Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
R20 PDF
Caricato da
fenec3000Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
R20 PDF
Caricato da
fenec3000Copyright:
Formati disponibili
ORIGINAL ARTICLE
Leveling the curve of Spee with a continuous
archwire technique: A long term
cephalometric study
Rael L. Bernstein,a Charles B. Preston,b and Judith Lampassoc
Buffalo, NY
Introduction: The orthodontic technique favored by a clinician frequently determines how a deep curve of
Spee (COS) is leveled. The primary purpose of this investigation was to confirm radiographically the
long-term effectiveness of a continuous archwire techniquethe Alexander disciplinein leveling the COS
in patients with Class II Division 1 deep-bite malocclusions treated without extractions. Methods: The sample
for this retrospective cephalometric study consisted of the randomly selected orthodontic records of 31 subjects
(22 female, 9 male) treated with the continuous archwire technique in the private practice of Dr R.G. Wick
Alexander in Arlington, Texas. Results: The mean pretreatment COS for this sample was 2.47 mm, and the
corresponding mean posttreatment COS was 0.19 mm. The COS was completely level in 21 patients after
treatment, and the rest had slight residual COS at the end of this phase. Ten of the 31 subjects remained level
from 5 to 25 years after orthodontic treatment. Conclusions: The results indicate that most leveling was
accomplished by the extrusion of the premolars. The continuous archwire technique is effective in leveling the
COS in patients with Class II Division 1 deep-bite malocclusions treated without extractions when the initial COS
is 2 to 4 mm. The leveling of the COS with the continuous archwire technique takes place by a combination of
premolar extrusion and, to a lesser extent, incisor intrusion. (Am J Orthod Dentofacial Orthop 2007;131:363-71)
he need to correct an accentuated curve of Spee
(COS) that is commonly encountered in a malocclusion characterized by a deep bite presents
diagnostic and therapeutic challenges for the orthodontist.1,2 Unfortunately, the orthodontic technique favored
by each clinician, rather than the nature of a specific
malocclusion, will frequently determine how deep bites
are corrected. There is some disagreement among the
proponents of the various orthodontic techniques as to
what mechanical approach is the most suitable to level
an exaggerated COS.3-5 Clinicians who follow a segmented wire approach to arch leveling suggest that
leveling with continuous archwires will extrude the
posterior teeth, which, in turn, will result in increased
lower facial height.3-7 They also believe that, in patients
with strong muscles of mastication, the extrusion of the
buccal segments will tend to relapse after orthodontic
treatment. Furthermore, these clinicians believe that
placing a reverse COS in a continuous archwire for arch
a
Private practice, Calif.
Professor and chair, School of Dental Medicine, University at Buffalo.
c
Assistant professor, School of Dental Medicine, University at Buffalo.
Reprint requests to: Charles B. Preston, School of Dental Medicine, State
University of New York at Buffalo, 140 Squire Hall, 3435 Main St, Buffalo,
NY 14214; e-mail, cbp@buffalo.edu
Submitted, February 2005; revised and accepted, May 2005.
0889-5406/$32.00
Copyright 2007 by the American Association of Orthodontists.
doi:10.1016/j.ajodo.2005.05.056
b
leveling will almost always flare the mandibular incisors labially.8,9 On the other hand, proponents of the
continuous-arch treatment philosophy contend that premolar and molar extrusions represent stable occlusal
changes, whereas mandidular incisor intrusion is an
unstable movement that will almost certainly relapse in
time.6,7,10-16
Cephalometric studies undertaken to compare the
sectional and continuous arch leveling methods report
that both the Ricketts4 and the modified Tweed5 techniques successfully correct deep overbites. At the same
time, a comparative study of these 2 approaches to
orthodontic treatment found that they result in similar
mandibular incisor positions.17
In support of the contention that it is important to
level an excessive COS, Andrews18 noted that the
occlusal planes of nonorthodontically treated normal
occlusions tend to be level. He associated a COS with
postorthodontic treatment relapse and concluded that,
even though not all normal occlusions have flat planes
of occlusion, this should be an orthodontic treatment
goal. Because of the tendency for the COS to return
after orthodontic treatment, other authors in support of
Andrews point of view suggest that it should be an aim
of orthodontic treatment to establish a level occlusal
plane.19,20
Several authors commented on the amount and
363
364 Bernstein, Preston, and Lampasso
American Journal of Orthodontics and Dentofacial Orthopedics
March 2007
Table I. Sample (n 31; 9 male, 22 female) and time
characteristics
Characteristic
Mean
Mean
Mean
Mean
Mean
Mean
age at T1
age at T2
age at T3
treatment time (T2-T1)
fixed retention time
postretention time (T3-T2)
Time
12
14
26
2
3
11
y
y
y
y
y
y
6 mo
11 mo
4 mo
5 mo
4 mo
5 mo
type of occlusal relapse after orthodontic treatment.3,12,17,21-30 In general, these studies noted increases in overjet, overbite, and mandibular incisor
crowding along with decreases in arch length and arch
width. Although postorthodontic relapse was studied in
some detail, relatively little is known about the longterm stability of leveling the COS and how the different
methods of arch leveling relate to its subsequent relapse.
The primary purpose of this investigation was to
determine radiographically the long-term effectiveness
of the Alexander discipline (continuous archwire technique) in leveling the COS in Class II Division 1
deep-bite nonextraction patients. We also report on
some relevant cephalometric changes that take place
during arch leveling with the continuous archwire
technique. The cephalometric data obtained were used
to determine whether a COS that was leveled remains
stable in the long term.
MATERIAL AND METHODS
The sample for this retrospective study consisted of
the randomly selected orthodontic records of 31 white
patients treated without extractions in the private practice of Dr R.G. Wick Alexander in Arlington, Texas
(Table I). These patients all met the following criteria
for selection: they had Class II (ANB angle 4)
skeletal patterns, at least half-step Class II molar dental
relationships, incisor overbites of 50% or greater as
measured on the initial (T1) study models, and angles
between the mandibular plane (MP) (Go-Gn) and the
sella-nasion (S-N) line less than 32. A COS equal to or
deeper than 2 mm was present on all T1 models.
Only patients with complete clinical records were
included in this study. These records consisted of
radiographs and dental casts taken at T1, posttreatment
(T2), and postretention (T3). All patients were retained
with lower fixed canine-to-canine lingual retainers for a
mean period of 3 years 4 months. The patients were all
treated with fully preadjusted fixed orthodontic appliances according to the continuous archwire technique.
We selected this technique for this study because of its
Fig 1. Cephalometric landmarks and lines.
biomechanical principles that aim to provide a level
occlusal plane (OP) during and at the end of active
treatment.31
Three radiographs (T1, T2, T3) were collected for
each subject. The 93 radiographs were assigned random
numbers to enable 1 investigator (R.L.B.) to measure
each in a random, blind fashion.
All radiographs were taken on a Quint Sectograph
machine (Los Angeles, Calif) and were hand traced by
1 operator (R.L.B.) from the original radiographs.
Standard cephalometric landmarks (S, N, ANS, PNS,
A, B, Go, Gn) were used to construct the reference lines
required to obtain the craniofacial measurements recorded in this study (Fig 1).32 The functional OP was
defined by a line intersecting the intercuspation of the
posterior occlusion (Fig 2).33 The following additional
reference points and planes were used to measure the
COS; these form the focus of this study (Figs 1 and 2):
I1, the incisal tip of the most extruded mandibular
incisor; L6, the highest cusp tip of the mandibular
permanent first molar; L1-MP, tip of the L1 perpendicular to Go-Gn; L6-MP, mesial cusp tip of the L6
perpendicular to Go-Gn; L4-MP, the cusp tip of the L4
perpendicular to Go-Gn; COS line, the line joining the
Bernstein, Preston, and Lampasso 365
American Journal of Orthodontics and Dentofacial Orthopedics
Volume 131, Number 3
Fig 2. COS and lower dental height measurements.
highest cusp tip of the L6 to the tip of the most extruded
mandibular incisor (L1)34; and COS, the depth of the
COS measured as the perpendicular distance from the
tooth cusp of the most infra-erupted premolar to the
COS line.
The premolar used in measuring the deepest part of
the COS had to be in occlusal contact with an opposing
tooth in the maxillary dentition. Because no patients
in this study had their second molars fully erupted at
T1, the COS was measured to the first molars only.
Each COS was measured from the radiographic tracings by using a commercially available 0.5-mm scale
ruler. Because the cephalometric radiographic scans
taken on the Quint Sectograph were adjusted to focus
primarily on the left half of the face, only the depth of
the COS on the left side could be determined accurately. The arch leveling was measured by the changes
in the measurements of the distances of L1, L4, and L6
to the MP (Go-Gn).
The size of the combined method error in locating,
superimposing, and measuring the changes of the various landmarks was calculated. Thirty radiographs (10
subjects) were randomly selected from the original
sample and remeasured by the same operator 2 weeks
later, without reference to the previous measurements.
The casual error was calculated according to Dahlbergs formula35: S2 d2/2n, where S2 is the error
variance and d is the difference between the 2 determinations of the same variable, and the systematic error
was calculated with paired t tests. A significance level
of 1% was used for this part of the study.
The results achieved for the COS measurements
from an earlier study were compared statistically with
paired t tests with those we obtained.21 These 2 sets of
data were recorded independently at different times and
in a random, blind fashion. The same sample group was
used in both studies, and the respective study models
and radiographs were obtained at the same time.
Because on average all patients in the sample were
still undergoing active skeletal growth during and after
the treatment period, the growth of the mandible
probably had some effect on the observed changes in
the linear measurements. Sex-based growth charts of
untreated normal patients in the same age and time
period showed that, in our sample, the COS measurements could have been affected by appositional bone
growth in the mandibular incisor, premolar, and molar
regions. To calculate net mean dental movement, the
appropriate mean growth increments were added to the
affected dimensions.36 The limitations inherent with
using historical data, as was done here, must, however,
be kept in mind.37
RESULTS
The casual errors determined in this study did not
exceed 0.5 mm or 0.5, and no variable had
statistically significant (P .01) systematic errors. Indications of nonnormality of the data at T1 (Dn
0.2336, Lilliefors P .001) and T2 (Dn 0.4182,
Lilliefors P .001) reflect the high number of repeats
in the measurements (eg, 12 twos at T1 and 21 zeros at
T2). Because the sample size was greater than 30, the
results of the t tests can, however, be considered
acceptably accurate.
There were no statistically significant differences
(P .01) between the pairs of COS measurements (radiographic vs study model21) for any of the 31 patients
studied at T1, T2, and T3. The cephalometric data
measured from the sample of radiographs are given in
Tables II and III. Paired t tests were conducted for these
measurements, and the statistical findings are shown in
Table IV.
The mean reduction in the ANB angle as a result of
treatment (T2-T1) was 2.98 (SD, 1.55) (P
.0001); this is equivalent to a 57.75% decrease in the
size of this angle. The overall (T3-T1) mean reduction
of the ANB angle was 3.16 (SD, 2.34).
The mean Y-axis change associated with treatment
was a clockwise rotation of 1.05 (SD, 1.34)
(P .0001). After treatment, this angle became more
acute by a mean of 0.34 (Table II), producing an
overall (T3-T1) mean opening rotation of the Y-axis
angle of 0.71 (SD, 1.73).
Associated with treatment (T2-T1), the SN-OP
angle showed a mean reduction of 2.98 (SD,
3.09), whereas the mean treatment change in the
366 Bernstein, Preston, and Lampasso
Table II.
American Journal of Orthodontics and Dentofacial Orthopedics
March 2007
Changes in cephalometric measurements from T1 to T3
T1
T2
T3
Measurement
Mean
SD
Mean
SD
Mean
SD
L4-COS line (mm)
L1-MP perp (mm)
L4-MP perp (mm)
L6-MP perp (mm)
L1-MP ()
L1 to A-Po (mm)
L1-NB ()
SNA angle ()
SNB angle ()
ANB angle ()
Y-axis ()
SN-MP ()
SN-OP ()
OP-MP ()
SN-PP ()
U6-PP perp (mm)
U6-PP ()
U1-PP perp
U1-PP ()
U1-NA ()
U1-L1 ()
L6-MP ()
2.47
38.89
32.50
29.16
94.85
1.18
22.81
82.03
76.87
5.16
66.21
31.23
17.76
13.47
8.00
20.00
78.89
26.29
109.24
19.18
134.27
84.95
0.69
3.02
2.76
2.14
5.43
1.98
5.16
3.33
3.34
1.60
2.91
4.35
3.31
3.18
2.89
4.15
6.29
2.46
9.31
8.27
13.56
4.10
0.19
39.42
35.31
31.47
95.68
0.34
24.18
79.39
77.21
2.18
67.26
32.21
14.77
17.44
8.95
22.73
81.00
26.87
111.23
22.68
130.53
78.53
0.31
2.94
3.01
2.81
6.93
1.51
4.82
4.08
3.75
1.76
3.36
5.54
2.94
4.58
3.35
2.52
6.24
2.84
5.30
4.25
7.02
5.60
0.69
41.08
36.31
32.70
94.50
0.24
23.15
79.76
77.76
2.00
66.92
31.65
14.58
17.06
8.23
23.97
83.11
28.29
111.97
23.68
131.35
80.40
0.64
3.27
3.18
3.20
5.80
2.04
4.94
4.14
3.91
2.25
3.77
6.30
3.63
4.23
3.04
2.84
6.27
3.10
7.87
5.74
7.98
6.05
Perp, Perpendicular.
OP-MP angle was 3.90 (SD, 3.83). Both changes
were statistically significant (P .0001).
According to the literature, angular changes of less
than 10 in the long axes of the teeth do not have a
significant effect on the perpendicular linear measurements made from L1, L4, or L6 to the MP.38 In this
radiographic study, no patients had angular changes
greater than 10 for any teeth in question (Table III).
The mean COS at T1 for the 31 patients treated with
the continuous archwire technique was 2.47 mm (SD,
0.69 mm; range, 2.00-4.00 mm). The mean COS at T2
for this sample was 0.19 mm (SD, 0.31 mm; range,
0.00-1.00 mm) (P .0001). During treatment, the mean
reduction in the COS was 2.27 mm (SD, 0.77 mm),
which corresponds to a 92.16% average reduction in
this measurement. Twenty-one of the 31 subjects
(about 67.80%) were completely level at T2, but 10 had
slight residual COS at the end of this phase. The mean
COS at T3 was 0.69 mm (SD, 0.64 mm; range,
0.00-2.00 mm). The mean increase in the COS from T2
to T3 was 0.49 mm (SD, 0.69 mm) (P .001). The
overall mean time from T1 to T3 was 14 years 4
months, with a range of 7 years to 28 years 8 months.
Over this period, the overall effect on the COS was an
average reduction of 1.78 mm, which represents a
72.97% reduction.
The perpendicular heights of the mandibular first
molar (L6), the most infra-occluded premolar (L4), and
the most extruded incisor (L1) were measured with
reference to the mandibular plane. Since appositional
bony growth at the inferior border of the mandible can
add significant amounts to these measurements, growth
prediction charts for normal white American youths
were used to calculate net treatment (T2-T1) and
posttreatment (T3-T2) changes.36 No growth data were
found for mandibular premolar heights (L4-MP); therefore, figures midway between those of the molars and
the incisors were used for comparison.36 Growth adjustments were made by adding the relevant mean
growth increments from the growth charts to the
respective measurements made at T2 and T3. Paired
t tests (with set at 0.01) were calculated for both
the growth-adjusted and the unadjusted measurements (Table IV).
Analysis of the data, unadjusted for growth, showed
that there were statistically significant changes associated with treatment for premolar (L4-MP) and first
molar (L6-MP) vertical heights (P .0001). The mean
treatment changes for the dental heights were 0.53 mm
(SD, 1.60 mm) for L1-MP, 2.81 mm (SD, 1.69
mm) for L4-MP, and 2.31 mm (SD, 2.28 mm) for
L6-MP (Table III). All unadjusted posttreatment (T3T2) t test results for the L1, L4, and L6 perpendiculars
Bernstein, Preston, and Lampasso 367
American Journal of Orthodontics and Dentofacial Orthopedics
Volume 131, Number 3
Table III.
Cephalometric measurements from T1 to T3
Treatment changes
(T1-T2)
Posttreatment changes
(T2-T3)
Total change
(T1-T3)
Measurement
Mean
SD
Mean
SD
Mean
SD
L4-COS line (mm)
L1-MP perp (mm)
L4-MP perp (mm)
L6-MP perp (mm)
L1-MP perp: growth (mm)
L4-MP perp: growth (mm)
L6-MP perp: growth (mm)
L1-MP ()
L1 to A-Po (mm)
L1-NB ()
SNA angle ()
SNB angle ()
ANB angle ()
Wits (mm)
Y-axis ()
SN-MP ()
SN-OP ()
OP-MP ()
SN-PP ()
U6-MP perp (mm)
U6-MP ()
U1-PP perp (mm)
U1-PP ()
U1-NA ()
U1-L1 ()
L6-MP ()
2.50
0.53
2.81
2.31
0.87
1.26
0.61
0.82
1.51
1.37
2.65
0.34
2.98
0.52
1.05
0.98
2.98
3.90
0.95
2.73
2.11
0.58
1.98
3.50
3.70
6.42
0.77
1.60
1.69
2.28
0.49
1.66
1.00
1.23
0.66
0.00
0.23
1.18
0.10
1.03
0.37
0.55
0.18
0.06
0.34
0.56
0.19
0.32
0.73
1.24
2.11
1.42
0.74
1.00
0.82
1.87
0.69
2.30
2.00
2.38
1.78
2.19
3.81
3.53
0.21
1.26
0.84
0.35
1.41
0.34
2.27
0.89
3.16
0.59
0.71
0.42
3.18
3.58
0.23
3.97
4.23
2.00
2.73
4.50
2.92
4.55
0.74
2.37
2.15
2.24
6.08
1.57
4.81
2.17
1.29
1.55
1.86
1.34
2.43
3.09
3.83
1.91
2.85
5.32
1.99
9.29
8.09
11.37
3.04
5.21
1.31
4.21
2.23
1.34
2.06
1.45
1.33
2.44
2.56
3.14
1.64
1.59
5.40
1.79
5.22
3.92
6.55
4.63
3.91
1.57
4.35
2.51
1.58
2.34
1.95
1.73
2.75
3.22
3.18
1.78
2.56
5.67
2.20
9.00
7.24
10.28
5.37
Perp, Perpendicular.
Table IV.
Paired t tests for cephalometric measurements
Measurements
COS
L1 perp to MP
L4 perp to MP
L6 perp to MP
L1 perp to MP, growth
L4 perp to MP, growth
L6 perp to MP, growth
L1 to MP
L1 to A-Po line
L1 to NB
SN-MP
Y-axis
OP-MP
SN-OP
SN-PP
ANB angle
T1 vs T2
P
P
P
P
P
P
P
P
P
P
P
P
P
P
P
P
.0001
.0742
.0001
.0001
.0052
.0001
.1482
.4569
.0001
.1227
.0316
.0001
.0001
.0001
.0095
.0001
T2 vs T3
P
P
P
P
P
P
P
P
P
P
P
P
P
P
P
P
.0004
.0004
.0093
.007
.0001
.0627
.0001
.2181
.6829
.1822
.2072
.1651
.5151
.6769
.0198
.6357
Perp, Perpendicular.
to the mandibular plane (Tables III and IV) were
statistically significant (P .01).
After the relevant age- and sex-related mean growth
increments were added to the data, the following results
were recorded. The mean adjusted (T2-T1) changes for
L1-MP and L4-MP (Tables III and IV) were statistically significant (P .0052). The mean treatment
changes allowing for growth were 0.87 mm for
L1-MP, 1.26 mm for L4-MP, and 0.61 mm for L6-MP.
The negative value calculated for the incisor represents
relative intrusive movement over this time period. The
posttreatment (T3-T2) changes for L1-MP and L6-MP
adjusted for growth were statistically significant (P
.0001). The mean net posttreatment dental movements,
taking growth into account, were 0.66 mm for L1-MP,
0.00 mm for L4-MP, and 0.23 mm for L6-MP.
At T2, the mean increase in mandibular incisor
inclination to the mandibular plane was 0.82 (SD,
6.08) (Table III). The mean amount of relapse (T3-T2)
was 1.18 (SD, 5.21). A negative number represents lingual movement (uprighting) of the mandibular
incisors relative to the MP. The overall effect (T3-T1)
on the mandibular incisor inclination to the MP was
0.35 (SD, 3.91).
Associated with orthodontic treatment, the mandibular incisors advanced a mean distance of 1.51 mm
(SD, 1.57 mm) relative to the A-Po line (Table III).
368 Bernstein, Preston, and Lampasso
After treatment, the incisors retroclined a mean distance of 0.10 mm relative to the A-Po line, resulting
in an overall (T3) mean proclination of 1.41 mm
(SD, 1.57 mm). A negative value for the measurement
represents lingual movement of the tip of the tooth.
There was a statistically significant difference between
the T1 and T2 measurements (P .0001) (Table IV).
DISCUSSION
It is generally accepted that, with a few notable
exceptions, leveling a deep COS makes an important
contribution to the success of orthodontic treatment.18-20,34,39-43 In a study that compared sectional
and continuous archwire treatments of adolescent patients with Class II, deep-bite, low-angle malocclusions, it was found that both techniques corrected deep
bites.4,5 Although these studies compared the effectiveness of overbite correction as measured on cephalometric x-rays, they did not measure the COS, or the
effectiveness and long-term stability of leveling the
COS. Our study was prompted by a belief that there
was a need for a long-term, comprehensive, radiographic, and study model analysis of the effectiveness
and stability of leveling the COS.
Before we analyzed the data from the cephalometric
investigation, the radiographic assessment of the COS
performed in this investigation required validation.
Integral to this process were the COS measurements
recorded by Carcara et al21 in their study model
analysis of the COS in the same sample group. The 2
sets of measurements were compared and analyzed to
determine whether the method of recording the COS
from lateral cephalographic x-rays produced the same
results as those recorded from the study models. There
were no statistically significant differences (P .01)
between the radiographic and the study model COS
measurements for any of the 31 patients at T1, T2, and
T3.21 The correlation percentage between the 2 methods was approximately 97%. Only 1 patient who was
measured to be level after treatment in the study model
analysis was not considered level in the cephalometric
analysis. Taking into account all factors that could have
influenced the recordings of the COS by the 2 methods
and the closeness of the results, we believe that the
proposed radiographic assessment of the COS is valid.
The cephalometric radiographs were taken on a Quint
Sectograph that was set to focus on the cranial landmarks on the left side of the face.
From this study, it seems that the continuous
archwire technique is an effective orthodontic approach
for leveling a COS in Class II Division 1 nonextraction
deep-bite patients whose initial COS was 2 to 4 mm.
Sixty-eight percent of the patients studied here were
American Journal of Orthodontics and Dentofacial Orthopedics
March 2007
leveled completely, whereas 32% had slight residual
COS at T2. For the latter patients, the average amount
of COS at T2 was 0.19 mm; this is probably clinically
insignificant. The T2 models all showed Class I molar
and canine relationships with properly finished buccal
occlusions and normal overjets and overbites.21
Results of the paired t test comparing the COS at T2
with that at T3 indicated a statistically significant
change (P .001) in this metrical character. The COS
increased from a mean of 0.19 mm at T2 to a mean of
0.69 mm at T3. Thus, the COS relapsed on average 0.5
0mm over a mean period of 7 years 5 months after the
fixed lingual canine-to-canine mandibular retainers
were removed (an average of 11 years 5 months
postdebond). Although the relapse in the COS might be
statistically significant, it is a relatively small change,
which, in turn, probably represents a normal physiologic process.19-21,27 A previous study, although confirming that the leveling of the COS is a stable
treatment outcome, could not show that the amount of
leveling was correlated with the amount of relapse of
this parameter.44 Unfortunately, those authors did not
specify the treatment technique used to treat their
patients, who had various malocclusion types. In our
study, the COS tended to relapse more in subjects with
the deepest COS at T1. The Pearson correlation coefficient (initial COS vs posttreatment changes) was
0.380 (P .0349); this was statistically significant with
set at 0.05 but not with set at 0.01. At least 1 other
study confirmed our finding that the more the COS is
leveled during treatment, the more it relapses after
treatment.45 That study had a relatively short mean
posttreatment time of 2 years 8 months in their patients,
who were treated with various appliances, and who had
different malocclusion types. Although dental heights
were recorded in the study of mixed malocclusions, no
attempt was made to compensate for the affects of
growth on these dimensions.
The overall long-term (T3-T1) effect of orthodontic
treatment with the continuous arch technique was an
average of 72.97% reduction in the pretreatment COS.
Ten of the 31 patients remained 100% level over a time
span of 5 to 25 years after orthodontic treatment. Only
5 patients had residual COS of over 1 mm, and none
was deeper than 2 mm. This study indicates that relapse
in the COS occurred slowly and over an extended
period of time.
Although there are speculations in the literature
about the contributions of various occlusal elements
involved in leveling the COS, these reports do not
quantify the contributions.3,19,43-47 At the outset of this
study, there was an attempt to use a mandibular
superimposition method,48 patterned after Bjrks
American Journal of Orthodontics and Dentofacial Orthopedics
Volume 131, Number 3
structural method,49 to measure the treatment-induced
changes in dental heights. Whereas this technique was
suitable for measuring changes in the mandibular incisor region (L1-MP), it produced method errors that
were unacceptably large for the other 2 dimensions
studied (L4-MP and L6-MP).
Our results indicate that most of the leveling of the
COS was accomplished by relative extrusion of the
premolars (mean, 2.81 mm) as measured by the L4-MP
perpendicular distance (Table III). It is, however, likely
that some of the mean increase in this dimension could
be attributed to bone apposition at the inferior border of
the mandible. Without control growth data for Class II
subjects, we decided to use the growth charts derived
from normal white American youths. In support of the
use of normal growth data, our selection criteria favored subjects with normal to shorter-than-average
lower anterior facial heights as measured by the MP to
SN angle (32). The appositional growth in the
premolar area was taken to be the average of the
available mean growth increments of the molar and
incisor regions.36 In this study, the mean contribution
of growth to the L4-MP perpendicular distance was
calculated as 1.55 mm.36 If this estimated growth is
taken into account, then the mean net extrusion of the
premolar was 1.26 mm. Likewise, taking appositional
growth (1.7 mm) into account,36 it can be said that
during treatment the mean change in the L6-MP distance was 0.61 mm. Allowing for growth (1.4 mm)36
from T1 to T2, the perpendicular distance L1-MP
decreased by a mean of 0.87 mm. The premolar and
incisor changes were statistically significant (P .01)
before and after the possible effects of growth were
taken into account. These findings agree with previous
studies suggesting that straight-wire techniques level
the COS by a combination of premolar extrusion and
incisor intrusion.4,5,19,46 Those studies did not, however, provide data to quantify the suggested tooth
movements.
The relapse of the COS (T3-T2), although small,
was nonetheless statistically significant (P .01). The
mean observed relapse in the COS could be attributed
to changes in the relative vertical heights of 2 of the
dental elements that were used to define the curve.
Taking posttreatment growth changes into consideration, the mandibular incisor (L1-MP) erupted a mean
distance of 0.66 mm, whereas the molar erupted a mean
distance of 0.23 mm after treatment. The premolar,
however, had no additional mean vertical dental height
change after treatment and thus had no relapse. These
results confirm previous findings of a slight return of
the COS after treatment.19-21,27
Several authors noted the effects of continuous
Bernstein, Preston, and Lampasso 369
archwire mechanics.3-9 These effects include flaring of
the mandibular incisors, extrusion of the mandibular
molars, and clockwise opening rotation of the OP.
Some features of the continuous arch technique, including the 5 of torque in the mandibular incisors and the
6 of distal tip in the mandibular molars, are somewhat unique to this technique. These features, along
with heat-treated stainless steel archwires with reverse
COS in the mandibular arch and omega stops tied back
to the molar tubes, might play a role in preventing the
side effects reported with other straight-wire techniques.3-9
All subjects in this study had mild to moderate
mandibular incisor crowding that, with a straight
wire and a nonextraction approach to treatment,
would have been aggravated by the leveling of the
COS.39 Despite the incisor crowding in our sample of
patients, the effects of the orthodontic treatment on the
position of their mandibular incisors were minimal. The
angles (L1-NB, L1-MP) were not statistically significantly changed as a result of treatment (P .01). The
mean treatment change of the significantly (P .01)
altered variable (L1 to A-Po) was 1.51 1.57 mm.
Because the T1 average position for the L1 to A-Po was
1.18 mm, a mean proclination of 1.51 mm placed the
tip of the L1 ahead of the A-Po line by a mean of 0.33
mm. It is thus fair to say that, in this sample, orthodontic treatment did not result in excessive flaring of the
mandibular incisors.
Since there was very little alteration in the measures
of the mean positions of the mandibular incisors during
treatment, it was expected that little posttreatment
change would occur. This was indeed the case; the
posttreatment changes in the 3 measurements of mandibular incisor position studied here were small and not
statistically significant (P .01). The L1 to A-Po
distance relapsed an average of 0.10 mm to leave the
tip of L1 just 0.23 mm ahead of the A-Po line. Both
the T2 and the T3 recordings for the L1 to A-Po
distance were close to the stated ideal position of this
parameter.46 In this group of patients, it can be concluded that the treatment-induced average advancement
of the mandibular incisor was clinically acceptable and
stable in the long term.
From the data, it appears that the mean treatment
change (T2-T1) for the mandibular molar inclination to
the mandibular plane was 6.42 (SD, 3.04). This
finding indicates that the full 6 of tip back built into
the molar attachments was expressed in most patients.
The additional 0.42 might have been due to the use of
reverse curved archwires that would tend to cause the
posterior teeth to tip back even farther than the tip
incorporated in the prescription of the appliance. This
370 Bernstein, Preston, and Lampasso
second-order movement relapsed an average of 1.87
(SD, 4.63), resulting in a mean long-term uprighting
of 4.55.
A straight-wire approach to Class II orthodontic
treatment requiring leveling of the COS has been
associated with increases in the vertical dimensions of
the face.3,5-7 An analysis of the data from this study
shows that in our patients the treatment did not have a
major effect on 2 measurements of lower facial height.
Although the Y-axis changed statistically significantly
from T1 to T2 (P .001), the mean change was only
1.05. During treatment, the MP angle (SN-MP)
changed by less than a mean of 1.0 (SD, 2.43),
which was not statistically significant (P .0316).
There were changes in the mean angular relationships of the OP during treatment. During treatment,
there were a mean reduction of 2.98 in the SN-OP
angle and a mean increase of 3.90 in the OP-MP angle.
These changes occurred during the leveling of the COS,
and they represent counterclockwise rotation in the OP.
The posttreatment changes in these 2 angles were not
statistically significant (P .01).
We studied only patients with Class II Division 1
malocclusions with specifically defined parameters.
Our results cannot be arbitrarily extrapolated to the
success that can be achieved with other categories of
malocclusions such as those characterized by vertical
growth patterns.
CONCLUSIONS
1. It is feasible to determine the depth of the COS
from cephalometric radiographs taken with the
Quint Sectograph cephalometer.
2. The continuous archwire technique effectively leveled the COS in this sample of Class II Division 1
deep-bite patients treated without extractions.
3. In this study, the leveling of the COS with the
continuous archwire technique occurred by a combination of mainly premolar extrusion and, to a
lesser extent, incisor intrusion.
4. In the subjects studied here, the continuous archwire technique effectively controlled the mandibular incisor position during the leveling process.
These results appear to be stable in the long term.
6. The 6 of tip back in the molar band tipped the
mandibular first molar back at least that amount
during treatment.
7. In this study, the continuous archwire technique did
not cause excessive opening rotation of the Y-axis
or the MP angle.
American Journal of Orthodontics and Dentofacial Orthopedics
March 2007
REFERENCES
1. Tweed CH. Clinical orthodontics. St Louis: C. V. Mosby; 1966.
p. 2-82.
2. Ricketts RM. Bioprogressive therapy as an answer to orthodontic
needs. Part I. Am J Orthod 1969;70:241-68.
3. Otto RL, Anholm JM, Engel GA. A comparative analysis of
intrusion of incisor teeth achieved in adults and children according to facial types. Am J Orthod 1980;77:437-46.
4. Dake ML, Sinclair PM. A comparison of the Ricketts and
Tweed-type arch leveling techniques. Am J Orthod Dentofacial
Orthop 1989;95:72-8.
5. Weiland FJ, Bartleon HP, Droschl H. Evaluation of continuous arch and segmented arch leveling techniques in adult
patients: a clinical study. Am J Orthod Dentofacial Orthop
1996;110:647-52.
6. Wylie WL. Overbite and vertical facial dimensions in terms of
muscle balance. Angle Orthod 1944;14:13-7.
7. Bench RW, Gugino CF, Hilgers JJ. Bioprogressive therapy. Part 2.
J Clin Orthod 1977;11:661-82.
8. Berman MS. Straight wire mythsBritish Journal of Orthodontics interview. Br J Orthod 1988;151:57-61.
9. Woods M. A reassessment of space requirements for lower arch
leveling. J Clin Orthod 1986;20:770-8.
10. Merritt J. A cephalometric study of the treatment and retention of
deep overbite cases (thesis). Baylor: University of Texas; 1964.
11. Schudy FF. The association of anatomical entities as applied to
clinical orthodontics. Angle Orthod 1966;36:190-203.
12. Graber TM. Orthodontics: principles and practice. 3rd ed. Philadelphia: W. B. Saunders; 1972. p. 572-608.
13. Ferguson JW. Lower incisor torque: the effects of rectangular
archwires with a reverse curve of Spee. Br J Orthod 1990;17:
311-5.
14. Schudy FF. Cant of the occlusal plane and axial inclination of
teeth. Angle Orthod 1963;23:69-82.
15. Schudy FF. Vertical growth versus antero-posterior growth as
related to function. Angle Orthod 1964;34:756-93.
16. Lett RL. Overbite correction and relapse as analyzed by some
cephalometric and treatment related variables (thesis). Minneapolis: University of Minnesota; 1969.
17. Ellen EK, Schneider BJ, Selke T. A comparative study of
anchorage in bioprogressive vs. standard edgewise treatment in
Class II correction with intermaxillary elastic force. Am J Orthod
Dentofacial Orthop 1998;114:430-6.
18. Andrews LF. The six keys to normal occlusion. Am J Orthod
1972;62:296-309.
19. Koyama T. A comparative analysis of the curve of Spee (lateral
aspect) before and after orthodontic treatmentwith particular
reference to overbite patients. J Nihon Univ Sch Dent 1979;21:
25-34.
20. Okeson JP. Management of temporomandibular disorders and
occlusion. 5th ed. St Louis: Mosby; 2003. p. 93-146.
21. Carcara S, Preston CB, Jureyda O. The relationship between the
curve of Spee, relapse, and the Alexander discipline. Semin
Orthod 2001;7:90-9.
22. Fidler BC, rtun J, Joondeph DR, Little RM. Long-term stability
of Angle Class II Division 1 malocclusions with successful
occlusal results at the end of active treatment. Am J Orthod
Dentofacial Orthop 1995;107:276-85.
23. Williams R. Eliminating lower retention. J Clin Orthod 1985;22:
342-9.
24. Little RM. The irregularity index: a quantitative score of mandibular anterior teeth. Am J Orthod 1975;68:554-63.
Bernstein, Preston, and Lampasso 371
American Journal of Orthodontics and Dentofacial Orthopedics
Volume 131, Number 3
25. Bishara SE, Jakobsen JR, Treder JE, Stasi M. Changes in the
maxillary and mandibular tooth size-arch length relationship
from early adolescence to early adulthood. Am J Orthod Dentofacial Orthop 1989;95:46-59.
26. Burstone CJ. The mechanics of the segmental arch technique.
Angle Orthod 1966;36:99-120.
27. Elms TN, Buschang PH, Alexander RG. Long-term stability of
Class II Division 1 nonextraction cervical face-bow therapy: I.
model analysis. Am J Orthod Dentofacial Orthop 1996;109:
271-6.
28. Glenn G, Sinclair PM, Alexander RG. Nonextraction orthodontic
therapy: postreatment dental and skeletal stability. Am J Orthod
Dentofacial Orthop 1987;92:321-8.
29. Little RM, Reidel RA, rtun J. An evaluation of changes in
mandibular anterior alignment from 10 to 20 years postretention.
Am J Orthod Dentofacial Orthop 1988;93:423-8.
30. Sinclair PM, Little RM. Maturation of untreated normal occlusions. Am J Orthod 1983;84:114-23.
31. Alexander RG. The Alexander discipline, contemporary concepts and philosophies. Glendora, Calif: Ormco; 1986.
32. Rakosi T. An atlas and manual of cephalometric radiography.
Worcester, United Kingdom: Ebenezer Baylis & Son; 1982.
p. 35.
33. Bimler HP. Bimler cephalometric analysis. J Clin Orthod 1985;
56:501-23.
34. Germane N, Staggers JA, Rubenstein L, Revere JT. Arch length
consideration due to the curve of Spee: a mathematical model.
Am J Orthod Dentofacial Orthop 1992;102:251-5.
35. Dahlberg G. Statistical methods for medical and biological
students. London: George Allen and Unwin; 1940. p. 122-32.
36. Riolo ML, Moyers RE, McNamara JA Jr, Hunter WS. An atlas
of craniofacial growth. Craniofacial Growth Series. Ann Arbor:
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
Center for Human Growth and Development; University of
Michigan; 1974. p. 126-8.
Proffit WR, Fields HW. Contemporary orthodontics. St Louis:
Mosby; 2000. p. 242.
Gordon JB. Lower incisor intrusion in low angle, deep bite cases
(thesis). Los Angeles: University of California at Los Angeles;
1977.
Baldridge DW. Leveling the curve of Spee: its effect on
mandibular archlength. J Pract Orthod 1969;64:26-41.
Dawson P. Evaluation, diagnosis and treatment of occlusal
problems. St Louis: C. V. Mosby; 1974. p. 190-205.
Hellsing E. Increased overbite and craniomandibular disordersa clinical approach. Am J Orthod Dentofacial Orthop
1990;98:516-22.
Wheeler RC. A textbook of dental anatomy and physiology. 2nd
ed. Philadelphia: W. B. Saunders; 1950. p. 352-405.
Braun S, Hnat WP, Johnson BE. The curve of Spee revisited.
Am J Orthod Dentofacial Orthop 1996;110:206-10.
De Praeter J, Dermaut L, Martens G, Kuijpers-Jagtman A.
Long-term stability of the leveling of the curve of Spee. Am J
Orthod Dentofacial Orthop 2002;121:266-72.
Shannon KR, Nanda RS. Changes in the curve of Spee with
treatment and at 2 years postreatment. Am J Orthod Dentofacial
Orthop 2004;125:589-96.
Engel G, Comforth G, Damerall JM, Gordon J, Levy P, McAlpine J, et al. Treatment of deep-bite cases. Am J Orthod 1980;77:
1-13.
Williams R. The diagnostic line. Am J Orthod 1969;55:458-76.
Al-Buraiki H, Sadowsky C, Schneider B. The effectiveness and
long-term stability of overbite correction with incisor intrusion
mechanics. Am J Orthod Dentofacial Orthop 2005;127:47-55.
Bjrk A. Prediction of mandibular growth rotation. Am J Orthod
1969;55:585-99.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Color Atlas of Porcelain Laminate VeneersDocumento244 pagineColor Atlas of Porcelain Laminate Veneersnorma paulina carcausto lipaNessuna valutazione finora
- AL MOHAJER KKK4545 DocumentDocumento163 pagineAL MOHAJER KKK4545 DocumentleeminhoangrybirdNessuna valutazione finora
- BOPT Technique (2013)Documento14 pagineBOPT Technique (2013)Joselyn RodríguezNessuna valutazione finora
- History of CeuDocumento6 pagineHistory of CeuFRANCHES CAMIL ROSALES100% (1)
- Buku Menu Bening'sDocumento57 pagineBuku Menu Bening'sAlfina AmaliaNessuna valutazione finora
- Instructions for Use: Gnatus Syncrus H Dental Delivery UnitDocumento36 pagineInstructions for Use: Gnatus Syncrus H Dental Delivery UnitFill100% (1)
- Davis 2014Documento11 pagineDavis 2014Monica JohanaNessuna valutazione finora
- Periodontal Surgery Involving Modified Widman FlapDocumento11 paginePeriodontal Surgery Involving Modified Widman FlapChandra BudiNessuna valutazione finora
- Periodontology 2000 - 2022 - BarootchiDocumento28 paginePeriodontology 2000 - 2022 - BarootchitzulinNessuna valutazione finora
- Bauman-Wengler Speech Motor Assessment FormDocumento5 pagineBauman-Wengler Speech Motor Assessment FormLorenz ReyesNessuna valutazione finora
- Transient MalocclusionsDocumento30 pagineTransient Malocclusionsdrsasi100% (1)
- Modal Verbs Must or MustntDocumento3 pagineModal Verbs Must or MustntCamila VasquezNessuna valutazione finora
- How To Write An Expert Opinion LetterDocumento3 pagineHow To Write An Expert Opinion LetterAna-Maria DucuNessuna valutazione finora
- Interappointment Flare-Up in Endodontics: A Case Report and An OverviewDocumento4 pagineInterappointment Flare-Up in Endodontics: A Case Report and An OverviewAnonymous cTV8BbsCeNessuna valutazione finora
- Recent Trends in Tricalcium Silicates For Vital Pulp TherapyDocumento8 pagineRecent Trends in Tricalcium Silicates For Vital Pulp TherapypoojaNessuna valutazione finora
- ETK IMPLANT - Company - ENDocumento16 pagineETK IMPLANT - Company - ENPhạm CườngNessuna valutazione finora
- Dental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective StudyDocumento7 pagineDental Caries - Its Sequelae and Treatment Among Patients in A Tertiary Hospital in North-Western Nigeria-A Retrospective Studyabdurrazaq taiwoNessuna valutazione finora
- Methods of Data Collection in QualitativeDocumento5 pagineMethods of Data Collection in QualitativeYina Perez SanchezNessuna valutazione finora
- 39.full Violin and Its Effects ArticleDocumento8 pagine39.full Violin and Its Effects ArticleROMCNessuna valutazione finora
- 3D Printing Applications in DentistryDocumento4 pagine3D Printing Applications in Dentistryyoursie accountNessuna valutazione finora
- AJODO-2013 Brunetto 143 5 633Documento12 pagineAJODO-2013 Brunetto 143 5 633player osamaNessuna valutazione finora
- How To Collect A Saliva Sample For A Cortisol TestDocumento1 paginaHow To Collect A Saliva Sample For A Cortisol TestJheo TorresNessuna valutazione finora
- Principle of PanormicDocumento64 paginePrinciple of PanormicRishabh Madhu Sharan100% (1)
- MDNSDocumento7 pagineMDNSRamon HipolitoNessuna valutazione finora
- Overseas Registration Exam: Application Form Guidance NotesDocumento8 pagineOverseas Registration Exam: Application Form Guidance NotesSohaib DurraniNessuna valutazione finora
- Question BankDocumento104 pagineQuestion BankKrishna GuptaNessuna valutazione finora
- Distalization With The Miniscrew-Supported EZ Slider AuxiliaryDocumento37 pagineDistalization With The Miniscrew-Supported EZ Slider AuxiliaryAnushriya DuttaNessuna valutazione finora
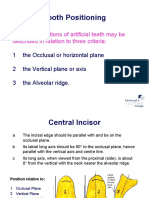
- Tooth Positioning: The Basic Positions of Artificial Teeth May Be Described in Relation To Three CriteriaDocumento19 pagineTooth Positioning: The Basic Positions of Artificial Teeth May Be Described in Relation To Three CriteriaCherine SnookNessuna valutazione finora
- Biomechanics in Orthodontics - A Review (Part 1) IJODODocumento11 pagineBiomechanics in Orthodontics - A Review (Part 1) IJODOPranshu MathurNessuna valutazione finora
- Carey's AnalysisDocumento26 pagineCarey's AnalysisRavi Gowda100% (1)