutazione finora
- Learner DiversityDocumento1 paginaLearner DiversityHenry Buemio100% (1)
- Memorandum: Philippine National Police Training Institute Regional Training Center 8Documento2 pagineMemorandum: Philippine National Police Training Institute Regional Training Center 8DUN SAMMUEL LAURENTENessuna valutazione finora
- Ketones &ketone Urine Test - Purpose, Procedure, ResutlsDocumento6 pagineKetones &ketone Urine Test - Purpose, Procedure, ResutlsEiann Jasper LongcayanaNessuna valutazione finora
- Review Jurnal Bunga Aurelia (18621005)Documento3 pagineReview Jurnal Bunga Aurelia (18621005)bungaNessuna valutazione finora
- Borderline and Histrionic Personality DisordersDocumento38 pagineBorderline and Histrionic Personality DisordersSahel100% (1)
- Pola 2017Documento10 paginePola 2017RobertoNessuna valutazione finora
- Paridhi English LanguageDocumento7 pagineParidhi English LanguageKasturi GhoshNessuna valutazione finora
- MS Civil Engineering Construction and Safety Management Assignment No. 1 MCE191010 Abdur RehmanDocumento5 pagineMS Civil Engineering Construction and Safety Management Assignment No. 1 MCE191010 Abdur RehmanAbdur RehmanNessuna valutazione finora
- Respect in The Workplace: The Management of Disrespectful ConductDocumento8 pagineRespect in The Workplace: The Management of Disrespectful ConductHP w1907Nessuna valutazione finora