Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Newsletter - Rob S Vol 8 August 2015
Caricato da
api-323491985Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Newsletter - Rob S Vol 8 August 2015
Caricato da
api-323491985Copyright:
Formati disponibili
Y
Professional PT
Clinical Corner
Issue 8
August 2015
Professional PT/Maitland Seminars:
Inside this issue:
Professional PT/
MAPS
Customer Service/
Quiz
Multifidus
Compliance
New York State Concussion Law
Shoulder article re-
Compaction Test
Case Study
Case Study
GEMS
10
Announcements:
Maitland seminars sponsored course coming
Sept 11-13 2015
Tim Hewitt ,Professional
PT sponsored ,seminar
coming in October
McKenzie series continues in November
Regional study groups to
start soon!
Professional Physical Therapy is proud to
partner with MAPS (Maitland Australian
Physiotherapy Seminars). The first seminar entitled MT-2 (spine) will be offered
on September 11-13, 2015. There are no
pre-requisites for this course.
approach is recognized worldwide as an
efficient, safe and gentle way to evaluate
and treat the orthopedic patient to alleviate pain, reduce inflammation, restore
movement, and maximize function.
The Maitland approach requires the development and continual refinement of
The Maitland-Australian Approach is high- clinical assessment skills and clinical
ly efficient and effective in the managejudgment by utilizing thorough, accurate
ment of neuromusculoskeletal conditions. assessment (both subjective and objecPioneered in the 1950s by the legendary tive), and the use of eight clinical hypothAustralian Physiotherapist Geoffrey Mait- esis categories, as described by reland, it has continued to evolve over the
nowned physiotherapists Mark Jones and
years with groundbreaking concepts such David Rivett. This dynamic thought proas Irritability, Neurodynamics, Combined cess of patient classification through hyMovements, Stabilization Training, and
pothesis formation and modification-Advanced Clinical Reasoning with supcommonly known as Clinical Reasoning-porting Evidence-Based Medicine reresults in a more knowledgeable treating
search. Geoff Maitland's #1 Core Princi- clinician. The improvement in clinical exple is, "Sublimation of self and a positive pertise and thought processes embedded
personal commitment to understand what in the Maitland concept and in the MAPS
the patient is enduring, and the effects
curriculum puts clinicians on a path of
the disorder has upon the patient." The
professional growth, personal excellence
Maitland approach has always been, and and, ultimately, vastly improved patient
continues to be, concerned with the pacare.
tient's needs above all. Few philosophies
of manual therapy can claim the same
Throughout MAPS seminars assessment
level of commitment to the patient's val- and treatment techniques are clearly
ues and well-being, as the Maitland Apdemonstrated to participants, who immeproach.
diately practice the techniques under the
watchful eye of the Instructor. The InThis approach is patient-centric, and restructor provides each participant with
spects the diagnosis with an understand- constructive feedback, including refineing of the pathology. Biomechanical
ments and modifications, to ensure the
knowledge is used when applicable.
technique has been properly understood
MAPS develops the Maitland Approach a
and applied by the participant.
step further, providing advanced training All of the principles, processes and techto qualified clinicians in the Maitlandniques come together and are reinforced
Australian Approach, which combines the when the Instructor performs an Evalualatest Evidence-Based research in Manual tion of a Real Patient, with Real PatholoTherapy/Physiotherapy with the Maitland gy, Live In Front Of The Class (where
Approach and associated evaluation and
permitted). This is truly "where the rubtreatment techniques. The Maitland Aus- ber meets the road." The clinical utility
tralian Approach intentionally gently pro- and real life clinical effectiveness of the
vokes the patient's actual symptoms usMaitland Approach becomes plainly obviing carefully graded osteokinematic
ous during these patient demonstrations.
(physiological) and arthrokinematic
(accessory) passive mobilization. This
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2014
Professional PT Clinical Corner
Page 2
Create Raving Fans with Exceptional Customer Service
David Skudin, Director of Customer Service
Patient Satisfaction is the term we often use when
we talk about Customer Service. In fact, our patient feedback is even called a Patient Satisfaction survey, but the truth is if our patients say
they are satisfied with the service we provide
then our service isnt good enough.
A satisfied customer isnt going to tell everyone
what a great experience they had with you and
Professional Physical Therapy. They wont make
sure they dont do business with any other physical therapy provider but you ever again.
treatment and may not quibble about a copayment but you can bet that they will be open to
trying another physical therapy practice next time.
So forget about merely satisfying customers because satisfying them wont help you or Professional succeed as the Provider of Choice in the
increasingly competitive physical therapy world.
To do that you need to provide an Exceptional Patient Experience and create Raving Fans, customers who are so devoted to you and our services that they wouldnt dream of taking their
business elsewhere and will sing from the rooftops
about just how great you are.
A satisfied patient may not complain about their
I hope you are enjoying your summer and find some time to catch up on
some well deserved rest. We are sponsoring some great seminars in the
next few months and hope you will take advantage of these great learning
experiences. A special welcome to Premiere Physical Therapy, we are excited to have you as part of Professional PT.
Enjoy and please feel free to send me feedback, it gets lonely behind the
key board. :)
Robert Shapiro
Random quiz questions
1. What muscle is the only muscle to lie on the posterior surface of the
sacrum?
2. What are the borders of the quadrangular space in the shoulder?
3. According to Mulligan what does the SNAGS stand for?
4. What ligament connects the odontoid process to the occiput?
5. What attaches to the adductor tubercle on the distal femur?
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
YPage 3
Professional PT Clinical Corner
Multifidus Muscle Function:
The lumbar multifidi are small but
important muscles. They lie on each
side of the spinous processes of the
lumbar vertebrae and fill the deep
space in the laminar groove. The
multifidi provide lumbar segmental
stability by orienting adjacent vertebrae to each other and due to its line
of action, posterior to the lumbar
curve, it extends the lumbar spine
and increases lumbar lordosis. As
the oblique muscles fire to rotate the
upper body, lumbar flexion would
have to occur if it were not for the
action of the multifidus, which prevents flexion from occurring. This
allows the spine to remain vertical
when pure rotation is desired.
Robert Shapiro MA PT COMT
Group one received medical treatment only consisting of advise on
minimal bed rest (1-3 days) and minor analgesics. Group two received
the same medical treatment plus
specific, localized exercise therapy.
Therapeutic exercises were aimed at
facilitating the activation of the multifidus muscle to perform its role in
local segmental stabilization. The
exercises involved isometric multifidus contraction with co-contraction
of the deep abdominal muscles.
Studies have shown that the multifidus muscles get activated before
any action is carried out so to protect our spine from injury. An example is when you are about to lift
an item or before moving your arm,
the multifidus muscles will start contracting prior to the actual movement of the body and the arm so as
to prepare the spine for the movement and prevent it from getting
hurt.
2. Prone: locate multifidi as above
and have the patient extend one
hip, the order of activation of
muscles should be: the ipsilateral hamstring first, followed by
the ipsilateral gluteus maximus
followed immediately by the opposite multifidus and then the
ipsilateral multifidus. Look/feel
for the correct firing patterns.
3. Standing: palpate segmental
lumbar multifidi as above and
have patient fully flex one shoulder, the opposite multifidus
should fire to control motion. If
this doesn't occur the patient
may have segmental inhibition
at that level. If you are unsure
if you feel muscle activation you
can have the patient lift a 3-5 lb
weight and activation (or not)
should be more obvious.
4. Standing: this tests the anti flexion function of the multifidus.
Have the patient maintain a norPain scores, disability test scores,
mal lumbar lordosis as they flex
ROM values and ultrasound imagines
forward at the hips (waiters
to assess asymmetry of multifidi
bow), look for any flexion momuscle size were obtained day 1,
ments in the lumbar segments, if
week 4 and week 10. This study
the patient cant control a specific
determined that lumbar multifidus
segment there is decreased mulJulie Hides et al conducted a study
muscle recovery in patients with
tifidus control at that level.
to determine if multifidus muscles
acute lower back pain did not occur
recover muscle function spontaneously following an acute lumbar inju- spontaneously once pain subsided.
5. Quadruped: same test as above
ry. Subjects were recruited from an Although patients in group 1
but in quadruped, have the paER department in a hospital during a (medical management only) retient attain a quadruped posisumed normal activities by week 10
6 month period. Patients in this
tion, while maintaining slight
study were between the ages of 18- they still exhibited decreased multifilumbar extension, have the padus muscle size. Patients in group 2
45 and had to be experiencing their
tient sit back towards their heels
first episode of unilateral mechanical experienced a more rapid and
while maintaining a normal lumlower back pain for less than 3
more complete recovery in multibar curve, if you see flexion ocweeks with symptoms located becurring at a specific segment
fidi function. This study highlights
tween T12 and the gluteal fold. Ex- the importance of specific muscle
the patient may have decreased
cluded from the study were patients strengthening program after a lumcontrol at that level.
with a history previous lower back
bar injury.
pain or surgery, spinal abnormalities
Hides, J., Richardson, C., & Jull, G.
as per x-ray, neurological signs, red Clinically, multifidus function can be (n.d.). Multifidus Muscle Recovery Is
Not Automatic After Resolution of
flags, evidence of any systematic
tested in a few different ways:
Acute, First-Episode Low Back
disease, pregnancy or involvement
Pain. Spine, 2763-2769.
in any sport or fitness training in1. palpation: with patient prone
volving the lower back musculature
the lumbar multifidi are located
performed in the past 3 months.
just medial to the spinous proForty one patients were accepted
into the study and were randomly
assigned into one of 2 groups.
cesses in the lumbar spine, normal tone can be assessed by
compressing one side and comparing tone to the opposite side.
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
YPage 4
Professional PT Clinical Corner
Compliance Corner:
Daniel Hirsch PT, DPT | Director of Internal Audit
In this August edition of the Compliance Corner, we would like to
discuss some work place concepts
and laws related to proper speech
in the clinic. All three stretch
goals in the ProPT Strategic Plan
directly relate to how we communicate with others. The future
success of each individual physical
therapist, staff member, clinic and
regional staff member are only
obtainable through proper dialog
over multiple mediums.
paper, orally or in any other form.
As the provider of choice, patients
must feel that we carefully protect
and care about their privacy. As a
health care provider, it is imperative that we ensure confidentiality
standards under HIPAA, as well as
make sure that all state laws are
met. ProPT has in place a HIPAA
Manual which sets forth confiden-
Mozart is quoted as saying: To
talk well and eloquently is a very
great art, but that an equally
great one is to know the right moment to stop. In order to make
our workplace more desirable we
should strive to keep conversations positive and constructive
and avoid conversations that are
negative and damaging. After all,
listening to negative conversations can be just as destructive as
speaking negatively.
Strategic Plan Stretch Goals:
The third goal of being the
Growth Strategist of Choice and
By 2017 PPT will be the Proexecuting an aggressive growth
vider of Choice for outpastrategy requires common sense
tient orthopedic rehabilitaand a healthy perspective of
tion in the tristate area.
growth. A non-disclosure agreement provides legal protection of
BY 2017 PPT will be the Eminformation generally unknown to
ployer of Choice and the
others and is used during contract
most desirable work place
negotiations, acquisitions and othin the outpatient orthopeer purchases. As our company
dic rehabilitation sector.
grows and expands, all company
By 2017 PPT will be the
individuals must uphold the reGrowth Strategist of
sponsibility of ensuring privileged
Choice and demonstrate
tiality standards. Specifically,
knowledge. If you have any
aggressive growth strategy page 4 & 5 of the HIPAA Manual
questions, concerns or comments
in the outpatient rehabilirelated to confidentiality; please
describe appropriate privacy
contact the Privacy Officer (Daniel
tation sector.
standards to help maintain this
important aspect of physical ther- Hirsch:
The first goal of being the
dhirsch@professionalpt.com ),
Provider of Choice is affected by apy services.
Security Officer (Domingo Lopez:
proper enforcement of HIPAA and The second stretch goal of bedlopez@professionalpt.com ) or
excellent customer service. The
ing the Employer of Choice and General Counsel (Janna King:
jking@professionalpt.com ).
protected health information
the most desirable work place in
(PHI) of each patient is defined our sector provides a segue for
Thank you for reading this inforunder HIPAA as health inforhow we discuss patient information. We expect each employee
mation which when matched with mation with others, to how we
to contribute to our companys
another piece of information, can communicate between ourselves
culture by influencing others in
lead to identification of the indias employees in this company.
vidual (for example: name, SSN, As the gold standard for excellent the clinic and always practicing
address, DOB, certificate numwithin the law and Gold Standard
customer service, David Skudin
ber). PHI is individually identifia- educates each employee on how
practices to help us reach our
ble information that is transmitted to respectfully and professionally goals!
or maintained electronically, on
speak to co-workers. Wolfgang
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Page 5
Issue 8
New York State Concussion Laws:
As we transition from our summer
clinical roles back into the outreach
settings, we need to read over the
NYS concussion Laws and the NATA
position statement on concussions,
here is a summary of the most recent
(2014) data.
http://www.p12.nysed.gov/sss/
schoolhealth/schoolhealthservices/
ConcussionManageGuidelines.pdf
*New York State School Health Services defines a concussion as a type
of traumatic brain injury (TBI), are
injuries to the brain that occur as the
result of a fall, motor vehicle accident, or any other activity that results in an impact to the head or
body.
Bridget Rodin ATC
*it should be determined, depending
on symptoms, whether the athlete
should be referred to the ER
*the severity of a concussion is based
on how long your symptoms last.
*being unconscious, a lose of
*the athlete must be seen by a physi- memory, headache, dizziness, etc.
cian, nurse practitioner or physician
are all considered symptoms of a
assistant as soon as possible
concussion, but do not determine the
severity
* the athlete cannot return to sport/
activity until cleared by a physician
When can you return to play after
a concussion?
Frequently Asked Questions
*once you are symptoms free for 48
Be prepared to answer these queshours and have completed a 5-day
return-to- play protocol
If my child sustains a concussion,
should I wake them every 2
hours at night?
*it is actually recommended to have
your child sleep as much as possible,
this aides in the healing process
As of January 2014 it is recommended that a district include the following
in their concussion management policy:
Should I take my child out of
school if they have sustained a
concussion?
*a list of preventative methods and
strategies.
*you may consider shortening their
school day or taking them out altogether depending on the severity of
their symptoms.
*a procedure and treatment plan for
responding to head injuries.
*a plan to ensure the appropriate
staff has taken the required NYSED
approved training course for concussions.
*a communication plan involving private providers and school staff.
*a procedure for a periodic review of
the concussion policy
In the event of a suspected concussion:
*the player should be removed from
play immediately and sent to either
the athletic trainer, school nurse or
other medical professional
tions when approached by a parent.
Who can diagnose a concussion?
*Physicians, Nurse Practitioners, Physician Assistants
How are concussions graded?
*there is no longer a grading scale for
concussions.
Signs of Headache of Cervical Origin:
Occipital or suboccipital component to headache
Abnormal head or neck posture
Abnormal mobility of C0-C1
Sensory abnormalities in occipital and/or sub occipital regions.
Neck movement alters headache.
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Professional PT Clinical Corner
Page 6
Prognosis in Individuals With Shoulder Pain Receiving Cervico-thoracic Manipulation: Review
by Robert Shapiro MA PT COMT
Mintken PE, Cleland JA, Carpenter
KJ, Bieniek ML Whitman JM. Identifying prognostic factors for successful short-term outcomes in
individuals with shoulder pain receiving cervico-thoracic manipulation. Phys Ther. 2009: In Press
red flags, acute fractures, acute
severe cervical or thoracic trauma
in the past 6 weeks, cervical stenosis of bilateral UE symptoms,
osteoporosis, prior cervical or thoracic surgeries, evidence of CNS
involvement, signs of nerve root
compression.
80 subjects participated in the
study with a mean age of 40.4
(59% of female and 41 % male).
Mintken et al developed a clinical
prediction rule to determine when
the application of cervico-thoracic
manipulation would be useful in
patients complaining of shoulder
pain.
The authors conducted a prospective single-arm trial of consecutive
individuals who met the inclusion
criteria. (A single arm prospective
study means everyone enrolled in
the clinical trial will be treated the
same way.) Nine therapist from 7
different facilities participated in
the examination and treatment
process.
Following a standardized examination participants where treated
with a series of 6 thrust and nonthrust manipulations directed at
the cervico-thoracic region. FolInclusion criteria for this study
lowing manual intervention each
were patients between the ages of patient was instructed to perform
18-65 who had a primary com2 different spinal mobility exercisplaint of shoulder pain and basees (3 finger ROM exercise and
line Shoulder Pain and Disability
thoracic flexion/extension supine
Index Score (SPADI) over 20.
over a bolster).
The Shoulder Pain and Disability
Patients were classified as having
Index (SPADI) was developed to
a successful or unsuccessful outmeasure current shoulder pain
come after the 2nd or 3rd session.
and disability in an outpatient setSuccess was defined as achieving
ting. The SPADI contains 13 items
a +4 (moderately better) on the
divided into two subscales: a 5GROC score. The Global Rating of
item subscale that measures pain
Change (GROC) is a 15 point
and an 8-item subscale that
score which has the patient rate
measures disability. The higher
the amount of perceived change
score the worse the disability.
in their condition. A score of +4
Exclusion criteria for this study
or greater indicates that the pawas: any patient who displayed
tient believes moderate changes
For internal use only. Not intended for external sharing or distribution.
have occurred with treatment.
The authors used a final regression model (a statistical process
for estimating the relationships
among variables.) to determine
five variables that were present in
those individuals who achieved a
successful outcome. The five
prognostic indicators used were:
pain free shoulder flexion less
than 127 degrees, shoulder IR
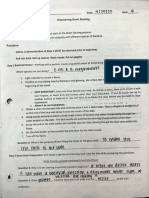
less then 53 degrees at 90 de# of Predictor Variables
Met
Met all 5
Probability of
success (%)
100
Met at least 4
100
Met at least 3
89
Met at least 2
78
Met at least 1
61
grees of abduction, negative Neer
test, not taking medications for
their shoulder pain and symptoms
for less than 90 days.
If 3 out 5 variables were present
the likelihood of a successful outcome went form 61% (with one
criteria met) to 89%.
The study identified prognostic
variables that will allow clinicians
to identify patients with shoulder
pain who would benefit from cervical/thoracic manipulation.
Some limitations of this the study
are: there was no control group,
# of treatments was not standardized, small sample size, and
since the data was collected for
short term outcomes we can not
know whether these patients did
well long term.
Professional Physical Therapy 2015
YPage 7
Professional PT Clinical Corner
Cervical Compaction Test:
We often see patients in the clinic
who complain of pain in the cervical
and lumbar regions at the same
time. It can be difficult to tell if one
region is driving the dysfunction
into the other region. For example,
are the patients cervical symptoms
being perpetuated by imbalances in
the lumbar and pelvic muscles.
The Cervical Compaction Test is
a great tool to help the therapist sort
out where the major dysfunctions
lie. As always, a thorough examination is necessary to rule out any red
flags and to determine the irritability
of the condition. Assuming there are
no red flags and the patients condition is not irritable this test can be
used to help guide treatment.
Robert Shapiro MA PT COMT
Results:
tient is now able to raise their legs
with greater ease the test is considIf the patient is able to lift both legs
ered positive and the cervical region
off the table without any difficulty it
is considered to be the primary dyscan be assumed that the lumbofunction. This tells us that once we
pelvic region is functioning normally.
give the cervical region stability the
lumbo-pelvic region can function
normally. The cervical region needs
to be corrected first.
If the patient has greater difficulty
lifting both legs of the table when
cervical compression is added then
the primary dysfunction is most likely in the lumbo-pelvic region. If this
is the case the lumbo-pelvic region
needs to be addressed first.
If the patient has difficulty or can
not lift their legs off the table there
Test: the patient is lying supine with
is a possibility that the lumbo-pelvic
both legs straight. The therapist sits
region is problematic and further
at the head of the table, holding the
testing is necessary.
patients head with a bilateral contact
The next step is to add cervical com(without applying a compressive or
pression while the patient attempts
distractive force initially). The patient attempts to lift both legs off the to raise both legs off the table at the
same time. Adding cervical comtable at the same time.
pression stabilizes the articular facets in the cervical spine. If the pa-
MedBridge Facts:
Professional Physical Therapy clinicians earned C.E.U's 1580 and completed 895 courses this year
through MedBridge.
Top 5 clinics in completed courses are :
1. West Side (48)
2. Queens (47)
3. Mamaroneck (39)
4. Garden City (39)
5. Rosyln (37)
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Page 8
Issue 8
Case study: Cervical/Shoulder/Elbow:
Robert Shapiro MA PT COMT
SUBJECTIVE
Patient Profile:
Findings
33 year male, grant administrator for a
local university, works at a computer 8
hrs/day, activities outside work include
biking, running, lifting weights and
swimming.
Therapist thoughts:
Pt has an active lifestyle, motivated, work environment needs to be explored
History of Present complaint:
Long history of right posterior shoulder
pain possibly due to lifting weights 8-10
years ago. Cervical and upper back
pain started 3 months ago after performing pull ups and bent over rows.
Pt started to notice right medial elbow
pain 3 weeks ago and is not sure of the
cause.
Cervical: pain right side of neck to right
upper trap and right medial scapula to
approximately T6, pain is described as
an intermittent ache.
Shoulder/arm: right AC joint
(intermittent, ache), posterior shoulder
and right medial elbow (intermittent,
deep and sore)
Acute injury on a chronic problem. Need to sort
out each area and determine their relationship
to each other.
Cervical:
1. sleeping on stomach with head
turned to the right/ eases once out
of position (OOP).
2. Biking for a few hours/eases once
out OOP.
My examination can be rigorous since the patients condition does to appear to be irritable. I
can use this information to gauge my patients
progress
Body chart:
Aggravating factors
Multiple areas of pain, I need to figure out the
relationships of these different pains during by
objective exam.
Shoulder:
1. sleeping on right side for 10 mins/
eases in a few minutes
2. Horizontal adduction/ eases immediately once OOP
3. Swimming any stroke, pain starts
at 10 mins/sore for 1-2 days after
swim
Easing factors
Elbow: grasping/lifting objects /eases
with stretching and meds
Cervical and shoulder : OOP
Elbow: stretching and meds.
Patients condition is not irritable and my exam
can be moderately aggressive.
Initial Hypothesis: Based on the subjective exam the patients symptoms appear to be not severe since he
is able to perform his normal activities. According to Maitland severity refers to the intensity of the patient's
symptoms and is based on the patient's perception of the symptoms and how much the symptoms
limit the patient's activities. The cervical and shoulder regions are non-irritable since pain goes away quickly
after activity, but the elbow pain may exhibit some irritability since it takes some meds and rest to ease. The
stage of the cervical and shoulder pain appears to be chronic but the elbow pain is sub acute (onset 3 weeks
ago with some irritability) . My hypothesis, after the subjective exam, is C6/7, C7/T1 joint dysfunction, with possible C7 disc, possible shoulder instability, AC joint irritation, with right ulnar nerve adverse neural tension.
Based on the subjective exam the focus of my objective exam will be to prove or disprove my hypothesis. My
examination can be rigorous due to the stage and lack of irritability of the condition.
(continued on the next page)
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Professional PT Clinical Corner
Page 9
Case Study : Cervical/Shoulder
Objective Exam
(continued rom previous page)
+ findings
Therapist Thoughts
Posture:
Prominent thickening in the C7/T1 region, mod forward head
AROM
Cervical flexion: 2 fingers from chest, poor unwinding most
of the motion occurring at C6/7
Cervical extension (dorsal glide): 1/4 ROM, right upper trap
pain produced.
Right rotation: 55 degrees with pulling sensation on the left
Left rotation: 60 degrees
Lateral flexion: right 30 degrees with pinch on the right.
This is evidence of increased
activity and strain at the CT
junction and this area needs to
be further examined.
The patients exact trap pain
was produced with Cervical DG
and right lateral flexion
Right shoulder: all WNL except hand behind back (T9) with
scapula winging and horizontal adduction: 3/4 ROM
Elbow/wrist WNL
Passive Physiological Movements
Neuro exam/ULTT tests
Passive Accessory Motion
testing
Special test (+
tests)
Palpation
Right shoulder : ER 100 (at 90 abduction), IR 45 degrees. GH
flexion (w/o allowing scap movement) 130 (N=120)
Myotomal, dermatomal and reflex testing are normal.
ULTT1: at 45 degrees of EE pt experiences right thumb numbness
ULTT3; (ulnar nerve bias): medial elbow pull at ER 80 degree
and abduction to 100
Hypomobile:
C5 CPA, (central posterior to anterior pressure) right UPA
(Unilateral posterior to anterior pressure)
C6/ C7 right UPA, CPA with production of neck/UT pain
and T1/T2 CPA
GH joint: all WNL except A/P at 90 degrees abduction (slightly
hypo)
Negative medial epicondylitis tests
Positive right AC Cross over test
Positive Spurling on the right causing right elbow pain
Mild positive shoulder laxity testing at 120 abduction with full
ER
There may be some laxity of
the right shoulder anterior capsule
No nerve root compression that
we can discern on PE.
The medial elbow pain appears
to be related to adverse neural
tension.
Supports/Indicates a unilateral
extension dysfunction
AC joint and shoulder laxity issues need to be addressed
Increased tone, right UT, right middle scalenes, right triceps,
right levator scapulae
Summary of significant findings (or as Maitland terms, the comparable signs):
1. Dorsal glide of the Cervical Spine causes right Upper trap pain at 1/4 ROM
2. ULTT3 was mildly positive causing right medial elbow pain at ER 80, abduction 100
3. C6 passive accessory motion caused right cervical/scap pain
4. Cervical rotation right 50 degrees causes pull on left, right lateral flexion 30 degrees with a pinch on the
right.
These comparable signs need to checked after each technique to determine the effect of treatment.
Treatment on Day 1 was CPA (Central posterior to anterior pressure) C6, &, T1-3 the results : DG 1/2 ROM with
right UT pain, cx rot right 60, lat flexion right 35 degrees, ULTT3 ER 85 degrees, abduction 105 degrees.
Treatment goals after the first visit:
1. improve/restore mobility at the CT junction
2. Restore shoulder FF/IR mobility
3. restore normal gliding to the ulnar nerve
4. Assess scapula thoracic stability including muscle length and strength.
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Professional PT Clinical Corner
Page 10
Clinical gems of the Month
The diaphragm can refer pain
to the right upper trap.
Dura mater is capable of referring pain into more than
one dermatome, this may be
due to the extensive overlap
of consecutive sinuvertebral
nerves to the anterior aspect
of the dura mater.
Anterior knee pain can be
caused by triggers points in
the rectus femoris, vastus medialis, adductor longus, and
adductor brevis.
The gallbladder can refer pain
to the right shoulder and
scapula regions.
The capsular pattern for the
cervical spine is all motions
are limited except for cervical
flexion.
The Trigeminocervical Nucleus
(TCN) is located in the midbrain and is considered the
Robert Shapiro MA PT COMT
nocioceptive nucleus for the
head and upper neck.
When observing the patients
calf during your posture exam
a tight soleus makes the lower
end of the leg look cylindrical
causing the lower leg loose its
normal contour (conical).
When testing for myotomal
weakness of the C6 nerve root
In order for standing lumbar
flexion to be considered normal the following must occur:
1) patient must be able to
touch toes and return to upright positon. 2) sacral angle
must be more than 70 degrees 3) TL junction mustweight shift posterior to the
foot. 4) uniform curve.
supination is great second
muscle to test along side elbow flexion.
Reverse Phalens test (full
If you have any GEMS you want
wrist extension with full finger to share please email me at :
extension) has been shown to
increase pressure in the carpal rshapiro@professionalpt.com
tunnel almost 10 x more than
the traditional Phalens test
(full wrist flexion)
Quiz answers:
1. multifidi
2. Subscapularis/teres minor, teres major below, long head of the
triceps medially and the surgical neck of the humerus laterally
3. Sustained Natural Apophyseal Glides
4. Alar ligament
5. Adductor Magnus
For internal use only. Not intended for external sharing or distribution.
Professional Physical Therapy 2015
Potrebbero piacerti anche
- Newsletter - Rob S Vol 10 October 2015Documento10 pagineNewsletter - Rob S Vol 10 October 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 11 Jan 2016Documento10 pagineNewsletter - Rob S Vol 11 Jan 2016api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 9 Sept 2015Documento11 pagineNewsletter - Rob S Vol 9 Sept 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 7 July 2015Documento12 pagineNewsletter - Rob S Vol 7 July 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 6 June 2015Documento10 pagineNewsletter - Rob S Vol 6 June 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 5 May 2015Documento11 pagineNewsletter - Rob S Vol 5 May 2015api-323491985Nessuna valutazione finora
- Clinical Newsletter - Rob S Vol 2 Feb 2015Documento7 pagineClinical Newsletter - Rob S Vol 2 Feb 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 4 April 2015Documento7 pagineNewsletter - Rob S Vol 4 April 2015api-323491985Nessuna valutazione finora
- Newsletter - Rob S Vol 3 March 2015Documento9 pagineNewsletter - Rob S Vol 3 March 2015api-323491985Nessuna valutazione finora
- Clinical Newsletter - Rob S Vol 1 January 2015Documento3 pagineClinical Newsletter - Rob S Vol 1 January 2015api-323491985Nessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Rubric On Baking CakesDocumento3 pagineRubric On Baking CakesshraddhaNessuna valutazione finora
- Colonel SandersDocumento17 pagineColonel SandersAmandaNessuna valutazione finora
- What Is Aerobic Exercise?Documento27 pagineWhat Is Aerobic Exercise?Zedy GullesNessuna valutazione finora
- Pediatric Medication Dosing GuildelinesDocumento2 paginePediatric Medication Dosing GuildelinesMuhammad ZeeshanNessuna valutazione finora
- FF Recipe BookDocumento17 pagineFF Recipe BookElectrox3dNessuna valutazione finora
- 2mw Biomass Gasification Gas Power Plant ProposalDocumento9 pagine2mw Biomass Gasification Gas Power Plant ProposalsabrahimaNessuna valutazione finora
- 2021 Physician Compensation Report - Updated 0821Documento24 pagine2021 Physician Compensation Report - Updated 0821Michael Knapp100% (3)
- Atomic Structure Worksheet: Name PeriodDocumento4 pagineAtomic Structure Worksheet: Name Periodapi-496534295100% (1)
- 4Dx - Series B Capital Raising IMDocumento42 pagine4Dx - Series B Capital Raising IMsamNessuna valutazione finora
- Pipe TobaccoDocumento6 paginePipe TobaccoVictorIoncuNessuna valutazione finora
- Kolano - Plastrowanie DynamiczneDocumento9 pagineKolano - Plastrowanie DynamiczneRobert WadlewskiNessuna valutazione finora
- Sikament®-4101 NS: Product Data SheetDocumento2 pagineSikament®-4101 NS: Product Data SheetShihab AhamedNessuna valutazione finora
- Separating Mixtures: Techniques and Applications: Evaporation, Distillation and FiltrationDocumento4 pagineSeparating Mixtures: Techniques and Applications: Evaporation, Distillation and FiltrationAndrea SobredillaNessuna valutazione finora
- All About Ocean Life-Rachel BladonDocumento6 pagineAll About Ocean Life-Rachel BladonRichard TekulaNessuna valutazione finora
- Serbia Malta & Bermuda Medical Instructions PDFDocumento3 pagineSerbia Malta & Bermuda Medical Instructions PDFGISI KeyBOarD0% (1)
- Polymer LedDocumento14 paginePolymer LedNaveenNessuna valutazione finora
- Fan Adta-En-50hz-March-2018 - 20180315Documento52 pagineFan Adta-En-50hz-March-2018 - 20180315Andi JatmikoNessuna valutazione finora
- Affidavit: IN WITNESS WHEREOF, I Have Hereunto Affixed MyDocumento2 pagineAffidavit: IN WITNESS WHEREOF, I Have Hereunto Affixed Myceleste LorenzanaNessuna valutazione finora
- Carapace DigitalDocumento15 pagineCarapace DigitalVillain ChatNessuna valutazione finora
- Polymer ProDocumento25 paginePolymer ProJeerisuda KingklangNessuna valutazione finora
- 1635 The Papal Stakes - Eric FlintDocumento1.813 pagine1635 The Papal Stakes - Eric Flintwon100% (2)
- Microbiiology Lab LayoutDocumento9 pagineMicrobiiology Lab LayoutNageswara raoNessuna valutazione finora
- Review Related LiteratureDocumento3 pagineReview Related LiteratureHanz EspirituNessuna valutazione finora
- Recipe Book: Yule Logs 2020Documento28 pagineRecipe Book: Yule Logs 2020Cwt Chan100% (1)
- PS Ebook BagsPouches2 1116 HRDocumento58 paginePS Ebook BagsPouches2 1116 HRGovindarajulu RNessuna valutazione finora
- Translating Child Development Research Into Practice - Can Teachers Foster Children's Theory of Mind in Primary SchoolDocumento14 pagineTranslating Child Development Research Into Practice - Can Teachers Foster Children's Theory of Mind in Primary SchoolpecescdNessuna valutazione finora
- Form Apr 22 2022Documento4 pagineForm Apr 22 2022api-589628245Nessuna valutazione finora
- 06-433rev7 HFC-227ea IVO ManualDocumento109 pagine06-433rev7 HFC-227ea IVO ManualFelix MartinezNessuna valutazione finora
- Tom Kenyon - ImmunityDocumento9 pagineTom Kenyon - ImmunityDren Hoti100% (2)
- Ujian Diagnostik Ting 2 EnglishDocumento9 pagineUjian Diagnostik Ting 2 EnglishJ-Gie JaulahNessuna valutazione finora