Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Comparison of Superficial Mycosis Treatment Using Butenafine and Bifonazole Nitrat Clinical Efficacy
Caricato da
nuralitarpCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Comparison of Superficial Mycosis Treatment Using Butenafine and Bifonazole Nitrat Clinical Efficacy
Caricato da
nuralitarpCopyright:
Formati disponibili
Global Journal of Health Science; Vol. 5, No.
1; 2013
ISSN 1916-9736 E-ISSN 1916-9744
Published by Canadian Center of Science and Education
Comparison of Superficial Mycosis treatment using Butenafine and
Bifonazole nitrate Clinical Efficacy
Mohammed A. Abdul Bari1
1
Baghdad Collage of Pharmacy, Baghdad, Iraq
Correspondence: Mohammed A Abdul Bari, Baghdad Collage of Pharmacy, Baghdad, Iraq. E-mail:
najem20042003@yahoo.com
Received: September 5, 2012
Accepted: September 18, 2012
Online Published: November 11, 2012
doi:10.5539/gjhs.v5n1p150 URL: http://dx.doi.org/10.5539/gjhs.v5n1p150
Abstract
Superficial fungal infections are commonly encountered by the physician. And the continuously changing
epidemiology of invasive fungal infections results in the need for an expanded armamentarium of antifungal
therapies. This study was designed to evaluate the safety and efficacy of Butenafine (BTF) versus Bifonazole
(BFZ) in the treatment of superficial mycosis in a randomized, double-blind, parallel-group trial. Of 96 patients,
48 applied (BTF) cream and 48 applied (BFZ) cream for 2 weeks to tinea versicolor, corporis and cruris treat,
while tinea of feet & hands was treated for 4 weeks duration. Efficacy was assessed after the end of treatment
and 2 weeks later. At the end of therapy, we find somewhat more patients using (BTF) than using (BFZ) had a
mycologic cure ((BTF), 87.5%; (BFZ) 83.3%) and effective clinical response ((BTF), 91.7%; (BFZ), 83.3%).
(BTF) provides rapid and persistent antifungal activity and symptom relief in patients with superficial mycosis
during treatment. And patients continued to improve for at least 2 weeks after treatment. The Rates of mycologic
cure and effective treatment with (BTF) were higher than with (BFZ) at cessation of treatment and 2 weeks later.
However, no significant difference found between the two drugs (p> 0.05).
Keywords: butenafine, bifonazole, superficial mycosis
1.Introduction
Superficial fungal infections, including rare infections and commons skin disease confine to be limit to groups of
patients or geographical areas. Superficial mycosis has been considered to be as major world public health
problem and one of the most frequent diseases in human beings and animals (Burns et al., 2004; Kibbler et al.,
1996; Midgley et al., 1997; Merlin et al., 1990). Hence; the superficial mycosis clinical treatment has been
introduced by many of antifungal agents (Zarowny et al., 1995; Fredriksson, 1983; Kokoschka et al., 1986;
McVie et al., 1986; Groll & Tragiannidis, 2010; Nolting et al., 1992; Reyes et al., 1998; Del Palacio et al., 1999).
Nevertheless the increased use of such agents in recent years has caused the development of resistance to
available drugs. For this reason, a constant effort toward the synthesis of new antifungal agents has been made in
the last few years. In particular, the class of azoles (imidazole and Triazole derivatives) has supplied many
effective antifungal drugs currently in clinical use, and newer azoles with expanded spectrum of activity are at
the moment in continuous development (Han et al., 2011). Bifonazole (BFZ), an imidazole derivative, has a
broad spectrum of action used currently for topical therapy of mycoses and dermatomycoses (Gupta & Sauder,
1994; European Pharmacopoeia Commission, 2001). Butenafine (BTF) is a synthetic benzylamine antifungal
agent with fungicidal activity against susceptible organisms that have been approved in many countries
worldwide (Georgopapadakou, 1998). The therapeutic efficacy of these two agents was compared in this study.
2.Materials and Methods
Our hospital received 96 patients with superficial mycosis disease complaints. Informed consent was obtained.
We begin with complete medical history for each patient and record all data, including sex, age, and symptoms
and signs of the disease. A physical examination included total body mass, weight and dermatological inspection.
150
www.ccsenet.org/gjhs Global Journal of Health Science Vol. 5, No. 1; 2013
A clinical examination with standard laboratory tests was also carried out at inclusion and repeated after the end
of treatment and 2 weeks later. In addition, vascular disease, particularly diabetes and other medical condition's
history are record. Hence, any patients received antibiotic or antifungal treatment for previous 90 days are
excluded.
For this study 96-subjects with superficial skin mycosis by carry out KOH and fungal cultures positive
randomized, parallel group; double-blind. The study group (subjects, including female 54 Male 42, age 14~72;
duration of disease 3~10 months) divided into two treatment groups.
Of 96 patients, twice daily for 2 weeks each 48 applied (BTF) hydrochloride 1 and 48 applied (BFZ) 1%
cream to the affected area to treat versicolor, corporis and cruris tinea and tinea of feet and hands need 4 weeks
treatment. Efficacy was assessed after the end of treatment and 2 weeks late.
In this paper, the skin scraping by curetting of the affected webs was used for mycological study. For each
patient, the Potas-sium hydroxide preparation was performed and Sabouraud dext-rose agar (SDA) was used for
all specimens. Firstly, SDA with 0.005% chloram-phenicol to inhibit bacterial contamination and 0.05%
cycloheximide to inhibit contaminating fungi were used for selective isolation of dermatophytes. Secondly, SDA
without cycloheximide used to grow non-dermatophyte fungi that are commonly considered saprophytes or
contaminants. With the aid of a straight needle, small fragments of skin were placed on the surface of the agar in
Petri's dishes containing 40 mL of culture medium and pressed onto the surface to make a good contact. The
samples were adjusted into four different areas, or at least in two spots in the case of a scanty sample. Petri's
dishes were surrounded by paraffin seal to prevent dehydration and incubated at 30 C for 4 weeks before being
considered negative for fungus. Media were tested every 34 days for growth of fungus. Plates overgrown with
contaminants growing from Petri dish edges were eliminated. Media were examined macroscopically and when
applicable, the texture and surface color of the colony, as well as any pigment diffusing into the medium, were
carefully noted and recorded. An adhesive tape strip was applied onto the surface of the colony, and then
mounted in a drop of lactophenol cotton blue stain.
2.1 Drug Administration
The first group was treated with 1% (BTF) hydrochloride cream.
The second group was treated with 1% (BFZ) cream.
Both of them were treated by applying the cream twice daily for 2 weeks to treat tinea cruris, tinea corporis and
Tinea versicolor.And 4 weeks for tinea of feet and hands Where:
1% (BTF) hydrochloride cream
Brand Names: brand name: mai ke shu (Seaside Pharmaceutical Company)
1% (BFZ) cream
Brand Names: brand name: mei ke (Yongda drug manufactory)
2.2 Efficacy Criteria
A) Clinical Assessment
Beginning symptoms and signs for each Patients before, after treatment had been record and two-week later
accord to 4 levels from zero to three depending on the degree of itching, redness, papules & pustules before as
follows.
Zero=no, one=mild, two=moderate and three for server one.
SSRI = (TSBT- TSAT)/(TSBT)
where
Symptom score reduces the index: SSRI
Total Score before Treatment: TSBT
Total Score after Treatment: TSAT
151
(1)
www.ccsenet.org/gjhs Global Journal of Health Science Vol. 5, No. 1; 2013
Cure: rash fade away; the symptoms disappear and microscopic examination of fungus and culture were
negative, efficacy index 100%.
Obvious effect: rash markedly improved, symptoms relieved significantly; microscopic examination of fungus
and culture were negative, the index effect 70%.
Improved: rash and symptoms were improved; microscopic examination of fungus and culture were negative or
positive effect index 30% ~ 70%.
Not effective: skin rash did not disappear and, fungi examination and / or culture were positive, effective index
less 30%.
B) Laboratory Assessment Mycological Cure:
Clear: Both microscopically and fungal cultures were negative.
Not cleared: fungi examination and / or culture were positive.
C) Safety Criteria
Clinical checkup had been done before treatment, and patients blood, creatinine, urea, urine ALT, etc. then two
weeks later all analysis done at cessation of treatment. All withdrawal treatment by laboratory abnormal
parameters and vital signs also recorded.
D) Results Analysis
SPSS software was performed to analyse an intention-to-treat basis and to determine Quantitative variables such
as means and standard relatively by class based on dichotomous variables as absolute or both deviations and
categorical. The two tests (t-test and MannWhitney test) had been used to determine the significance of
differences between mean values of two continuous variables, and to determine non-parametric distribution
respectively. ANOVA as one-way analysis of variance was employed for comparison of several groups means
and to determine the means significant differences between the two groups. In addition, multiple regression
analysis was used to predictor the best diagnosis as a dependent variable. P < 0.05 was considered significant. 3.
Result
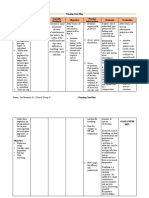
3.1 Clinical Effectiveness
There was high efficiency noticed for both drugs after end of treatment and 2 weeks later as shown in Table 1 and
Table 2.
Table 1. The effectiveness of clinical at of treatment
Group
cases
Cured
obvious effec
tiveness Improved
efficiency
BTF group
BFZ group
48
12
32
91.7
%
48
34
83.3
%
Significant difference was p> 0.05 for the two groups
Table 2. Clinical effectiveness 2 weeks after stooping treatment
Group
cases
Cured
obvious effec
tiveness
Improved
efficiency
BTF group
48
36
93.7
%
BFZ group
48
33
11
91.7
%
Also no significant difference found by comparing the two groups there was p> 0.05
3.2 Mycological Cure
High clearance rate is also noticed for both drugs after end of treatment and 2 weeks later as shown in Table 3
and Table 4.
152
www.ccsenet.org/gjhs Global Journal of Health Science Vol. 5, No. 1; 2013
Table 3. Mycological cure at end of treatment
Group
cases
BTF group
48
BFZ group
48
There wasnt any significant difference (p> 0.05)
cleared
clearance rate
42
40
87.5%
83.3%
Table 4. Mycological cure weeks after stooping treatment
Group
cases
BTF group
48
BFZ group
48
Similarly, there wasnt any significant difference (p> 0.05)
cleared
clearance rate
46
44
95.8%
91.7%
There was not any serious adverse effects.
For (BTF) cream there was no noticeable adverse reaction; also for (BFZ) cream apart from local skin erythema
and mild itching which require no treatment. Finally, no abnormality was found by laboratory examination for
the two groups treatment.
4.Discussion
The progress in managing of fungal infections, the incidence increased and response rates remain insufficient and
this may led to the development a new antifungal agent. Recent antifungal chemotherapy drugs show new
advances in offer clinician's fewer toxic alternatives and more effective at conventional therapy. BTF
hydrochloride has similar action a synthetic benzylamine derivative mode to that of the allylamine class of
antifungal drugs (Gerald & Mc Evoy, 2008).
The evaluation of randomized, double-blind, controlled trial for the safety and efficacy of 2 weeks, twice-daily
treatment with (BTF) versus (BFZ) for each patient with versicolor, cruris, and corporis tinea; and 4 weeks to
treat tinea of feet & hands. The final comparing the treatment of BTF group mycologic cure higher than a BFZ
show group (87.5, vs. 83.3%, p> 0.05). Similarly, the mycologic cure rates at the 2 weeks follow-up were 95.8%
vs. 91.7%, respectively (p >0.05). Clinical efficiencies were 91.7% for (BTF) group, compared to 83.3% for BFZ
group in the (p>0.05). Then after 2 weeks clinical efficiency was 93.7% for (BTF) group, compared to 91.7% for
BFZ group (p> 0.05). These results show that both (BFZ) and the significant advance for newer (BTF) treatment
of fungal infections. Their expanded activity gives the clinician efficacious, safe, inexpensive and available more
choices other than conventional treatment. Particularly, the optimal treatment of superficial mycosis still remains
in the resistant cases with neither drug class offering an overwhelming advantage. Slightly higher rates of
mycologic cure and effective treatment, (BTF) group offers a little advantages over (BFZ) group. The BTF main
benefits are appeared as safety, ease of use, and offset by its current additional costs.
No serious side effects were noted with (BTF) except for mild itching and skin rash, but it was tolerable and no
patient discontinued therapy due to an adverse event. In the adverse events for most commonly uncontrolled
trials, associated with the use of (BTF) group 1% cream included erythema, contact dermatitis, itching, and
irritation, for each occurring in less than 2% of patients (Syed et al., 1998).
5.Conclusion
In this paper, during patient treatment (at least 2 weeks) BTF provides rapid improving antifungal activity and
symptom relief with superficial mycosis The Rates of mycologic cure and effective treatment with (BTF) were
higher than with (BFZ) at cessation of treatment. However, statistically there was not any difference significant
between the two drugs (p> 0.05). References
Burns, T., Breathnach, S., Cox, N., & Griffiths, C. (2004). Rook's Textbook of Dermatology (4th ed).
http://dx.doi.org/10.1002/9780470750520
Del Palacio, A., Cuetara, S., & Perez, A. (1999). Topical treatment of dermatophytosis and cutaneous candidosis
with flutrimazole 1% cream: double-blind, randomized comparative trial with ketoconazole 2% cream.
Mycoses, 42, 64955. http://dx.doi.org/10.1046/j.1439-0507.1999.00520.x
European Pharmacopoeia Commission. (2001). European Pharmacopoeia, (4th ed), Council of Europe, 67075
Strasbourg Cedex, France, p. 737.
153
www.ccsenet.org/gjhs Global Journal of Health Science Vol. 5, No. 1; 2013
Fredriksson, T. (1983). Treatment of dermatomycoses with topical tioconazole and miconazole. Dermatologica
(Suppl), 66, 20 33. http://dx.doi.org/10.1159/000249910.
Georgopapadakou, N. H. (1998). Antifungals: mechanism of action and resistance, established and novel drugs.
Curr. Opin. Mirobiol, 1, 547-557. http://dx.doi.org/10.1016/S1369-5274(98)80087-8
Gerald, K., & Mc Evoy. (2008). AHFS Drug information. American Society of Health-System Pharmacists.
Bethesda. American Society of Health System Pharmacists.
Groll, A. H., & Tragiannidis, A. (2010). Update on antifungal agents for paediatric patients. Clin Microbiol
Infect, 16(9), 1343-53. http://dx.doi.org/10.1111/j.1469-0691.2010.03334.x
Gupta, A. K., & Sauder, D. N. (1994). Shear NH: Antifungal agents: An overview. Part II. J Am Acad Dermatol,
30, 91 I-933.
Han, K., Bies, R., Johnson, H., Capitano, B., & Venkataramanan, R. (2011). Population pharmacokinetic
evaluation with external validation and Bayesian estimator of voriconazole in liver transplant recipients.
Clin Pharmacokinet, 50(3), 201-14. http://dx.doi.org/10.2165/11538690-000000000-00000.
Kibbler, C. C., MacKenzie, D. W. R., & Odds, F. C. (1996). Principles and Practice of Clinical Mycology.
Chichester: Wiley.
Kokoschka, E. M., Niebauer, G., Mounari, M., & Monici Preti, P. (1986). Treatment of dermatomycoses with
topical fenticonazole and econazole. Mykosen, 29, 4550.
Mc Vie, D. H., Littlewood, S., Allen, B. R., Pollock, A. C., Wood, P., & Milne, L. J. (1986). Sulconazole versus
clotrimazole in the treatment of dermatophytosis. Clin Exp Dermatol, 11, 6138.
http://dx.doi.org/10.1111/j.1365-2230.1986.tb00518.x
Merlin, K., Kilkenny, M., & Plunkett, A. (1990). The prevalence of common skin conditions in Australian school
students:
4
tinea
pedis. Br
J
Dermatol,
140,
897901.
http://dx.doi.org/10.1046/j.1365-2133.1999.02822.x
Midgley, G., Clayton, Y. M., & Hay, R. J. (1997). Diagnosis in Colour. Medical Mycology. London: MosbyWolfe.
Nolting, S., Semig, G., & Friedrich, H. K. (1992). Double-blind comparison of amorolfine and (BFZ) in the
treatment of dermatomycoses. Clin Exp Dermatol (Suppl 1), 17, 5660.
Reyes, B. A., Beutner, K. R., Cullen, S. I., Rosen, T., Shupack, J. L., & Weinstein, M. B. (1998). A fungicidal
benzylamine derivative, used once daily for the treatment of interdigital tinea pedis. Int J Dermatol, 37,
4503. http://dx.doi.org/10.1046/j.1365-4362.1998.00245.x
Syed, T. A., Ahmadpour, O. A., & Ahmad, S. A. (1998). Shamsi S. Management of toenail onychomycosis with
2% butenafine and 20% urea cream: a placebo-controled, double-blind study. J Dermatol, 25(10), 648-52.
Zarowny, D. P., Rogers, R. S., & Tindall, J. P. (1995). Evaluation of the effectiveness of griseofulvin, tolnaftate,
and placebo in the topical therapy of superficial dermatophytoses. J Invest Dermatol, 64, 26872.
http://dx.doi.org/10.1111/1523-1747.ep12510680
154
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- BMJGH 2019 002080Documento9 pagineBMJGH 2019 002080nuralitarpNessuna valutazione finora
- Status UjianDocumento4 pagineStatus UjiannuralitarpNessuna valutazione finora
- Fetal Circulation & Common Cardiac Disorder in ChildrenDocumento17 pagineFetal Circulation & Common Cardiac Disorder in ChildrennuralitarpNessuna valutazione finora
- Morning Report: Department of Internal MedicineDocumento12 pagineMorning Report: Department of Internal MedicinenuralitarpNessuna valutazione finora
- Ex-Vivo Characterization of Human Colon Cancer: by Mueller Polarimetric ImagingDocumento12 pagineEx-Vivo Characterization of Human Colon Cancer: by Mueller Polarimetric ImagingnuralitarpNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- WelcomeDocumento74 pagineWelcomeSagarRathodNessuna valutazione finora
- Presc Audit ReportDocumento85 paginePresc Audit ReportAnuj KaushalNessuna valutazione finora
- Mental Health Class NotesDocumento3 pagineMental Health Class Notessuz100% (4)
- MTL CHAPTER 9 2020 ClickUpDocumento11 pagineMTL CHAPTER 9 2020 ClickUpcharlieNessuna valutazione finora
- Bazaar DrugsDocumento104 pagineBazaar DrugsKartik Vashishta100% (1)
- Invos System Improving Patient Outcomes Cerebral Somatic Oximetry BrochureDocumento6 pagineInvos System Improving Patient Outcomes Cerebral Somatic Oximetry Brochuremihalcea alinNessuna valutazione finora
- Master The Perfec Tnight of SleepDocumento10 pagineMaster The Perfec Tnight of SleepPaulo André Prada de CamargoNessuna valutazione finora
- Endocrine Glands PDFDocumento99 pagineEndocrine Glands PDFXochitl ZambranoNessuna valutazione finora
- Kode Penjelasan Keterangan: ObgynDocumento14 pagineKode Penjelasan Keterangan: Obgynanon_507132438Nessuna valutazione finora
- Cystic Hygroma - Symptoms - Diagnosis - Treatment of Cystic Hygroma - NY Times Health InformationDocumento3 pagineCystic Hygroma - Symptoms - Diagnosis - Treatment of Cystic Hygroma - NY Times Health InformationRenno AdiNessuna valutazione finora
- SAM 350P User ManualDocumento40 pagineSAM 350P User ManualkristiaNessuna valutazione finora
- HR 2 FormDocumento8 pagineHR 2 Formrkpatel40Nessuna valutazione finora
- Intra-Arterial Catheterization For Invasive Monitoring: Indications, Insertion Techniques, and Interpretation - UpToDateDocumento40 pagineIntra-Arterial Catheterization For Invasive Monitoring: Indications, Insertion Techniques, and Interpretation - UpToDatejuanpbagurNessuna valutazione finora
- Analytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajDocumento7 pagineAnalytical Case Study of Bmiof Mildly Symptomatic Covid-19 Patients With Reference To MizajyusufNessuna valutazione finora
- Drug Education 1-H and A & FDocumento4 pagineDrug Education 1-H and A & FLEON CAMPUSNessuna valutazione finora
- Splice PDFDocumento5 pagineSplice PDFpedroNessuna valutazione finora
- Nursing Care PlanDocumento13 pagineNursing Care PlanJan DamesNessuna valutazione finora
- Dermatology NotesDocumento59 pagineDermatology NotesAbdullah Matar Badran50% (2)
- Child Labor in The PhilippinesDocumento7 pagineChild Labor in The PhilippinesMark Gerald Lagamia0% (1)
- Principles of Adolescent Substance Use Disorder Treatment PDFDocumento42 paginePrinciples of Adolescent Substance Use Disorder Treatment PDFDanilo CozzoliNessuna valutazione finora
- Lecture 32 - Nutritional DisordersDocumento43 pagineLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Diseases of The CallitrichidaeDocumento48 pagineDiseases of The CallitrichidaeCristhian HernandezNessuna valutazione finora
- Assis 2017Documento19 pagineAssis 2017widyadariNessuna valutazione finora
- Bril (2002) - Validation of The Toronto Clinical Scoring System For Diabetic PolyneuropathyDocumento5 pagineBril (2002) - Validation of The Toronto Clinical Scoring System For Diabetic PolyneuropathyRicky WatariNessuna valutazione finora
- Structural Organisation in Animals - IIDocumento70 pagineStructural Organisation in Animals - IIMay HarukaNessuna valutazione finora
- Acute Cardiac EKG Interpretation - Basics Part 1 - ScriptDocumento2 pagineAcute Cardiac EKG Interpretation - Basics Part 1 - ScriptDarby GravinoNessuna valutazione finora
- At Merienda - Individual ActivityDocumento6 pagineAt Merienda - Individual ActivityMoreno, John Gil F.Nessuna valutazione finora
- USMLE Step 1 First Aid 2021-101-230Documento130 pagineUSMLE Step 1 First Aid 2021-101-230mariana yllanesNessuna valutazione finora
- Normal Periodontium 1Documento49 pagineNormal Periodontium 1mdio midoNessuna valutazione finora
- Group Assignment Population EconomicsDocumento7 pagineGroup Assignment Population EconomicsSayed Abdullah Shah SadaatNessuna valutazione finora