Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Sleep and Fatigue in Cancer Patient
Caricato da
SindhuNugrohoMuktiCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Sleep and Fatigue in Cancer Patient
Caricato da
SindhuNugrohoMuktiCopyright:
Formati disponibili
Other Medical Disorders
Charles F.P. George
123 Sleep and Fatigue in Cancer Patients
124 Fibromyalgia and Chronic Fatigue
125
Syndromes
Endocrine Disorders
126 Pain and Sleep
127 Gastrointestinal Disorders
128 Sleep in Chronic Kidney Disease
Sleep and Fatigue in Cancer Patients
Sonia Ancoli-Israel and Jose Savard
Abstract
Fatigue is a major complaint in patients with cancerbefore
treatment, while undergoing chemotherapy or radiation therapy,
and after the completion of therapy. The relation-ship, if any,
between fatigue and the quality or quantity of sleep or between
fatigue and the sleepwake circadian rhythm cycle is unknown.
One hypothesis is that some of the cancer-related fatigue may be
related to disturbed sleep or to dis-turbed sleepwake rhythms.
Different
dimensions
of
fatigue
(e.g.,
physical,
attentional/cognitive, emotional/affective) are likely to be
associated in some way with disrupted sleep and desynchronized
sleepwake rhythms. In cancer patients, as in other medically ill
patients, disturbed sleep may be important not only to the
expression of fatigue but to the patients quality
Patients with cancer complain of fatigue before treatment,
during chemotherapy or radiation therapy, and after the
completion of therapy.1 These patients also complain of
sleep disruption.2 Both fatigue and poor sleep probably
contribute to decreased quality of life. 3 There is a growing
body of literature on the relationship between fatigue and the
quality or quantity of sleep. This chapter will review the
evidence on cancer-related sleep disruption and fatigue and
their treatment, as well as the possible contribution of poor
sleep and desynchronized circadian rhythms to cancerrelated fatigue.
EPIDEMIOLOGY
Sleep Disruption
The prevalence of sleep complaints in cancer patients has
been studied primarily in cross-sectional studies using convenience samples with heterogeneous definitions and measures of sleep disturbances. In a large questionnaire study of
over 900 patients with different types of cancer, fatigue
(44%), leg restlessness (41%), insomnia (31%), and excessive sleepiness (28%) were the most prevalent complaints. 4
Another survey showed that 61% of the cancer patients had
significant sleep deficits, but there was no difference in sleep
complaints between the cancer patients and patients with
medical conditions other than cancer.5 Almost half of the
group had a poor sleep efficiency
1416
Section
15
Chapter
123
of life, to their tolerance to treatment, and to the development of
mood disorders, particularly clinical depression. Disrup-tions in
circadian rhythms themselves affect sleep quality and disrupt
many other physiologic mechanisms that pertain to fatigue.
Lack of entrainment to the daynight cycle and not keeping
regular hours can lead to feelings of grogginess, similar to the
feelings of jet lag. The degree of sleep disrup-tion found in
patients with cancer is not trivial. Objectively recorded sleep and
biological rhythms have not been well investigated in patients
with cancer, but because it appears that most may in fact not be
getting a good nights sleep, the goal of future research should
be to better characterize the sleep disruption and to find new
treatment approaches to improve sleep in this population.
(defined as the percentage of time spent asleep) below 85%.
Those patients receiving radiation or chemotherapy tended to
have more sleep disturbances than those not receiving
treatment. In addition, sleep problems predicted deficits in
quality of life.
Prevalence rates of insomnia symptoms have ranged from
30% to 50%.6,7 Only two studies have attempted to
distinguish between having subclinical and clinical levels of
insomnia in cancer patients. These studies found preva-lence
rates of insomnia symptoms of 48% in breast cancer
survivors and 32% in prostate cancer survivors. 8,9 With
insomnia syndrome defined as sleep-onset latency or wake
after sleep onset greater than 30 minutes, at least 3 nights per
week, associated with a sleep efficiency lower than 85% and
significant daytime impairments or marked distress, the
prevalences were 19% and 18%, respectively.8,9 In 95% of
the cases, the insomnia syndrome was chronic (i.e., duration
6 months).
Not much is known about how sleep disturbances vary as
a function of cancer sites. In one study, the prevalence of
sleep disturbances was greater in breast cancer patients,4 but
in another study the prevalence was greater in ovarian cancer
patients.10 Moreover, as most studies have been conducted
several months or even years after patients com-pleted their
cancer treatment, the extent to which insom-nia symptoms
are exacerbated by cancer treatments is unclear.
CHAPTER 123 Sleep and Fatigue in Cancer Patients 1417
Large-scale epidemiologic and longitudinal studies are
needed to better depict sleep difficulties in cancer patients,
characterize the natural course of sleep disturbances
throughout cancer care in terms of incidence and remis-sion,
and enable comparison across cancer sites and other cancer
characteristics. One ongoing longitudinal study conducted
among 998 patients with mixed cancer sites has found that
the overall prevalence rates of the insomnia syndrome and of
insomnia symptoms (including those with an insomnia
syndrome) at baseline (T1i.e., before or right after the
surgery) were 27.2% and 56.4%, and they decreased to
21.3% and 39.5% 2 months later (T2), respectively. 11 The
prevalence rates of insomnia symptoms were highest in
patients with breast cancer and gyneco-logic cancer and
lowest in patients treated for prostate cancer. The incidence
of insomnia from T1 to T2 was 19%, and the remission rate
was 32.0%. Together, these data indicate that insomnia is
already prevalent at the time of cancer diagnosis and surgery.
Future analyses will deter-mine the course of insomnia
symptoms as adjuvant treat-ments (e.g., chemotherapy,
radiation therapy, hormone therapy) are introduced.
Sleep disturbances are also very common in patients with
advanced cancer. In a study of patients with metastatic breast
cancer, 63% reported sleeping difficulties. Diffi-culty falling
asleep was associated with both depression and pain,
whereas increased awakening during the night was
associated just with depression.12 In another study of 100
palliative care patients attending a pain and symptom control
clinic, 72% reported sleep disturbances (63% reported
difficulty staying asleep; 40% reported difficulty falling
asleep).13 Difficulty falling asleep was mostly associ-ated
with fatigue and anxiety, whereas early awakening was more
strongly associated with fatigue. In a prospective study,
25.9% of terminally ill cancer patients reported sleep
disturbances at admission to a palliative care unit. 14 Another
study found that patients with advanced lung cancer reported
poorer sleep and more daytime sleepiness than healthy
controls, and that sleep disturbances of lung cancer patients
were characterized by breathing difficul-ties, cough,
nocturia, and frequent awakenings, all of which may be
suggestive of sleep-disordered breathing.15 Finally, a study
suggested that poor sleep quality and use of sleep
medications were, along with hopelessness and depression,
the best predictors of desire for hastened death in 102
terminally ill patients attending a palliative care unit, 16 thus
emphasizing the importance of offering appropriate sleep
management to these patients.
A few objective studies of cancer patients, using either
polysomnography or actigraphy, have been conducted to
characterize the sleep disturbances. When the sleep of
patients with breast or lung cancer, patients with insomnia,
and volunteers with no sleep problems were compared, the
insomnia patients had the shortest total sleep time on polysomnography, but the lung cancer patients had the longest
sleep onset latency, the lowest sleep efficiency, and the
greatest wake time during the night.17 There were no differences in stress levels or emotional state between the
cancer patients and the volunteers. There also was no difference in reported total sleep time between the cancer
patients and the volunteers. Interestingly, unlike the
insomnia patients, the cancer patients did not underesti-
mate total sleep time or overestimate wake time during the
night.
In the same study, although there was no difference in the
amount of sleep-disordered breathing, the cancer patients
had a higher prevalence of periodic limb move-ments in
sleep (PLMS) than insomnia patients or healthy volunteers. 17
However, more recently, in two small-scale studies (17 and
33 patients), an elevated prevalence of obstructive sleep
apnea (OSA), ranging from 12% to 91.7%, was found in
patients with head and neck cancer.18 Prospective studies are
warranted to investigate to what extent OSA is caused by the
cancer itself or by the cancer treatment. Sleep-disordered
breathing also appears to be frequent in patients with brain
tumors, with tumor removal resulting in a significant
decrease in the apneahypopnea index.19 An ongoing
research study indicates that the prev-alence of OSA in
women with breast cancer who have completed
chemotherapy was 48%, and the prevalence of PLMS was
36%.20 These high prevalence rates of PLMS and OSA may
help explain some of the sleep disturbance found in this
population.
Actigraphy, a noninvasive, continuous, ambulatory
measure of circadian restactivity rhythms, has also been
used to characterize the sleep and rhythms of patients with
cancer.21-24 Studies comparing cancer patients to healthy
controls have consistently shown less contrast between
daytime and nighttime activity in cancer patients, a pattern
indicative of circadian disruption. 21,25 In a study of 85
women with breast cancer, 72-hour actigraphy before the
start of chemotherapy demonstrated a mean total sleep time
of 6 hours, with only 76% of the night spent asleep. On
average, the women napped for about 1 hour a day. 23
Fatigue
Fatigue is one of the most frequent and disturbing complaints of patients with cancer3,26: more than 75% of patients
who undergo chemotherapy or radiation therapy report
feeling weak and tired. Cancer-related fatigue has been
defined as a persistent, subjective sense of tiredness related
to cancer and cancer treatment that interferes with usual
functioning.27 It is believed to be distinct from general
fatigue, as it is unrelated to exertion level and is not relieved
by rest or sleep. It has been reported that 76% of patients
receiving chemotherapy report fatigue at least a few days
each month,28 interfering with daily life, reduc-ing quality of
life,3,29 and being one of the key reasons for discontinuing
treatment.
An increasing number of studies in the past few years
have followed cancer patients over time. Overall, these
studies suggest that fatigue is highly prevalent before as well
as during and after treatment.26,29 In one study, 66% of the
women reported at least some fatigue before treat-ment and
84% reported fatigue during treatment. 23 Addi-tionally, the
percentage of women reporting extreme fatigue doubled
from approximately 5% before treatment, to approximately
10% during treatment. Several studies have suggested that
fatigue can continue for months, and even years, after the
completion of therapy. A recent sys-tematic review of the
literature identified 10 longitudinal studies on cancer-related
fatigue and concluded that can-cer-related fatigue may
persist for up to 5 years after com-pletion of adjuvant
treatments.30
1418 PARTII / Section 15 Other Medical Disorders
PATHOGENESIS
Pathogenesis of Sleep Disruption
Patients with cancer may complain of insomnia, hypersomnia, or both, but the pathogenesis of this sleep disruption can be quite varied. Chemotherapy, radiation therapy,
and hormone therapy may all contribute to the problem, but
studies looking at their different effects on sleep pat-terns are
lacking. In addition, commonly administered analgesics such
as opioids, and antiemetic medications such as
corticosteroids, are also known to disrupt sleep. 31 The
estrogen deficiency induced by chemotherapy and hormone
therapy, the abrupt cessation of hormone replace-ment
therapy at cancer diagnosis, or an ovary removal may each
trigger or exacerbate preexisting hot flashes. A study using
objective measurements of both sleep and hot flashes in
breast cancer survivors showed that nocturnal hot flashes
were associated with more wake time and more stage
changes to lighter sleep.32
The amount of insomnia in cancer patients can be as high
as the amount found in depressed patients, so clini-cians
should not overlook the possibility that poor sleep in cancer
patients may indicate some psychological distress. However,
there is evidence that, although insomnia and psychological
distress are interrelated, there are still a sig-nificant
proportion of patients who have only insomnia. In one
sample of newly diagnosed breast cancer patients, insomnia
was the most frequent symptom, reported by 88% of the
patients, and was correlated with high levels of distress and
anxiety.33 However, contrary to the belief that disturbed
sleep before treatment is attributable to the increased stress
and anxiety resulting from a recent diag-nosis of a lifethreatening illness, insomnia and fatigue were rated high
even in those patients who rated them-selves low on anxiety.
Similarly, another study revealed that 46% of prostate cancer
survivors with an insomnia syndrome did not have clinical
levels of anxiety or depres-sive symptoms.9
Pain has often been thought to be the cause of sleep
disruption, not only in patients with cancer but also in
patients with a multitude of other medical conditions. 2 It is
not yet known whether the pain contributes to poor sleep or
whether the pain medications contribute to poor sleep, or
both. One hypothesis is that pain may be the initial cause of
the frequent awakenings, but psychological distress prevents
the patient from falling back to sleep.34 A second hypothesis
is that while sleep leads to recovery and repair of tissue and
may offer a temporary cessation of the psychological
awareness of pain, poor sleep leads to difficulty managing
pain.35 In this way, a cycle of pain and poor sleep may
become self-perpetuating. In a study examining the
relationship between pain and sleep disrup-tion, patients with
breast cancer, lung cancer, insomnia (with no cancer) and
normal controls were questioned. Although those with breast
cancer reported pain before bedtime, neither their poor sleep
nor that of the patients with lung cancer was associated with
reports of pain.17 Another study conducted in patients with
advanced cancer showed significant correlations between
pain and poor sleep quality.36 Moreover, those patients with
poor quality of life had the most disturbed sleep and the
highest levels of pain.
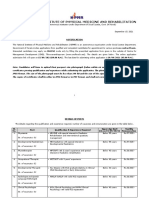
Physiological factors
e.g., pain
anemia
Psychological factors
e.g., depression
anxiety
Fatigue
Social/cultural factors
e.g., education
socioeconomic status
Chronobiological factors
e.g., sleep
circadian rhythms
Figure 123-1 Diagrammatic representation of possible factors
affecting fatigue. (Reprinted with permission from Ancoli-Israel S,
Moore P, Jones V. The relationship between fatigue and sleep in
cancer patients: a review. Eur J Cancer Care 2001;10[4]:245-255.)
Pathogenesis of Fatigue
Fatigue is believed to be caused by multiple factors, including physical (e.g., cachexia, weight loss, and biochemical,
hematologic, and endocrine abnormalities) and psychological (e.g., depression) and social factors (Fig. 123-1).
Anemia and other biochemical abnormalities are found in
cancer patients and cause fatigue, although hemoglobin
levels are only moderately related to fatigue and quality of
life. One study examining the incremental effect of increasing hemoglobin on quality of life found that improving the
anemia improved quality of life only to a point, beyond
which there was no further improvement. 37 Alternative
possible physiologic mechanisms include inflammation (e.g.,
increased proinflammatory cytokines), serotonin dysregulation, hypothalamic-pituitary-adrenal axis dysfunc-tion
(e.g., altered cortisol response), and altered muscle
metabolism.38 Among these potential mechanisms, inflammation is probably the one currently receiving the most
attention and is believed to be a common pathway through
which cancer and its treatment would lead to a variety of
behavioral consequences, including improved fatigue and
decreased sleep disturbances.38
Several studies have found significant relationships
between reports of fatigue and depression,26 but it is unclear
to what extent these are etiologically related. Indeed,
depression is far less common than fatigue in cancer patients,
which suggests that fatigue often occurs independently.
Moreover, it has been shown that cancer-related fatigue is
different from fatigue experienced by patients with
depression.
In addition, there is evidence that sleep disturbance is a
significant predictor of fatigue.39 Studies on symptom clusters have revealed that sleep and fatigue are often part of a
cluster of three or more symptoms. 40 Moreover, most crosssectional and prospective studies found a strong correlation
between self-reported sleep complaints and fatigue.
Evidence on the relationship between circadian rhythms
and subjective ratings of fatigue have been mixed, with most
studies finding a significant relationship. 24,41 Daytime
inactivity and nighttime restlessness were associated with
higher subjective ratings of cancer-related fatigue in one
CHAPTER 123 Sleep and Fatigue in Cancer Patients 1419
series of studies.41 Women with breast cancer who were
undergoing adjuvant chemotherapy reported more fatigue
during treatment, and less fatigue at chemotherapy cycle
midpoints, in a roller coaster pattern. Activity levels were
negatively correlated with reports of fatigue (i.e., those with
more fatigue showed less activity). Activity levels were
reduced during the three treatment sessions compared with
the cycle midpoints, thus showing the reverse roller-coaster
pattern, with inversely changing fatigue scores. Patients
tended to have more nighttime restlessness at treatment times
compared with cycle midpoints when higher activity during
the day prevailed and there were fewer nighttime
awakenings.41,42 Others24 found that self-reported fatigue
was significantly associated with an actigraphy measure of
sleepwake pattern stability (i.e., similarity versus
dissimilarity of rest and activity patterns across time, a
surrogate measure of circadian rhythm), but not with total
sleep time. Moreover, changes in fatigue from the second to
the fourth on-study chemotherapy cycles were significantly
associated with changes in the consistency of the sleepwake
pattern. On the other hand, a study of breast cancer patients
before chemotherapy23 found no significant relationship
between any of the rhythm variables or objective sleep
variables assessed using a 72-hour actigraphy recording, and
subjective reports of fatigue. Another study conducted in
breast cancer patients before chemotherapy found that most
actigraphy measures of sleepwake, activityrest, and
circadian rhythms derived from a 48-hour recording were not
significantly associated with fatigue. 22 Together, these
studies suggest that fatigue becomes a significant correlate of
circadian rhythms only after chemotherapy has been initiated
in breast cancer patients. However, longitudinal studies are
needed to verify the extent to which the relationship between
circa-dian rhythms and fatigue varies as a function of cancer
treatments. Overall, it seems clear that more research is
needed to understand the pathogenesis of cancer-related
fatigue.
TREATMENT
The complaints of sleep disturbances and fatigue in patients
with cancer are often overlooked in clinical practice and,
when a treatment is initiated, it is often a pharmacologic one
(e.g., sedative-hypnotics for insomnia, psychostimu-lants for
fatigue). While pharmacologic therapy may be appropriate at
times, there is accumulating evidence sup-porting the
efficacy of alternative treatments including psychological
treatments, activity-based interventions, and bright-light
therapy.
Sleep
PHARMACOTHERAPY
Hypnotic medications, particularly benzodiazepines, are by
far the most commonly prescribed treatment for sleep
disturbances in cancer patients.7 In 2005, the National
Institutes of Health (NIH) State of the Science Confer-ence
on Insomnia concluded that the newer, shorter acting
nonbenzodiazepines were safer and more effective than the
older, longer-acting benzodiazepines for the treatment of
insomnia.43 More recently, newer agents, such as a melatonin receptor agonist, have also been approved by the
U.S. Food and Drug Administration for the treatment of
insomnia. Although the efficacy of such medications is well
established for primary insomnia, its usefulness has yet to be
investigated in patients with comorbid cancer and insomnia.
BEHAVIORAL THERAPY
The NIH State-of-the-Science Conference on Insomnia also
concluded that cognitive-behavioral therapy (CBT) is the
most effective treatment for primary insomnia. 43 There is
now also accumulating evidence supporting its efficacy for
insomnia in cancer survivors.44,45 Overall, these studies have
been quite consistent in demonstrating that CBT (combining
stimulus control, sleep restriction, cognitive restructuring,
and sleep hygiene) results in increased sleep efficiency and
reduced total wake time, decreased psycho-logical distress,
and improved general quality of life. One study also showed
changes in immune functioning46 associ-ated with CBT for
insomnia, but the clinical relevance of these changes in terms
of cancer prognosis or other health outcomes is unknown.
Although replication is needed, it appears that the effects of
CBT in improving sleep would be mediated by both
nonspecific (i.e., treatment expectan-cies) and specific (i.e.,
reduced maladaptive sleep habits and dysfunctional beliefs)
factors.47
Some evidence from uncontrolled studies suggests that
mindfulness-based stress reduction interventions in cancer
patients result in improved daily sleep quality. 48 However, as
none of these studies selected patients on the basis of a
minimal insomnia severity, it is unclear whether this intervention is potent enough to treat syndromal or chronic
insomnia.
Fatigue
Numerous medications have been investigated for the
treatment of cancer-related fatigue, including hematopoietics (e.g., epoetin alfa, darbepoetin alfa), psychostimulants
(methylphenidate), antidepressants (e.g., bupropion, paroxetine), corticosteroids (e.g., methylprednisolone, prednisone), L-carnitine, and modafinil. A recent literature
review concluded that hematopoietics are effective in
reducing fatigue in patients with anemia.49 Promising results
have been obtained in open-label prospective studies
investigating the efficacy of other medication classes, in
particular psychostimulants and modafinil. However, data
from placebo-controlled trials, which would allow
counterbalancing beneficial and adverse effects, are
warranted, as many of these drugs have significant side
effects.49
Several nonpharmacologic interventions for fatigue have
been assessed in cancer patients. A recent review of the
literature identified a total of 41 publications, 24 assess-ing
the efficacy of various psychological interventions (e.g.,
cognitive-behavioral therapy) and 17 reporting on the efficacy of activity-based interventions.50 Overall, the effect size
obtained was of a small magnitude across all types of
intervention and outcome measures (e.g., fatigue, vigor).
When types of intervention were compared, a greater effect
size was found for psychological interventions than for
activity-based interventions. It is noteworthy, however, that
none of these studies used heightened levels of fatigue as an
inclusion criterion, thus limiting the power to detect
1420 PARTII / Section 15 Other Medical Disorders
intervention effects. Moreover, no study has yet investi-gated
the potentially superior effect of an approach com-bining
psychological and exercise-based interventions.
Not much is known about the possible mechanisms of
nonpharmacologic interventions for cancer-related fatigue.
Biological, environmental, behavioral, and cognitive factors
are all potential candidates.50 For example, an exer-cise
program may be beneficial for a variety of reasons, including
the resynchronization of the restactivity rhythms. A second
benefit of outdoor exercises would be the increased exposure
to bright light, which may promote greater daytime alertness.
Patients who report more fatigue tend to be exposed to less
light. 51 Although the causality of fatigue and light exposure
in breast cancer patients is not confirmed, there may be a
negative feedback loop such that less light exposure
desynchronizes patients circadian rhythms, which then
causes or deteriorates to fatigue, and fatigue further leads to
less light exposure.51
DIFFERENTIAL DIAGNOSIS: IS IT
SLEEPINESS, FATIGUE, OR
SOMETHING ELSE?
The clinician needs to determine the cause of a patients
symptoms, recognizing that the words used by the patient to
describe the symptoms may be vague. Is the symptom
related to sleepiness (the patient may describe unintended
episodes of falling asleep in the daytime or have an elevated
Epworth Sleepiness Scale score), or to fatigue (complaints of
muscular weakness, or lack of energy but not weakness)?
Patients may also have symptoms attributable to specific
effects of cancer or its treatment. When the patient has
complaints in one or more of these realms, they may become
very difficult to manage.
Sleepiness or Insomnia
When daytime sleepiness can be attributed to a specific sleep
disorder, treatment should target that sleep disorder. If a
patient has restless legs syndrome, the clinician should make
sure that the patient does not have iron deficiency, which
commonly occurs in patients with gastrointestinal
carcinomas. If the patient has developed movement disorders secondary to a chemotherapeutic agent, then a trial of a
dopaminergic agent should be initiated. If a patient has
developed obstructive sleep apneafor example, sec-ondary
to enlarged lymph nodes in the pharynx, as might occur with
lymphoma or with nasopharyngeal carcinoma then
continuous positive airway pressure treatment as well as
specific treatment directed at these areas should be initi-ated.
If the patient has developed clinical depression along with
insomnia, then concurrent therapy for the mood dis-order as
well as for the insomnia should be initiated.
Fatigue
As described earlier, fatigue, weakness, and loss of energy
are all hallmarks of cancer. Although the pathophysiology is
still poorly understood, the clinician should try to deter-mine
if the fatigue is caused in part by a correctable factor such as
electrolyte imbalance (this might occur in a patient on
chemotherapy with severe nausea or vomiting), an
underlying infection, or an undiagnosed metabolic disor-der
such as thyroid disease or diabetes mellitus. The latter
may develop as a result of some types of therapy, such as
large doses of corticosteroids. The fatigue might also be
exacerbated by poor sleep, in which case treating the
insomnia might result in improvements in the fatigue.
Direct Effect of Cancer
If the cancer is causing pain that is disturbing sleep, the pain
needs to be treated concurrently with the insomnia.
Hypoxemia caused by spread of cancer to the lung, or the
development of lung fibrosis in response to chemotherapy or
radiation therapy, may require treatment, as patients with
hypoxemia are known to have disturbed sleep.
PITFALLS AND CONTROVERSIES
Although the numbers of research studies in the past few
years have increased, there is still much that remains
unknown about the cause, consequences, and cures of
sleeping difficulties and fatigue in patients with cancer. In
particular, more longitudinal studies are needed to characterize the natural course of sleep complaints, circadian
rhythms impairments, and fatigue during the cancer trajectory, and to better understand how these disturbances are
interrelated. Areas for future research also include a better
characterization of those disorders across cancer sites. More
research is also warranted on patients with advanced cancer,
including clinical studies investigating the efficacy of
nonpharmacologic interventions for sleep disturbances and
fatigue, as it is unclear whether the same treatment
modalities can be offered to these patients. Finally, mechanisms through which these interventions are effective also
deserve investigation.
Fatigue and sleep disturbances are among the most
common and most distressing complaints of patients
with cancer. When left untreated, these symptoms can
significantly impair patients quality of life. Clini-cians
should screen more routinely for these distur-bances
and administer evidence-based treatment strategies to
help patients coping with them.
Acknowledgements
Supported by: NCI CA112035, NIA AG08415, Moores
UCSD Cancer Center, the Research Service of the Veter-ans
Affairs San Diego Healthcare System, the Canadian
Institutes of Health Research, the Canadian Breast Cancer
Research Alliance, and the Fonds de la recherche en sant
du Qubec.
This chapter is dedicated to the memory of Dr. J.
Christian Gillin, dear friend and colleague, who died of
cancer. He was fatigued but he never let it get to him. He
was an inspiration and a role model to us all.
REFERENCES
1. Zee PC, Ancoli-Israel S. Workshop Participants. Does effective management of sleep disorders reduce cancer-related fatigue? Drugs
2009;69(Suppl 2):29-41.
2. Fleming L, Gillespie S, Espie CA. The development and impact of
insomnia on cancer survivors: a qualitative analysis. Psychooncology In
Press 2010.
CHAPTER 123 Sleep and Fatigue in Cancer Patients 1421
3. Enderlin CA, Coleman EA, Cole C, et al. Sleep across chemotherapy
treatment: a growing concern for women older than 50 with breast
cancer. Oncol Nurs Forum 2010;37:461-A3.
4. Davidson JR, MacLean AW, Brundage MD, et al. Sleep disturbance in
cancer patients. Soc Sci Med 2002;54:1309-1321.
5. Fortner BV, Stepanski EJ, Wang SC, et al. Sleep and quality of life in
breast cancer patients. J Pain Symptom Manage 2002;24:471-480.
6. Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with
breast cancer. Sleep Med Rev 2006;10:419-429.
7. Savard J, Morin CM. Insomnia in the context of cancer: a review of a
neglected problem. J Clin Oncol 2001;19:895-908.
8. Savard J, Simard S, Blanchet J, et al. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer.
Sleep 2001;24:583-590.
9. Savard J, Simard S, Hervouet S, et al. Insomnia in men treated with
radical prostatectomy for prostate cancer. Psychooncology 2004;30:
474-484.
10. Portenoy RK, Thaler HT, Kornblith AB, et al. Symptom prevalence,
characteristics and distress in a cancer population. Qual Life Res
1994;3:183-189.
11. Savard J, Villa J, Ivers H, et al. Natural course of cancer-related
insomnia over a 2-month period. Proceedings of the American Psychosocial Oncology Society, Irvine, Calif, Feb 28-March 2, 2008.
12. Koopman C, Nouriani B, Erickson V, et al. Sleep disturbances in
women with metastatic breast cancer. Breast J 2002;8:362-370.
13. Sela RA, Watanabe S, Nekolaichuk CL. Sleep disturbances in palliative cancer patients attending a pain and symptom control clinic. Palliat
Support Care 2005;3:23-31.
14. Akechi T, Okuyama T, Akizuki N, et al. Associated and predictive
factors of sleep disturbance in advanced cancer patients. Psychooncology 2007;16:888-894.
15. Vena C, Parker K, Allen R, et al. Sleep-wake disturbances and quality
of life in patients with advanced lung cancer. Oncol Nurs Forum
2006;33:761-769.
16. Mystakidou K, Parpa E, Tsilika E, et al. The relationship of subjec-tive
sleep quality, pain, and quality of life in advanced cancer patients. Sleep
2007;30:737-742.
17. Silberfarb PM, Hauri PJ, Oxman TE, et al. Assessment of sleep in
patients with lung cancer and breast cancer. J Clin Oncol 1993; 11:9971004.
18. Nesse W, Hoekema A, Stegenga B, et al. Prevalence of obstructive
sleep apnoea following head and neck cancer treatment: a crosssectional study. Oral Oncol 2006;42:108-114.
19. Pollak L, Shpirer I, Rabey JM, et al. Polysomnography in patients with
intracranial tumors before and after operation. Acta Neurol Scand
2004;109:56-60.
20. Cornejo M, Liu L, Trofimenko V, et al. Obstructive sleep apnea in
breast cancer patients. Sleep 2008;31:A302.
21. Mormont MC, De Prins J, Levi F. Assessment of activity rhythms by
wrist actigraphy: preliminary results in 30 patients with colorectal
cancer. Bio Rhythm Res 1995;6:423.
22. Berger AM, Sankaranarayanan J, Watanabe-Galloway S. Current
methodological approaches to the study of sleep disturbances and
quality of life in adults with cancer: a systematic review. Psychooncology 2007;16:401-420.
23. Ancoli-Israel S, Liu L, Marler M, et al. Fatigue, sleep and circadian
rhythms prior to chemotherapy for breast cancer. Support Care Cancer
2006;14:201-209.
24. Roscoe JA, Morrow GR, Hickok JT, et al. Temporal interrelation-ships
among fatigue, circadian rhythm and depression in breast cancer
patients undergoing chemotherapy treatment. Support Care Cancer
2002;10:329-336.
25. Pati AK, Parganiha A, Kar A, et al. Alterations of the characteristics of
the circadian rest-activity rhythm of cancer in-patients. Chrono-biol Int
2007;24:1179-1197.
26. Ryan JL, Carroll JK, Ryan EP, et al. Mechanisms of cancer-related
fatigue. Oncologist 2007;12(Suppl 1):22-34.
27. Mock V, Atkinson A, Barsevick A, et al. NCCN practice guidelines for
cancer-related fatigue. Oncology (Williston Park) 2000;14: 151-161.
28. Curt GA, Breitbart W, Cella D, et al. Impact of cancer-related fatigue
on the lives of patients: new findings from the Fatigue Coalition.
Oncologist 2000;5:353-360.
29. Visser MRM, Smets EMA. Fatigue, depression and quality of life in
cancer patients: how are they related? Support Care Cancer 1998;6:101108.
30. Minton O, Stone P. How common is fatigue in disease-free breast
cancer survivors? A systematic review of the literature. Breast Cancer
Res Treat 2007;112:5-13.
31. Moore P, Dimsdale JE. Opioids, sleep, and cancer-related fatigue. Med
Hypotheses 2002;58:77-82.
32. Savard J, Davidson JR, Ivers H, et al. The association between nocturnal hot flashes and sleep in breast cancer survivors. J Pain Symptom
Manage 2004;27:513-522.
33. Cimprich B. Pretreatment symptom distress in women newly diagnosed with breast cancer. Cancer Nurs 1999;22:185-194.
34. Engstrom CA, Strohl RA, Rose L, et al. Sleep alterations in cancer
patients. Cancer Nurs 1999;22:143-148.
35. Lewin DS, Dahl RE. Importance of sleep in the management of
pediatric pain. J Dev Behav Pediatr 1999;20:244-252.
36. Mystakidou K, Parpa E, Tsilika E, et al. Depression, hopelessness, and
sleep in cancer patients desire for death. Int J Psychiatry Med
2007;37:201-211.
37. Crawford J, Cella D, Cleeland CS, et al. Relationship between changes
in hemoglobin level and quality of life during chemotherapy in anemic
cancer patients receiving epoetin alfa therapy. Cancer 2002;95:888-895.
38. Miller AH, Ancoli-Israel S, Bower JE, et al. Neuroendocrine-immune
mechanisms of behavioral comorbidities in patients with cancer. J Clin
Oncol 2008;26:971-982.
39. Roscoe JA, Kaufman ME, Matteson-Rusby SE, et al. Cancer-related
fatigue and sleep disorders. Oncologist 2007;12(Suppl. 1):35-42.
40. Liu L, Fiorentino L, Natarajan L, et al. Pre-treatment symptom cluster
in breast cancer patients is associated with worse sleep, fatigue and
depression during chemotherapy. Psychooncology 2009;18(2): 187-194.
41. Berger AM, Farr L. The influence of daytime inactivity and night-time
restlessness on cancer-related fatigue. Oncol Nurs Forum
1999;26:1663-1671.
42. Berger AM. Patterns of fatigue and activity and rest during adju-vant
breast cancer chemotherapy. Oncol Nurs Forum 1998;25: 51-62.
43. National Institutes of Health State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults,
June 13-15, 2005. Sleep 2005;28:1049-1057.
44. Savard J, Simard S, Ivers H, et al. Randomized study on the efficacy of
cognitive-behavioral therapy for insomnia secondary to breast cancer,
part I: sleep and psychological effects. J Clin Oncol 2005; 23:60836096.
45. Espie CA, Fleming L, Cassidy J, et al. Randomized controlled clinical
effectiveness trial of cognitive behavior therapy compared with treatment as usual for persistent insomnia in patients with cancer. J Clin
Oncol 2008;26:4651-4658.
46. Savard J, Simard S, Ivers H, et al. Randomized study on the efficacy of
cognitive-behavioral therapy for insomnia secondary to breast cancer,
part II: immunologic effects. J Clin Oncol 2005;23:6097-6106.
47. Tremblay V, Savard J, Ivers H. Predictors of the effect of cognitivebehavioral therapy for chronic insomnia comorbid with breast cancer. J
Consult Clin Psychol 2009;77(4):742-750.
48. Carlson LE, Garland SN. Impact of mindfulness-based stress reduc-tion
(MBSR) on sleep, mood, stress and fatigue symptoms in cancer
outpatients. Int J Behav Med 2005;12:278-285.
49. Carroll JK, Kohli S, Mustian KM, et al. Pharmacologic treatment of
cancer-related fatigue. Oncologist 2007;12:43-51.
50. Jacobsen PB, Donovan KA, Vadaparampil ST, et al. Systematic review
and meta-analysis of psychological and activity-based interventions for
cancer-related fatigue. Health Psychol 2007;26:660-667.
51. Liu L, Marler M, Parker BA, et al. The relationship between fatigue and
light exposure during chemotherapy. Support Care Cancer
2005;13:1010-1017.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Shostakovich: Symphony No. 13Documento16 pagineShostakovich: Symphony No. 13Bol DigNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Vocabulary Ladders - Grade 3 - Degree of FamiliarityDocumento6 pagineVocabulary Ladders - Grade 3 - Degree of FamiliarityfairfurNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Faust Part Two - Johann Wolfgang Von GoetheDocumento401 pagineFaust Part Two - Johann Wolfgang Von GoetherharsianiNessuna valutazione finora
- 10 Chapter 3Documento29 pagine10 Chapter 3felefel100% (1)
- Group Process in The Philippine SettingDocumento3 pagineGroup Process in The Philippine Settingthelark50% (2)
- BD9897FS Ic DetailsDocumento5 pagineBD9897FS Ic DetailsSundaram LakshmananNessuna valutazione finora
- Abstraction and Empathy - ReviewDocumento7 pagineAbstraction and Empathy - ReviewXXXXNessuna valutazione finora
- Histology Solution AvnDocumento11 pagineHistology Solution AvnDrdo rawNessuna valutazione finora
- Consumer Trend Canvas (CTC) Template 2022Documento1 paginaConsumer Trend Canvas (CTC) Template 2022Patricia DominguezNessuna valutazione finora
- Sta 305Documento156 pagineSta 305mumbi makangaNessuna valutazione finora
- Stephen Law Morality Without GodDocumento9 pagineStephen Law Morality Without GodJiReH MeCuaNessuna valutazione finora
- Building Brand ArchitectureDocumento3 pagineBuilding Brand ArchitectureNeazul Hasan100% (1)
- IPA Digital Media Owners Survey Autumn 2010Documento33 pagineIPA Digital Media Owners Survey Autumn 2010PaidContentUKNessuna valutazione finora
- Iyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)Documento298 pagineIyengar S., Leuschke G.J., Leykin A. - Twenty-Four Hours of Local Cohomology (2007)wojtekch100% (1)
- Mus Culo SkeletalDocumento447 pagineMus Culo SkeletalKristine NicoleNessuna valutazione finora
- Role LibrariesDocumento57 pagineRole LibrariesGiovanni AnggastaNessuna valutazione finora
- Diverse Narrative Structures in Contemporary Picturebooks: Opportunities For Children's Meaning-MakingDocumento11 pagineDiverse Narrative Structures in Contemporary Picturebooks: Opportunities For Children's Meaning-MakingBlanca HernándezNessuna valutazione finora
- Chapter 10: Third Party Non-Signatories in English Arbitration LawDocumento13 pagineChapter 10: Third Party Non-Signatories in English Arbitration LawBugMyNutsNessuna valutazione finora
- Read Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallDocumento1 paginaRead Chapter 4 Minicase: Fondren Publishing, Inc. From The Sales Force Management Textbook by Mark W. Johnston & Greg W. MarshallKJRNessuna valutazione finora
- Eapp Module 1Documento6 pagineEapp Module 1Benson CornejaNessuna valutazione finora
- Software Development Life CycleDocumento70 pagineSoftware Development Life CycleChaitanya MalikNessuna valutazione finora
- BEM - Mandatory CoursesDocumento4 pagineBEM - Mandatory CoursesmohdrashdansaadNessuna valutazione finora
- NIPMR Notification v3Documento3 pagineNIPMR Notification v3maneeshaNessuna valutazione finora
- Lesson Plan 2 Revised - Morgan LegrandDocumento19 pagineLesson Plan 2 Revised - Morgan Legrandapi-540805523Nessuna valutazione finora
- Disciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineDocumento12 pagineDisciplines, Intersections and The Future of Communication Research. Journal of Communication 58 603-614iplineErez CohenNessuna valutazione finora
- Deeg Palace Write-UpDocumento7 pagineDeeg Palace Write-UpMuhammed Sayyaf AcNessuna valutazione finora
- 160 LW Bending Tester v2.0Documento4 pagine160 LW Bending Tester v2.0Sá StrapassonNessuna valutazione finora
- Fabre, Intro To Unfinished Quest of Richard WrightDocumento9 pagineFabre, Intro To Unfinished Quest of Richard Wrightfive4booksNessuna valutazione finora
- Adventures in Parenting RevDocumento67 pagineAdventures in Parenting Revmakj_828049Nessuna valutazione finora