Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Sepsis and Septic Shock
Caricato da
بو عقيل الشيخ حسينDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Sepsis and Septic Shock
Caricato da
بو عقيل الشيخ حسينCopyright:
Formati disponibili
Sepsis and septic shock
Background:
Over many years, the terms sepsis and septicemia have referred to
several ill-defined clinical conditions present in a patient with
bacteremia. Definitions have not changed greatly since 1914, when
Schottmueller wrote, Septicemia is a state of microbial invasion from
a portal of entry into the blood stream which causes sign of illness.
In practice, these 2 terms have often been used interchangeably;
however, only about half of patients with signs and symptoms of sepsis
have positive results on blood culture. Furthermore, not all patients
with bacteremia have signs of sepsis. It follows, therefore, that sepsis
and septicemia are not in fact identical.
In the past few decades, the discovery of endogenous mediators of the
host response has led to the recognition that the clinical syndrome of
sepsis is the result of excessive activation of host defense mechanisms
rather than the direct effect of microorganisms. Sepsis and its sequelae
represent a continuum of clinical and pathophysiologic severity.
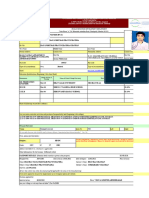
Serious bacterial infections at any site in the body (see the image
below), with or without bacteremia, are usually associated with
important changes in the function of every organ system in the body.
These changes are mediated mostly by elements of the host immune
system against infection. Shock is deemed present when volume
replacement fails to increase blood pressure to acceptable levels and
when associated clinical evidence indicates inadequate perfusion of
major organ systems, with progressive failure of organ system
functions. Although hyperlactecemia is commonly seen in severe
sepsis, its relationship to hypoperfusion is questionable and is more
often due to the acute inflammatory state, impaired lactate clearance,
and nonoxidative phosphorylation lactate production.
Multiple organ dysfunctions, the extreme end of the continuum, are
incremental degrees of physiologic derangements in individual organs
(ie, processes rather than events). Alteration in organ function can vary
widely, ranging from a mild degree of organ dysfunction to frank organ
failure. (See Multiple Organ Failure of Sepsis, Systemic Inflammatory
Response Syndrome (SIRS), Toxic Shock Syndrome, and Septic
Thrombophlebitis .)
This article does not cover sepsis of the neonate or infant. Special
consideration must be given to neonates, infants, and small children
with regard to fluid resuscitation, appropriate antibiotic coverage,
intravenous (IV) access, and vasopressor therapy. (See Neonatal
Sepsis, Pediatric Sepsis, Treatment of Sepsis and Septic Shock in
Children, Shock in Pediatrics, and Shock and Hypotension in the
Newborn.)
Shock Classification, Terminology, and Staging
Shock is identified in most patients by hypotension and inadequate
organ perfusion, which may be caused by either low cardiac output or
low systemic vascular resistance. Circulatory shock can be subdivided
into 4 distinct classes on the basis of underlying mechanism and
characteristic hemodynamics, as follows:
Hypovolemic shock
Obstructive shock
Distributive shock
Cardiogenic shock
These classes of shock should be considered and systematically
differentiated before a definitive diagnosis of septic shock is
established.
Hypovolemic shock results from the loss of blood volume caused by
such conditions as gastrointestinal (GI) bleeding, extravasation of
plasma, major surgery, trauma, and severe burns. Patients suffering
from hypovolemic shock demonstrate tachycardia, cool clammy
extremities, hypotension, dry skin and mucous membranes, and poor
turgor.
Obstructive shock results from an intrinsic or extrinsic obstruction of
circulation. Pulmonary embolism and pericardial tamponade both result
in obstructive shock.
Distributive shock is caused by excessive vasodilation and impaired
distribution of blood flow (eg, direct arteriovenous shunting), and it is
characterized by decreased resistance or increased venous capacity
from the vasomotor dysfunction. Patients with this type of shock have
high cardiac output, hypotension, a large pulse pressure, a low
diastolic pressure, and warm extremities with good capillary refill.
These findings on physical examination strongly suggest a working
diagnosis of septic shock.
Cardiogenic shock is characterized by primary myocardial dysfunction,
which renders the heart unable to maintain adequate cardiac output.
Affected patients demonstrate clinical signs of low cardiac output while
showing evidence of adequate intravascular volume. The patients have
cool clammy extremities, poor capillary refill, tachycardia, a narrow
pulse pressure, and low urine output.
Definitions of key terms
The basis of sepsis is the presence of infection associated with a
systemic inflammatory response that results in physiologic alterations
at the capillary endothelial level. The difficulty in diagnosis comes in
knowing when a localized infection has become systemic and requires
more aggressive hemodynamic support. No criterion standard exists
for the diagnosis of endothelial dysfunction, and patients with sepsis
may not initially present with frank hypotension and overt shock.
Clinicians often use the terms sepsis, severe sepsis, and septic shock
without following commonly understood definitions. In 1991, the
American College of Chest Physicians (ACCP) and the Society of Critical
Care Medicine (SCCM) convened a consensus conference to establish
definitions of these and related terms.
Systemic inflammatory response syndrome
The term systemic inflammatory response syndrome (SIRS) was
developed in an attempt to describe the clinical manifestations that
result from the systemic response to infection (fever or hypothermia,
tachycardia, tachypnea, and hyperleukocytosis or leukopenia). Criteria
for SIRS are considered to be met if at least 2 of the following 4 clinical
findings are present:
Temperature higher than 38C (100.4F) or lower than 36C
(96.8F)
Heart rate (HR) higher than 90 beats/min
Respiratory rate (RR) higher than 20 breaths/min or arterial
carbon dioxide tension (PaCO 2) lower than 32 mm Hg
White blood cell (WBC) count higher than 12,000/L or lower
than 4000/L or with 10% immature (band) forms
Note that a patient can have a severe infection without meeting SIRS
criteria; conversely, SIRS criteria may be present in the setting of many
other illnesses not caused by an infectious pro cess.
Potrebbero piacerti anche
- Hypovolemic Shock TEXTDocumento5 pagineHypovolemic Shock TEXTrhen1991Nessuna valutazione finora
- Stress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.Documento94 pagineStress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.sorbariNessuna valutazione finora
- Psychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Documento21 paginePsychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Eduardo Aguirre DávilaNessuna valutazione finora
- Dermatology NotesDocumento59 pagineDermatology NotesAbdullah Matar Badran50% (2)
- Power of VOLITION: All Actions Have Consequences A. AristotleDocumento6 paginePower of VOLITION: All Actions Have Consequences A. AristotleLiah ManlapigNessuna valutazione finora
- Sepsis: DR Aung Paing PhyoDocumento60 pagineSepsis: DR Aung Paing PhyoAg Paing PhyoNessuna valutazione finora
- Lewis: Medical-Surgical Nursing, 10 Edition: Shock, Sepsis, and Multiple Organ Dysfunction Syndrome Key Points ShockDocumento5 pagineLewis: Medical-Surgical Nursing, 10 Edition: Shock, Sepsis, and Multiple Organ Dysfunction Syndrome Key Points Shockann forsyNessuna valutazione finora
- ShockDocumento11 pagineShockNatalia WiryantoNessuna valutazione finora
- DengueDocumento99 pagineDengueJames DavidNessuna valutazione finora
- Early Identification and Treatment of SepsisDocumento4 pagineEarly Identification and Treatment of Sepsislisa yuliantiNessuna valutazione finora
- ABCDs During A Code Blue Response in An Adult PatientDocumento23 pagineABCDs During A Code Blue Response in An Adult PatientChakra PuspitaNessuna valutazione finora
- SepsisDocumento3 pagineSepsissivaNessuna valutazione finora
- Lesson Plan Renal CalculiDocumento17 pagineLesson Plan Renal CalculiAmrita Dean71% (7)
- Systemic Inflammatory Respon Syndrom: SyaharaDocumento41 pagineSystemic Inflammatory Respon Syndrom: Syaharaprima suci angrainiNessuna valutazione finora
- Unknown Bacteria Lab ReportDocumento13 pagineUnknown Bacteria Lab Reportapi-529628802Nessuna valutazione finora
- SepsisDocumento36 pagineSepsisWan FaizuddinNessuna valutazione finora
- Management of Severe Sepsis: Learning ObjectivesDocumento5 pagineManagement of Severe Sepsis: Learning ObjectivesVictoriano Valiente100% (1)
- Hypovolemic Shock 09Documento58 pagineHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Hypovolemic ShockDocumento10 pagineHypovolemic ShockUsran Ali BubinNessuna valutazione finora
- Plante-2016-Management of Sepsis and Septic Shock For The Obstetrician-Gynecologist PDFDocumento20 paginePlante-2016-Management of Sepsis and Septic Shock For The Obstetrician-Gynecologist PDFntnquynhproNessuna valutazione finora
- Sepsis and Septic ShockDocumento4 pagineSepsis and Septic ShockFebyan AbotNessuna valutazione finora
- Septic ShockDocumento16 pagineSeptic ShockGelo JvrNessuna valutazione finora
- Sepsis and Septic Shock - Critical Care MedicineDocumento2 pagineSepsis and Septic Shock - Critical Care MedicineMihaela MoraruNessuna valutazione finora
- Sepsis and The Systemic Inflammatory Response SyndromeDocumento22 pagineSepsis and The Systemic Inflammatory Response SyndromeLaburengkengNessuna valutazione finora
- Shock Septico EvidenciaDocumento8 pagineShock Septico EvidenciaFra1312Nessuna valutazione finora
- Sepsis in Adults and Foals: Marie-France Roy, DMVDocumento21 pagineSepsis in Adults and Foals: Marie-France Roy, DMVLuis Fernando Vargas JaraNessuna valutazione finora
- Septic Shock Rapid Recognition and Initial Resuscitation inDocumento19 pagineSeptic Shock Rapid Recognition and Initial Resuscitation inCristian Villarroel SNessuna valutazione finora
- Overview SepsisDocumento13 pagineOverview SepsisYanna RizkiaNessuna valutazione finora
- Sepsisandsepticshock: Patrick J. MaloneyDocumento18 pagineSepsisandsepticshock: Patrick J. MaloneyyoghaNessuna valutazione finora
- Distributive ShockDocumento26 pagineDistributive ShockYorim Sora PasilaNessuna valutazione finora
- Sirs 2Documento3 pagineSirs 2Silmi ThaherNessuna valutazione finora
- Berkas Panum PonorogoDocumento10 pagineBerkas Panum PonorogoDimas Novian SNessuna valutazione finora
- 1 Shock CdmaDocumento59 pagine1 Shock CdmaRoby KieranNessuna valutazione finora
- Background: EmbryologyDocumento25 pagineBackground: EmbryologydonisaputraNessuna valutazione finora
- SEPSIS - 2016 - 18 (Dr. Erwin)Documento68 pagineSEPSIS - 2016 - 18 (Dr. Erwin)Falayna Ithu DheisyaNessuna valutazione finora
- 11 - Shock - Current Diagnosis and Treatment Emergency MedicineDocumento18 pagine11 - Shock - Current Diagnosis and Treatment Emergency MedicineRon KNessuna valutazione finora
- Sepsis 1Documento14 pagineSepsis 1Andres Aqueveque BullNessuna valutazione finora
- ASSIGNMENT ON SHOCK (SEPTIC SHOCK) (AutoRecovered) (AutoRecovered)Documento17 pagineASSIGNMENT ON SHOCK (SEPTIC SHOCK) (AutoRecovered) (AutoRecovered)SabariNessuna valutazione finora
- Sepsis (from Gr. Σ: Systemic inflammatory response syndromeDocumento5 pagineSepsis (from Gr. Σ: Systemic inflammatory response syndromeReyes PaulNessuna valutazione finora
- Martin 2016Documento12 pagineMartin 2016rositha prabandariNessuna valutazione finora
- The Systemic Inflammatory Response Syndrome: Hanif Meeran and Mark MessentDocumento12 pagineThe Systemic Inflammatory Response Syndrome: Hanif Meeran and Mark MessentHatara Tim Justin TakeroiNessuna valutazione finora
- Chapter 176Documento13 pagineChapter 176Intan Sanditiya AlifNessuna valutazione finora
- City of Manila (Formerly City College of Manila) Mehan Gardens, ManilaDocumento8 pagineCity of Manila (Formerly City College of Manila) Mehan Gardens, Manilaicecreamcone_201Nessuna valutazione finora
- Lewis: Medical-Surgical Nursing, 10 Edition: Shock, Sepsis, and Multiple Organ Dysfunction Syndrome Key Points ShockDocumento5 pagineLewis: Medical-Surgical Nursing, 10 Edition: Shock, Sepsis, and Multiple Organ Dysfunction Syndrome Key Points ShockIndra TimsinaNessuna valutazione finora
- Severe Sepsis and Septic Shock in EDDocumento31 pagineSevere Sepsis and Septic Shock in EDtarrynwortmann5319Nessuna valutazione finora
- Bacteremia - Dan - Sepsis and ShockDocumento232 pagineBacteremia - Dan - Sepsis and ShockKiki Luhita SariNessuna valutazione finora
- Shock and Blood TransfusionDocumento41 pagineShock and Blood TransfusionpalNessuna valutazione finora
- Septic Shock: by Nsubuga Ivan BMS/12264/182/DU 4.2Documento55 pagineSeptic Shock: by Nsubuga Ivan BMS/12264/182/DU 4.2Nsubuga IvanNessuna valutazione finora
- Uro SepsisDocumento23 pagineUro SepsisJihad Anad100% (1)
- Septic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) - UpToDateDocumento38 pagineSeptic Shock in Children - Rapid Recognition and Initial Resuscitation (First Hour) - UpToDatepradeepgullipalli.1089Nessuna valutazione finora
- Urosepsis PDFDocumento14 pagineUrosepsis PDFYudi SiswantoNessuna valutazione finora
- Trauma Lethal TriadDocumento10 pagineTrauma Lethal TriadChristian Kuon-YengNessuna valutazione finora
- Sepsis RingkasDocumento19 pagineSepsis Ringkasblok etikakedokteranNessuna valutazione finora
- Shock 20231122 213304 0000Documento32 pagineShock 20231122 213304 0000Mikella E. PAGNAMITANNessuna valutazione finora
- Sepsis ShockDocumento11 pagineSepsis ShockDr. LNessuna valutazione finora
- Sepsis in Older PatientsDocumento8 pagineSepsis in Older PatientsFajar WasilahNessuna valutazione finora
- Risk and Setting For Multiple Organ Failure in Medical PatientsDocumento2 pagineRisk and Setting For Multiple Organ Failure in Medical PatientsabdullahNessuna valutazione finora
- Hemorrhagic Shock - StatPearls - NCBI BookshelfDocumento8 pagineHemorrhagic Shock - StatPearls - NCBI BookshelfRizqan Fahlevvi AkbarNessuna valutazione finora
- UpToDate Neonatal Shock 2018Documento20 pagineUpToDate Neonatal Shock 2018Ladislao QuezadaNessuna valutazione finora
- Multiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundDocumento6 pagineMultiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundrahayuNessuna valutazione finora
- Low Systemic Vascular ResistanceDocumento7 pagineLow Systemic Vascular ResistanceMuhammad BadrushshalihNessuna valutazione finora
- Acute Pulmonary Edema - NEJMDocumento4 pagineAcute Pulmonary Edema - NEJMSuzika Dewi0% (1)
- Referat SepsisDocumento18 pagineReferat SepsisImelva GirsangNessuna valutazione finora
- 03 Clinical Manifestation PathophysiologyDocumento16 pagine03 Clinical Manifestation Pathophysiologymochamd azam maqbullaNessuna valutazione finora
- Essentials of Sepsis Management: John M. GreenDocumento11 pagineEssentials of Sepsis Management: John M. GreencastillojessNessuna valutazione finora
- AN 623 - Adult Nursing Skills Underpinning Complex Care CW1Documento15 pagineAN 623 - Adult Nursing Skills Underpinning Complex Care CW1Gareth McKnight100% (2)
- Disorders of The PulpDocumento7 pagineDisorders of The Pulpابو الجودNessuna valutazione finora
- PhysiologyDocumento31 paginePhysiologyraza20100% (1)
- Multiple Pulp Polyps Associated With Deciduous TeethDocumento4 pagineMultiple Pulp Polyps Associated With Deciduous TeethJea Ayu YogatamaNessuna valutazione finora
- Zybio Company Profile 20211109CDocumento46 pagineZybio Company Profile 20211109CĐức Hòa100% (1)
- Intra-Arterial Catheterization For Invasive Monitoring: Indications, Insertion Techniques, and Interpretation - UpToDateDocumento40 pagineIntra-Arterial Catheterization For Invasive Monitoring: Indications, Insertion Techniques, and Interpretation - UpToDatejuanpbagurNessuna valutazione finora
- Hallie Berger Resume 11-2Documento2 pagineHallie Berger Resume 11-2api-281008760Nessuna valutazione finora
- Design Theory: Boo Virk Simon Andrews Boo - Virk@babraham - Ac.uk Simon - Andrews@babraham - Ac.ukDocumento33 pagineDesign Theory: Boo Virk Simon Andrews Boo - Virk@babraham - Ac.uk Simon - Andrews@babraham - Ac.ukuzma munirNessuna valutazione finora
- Hipertensi Portal Donny SandraDocumento67 pagineHipertensi Portal Donny SandrabobyNessuna valutazione finora
- Meiosis GizmosDocumento9 pagineMeiosis GizmosShaylee TorresNessuna valutazione finora
- Multi-Disease Prediction With Machine LearningDocumento7 pagineMulti-Disease Prediction With Machine LearningUmar KhanNessuna valutazione finora
- Mekong TMBO 02 Maret 2021Documento14 pagineMekong TMBO 02 Maret 2021Yolanda RahayuNessuna valutazione finora
- Gen EdDocumento14 pagineGen EdMark Julius G AlmadinNessuna valutazione finora
- Dermoscopy ReviewDocumento28 pagineDermoscopy ReviewMarwa RagabNessuna valutazione finora
- UnificationDocumento24 pagineUnificationFlyingWalrusNessuna valutazione finora
- Fever of Unknown OriginDocumento26 pagineFever of Unknown OriginFiona Yona Sitali100% (1)
- Wadsworth Publishing Critical Reasoning 6thDocumento468 pagineWadsworth Publishing Critical Reasoning 6thprabindra100% (1)
- Diagnostic TestDocumento4 pagineDiagnostic TestrizabesmonteNessuna valutazione finora
- Maui Medical Dispensary Application Redacted Sec3Documento541 pagineMaui Medical Dispensary Application Redacted Sec3melipasaNessuna valutazione finora
- Psychoactive Drugs ChartDocumento5 paginePsychoactive Drugs ChartAlessandra WilliamsNessuna valutazione finora
- HR 2 FormDocumento8 pagineHR 2 Formrkpatel40Nessuna valutazione finora
- Seatone InfoDocumento7 pagineSeatone InfoJugal ShahNessuna valutazione finora
- ST Peter, 2014, BI-Annual DR-TB Performance Report To AAHB, 15 March 2022. JohnDocumento43 pagineST Peter, 2014, BI-Annual DR-TB Performance Report To AAHB, 15 March 2022. Johnሀይደር ዶ.ርNessuna valutazione finora
- Odontogenesis: Dr. Brian E. EsporlasDocumento20 pagineOdontogenesis: Dr. Brian E. EsporlasJhonatan Alfaro RondinelNessuna valutazione finora