Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
El Uso Del Treponema Pallidum Específico Captia Sífilis IgG Ensayo en Conjunto Con La Reagina Plasmática Rápida para La Prueba de Sífilis
Caricato da
alexandre147Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
El Uso Del Treponema Pallidum Específico Captia Sífilis IgG Ensayo en Conjunto Con La Reagina Plasmática Rápida para La Prueba de Sífilis
Caricato da
alexandre147Copyright:
Formati disponibili
JOURNAL OF CLINICAL MICROBIOLOGY, May 1997, p.
11411143
0095-1137/97/$04.0010
Copyright q 1997, American Society for Microbiology
Vol. 35, No. 5
Use of the Treponema pallidum-Specific Captia Syphilis IgG
Assay in Conjunction with the Rapid Plasma Reagin
To Test for Syphilis
BARBARA S. REISNER,* LINDA M. MANN, CINDY A. THOLCKEN, REBECCA T. WAITE,
AND GAIL L. WOODS
Department of Pathology, University of Texas Medical Branch, Galveston, Texas
Received 8 October 1996/Returned for modification 5 December 1996/Accepted 6 February 1997
The Captia Syphilis IgG enzyme immunoassay (EIA) was evaluated for use in conjunction with the rapid
plasma reagin test (RPR) as a method to test for syphilis. A total of 1,288 serum specimens were tested by the
routine laboratory protocol of the RPR followed by microhemagluttination assay for Treponema pallidum
(MHA-TP) testing of RPR-reactive sera as well as the EIA-RPR protocol in which the automated EIA followed
by a manual RPR test for EIA-positive specimens is used. When using the routine protocol, 131 specimens were
initially reactive by the RPR, and 113 of these were reactive by MHA-TP. When using the EIA-RPR protocol,
170 specimens were initially positive by EIA, and of these, 112 were RPR reactive, indicating active disease.
When compared to the routine protocol, the EIA-RPR protocol had sensitivity, specificity, and positive and
negative predictive values of 96.5, 99.7, 97.3, and 99.7%, respectively. After resolution of discrepancies by
additional testing, the adjusted sensitivity, specificity, and positive and negative predictive values were 100,
99.8, 98.3, and 100%, respectively. This evaluation demonstrates that when used in conjunction with the RPR,
the Captia Syphilis EIA is a reliable method by which to test for syphilis.
Treponema pallidum, the causative agent of syphilis, is very
difficult to culture (1, 6), and specimens for direct detection are
often not available from patients with latent or late stages of
the disease; therefore, serologic testing plays an important role
in the diagnosis of syphilis. The serologic tests most commonly
used in the United States to screen for this disease are the
nontreponemal Venereal Disease Research Laboratory test
and the rapid plasma reagin test (RPR) (4). The nontreponemal tests, in general, are ideal for screening large numbers of
specimens because they are sensitive and technically simple to
perform. However, because they measure the hosts response
to nontreponemal antigens (lipoidal material released from
damaged host cells as well as lipoprotein-like material released
from the treponemes), they are not specific, and in certain test
populations as many as 50% of the RPR-reactive specimens
will be negative in a treponeme-specific test, indicating a falsepositive reaction (3). Because of the problem with specificity, a
positive nontreponemal screening test should be confirmed
with a specific treponemal test such as the fluorescent treponemal antibody-absorption test (FTA-ABS) or microhemagluttination assay for T. pallidum (MHA-TP).
While the nontreponemal screening tests are technically
simple, they are labor-intensive and their results can be difficult
to interpret. For laboratories that screen large numbers of
specimens, an automated method for performing the syphilis
screen is desirable. Recently, the Captia Syphilis IgG enzyme
immunoassay (EIA; Centacore Inc., Malvern, Pa.) became
available as an automated treponemal test for detecting antibodies against T. pallidum. Data from several studies in which
this test was evaluated indicate that the EIA is both sensitive
and specific (2, 5, 79). However, because antibodies to T.
pallidum persist long after the disease has been successfully
treated, some of these investigators recommended combining
the EIA with an additional test such as the RPR or Captia
Syphilis IgM EIA to specifically diagnose active disease (2, 5, 7,
8). The purpose of our study was to evaluate the use of the EIA
in conjunction with the RPR (EIA-RPR) as a laboratory protocol for diagnosing active syphilis.
* Corresponding author. Mailing address: Department of Pathology,
Clinical Microbiology Laboratory, University of Texas Medical
Branch, 301 University Blvd., Galveston, TX 77555-0740. Phone: (409)
772-1120. Fax: (409) 772-5683. E-mail: breisner@mspo4.med.utmd
.edu.
RESULTS
MATERIALS AND METHODS
Testing protocol. Sera were tested by the Macro-Vue RPR (Becton Dickinson
Microbiology Systems, Cockeysville, Md.) and Captia Syphilis IgG EIA. In the
routine laboratory protocol, RPR-reactive sera were subsequently tested by the
Sera-Tek MHA-TP (Miles Inc., Elkhart, Ind.). For RPR-reactive specimens, if
the results obtained by the EIA and MHA-TP did not agree, both tests were
repeated once. Sera whose results remained discrepant after repeat testing were
tested by the Virgo FTA-ABS (Pharmacia Diagnostics Inc., Franklin, Ohio).
Patient chart review was performed when discrepancies were not resolved by
additional testing. Sera that were RPR and MHA-TP or FTA-ABS reactive were
considered diagnostic of active syphilis.
Serologic methods. The RPR, MHA-TP, and the FTA-ABS were performed
according to the manufacturers instructions. The EIA was performed with the
WellPrep automated pipetting and washing system (Denley Instruments, Ltd.,
Billingshurst, United Kingdom). Briefly, 5 ml of specimens from patients and
controls (one high-positive control, three low-positive standards, and one negative control) were transferred to microtiter wells coated with T. pallidum antigen
containing 100 ml of diluent. After incubation for 60 min at 378C, the wells were
washed with phosphate-buffered saline (pH 7.0 to 7.2) containing 0.05% Tween
20. Anti-human immunoglobulin G (IgG) monoclonal antibody labeled with
biotin and streptavidin-horseradish peroxidase conjugate was added, and the
plate was incubated at 378C for 60 min. After a final wash, tetramethylbenzidine
substrate was added, and the plate was incubated at room temperature for 30
min. Index values, calculated by dividing the test sample absorbances by the
mean absorbance for the three low-positive standards, were used to determine
positive and negative results.
Samples with equivocal EIA results were retested in duplicate, as recommended by the manufacturer. Results for specimens that remained equivocal
after repeat testing were not used in the comparison.
A total of 1,288 serum specimens were included in the evaluation. When the routine laboratory protocol was used (RPR
followed by MHA-TP), 131 specimens were RPR reactive and
1141
1142
REISNER ET AL.
J. CLIN. MICROBIOL.
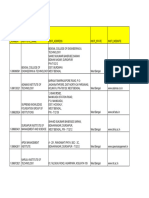
TABLE 1. Comparison of EIA-RPR to the RPR-MHA-TP for the
laboratory diagnosis of syphilis
EIA-RPR
resulta
No. of serum specimens with the following RPRMHA-TP result:
Reactive
Nonreactive
Total
Positive
Negative
109
4
3
1,167
112
1,171
Total
113
1,170
1,283
Sensitivity, 96.5%; specificity, 99.7%.
113 of these were reactive by MHA-TP. By the EIA-RPR
protocol, 170 specimens were EIA positive and 112 of these
were RPR reactive. Four specimens were repeatedly equivocal
by EIA (all four were RPR and MHA-TP nonreactive), and
one specimen had equivocal results by EIA but an insufficient
amount of sample was available for retesting (this specimen
was RPR and MHA-TP reactive). The test results for these five
specimens were excluded from further analysis.
When comparing the EIA-RPR protocol to the routine protocol for the remaining 1,283 specimens, 109 specimens were
positive by both methods, 4 were positive by the routine protocol only, 3 were positive by the EIA-RPR protocol only, and
1,167 specimens were negative by both methods (Table 1). The
sensitivity, specificity, and positive and negative predictive values of the EIA-RPR protocol for the diagnosis of syphilis were
96.5, 99.7, 97.3, and 99.7%, respectively.
In an attempt to resolve the discrepancies that occurred
between the two protocols, the EIA and the MHA-TP were
repeated for specimens with discrepant results. None of the
MHA-TP results changed upon repeat testing; however, for
the four specimens that were initially RPR and MHA-TP reactive but EIA negative, the EIA result became positive on
retesting. The three specimens that were initially EIA positive,
RPR reactive, and MHA-TP nonreactive remained EIA positive on retesting. One of these specimens was FTA-ABS reactive. The other two were FTA-ABS nonreactive; one was from
a patient being treated for syphilis, but the clinical indications
for treatment were not mentioned in the patients chart; the
other was from a patient with no history of syphilis. The RPR
titers for the latter two specimens were 1:1 and 1:2, respectively. After resolution of the discrepancies by additional testing, 114 specimens were positive by the EIA-RPR protocol and
reactive by the RPR and MHA-TP or FTA-ABS, 1,167 specimens were negative by both protocols, and 2 specimens were
positive by the EIA-RPR protocol only (Table 2). The adjusted
sensitivity, specificity, and positive and negative predictive values after resolution of the discrepancies were 100, 99.8, 98.3,
and 100%, respectively.
TABLE 2. Performance of EIA-RPR protocol after resolution
of discrepancies
EIA-RPR
resulta
No. of serum specimens with results:
Diagnostic of
syphilis
Not diagnostic of
syphilis
Total
Positive
Negative
114
0
2
1,167
116
1,167
Total
114
1,169
1,283
Sensitivity, 100%; specificity, 99.8%.
DISCUSSION
We evaluated the ability of the Captia Syphilis IgG EIA in
conjunction with the RPR to accurately diagnose syphilis.
When using the EIA as a preliminary screen to identify those
specimens that required additional testing by the RPR to diagnose active syphilis, 170 specimens required additional testing. When using the RPR as a preliminary screen to identify
those specimens that required additional testing by MHA-TP
to confirm the specificity of the reaction, 131 specimens required additional testing. Although the EIA-RPR protocol
resulted in more specimens that required additional testing
because it detects antibody in sera from patients with a history
of treated syphilis, the reduction in the number of manual
RPR performed by this protocol results in considerable savings
in technical time. On the basis of a time study performed in our
laboratory, the technical time required to perform the EIA is
roughly half that required to perform the manual RPR (approximately 0.5 and 1 min per specimen, respectively). Because
the reagent cost for the EIA is greater than that for the RPR,
each laboratory should determine the potential savings on the
basis of in-house time studies and the volume of tests performed.
The sensitivity and specificity of the EIA in conjunction with
the RPR for the laboratory diagnosis of syphilis were high,
both in the initial testing (96.5 and 99.7%, respectively), which
reflects the performance that can be expected in actual use,
and after resolution of discrepancies (100 and 99.8%, respectively). For the four specimens with discrepant results that
were initially EIA negative but that retested EIA positive, the
reason for the error is unknown; it is likely that technical errors
occurred, but it is not clear whether these were instrument or
operator errors. The high sensitivity and specificity of the EIARPR in this study are similar to the findings of previous studies
in which the EIA was used alone to diagnose syphilis. The
reported sensitivities in those studies were 93.9 and 100% and
the specificities were 98.6 and 98.2% (2, 7). The increased
specificity that we observed is likely a result of including RPR
testing in our protocol to test for active disease.
Resolution of equivocal results is an important consideration when using the EIA. During the evaluation reported
here, 17 of the 1,288 specimens initially had equivocal results
by EIA: the results for 5 specimens could not be resolved by
repeat testing and were subsequently excluded from the analysis; 5 specimens retested EIA negative, agreeing with the
MHA-TP result; 2 specimens retested EIA positive, agreeing
with the FTA-ABS result or the patient history of syphilis; and
5 specimens retested EIA positive, but the results disagreed
with those of the other treponemal serologic tests and chart
review indicated no history of syphilis. All five of the specimens
in this last group were RPR negative; therefore, the EIA result
should not have affected the treatment of the patient. However, this finding suggests that retesting of EIA-equivocal,
RPR-nonreactive specimens is unreliable.
Following the completion of this evaluation, we began using
the EIA-RPR protocol to test for syphilis in our laboratory,
which performs up to 2,600 tests per month. In our protocol,
sera are initially screened for antibodies against T. pallidum by
EIA, with all positive sera subsequently tested by the RPR.
When an equivocal EIA result is obtained, an RPR is performed; if the RPR is nonreactive, no further testing by EIA is
performed on the specimen to resolve the equivocal result. If
the RPR is reactive, the EIA is repeated in duplicate. For
RPR-reactive specimens whose results remain equivocal by
EIA, an MHA-TP is performed to obtain a final result.
Since implementing this protocol in our laboratory, 302
VOL. 35, 1997
CAPTIA SYPHILIS IgG EVALUATION
(2.8%) of the first 10,763 specimens had equivocal results. Of
these 302 specimens, 187 were RPR nonreactive, and no further testing was done, as indicated by our protocol. Of the 115
that were RPR reactive, the results for 47 were resolved on
repeat testing, but 68 (0.6% of the total specimens tested)
repeatedly had equivocal results and were subsequently tested
by MHA-TP (60 were MHA-TP reactive and 8 were MHA-TP
nonreactive). Our experience demonstrates that it is important
for laboratories that use this EIA to have a protocol in place
for resolving the results for specimens with repeatedly equivocal results. It is our recommendation that another treponemal
test, such as the MHA-TP, be used to resolve equivocal results
for these specimens.
REFERENCES
1. Fieldsteel, A. H., D. L. Cox, and R. A. Moeckli. 1981. Cultivation of virulent
Trepomena pallidum in tissue culture. Infect. Immun. 32:908915.
1143
2. Hooper, N. E., D. C. Malloy, and S. Passen. 1994. Evaluation of a Treponema
pallidum enzyme immunoassay as a screening test for syphilis. Clin. Diagn.
Lab. Immunol. 1:477481.
3. Larsen, S. A. 1989. Syphilis. Clin. Lab. Med. 9:545557.
4. Larsen, S. A., B. M. Steiner, and A. H. Rudolph. 1995. Laboratory diagnosis
and interpretation of tests for syphilis. Clin. Microbiol. Rev. 8:121.
5. Lefevre, J. C., M. A. Bertrand, and R. Bauriaud. 1990. Evaluation of the
Captia enzyme immunoassays for detection of immunoglobulins G and M to
Treponema pallidum in syphilis. J. Clin. Microbiol. 28:17041707.
6. Norris, S. J. 1982. In vitro cultivation of Treponema pallidum: independent
confirmation. Infect. Immun. 36:437439.
7. Silletti, R. P. 1995. Comparison of Captia Syphilis G enzyme immunoassay
with rapid plasma reagin test for detection of syphilis. J. Clin. Microbiol.
33:18291831.
8. Young, H., A. Moyes, A. McMillan, and J. Patterson. 1992. Enzyme immunoassay for anti-treponemal IgG: screening or confirmatory test? J. Clin.
Pathol. 45:3741.
9. Young, H., A. Moyes, A. McMillan, and D. H. H. Robertson. 1989. Screening
for treponemal infection by a new enzyme immunoassay. Genitourin. Med.
65:7278.
Potrebbero piacerti anche
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Development Developmental Biology EmbryologyDocumento6 pagineDevelopment Developmental Biology EmbryologyBiju ThomasNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Tool Charts PDFDocumento3 pagineTool Charts PDFtebengz100% (2)
- Building Services Planning Manual-2007Documento122 pagineBuilding Services Planning Manual-2007razanmrm90% (10)
- IEC TC 56 Dependability PDFDocumento8 pagineIEC TC 56 Dependability PDFsaospieNessuna valutazione finora
- Sources of Hindu LawDocumento9 pagineSources of Hindu LawKrishnaKousikiNessuna valutazione finora
- Meno's Paradox of Inquiry and Socrates' Theory of RecollectionDocumento10 pagineMeno's Paradox of Inquiry and Socrates' Theory of RecollectionPhilip DarbyNessuna valutazione finora
- Activity On Noli Me TangereDocumento5 pagineActivity On Noli Me TangereKKKNessuna valutazione finora
- Canon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFDocumento13 pagineCanon Powershot S50 Repair Manual (CHAPTER 4. PARTS CATALOG) PDFRita CaselliNessuna valutazione finora
- 2014 - A - Levels Actual Grade A Essay by Harvey LeeDocumento3 pagine2014 - A - Levels Actual Grade A Essay by Harvey Leecherylhzy100% (1)
- Desktop 9 QA Prep Guide PDFDocumento15 pagineDesktop 9 QA Prep Guide PDFPikine LebelgeNessuna valutazione finora
- Quiz 140322224412 Phpapp02Documento26 pagineQuiz 140322224412 Phpapp02Muhammad Mubeen Iqbal PuriNessuna valutazione finora
- Journal of Biology EducationDocumento13 pagineJournal of Biology EducationFarah ArrumyNessuna valutazione finora
- ReadmeDocumento2 pagineReadmechethan100% (1)
- DBMS Lab ManualDocumento57 pagineDBMS Lab ManualNarendh SubramanianNessuna valutazione finora
- rp10 PDFDocumento77 paginerp10 PDFRobson DiasNessuna valutazione finora
- WBDocumento59 pagineWBsahil.singhNessuna valutazione finora
- Review On AlgebraDocumento29 pagineReview On AlgebraGraziela GutierrezNessuna valutazione finora
- AMULDocumento11 pagineAMULkeshav956Nessuna valutazione finora
- Genetics Icar1Documento18 pagineGenetics Icar1elanthamizhmaranNessuna valutazione finora
- BrochureDocumento3 pagineBrochureapi-400730798Nessuna valutazione finora
- English Homework 10 Grammar Focus 2: Lecturer: Mr. Dr. H. Abdul Hamid, M.SiDocumento4 pagineEnglish Homework 10 Grammar Focus 2: Lecturer: Mr. Dr. H. Abdul Hamid, M.SiMutiara siwa UtamiNessuna valutazione finora
- Cyber Briefing Series - Paper 2 - FinalDocumento24 pagineCyber Briefing Series - Paper 2 - FinalMapacheYorkNessuna valutazione finora
- Aleutia Solar Container ClassroomDocumento67 pagineAleutia Solar Container ClassroomaleutiaNessuna valutazione finora
- Economic Review English 17-18Documento239 pagineEconomic Review English 17-18Shashank SinghNessuna valutazione finora
- Microsmart GEODTU Eng 7Documento335 pagineMicrosmart GEODTU Eng 7Jim JonesjrNessuna valutazione finora
- Standard Answers For The MSC ProgrammeDocumento17 pagineStandard Answers For The MSC ProgrammeTiwiNessuna valutazione finora
- Brand Strategy - in B2BDocumento6 pagineBrand Strategy - in B2BKrishan SahuNessuna valutazione finora
- Caspar Hirschi - The Origins of Nationalism - An Alternative History From Ancient Rome To Early Modern Germany-Cambridge University Press (2012)Documento255 pagineCaspar Hirschi - The Origins of Nationalism - An Alternative History From Ancient Rome To Early Modern Germany-Cambridge University Press (2012)Roc SolàNessuna valutazione finora
- ML Ass 2Documento6 pagineML Ass 2Santhosh Kumar PNessuna valutazione finora
- Aluminum PorterDocumento2 pagineAluminum PorterAmir ShameemNessuna valutazione finora