Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
00 B 7 D 53 A 1 B 24 B 2 Fe 76000000
Caricato da
Sri HariTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
00 B 7 D 53 A 1 B 24 B 2 Fe 76000000
Caricato da
Sri HariCopyright:
Formati disponibili
International Journal of Medicine and Medical Sciences Vol 1.(10) pp.
425-431, October, 2009
Available online http://www.academicjournals.org/ijmms
ISSN 2006-9723 2009 Academic Journals
Full Length Research paper
Prevalence of breast cancer in menopausal blind
women
K. Pushkala1* and P. D. Gupta2
1
S. D. N. B. Vaishnav College for Women, Chennai, India.
2
Manipal University, Karnataka, India.
Accepted 18 September 2009
A correlation between prevalence of breast cancer with blindness has not been attempted in India and
only scanty information is available at the world scenario as well. We have done a pilot study by
epidemiological survey of blind menopausal (high risk age group) women (n = 204) from Chennai to find
the prevalence of the disease. In the present study, menopausal visually challenged women have
shown that the ratio at risk of developing breast cancer in this group is very much lower ( 1:100 )
compared to sighted women in the similar age group, The risk of developing breast cancer is 1:78
(Cumulative Risk 35 - 64 age), among sighted women in Chennai. Statistical analysis of the present
data also provide enough evidence that blind women who are > 40 years of age had 13% greater risk of
breast cancer compared with those in the study group < 40 years (RR = 1.125; 95% CI = 0.07 to
17.74).The susceptibility to develop the disease among partially blind women is almost twice than that
of totally blind women (RR = 2.14; 95% CI = 0.14 to 33.68). Similarly menopausal stage of a woman has
more risk of developing breast cancer than pre-menopausal stage (RR = 5.18; 95% CI = 0.33 to 80.75).
Vision loss after menarche also indicates an increased risk (RR = 8.27; 95% CI = 0.54 to 127.6).The
intervals for these risks give a very wide range of possible values for the corresponding risk ratio due
to small sample size and the rarity of breast cancer among blind women. The topographical location of
India close to the equator and life style pattern of the people could be the major reasons for the very
low prevalence of breast cancer in Chennai. None of the other high or low risk factors were found to be
influencing blind women to develop breast cancer. The relationship between visible light and breast
cancer can be studied by taking blind menopausal women as a model.
Key words: Blindness, breast cancer, epidemiology.
INTRODUCTION
Blue light is being identified as a new environmental
pollutant. Earlier we studied the effects of day light in
anopthalmic rats and concluded that the mammalian eye
sub serves at least two photic systems: the occipital
cortex, which mediates the conscious perception of light
and recognition of images and a subcortical system that
med-iates light-sensitive synchronization of the circadian
pace-maker (Foster et al., 1991; Chaurasia and Gupta,
1999; Jagota et al., 1999).
The clock-cancer connection has been proved from
investigations involving pilots, female flight attendants
and shift workers who are more likely to have disrupted
circadian cycles due to abnormal working hours in different
*Corresponding author. E-mail: kpushkala@gmail.com.
different parts of the world. Artificial light at night
disrupting the natural melatonin- estrogen balance was
linked with the increase in hormone regulated breast
cancer among women (Pukkala et al., 1995; Tynes et al.,
1996; Hansen, 2001 a, b; Pukkala et al., 2003; Hansen,
2006; Davis and Mirick, 2006; Schernmmer et al., 2006;
Franzese and Nigri, 2007; Viswanathan et al., 2007).
Blind women follow natural system of rhythm due to lack
of light through eyes. Blast et al. (2005) have established
that increase in melatonin levels causes the suppression
of tumor growth in-vivo in nude mice model.
The literature survey showed very scanty information
on the prevalence of breast cancer in blind women worldwide. The first preliminary evidence linking light to cancer
in people emerged from the register based studies of
Hahn (1991). He computed the incidence of this
malignancy in blind and sighted women and discussed
426 Int. J. Med. Med. Sci.
Low risk factor
High risk factor
250
200
150
100
50
0
Obesity
Problem in
the Breast
Pariety
Breast
Feeding
Family
history of
any cancer
Other
Cancers
Figure 1. Prevailing ratio of established risk factors observed among study subjects.
the connection between light and melatonin in visually
impaired women. As early as 1990, scientists reasoned
that anybody whose eye cannot detect light should be
resistant to estrogen generated tumors. This angle of
discussion paved way for the epidemiologist to reason
that people whose eyes can not detect light should prove
resistant to tumor growth. Subsequently, Feychting et al.
(1998) and Verkasalo et al. (1999) supported melatonin
hypothesis from their studies based on cancer registry in
Sweden and Finland respectively.
The later found 50% decreased risk of the disease and
an inverse association between breast cancer incidence
and degree of visual impairment. Similarly, Kliukiene
(2001) found only 5 subjects suffering from breast cancer
among15, 412 visually impaired subjects in Blind Registry
in Norway. Pukkala et al. (1999; 2006), added to the suggestive epidemiological evidence for the 40% decreased
risk of hormone related cancers in people with visual
impairment and consequently established a relationship
between exposer of visible light at night and breast
cancer risk in Finland.
The hypothesis is further advanced that blindness from
an early age may lead to a further reduced risk of breast
cancer through altered patterns of melatonin secretion by
the pineal gland. The effect of age at the onset, duration
and degree of blindness could also be assessed after
adjustment for known risk factors for breast cancer
(Coleman and Reiter, 1998).
India is the home to one of the worlds largest
population (12 million suffering from visual impairment,
Census of India, 2001). The literature survey did not
show any published data on visually impaired adult
menopausal women suffering from breast cancer in India.
We are interested to have data on breast cancer among
visually impaired menopausal women in the Indian
population, therefore, a pilot epidemiological survey was
undertaken to establish the prevalence of breast cancer
among visually impaired menopausal women in Chennai.
MATERIALS AND METHODS
This study included menopausal women with visual impairment
registered in governmental and non-governmental rehabilitation
centers as well as MMTR (Madras Metropolitan Tumor Registry)
during June, 2006 June, 2007. Since national registry for the blind
is not available, these three sources of information helped in the
present epidemiological survey.
In the present study, data were obtained from personal
communication with the study population of women as well as from
the cancer registry. For ascertaining the degree of visual
impairment (total blindness and partial blindness) a manual of
classification of impairments, disabilities and handicaps, WHO
Geneva, (1980) was used. The data on the risk of developing
cancer among normally sighted women was procured as curtsey
from MMTR 2003 - 2005 for comparison. Special care is taken to
prepare a proforma for recording the data (Sample is enclosed).
Only blind women menopausal age (30 - 40) and post menopausal
age as above 40 (risk age) were considered for the present study.
Women having menstrual cycle after 40 years are also included as
pre-menopausal stage. Statistical software Epi - Info (2005) was
used to analyze the data.
RESULTS
Chennai is situated at the sea level on the East coast of
India. It lies between 12 9' and 13 9' of the northern
latitude and 80 12' and 80 19' of the Southern longitude
2
spreading in 178.20 km area.
In the survey out of 204 (collected during 2006 - 2008)
menopausal blind women, we found only two subjects
suffering with breast cancer. The cancer was operated at
appropriate time and the subjects are now leading a
normal life until December, 2008.
"Well established" high risk factors for prevalence of
breast cancer such as obesity, problem in the breast,
parity, breast feeding, age of the first pregnancy, family
history of any cancer (genetic), age, suffering from other
cancers and suspected risk factors such as partial
blindness, late menopause (beyond 45 years) and age of
onset of blindness (before or after menarche) were also
considered for the analysis to find how many are at risk of
developing breast cancer in addition to their age (Figure 1).
The ratio of "well established" high risk factors for
prevalence of breast cancer such as, obesity, problem in
breast tissue, nulliparity, not breast fed, age of the first
pregnancy (above 35 years of age), family history of any
Pushkala and Gupta
427
Table 1. Observed frequencies for determining risk ratio or relative risk.
Exposed to factor
Unexposed to factor
Total
Disease present
a
c
a+c
cancer and those already suffering from other types of
cancer observed among the study group is represented
in the bar chart in Figure 1.
High risk factors
Disease absent
b
d
b+d
Total
a+b
c+d
n = a+b+c+d
Estimated relative risk (RR) =
Estimated risk in the exposed group
Estimated risk in the unexposed group
= a /(a+b)
c/(c+d)
The 95% confidence interval for the true population, ln
RR is given by:
Obese, problem in the breast, no parity, not breast fed,
having family history of cancer, prevalence of other
cancers.
(ln RR - 1.96* SE (ln RR)) to (ln RR + 1.96* SE (ln RR))
and the standard error (SE) of ln RR is given by:
Low risk factors
SE (ln RR) =
No problem in the breast, parity, breast fed, no family
history of cancer, absence of other cancers.
1
1
1
1
+
a a+b c c+d
Among the study subjects 4% were obese, 11.27% suffer
from other problems in the breast tissue. 60.78% did not
feed their children and 14.22% show nulliparity. 12.25%
had the first child above 35 years old (late pregnancy)
and 12.25% have family history of cancer. In addition,
suspected risk factors such as late menopause (16.2%),
partial blindness ( 31.86%) and age of on set of blindness
(after menarche) ( 10.78%) were also recorded. Even
though these risk factors were observed, among the
study group only two had breast cancer. Among those,
one is forty five years old (in 2007), weaver, suffers from
total blindness, lost her vision when she was 13 days old
baby, unmarried, attained menarche at the age of 13 and
is in menopause now and the other one is thirty seven
years old (in 2007) partially blind, homemaker,
unmarried, attained menarche at the age of 12 (early
menarche) and is in pre-menopausal stage now.
Antilog (e ) of these lower and upper limits in order gives
the 95% confidence interval for the population relative
risk.
Statistical analyses of the data also provide enough
evidence that blind women who are > 40 years of age
had 13% greater risk of breast cancer compared with
those in the study group < 40 years (RR = 1.125; 95% CI
= 0.07 to 17.74) in our study. The susceptibility to
develop the disease among partially blind women is
almost twice than that of totally blind women (RR = 2.14;
95% CI = 0.14 to 33.68). Similarly postmenopausal stage
of a woman has more risk of developing breast cancer
than pre-menopausal stage (RR = 5.18; 95% CI = 0.33 to
80.75). Vision loss after menarche also indicates an
increased risk (RR = 8.27; 95% CI = 0.54 to 127.6).
The intervals for these relative risks give a very wide
range of possible values for the corresponding risk ratio
may be due to the small sample size and the rarity of
breast cancer among blind women.
Statistical analyses
DISCUSSION
Relative risk (RR) was used as a measure of association
between risk factors and susceptibility to develop breast
cancer in women; the RR was defined as the ratio of the
risk of developing a disease among those exposed to a
specified risk to those not exposed to this risk. The 95%
confidence intervals (CI) for these relative risks were also
calculated.
The risk ratio or relative risk (RR) is used to find the
association between a disease and a possible risk factor.
The observed frequencies are given in Table 1. RR is
calculated thus:
Breast cancer is the leading cause of death in women all
over the world. According to the report of World Health
Organization (WHO) 519, 000 deaths occur every year
worldwide (WHO, 2009).
Studies indicate that due to changed life style in India
increasing rate of breast cancer is quite alarming. Now, it
is second most common malignancy in Indian women
(Yeole and Kurkure, 2003). During 2005, study
conducted by the International Association of Cancer Research, based in Lyon, France, projected that there would
be 250, 000 cases of breast cancer in India by 2015, a 3%
428 Int. J. Med. Med. Sci.
increase per year. Currently, India reports roughly 100,
000 new breast cancer cases annually though a
significant regional variations in incidence rates persists.
The overall rate is now estimated at 80 new cases per
100, 000 population per year (Bagchi, 2008). According
to an Indian health News report one in 22 women in India
are likely to suffer from breast cancer during their lifetime,
while the figure is definitely more in America with one in
eight being a victim of this cancer. Breast cancer
incidence had zoomed by 200% since 1982. The threeand-half-year-long study was initiated after the number of
breast cancer cases exceeded that of cervical cancer in
the Madras Metropolitan Tumor Registry in 2003. In
Chennai, the most common cancer among women
relates to the breast and though the incidence is 50%
lower in rural areas, it has been steadily increasing. Women
above 30 years of age are the most likely to get cancer
(Shantha et al., 2003).
This pilot epidemiological study is the first attempt to
collect scientific data on blind menopausal women with
respect to breast cancer. No studies have been done in
India earlier to find neither prevalence nor incidence rate
of breast cancer in blind women. Comparison of the present data is not possible with existing observations of the
register based studies from Scandinavian countries due
to lack of registry for blind subjects in India.
In the present study, visually challenged menopausal
women has shown the risk of developing breast cancer in
life time is very much lower 1:100 (n = 204) since, only
two suffered from the disease among our study group.
However, Shantha et al. (2008) showed that the risk of
developing breast cancer among sighted women in
Chennai is 1:78 (Cumulative Risk 35 - 64 age).
Feychting et al. (1998) supported melatonin hypothesis
with the cohort study consisting of 1, 567 totally blind and
13, 292 severely visually impaired subjects from Swedish
cancer registry and found that blind people have a lower
cancer incidence. Similarly, Verkasalo et al. (1999) also
found 50% decrease in the risk of developing the
disease. They also showed an inverse association
between breast cancer incidence and degree of visual
impairment from cancer registry in Finland. The health
survey data from the cancer registry of Norwegian
government had approximately 15, 412 visually impaired
entries. Among them only 5 subjects suffered from breast
cancer (Kliukiene, 2001).
Subsequently, Pukkala et al. (1999; 2006), from a
cohort study consisting of people with visual impairment
identified from Finnish cancer registry for years 1983 2003 added to the suggestive epidemiological evidence
for the decreased risk of hormone related cancers in
people with visual impairment. The cohort consisted of
17, 557 of persons with visual impairment (11, 147
women, 6,410 men) showing only 184 cases of breast
cancer, which represented a 40% decrease in the risk of
developing breast cancer and established a relationship
between visible light at night and breast cancer risk.
Due to the topographical location of India (being close
to the equator), having almost 12 h light and dark cycle,
unlike the Scandinavian countries, having long day / night
periods due to the location close to the poles. Image
forming photic receptors are absent in blinds but photic
receptors for synchronization of circadian rhythms are
present in visually impaired subjects. Therefore, they
maintain a natural and normal circadian rhythm Jagota et
al. (1999). However, the photic reception which is responsible for perception of light is lacking in blind women and
so they may become less prone to breast cancer. In the
Indian scenario circadian rhythms are more stable than
Scandinavian countries and this could be the major
reason for the very low prevalence of breast cancer reported compared to the Scandinavian countries in this study.
Other reasons for low prevalence of breast cancer in
Indian blind population may be due to their abstinence
from smoking (Gammon et al., 2004), alcohol and under
taking vigorous physical activity compared to
Scandinavian population (Detailed Guide: Breast Cancer,
2008). In the present investigation among our study
group 60.78% did not feed their children and 14.22%
showed nulliparity, 12.25% had their first child above 35
years old (late pregnancy) showing that they fall under
"well established" risk factors (Barnett et al., 2006;
Goodwin, 2008; Travis et al., 2006) for developing breast
cancer however, these risk factors did not show much
effect on blind population, nevertheless these account for
50 55% of the breast cancer risk among Westernized
populations.
Similarly, single women and nulliparous married
women were prone to the disease approximately 1.4
times more than that of parous married women. The
published data showed that, women who breast fed their
infants had a 17% lower risk of breast cancer compared
to women who did not breast fed (Hendry, 2008). Women
whose first child was born before they were 20 years of
age had approximately less 50% risk of developing
breast cancer than women whose first birth was at age
30 years (Leslie Bernstein et al., 2003). Among the study
subjects 12.25% have family history of cancer. About 5 to
10% of breast cancer cases world wide are thought to be
hereditary, resulting directly from gene mutations,
inherited from a parent(s). Altogether, about 20 to 30% of
women with breast cancer have a family member with
this disease (Detailed Guide: Breast Cancer, 2008;
Gajalakshmi et al., 1998). In addition, suspected risk
factors such as, obesity (4%), other problems in the
breast tissue (11.27%), late menopause (16.2%), partial
blindness (31.86%) and age at on set of blindness (after
menarche) (10.78%) were also recorded. It has been
calculated that women with menopause at each 5 year
age difference have 17% higher risk of breast cancer
(Hsieh et al., 2006).
It is surprising that the above discussed risk factors
seem to be either non-operative or suppressed in blind
menopausal women to develop the disease. However in
the two breast cancer cases the risk factors such as
nulliparity, not breast fed, early menarche and partial
Pushkala and Gupta
blindness (case-I) could be the contributory factor of the
cancer susceptibility genes such as P53, BRCA I and
BRCA II etc. (Detailed Guide: Breast Cancer, 2008). No
other obvious reasons can be assigned to these two
cases for developing breast cancer in the present study.
Encouraged with this data we have extended our study to
the whole province of Tamil Nadu with the population 62,
405, 679 including 964, 063 visually handicapped
subjects.
Conclusion
The result of the present study is an additional epidemiological evidence suggesting a relationship between visible light
and breast cancer risk. However, little is known about
possible molecular mechanisms underlying this clockcancer connection. So, further study at the molecular
level is very essential to confirm the reason for the very
low prevalence of breast cancer in the Indian scenario.
ACKNOWLEDGEMENTS
Our sincere thanks to Dr. R. Swaminathan, Senior
Biostatistician, Division of Epidemiology and Cancer
Registry, Cancer Institute (Indian Womens Association
W. I. A), Adayar, Chennai, Dr. R. Ramakrishnan, Deputy
Director, National institute of epidemiology, Chennai,
Christian foundation for the Blind-India (CFBI), Chennai
and Dr. R. Malathi and Dr. R. Geetha from Statistics
Department, S. D. N. B. Vaishnav College for women,
Chennai for their help in the statistical analysis of the
data The financial support from UGC , New Delhi is also
acknowledged.
REFERENCES
Bagchi S (2008). Breast cancer rises in India. Can. Med. Assoc. J., 179
: 27.
Barnett GC, Shah M, Redman K, Easton DF, Ponder AJ, Pharoah PDP
(2008). Risk Factors for the Incidence of Breast Cancer: Do They
Affect Survival From the Disease? J. Clin. Oncol., 26: 3310-3316.
Bernstein L, Teal CR, Joslyn S, Wilson J ( 2003). Ethnicity-Related
Variation in Breast Cancer Risk Factors, Cancer, 97: 222229.
Blask DE, Brainard GC, Dauchy RT, Hanifin JP, Davidson LK, Krause
JA, Sauer LA, Rivera-Bermudez MA, Dubocovich ML, Jasser SA,
Lynch DT, Rollag MD, Zalatan F (2005). Melatonin-depleted blood
from premenopausal women exposed to light at night stimulates
growth of human breast cancer xenografts in nude rats. Cancer Res.,
65: 11174-11184.
Chaurasia SS, Gupta PD (1999). Cryptochromes: The novel circadian
photo receptors. Curr. Sci., 77: 55.
Coleman MP, Reiter RJ
(1992). Breast cancer, blindness and
melatonin. Eur. J. Cancer, 28: 501-503.
Davis S, Mirick DK (2006). Circadian disruption, shift work and the risk
of cancer: a summary of the evidence and studies in Seattle. Cancer
Causes and Control, 17:539-545.
Detailed Guide: Breast Cancer; What Are the Risk Factors for Breast
Cancer?. Copyright 2008 American Cancer Society, Inc. [Revised:
09/13/2007]. Available from: http://www.cancer.org/docroot/CRI/
429
content/CRI_2_4_2X_What__are_the_risk_factors_for_breast_cancer_
5.asp?sitearea=
Disabilities Data, Directorate of Census Operations-Tamil Nadu,
Census of India, 2001.
Epi Info [computer program]. Version 3.3.2.Atlanta: Centers for Disease
Control and Prevention; 2005.
Feychting M, Osterlund B, Ahlbom A (1998). Reduced cancer
incidence among the blind. Epidemiol., 5: 490-494.
Foster RG, Provencio I, Hudson D, Fiske S, De Grip WJ, Menaker M
(1991). Circadian Photoreception in the retinally degenerate mouse
(rd/rd). J Comp Physiol., A. 169 :39-50.
Franzese E, Nigri G (2007). Night work as a possible risk factor for
breast cancer in nurses. Correlation between the onset of tumors
and alterations in blood melatonin levels. Prof Inferm., 60: 89-93.
[Article in Italian].
Gajalakshmi CK, Shanta V, Matti Hakama M (1998). Risk factors for
contralateral breast cancer in Chennai (Madras), India. Intern J
Epidemiol., 27:743-750.
Gammon MD, Eng SM, Teitelbaum SL, Britton JA, Kabat GC, Hatch M.
et al. (2004). Environmental tobacco smoke and breast cancer
incidence. Environ Res., 96:176-185.
Goodwin PJ (2008). Host-Related Factors in Breast Cancer: An Under
appreciated Piece of the Puzzle? J. Clin. Oncol., 26: 3299-3300.
Hahn RA (1991). Profound bilateral blindness and the incidence of
breast cancer. Epidemiol., 2:208210.
Hansen J (2001a). Light at Night, Shift work, and Breast Cancer Risk.
J Natl Cancer Inst.93: 1513-1515.
Hansen J (2001b). Increased breast cancer risk among women who
work predominantly at night. Epidemiol., 12:7477.
Hansen J (2006). Risk of breast cancer after night- and shift work:
current evidence and on going studies in Denmark. Cancer Causes
and Control, 17: 531-537.
.Hendry J (2008). Being breast-fed may lower breast cancer risk. Print.
Last Updated: 2008-05-09 12:00:24 -0400 (Reuters Health)
www.breastcancer.org/risk/new_research/ 20080509.jsp )
Hsieh C, Trichopoulos D, Katsouyanni K, Yuasa S (2006). Age at
menarche, age at menopause, height and obesity as risk factors for
breast cancer: Associations and interactions in an international casecontrol study. Int. J. Cancer, 46 : 796-800.
Jagota A, Olcese J, Harinarayana Rao S, Gupta PD (1999). Pineal
rhythms are synchronized to light-dark cycles in congenitally
anophthalmic mutant rats. Brain Res. 825 :95-103.
Kliukiene J, Tynes T, Andersen A (2001). Risk of breast cancer
among Norwegian women with visual impairment. Brit J. Cancer,
84:397399.
Pukkala E, Auvinen H, Wahlberg G (1995). Incidence of cancer
among Finnish airline cabin attendants, 196792. Brit. Med. J.,
311:64952.
Pukkala E, Verkasalo PK, Ojamo M, Rudanko SL (1999). Visual
impairement and cancer: a population based cohort study in Finland.
Cancer Causes and Control, 10: 13-20.
Pukkala E, Aspholm R, Auvinen A, Eliasch H, Gundestrup M, Haldorsen
T, Hammar N, Hrafnkelsson J, Kyyrnen P, Linnersj A, Rafnsson V,
Storm H, Tveten U (2003).Cancer incidence among 10,211 airplain
pilots: A Nordic study. Aviat Space Environ. Med. 74 : 699-706.
Pukkala E, Ojamo M, Rudanko SL, Stevens RG, Verkasalo PK (2006).
Does incidence of breast cancer and prostate cancer decrease with
increasing degree of visual impairment. Cancer Causes and Control,
17:573576.
Schernmmer ES, Kroenke CH, Laden F. Hankinson SE (2006). Night
work and risk of breast cancer. Epidemiol., 17: 108-111.
Shantha V, Swaminathan R, Nalini, Kavitha M. Population based
cancer registry, Chennai Cancer Institute (WIA ...File Format:
PDF/Adobe Acrobat - View as HTMLIndividual Registry Data: 20012003. Chennai. 135.
Cancer Institute (WIA), Adyar, Chennai. Registration area ...
www.icmr.nic.in/...2001.../04_Chennai%20Pages%20135%20to%201
53.pdf - Similar
Shantha V, Swaminathan R, Balasubramanian S (2008). Cancer
incidence and mortality in Chennai-India : 2003-2005. National
cancer registry Programme Cancer Institute (W.I.A.), Chennai.
Travis RC, Allen DS, Fentiman IS, Key TJ (2004). Melatonin and Breast
430 Int. J. Med. Med. Sci.
Cancer: A Prospective Study. J Natl Cancer Inst. 96:475-482.
Tynes T, Hannevik M, Andersen A, Vistnes A, Haldorsen T (1996).
Incidence of breast cancer i Norwegian female radio and telegraph
operators. Cancer Causes and Control. 7:197204.
Verkasalo PK, Pukkala E, Stevens RG, Ojamo M, Rudanko SL (1999).
Inverse association between breast cancer incidence and degree of
visual impairment in Finland. Brit. J. Cancer. 80:14591460.
Viswanathan AN, Hankinson SE, Schernmmer ES (2007). Night
shift work and the risk of endometrial cancer. Cancer Res. 67:
10618-10622.
World Health Organization, 1980). 2. International Classification of
Functioning, Disability and Health (Geneva: World Health
Organization, 2001). ...
secure.cihi.ca/cihiweb/en/downloads/icf_
jun02_papers_3B_e.pdf WHO/World Cancer Day. 4 February 2009. Cancer is a leading cause
of death around the world. WHO estimates that 84 million people will
die of cancer between 2005 ... www.who.int/ mediacentre/
events/.../world_ cancer.../index.html
Yeole BB , Kurkure AP (2003). An epidemiological assessment of
increasing incidence and trends in breast cancer in Mumbai and
other sites in India, during the last two decades . Asian Pac. J.
Cancer Prev. 2003 ; 4: 51-56
APPENDIX
INCIDENCE OF BREAST CANCER IN BLIND WOMEN EPIDEMIDLOGICAL STUDIES
Proforma 1.
(A)
(B)
1 Project area: Eye research
2 Organization undertaking the project -------------------------3 Name of field worker: ----------------------------------------------4 Name of village: ----------------------------------------------------5 Taluka and District: -------------------------------------------------6 Date of survey: ------------------------------------------------------1.
2.
3.
4.
5.
6.
7.
8.
9.
Name of the subject: ---------------------------------------------Address: ----------------------------------------------------------Date of birth and age: -------------------------------------------Type of blindness: Total -------- Partial ----------------Occupation: -------------------------------------------------------Cast / Religion: ---------------------------------------------------Marital status: Married----------- Unmarried ----------Age of marriage: ----------------------Issues:
Age of first pregnancy: --------------Age of second pregnancy: ---------Age of third pregnancy: --------------
10.
11.
Miscarriages / Abortions: Yes ------- No -------Breast feeding the baby: Yes ------ No ------If No why: ----------
12.
13.
Have you any problem in breast: (A) Lump ------ (B) Pain ----- (C) Any other
Any family history of breast cancer: (A) Grandmother ------ (B) Mother -----(C) Mothers sister ----- (D) Sister --------
Proforma 2.
1. Food habits :
Vegetarian -----Non-vegetarian -----2. Physical status :
Obese ----Normal ----week ----3. Socioeconomic condition :
Higher Middle -------Middle -----Lower Middle class ----4. Age of menarchy:
---------------5. Age of menopause:
--------------6. Age of acquirement of blindness:
-------------------
Pushkala and Gupta
7. Reason of blindness :
8. Any other disease :
9.
10.
11.
12.
Accidental ----- Disease -----Which ----------From when ------------
Congenital -------
Gynecological disease : -----------Regularity of cycle:
------------Have you taken any steroid medicine: Yes/No, if Yes Which -------Any Diagnosis/ Advise/ Treatment from doctor regarding the breast problem:-----------
431
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Renogram GuidelineDocumento14 pagineRenogram GuidelineSri HariNessuna valutazione finora
- 30 37Documento8 pagine30 37Sri HariNessuna valutazione finora
- Chapter 2 Radionuclide ImagingDocumento5 pagineChapter 2 Radionuclide ImagingSri HariNessuna valutazione finora
- Gallium and Indium ScanDocumento1 paginaGallium and Indium ScanSri HariNessuna valutazione finora
- Urological Applications of RadionuclidesDocumento89 pagineUrological Applications of RadionuclidesSri HariNessuna valutazione finora
- Lesson 1Documento6 pagineLesson 1Sri HariNessuna valutazione finora
- Intraluminal Navigation Through Any Hollow Viscus Is PossibleDocumento3 pagineIntraluminal Navigation Through Any Hollow Viscus Is PossibleSri HariNessuna valutazione finora
- Uro Dynamics 1Documento22 pagineUro Dynamics 1Sri HariNessuna valutazione finora
- Management of Acute and Chronic Retention in MenDocumento52 pagineManagement of Acute and Chronic Retention in MenSri HariNessuna valutazione finora
- Urological Applications of RadionuclidesDocumento89 pagineUrological Applications of RadionuclidesSri HariNessuna valutazione finora
- UroflowDocumento41 pagineUroflowSri HariNessuna valutazione finora
- Captopril Renography: Physiologic Principle - Loss of Preferential Vasoconstriction of The EfferentDocumento3 pagineCaptopril Renography: Physiologic Principle - Loss of Preferential Vasoconstriction of The EfferentSri HariNessuna valutazione finora
- Uro DynamicsDocumento64 pagineUro DynamicsSri HariNessuna valutazione finora
- Usg in UrologyDocumento25 pagineUsg in UrologySri HariNessuna valutazione finora
- Contrast Arteriography: Reasons Not As A Preliminary Screening ToolDocumento3 pagineContrast Arteriography: Reasons Not As A Preliminary Screening ToolSri HariNessuna valutazione finora
- CT Angiography in UrologyDocumento2 pagineCT Angiography in UrologySri HariNessuna valutazione finora
- Xray AbdomenDocumento22 pagineXray AbdomenSri HariNessuna valutazione finora
- Contrast Induced NephropathyDocumento2 pagineContrast Induced NephropathySri HariNessuna valutazione finora
- Contrast Induced NephropathyDocumento75 pagineContrast Induced NephropathySri HariNessuna valutazione finora
- Contrast Media: Dr.R.Abhiman Gautam, MCH Urology Prof - DR.RK Unit Stanley Medical CollegeDocumento18 pagineContrast Media: Dr.R.Abhiman Gautam, MCH Urology Prof - DR.RK Unit Stanley Medical CollegeSri HariNessuna valutazione finora
- Contrast Induced Nephropathy in Urology: Viji Samuel Thomson, Kumar Narayanan, J. Chandra SinghDocumento9 pagineContrast Induced Nephropathy in Urology: Viji Samuel Thomson, Kumar Narayanan, J. Chandra SinghSri HariNessuna valutazione finora
- Contrast Induced Nephropathy in Urology: Viji Samuel Thomson, Kumar Narayanan, J. Chandra SinghDocumento9 pagineContrast Induced Nephropathy in Urology: Viji Samuel Thomson, Kumar Narayanan, J. Chandra SinghSri HariNessuna valutazione finora
- Clean Intermittent Catheterization (CIC) : IndicationsDocumento2 pagineClean Intermittent Catheterization (CIC) : IndicationsSri HariNessuna valutazione finora
- Intravenous Radiographic Contrast Induced Adverse Reactions - Their Causes, Prevention and Relief MeasuresDocumento7 pagineIntravenous Radiographic Contrast Induced Adverse Reactions - Their Causes, Prevention and Relief MeasuresSri HariNessuna valutazione finora
- Contrast Induced NephropathyDocumento2 pagineContrast Induced NephropathySri HariNessuna valutazione finora
- Mccormick: Michael J. CoughlinDocumento1 paginaMccormick: Michael J. CoughlinSri HariNessuna valutazione finora
- Access SheathDocumento22 pagineAccess SheathSri HariNessuna valutazione finora
- Basic Sciences Pertaining To Critical CareDocumento6 pagineBasic Sciences Pertaining To Critical CareSri HariNessuna valutazione finora
- P-IV Recent Advances, Critical Care Audit and Quality ImprovementDocumento6 pagineP-IV Recent Advances, Critical Care Audit and Quality ImprovementSri HariNessuna valutazione finora
- P-II General Principles and Practices of Critical Care and ResuscitationDocumento6 pagineP-II General Principles and Practices of Critical Care and ResuscitationSri HariNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Mito-Meiosis Test AnswersDocumento11 pagineMito-Meiosis Test Answersrosidin_551390Nessuna valutazione finora
- Lec 1-2Documento7 pagineLec 1-2Monenus KedirNessuna valutazione finora
- Form No.1 Birth Report PDFDocumento4 pagineForm No.1 Birth Report PDFRiyas TkNessuna valutazione finora
- Her Deepest, Darkest Sex Secrets RevealedDocumento4 pagineHer Deepest, Darkest Sex Secrets RevealedporqNessuna valutazione finora
- Stages of LaborDocumento43 pagineStages of LaborMASII100% (1)
- Year 7 Cells and Reproduction-2Documento10 pagineYear 7 Cells and Reproduction-2BioScMentor-1Nessuna valutazione finora
- Get A Girl You LikeDocumento9 pagineGet A Girl You LikeKollin2150% (2)
- COURSE in The WARD Interhospital FinalDocumento8 pagineCOURSE in The WARD Interhospital Finalkimadlo656Nessuna valutazione finora
- Hipospadia Dan EpispadiaDocumento24 pagineHipospadia Dan EpispadiaAbdillah Fat-hiNessuna valutazione finora
- PrepositionsDocumento4 paginePrepositionsJelai M. BarreraNessuna valutazione finora
- Chaper 1 - PPT - CompleteDocumento49 pagineChaper 1 - PPT - CompleteUrjayatiNessuna valutazione finora
- Menstrual Cycle Biology ProjectDocumento4 pagineMenstrual Cycle Biology ProjectaddyNessuna valutazione finora
- ARH Action Plan 2019-2020Documento3 pagineARH Action Plan 2019-2020EM EM95% (19)
- Anovulation, Delayed Ovulation and Luteal InsufficiencyDocumento4 pagineAnovulation, Delayed Ovulation and Luteal InsufficiencySanjay C. Parmar0% (1)
- Who Preterm Birth 2018Documento5 pagineWho Preterm Birth 2018Santi Ayu LestariNessuna valutazione finora
- Deep ThroatingDocumento2 pagineDeep Throatingnathan100% (1)
- Fetal CirculationDocumento18 pagineFetal CirculationDr_ibk100% (1)
- The Y Chromosome Is DisappearingDocumento4 pagineThe Y Chromosome Is DisappearingJuan CarcaustoNessuna valutazione finora
- Revised IRR of RPRH Law of 2012Documento91 pagineRevised IRR of RPRH Law of 2012Mark Emann Baliza MagasNessuna valutazione finora
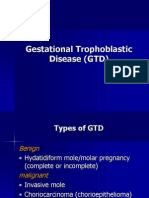
- Gestational Trophoblastic Diseases Hydatiform MoleDocumento40 pagineGestational Trophoblastic Diseases Hydatiform MoleL3SNessuna valutazione finora
- Maternity Nursing An Introductory Text 11th Edition Leifer Test BankDocumento9 pagineMaternity Nursing An Introductory Text 11th Edition Leifer Test BankSerenaNessuna valutazione finora
- Professor Dr. Gerd Ludwig, Professor Dr. Julian Frick (Auth.) - Spermatology - Atlas and Manual-Springer Berlin Heidelberg (1990)Documento169 pagineProfessor Dr. Gerd Ludwig, Professor Dr. Julian Frick (Auth.) - Spermatology - Atlas and Manual-Springer Berlin Heidelberg (1990)leandroNessuna valutazione finora
- Patologi KehamilanDocumento71 paginePatologi Kehamilanarie novardNessuna valutazione finora
- Benefits of Human CloningDocumento7 pagineBenefits of Human Cloningapi-385481351Nessuna valutazione finora
- 6th Grade Structure Processes and Responses To Plants 6bDocumento9 pagine6th Grade Structure Processes and Responses To Plants 6bapi-232424041Nessuna valutazione finora
- 12 6 05Documento15 pagine12 6 05Rachel Torres AlegadoNessuna valutazione finora
- MetodeDocumento17 pagineMetodeiuliaschiporNessuna valutazione finora
- Reproduction Concept MapDocumento1 paginaReproduction Concept Mapapi-392216729Nessuna valutazione finora
- Cleaning Your PenisDocumento11 pagineCleaning Your PenissearchhistorycollectionNessuna valutazione finora
- Jurnal Water Brith2Documento8 pagineJurnal Water Brith2salpa npNessuna valutazione finora