Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pressure Points - Postnatal Care Planning
Caricato da
NoraDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pressure Points - Postnatal Care Planning
Caricato da
NoraCopyright:
Formati disponibili
Postnatal care planning
Postnatal care planning
The message we are getting from
our members is clear. We must do
something to address the state of
postnatal care. Thats what our
campaign Pressure Points is all
about. Presenting the evidence and
making a case for better provision
of postnatal care enabling
midwives, maternity support workers
and student midwives to give
women and their families the care
that they deserve.
This report continues our study by
focusing on postnatal care planning
and demonstrating how the situation
could be improved through the
funding of more midwives. One thing
is certain our members cannot
continue to paper over the cracks in
an underfunded and under-resourced
postnatal environment, without
there being detrimental effects on
the health of women, children and
the over-stretched maternity teams
who are crying out to be given the
tools to support them.
Pressure Point 4
Postnatal care planning
The background
The impact that good postnatal care could have on womens
experiences and their long-term health in the context of the
increasing complexity of the health of women who become
pregnant, more intervention in labour, the high rate of caesarean
sections and widespread morbidity should not be underestimated.
Surveys of womens views of maternity care
repeatedly inform us of their unhappiness with the
current provision of postnatal care which is not able
to provide them with the support they need.
Despite policy rhetoric that supports womens
choice and their involvement in decision making,
the findings in this report evidence the fact that
the NICE recommendation for individualised care
planning that could improve continuity of care and
ensure women and their babies receive the number
of postnatal contacts appropriate to their needs, is
not being implemented.
The role of the maternity team in supporting
women and recognising the onset of complications
is vital. However, there has been a decrease in
the length of postnatal stay in hospital and the
number of home visits and there appears to be little
recognition of the value of continuity of care.
This has led to a situation where the current
content and timing of postnatal care is not meeting
womens health needs.
Chief Executive,
Royal College of Midwives
Postnatal care planning
What should women be receiving?
Individualised care is key to providing
important information at the appropriate time,
recognising when additional support is needed
and offering targeted interventions through the
appropriate multiple agency care pathways.
We know that women are asking for postnatal
care that is able to be supportive and listening
and where possible in their own home. These
aspirations are reflected in the NICE quality
standard on postnatal care.
What NICE guidance says
Postnatal care should be a continuation of
the care the woman received during her
pregnancy, labour and birth and involve
planning and regularly reviewing the content
and timing of care, for individual women and
their babies. Each postnatal contact should be
provided in accordance with the principles of
individualised care.
The NICE quality standard recommends that:
A documented, individualised postnatal care
plan should be developed with the woman
ideally in the antenatal period or as soon as
possible after birth. This should include:
The survey results
Between September and November 2013 the RCM surveyed our
midwife, maternity support workers and student midwife members
across the UK. We then asked the mothers at www.netmums.com for
their experiences within the postnatal care period. These are the results.
relevant factors from the antenatal,
intrapartum and immediate postnatal period
details of the healthcare professionals
involved in her care and that of her baby,
including roles and contact details
plans for the postnatal period including:
> details about adjustment to
motherhood, emotional wellbeing and
family support structures
> plans for feeding, including specific
advice about either breastfeeding
support or formula feeding.
Midwives
MSWs
Student Midwives
Mothers
The plan should be reviewed at each postnatal
contact. Planning and regularly reviewing the
content and timing of care for individual women
and their babies, and communicating this
(to the woman, her family and other relevant
postnatal care team members) through a
documented care plan can improve continuity
of care. Women and their babies should receive
the number of postnatal contacts appropriate to
their care needs.
Postnatal care planning
Influencing factors
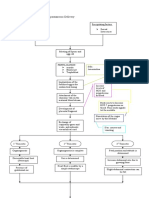
Overwhelmingly, two-thirds of midwives said the
most important factor influencing the number
of postnatal visits a woman receives was not the
womans needs, but was the pressure on the service
from, for example, the midwife shortage.
We asked midwives
- What is the most
significant factor
influencing the decision
about the number of
postnatal visits a
woman receives?
23%
65%
9%
3%
That only one midwife in four told us that it was
womens needs which determined the number of
visits received, is deeply worrying.
Postnatal care should always be based on
womens needs and not on how underfunded and
overstretched local maternity services are.
Midwives ability to plan care with women
will reflect the directives from managers and
commissioners. It is clear that our members feel it is
this which is seen to be prescribing and limiting the
number of visits.
Womens needs
Organisational pressures
Commissioners directives
Traditional service provision
Recommendation
Postnatal services must be commissioned and
provided in a way that is consistent with NICE quality
standard recommendations It is unacceptable
that women are not currently provided with an
individualised postnatal care plan and equally
unacceptable that there are not enough midwives to
ensure women receive the number of postnatal visits
that are appropriate to their needs.
Postnatal care planning
Opportunities for developing and
reviewing the care plan.
We asked
mothers - Did
the midwife tell you
before you had the
baby what sort of care
you would receive
after birth?
We
asked mothers
- Did you discuss
your postnatal plan
with a member of the
maternity team
after the birth?
No
Nearly half of women did not remember discussing
a postnatal care plan before the birth. Although an
explanation for this may be that most women are
unlikely to receive postnatal care from the midwife
they met while they were pregnant, it is worrying that
mothers are not made aware of the level of service and
support that they can expect in the postnatal period.
10%
Yes she told me exactly when and how often she would visit
37%
Yes but only in general terms
44%
No she didnt tell me
9%
I dont remember if we discussed this or not
64%
21%
15%
Yes
Dont remember
It is perhaps even more worrying that nearly twothirds of mothers had not discussed the postnatal
care plan after the birth either.
If these conversations between women and
midwives are not happening because resources
are stretched, it is no wonder that both are left
disappointed with the postnatal care being offered.
Postnatal care planning
We asked midwives
and MSWs - Can you
identify in which of the
following subjects you think
there is usually enough time
and resources to support
and inform women?
10
Home safety (eg room temperature, smoking)
59%
60%
Hand hygiene and general cleanliness
51%
45%
Changing the nappy
50%
64%
Cord care
68%
74%
Bathing the baby demonstration
20%
46%
Breastfeeding latching
71%
76%
Breastfeeding position
70%
71%
Artificial feeding sterilisation of equipment
33%
45%
Artificial feeding preparation of feeds
34%
46%
Safer infant sleeping
74%
62%
Normal infant behavior
35%
39%
Maternal physical wellbeing
67%
55%
Maternal emotional wellbeing
41%
40%
Contraception
44%
33%
Reviewing the postnatal care plan
35%
35%
Our members have consistently reported that
there is seldom enough time to convey all the
information they would like to about postnatal
care. It is particularly concerning that only 35% of
midwives and MSWs say they have enough time
to review the postnatal care plan. This makes it
clear that individualised care is not the case for the
majority of women. The care being offered cannot
be responsive to womens needs when there is not
enough time to discuss it with them.
11
Postnatal care planning
mother - I had a specialist gateway midwife who gave me
amazing care in the community. I dread to think how I would
have done without the amazing service and care I received.
Number of visits
We asked midwives
and MSWs - What is
the average number
of postnatal visits a
woman receives?
Midwives
Maternity Support Workers
60%
54%
48%
41%
36%
28.9%
24%
23%
18.1%
12%
0%
12%
2%
4.8%
One
Two
The number of postnatal contacts has decreased
significantly during recent years, with little
evaluation of the impact. Despite national
policy describing the need for effective care
to meet the needs of women and their babies
up to 6 to 8 weeks after birth and if need be
beyond, postnatal services are currently being
dramatically cut. Serious attention needs to be
12
8%
7.2%
Three
Four
We asked mothers - How
many postnatal visits
did you receive once you
were at home?
None
3.4%
One
14.4%
Two
25.6%
Three
25.0%
More than three
31.6%
It is disappointing but not surprising in the current
context that 14% of women only received one visit
and a small minority received no visit whatsoever.
Individualised care plans centred on a continuity of
care model, would help ensure that women receive
the care and support they need in the postnatal
period and reduce the risk of the needs of women
falling between overstretched midwives.
mother - Once I got
home I saw a midwife for
no more than 10 minutes
on two occasions both
within 8 days of giving
birth. I never, before or
after birth, saw the same
midwife twice, so I often
had to explain everything
over and over which
took up all the time in
my appointments rather
than them being a time
for discussing my care.
Despite strong policy rhetoric advocating womens
choice and involvement in decision making in
maternity care, the findings here confirm that
midwives and maternity support workers do not
have enough time to appropriately review the
postnatal care plan and offer the women in their
care involvement in the decision making.
Five
given as to whether the three visits, which the
majority of midwives and MSWs thought to be
the average number undertaken, is an acceptable
average, and whether it is capable of offering
safe care, in the context of early discharge from
hospital and increasing readmission rates of
mother and babies, increasing infection rates
and postnatal morbidity.
Recommendation
Providers of NHS maternity care need to ensure that
midwives and MSWs are given time to prioritise a
postnatal care plan with women. This would be aided
by offering models of care that provide continuity.
The RCM recognises that continuity of care is a very
significant factor in determining the satisfaction
women feel when reviewing their postnatal care. We
ask that NHS commissioners now listen to women,
midwives and maternity support workers and help us
implement a truly effective model of care.
13
Postnatal care planning
Where postnatal care takes place
We asked mothers Do you feel you had
enough time in hospital
after giving birth?
9%
No - I felt rushed out before I was ready
31%
I was keen to get home but also felt
unsupported and not quite ready to leave
29%
Yes - they made me feel I was
happy to stay until I was ready
31%
I had to stay longer than I would have
liked because me (or my baby) were unwell
Alarmingly only 29% of women felt able to
stay as long as they felt they needed. Even more
disturbingly, 9% felt that they were rushed out
before they were ready. The length of stay has
steadily decreased over the last fifteen years
with the majority of women now leaving hospital
within six hours of the birth. This reduction in
postnatal length of stay is in the context of
14
mother - I had great care with my first
baby, with the 2nd I was rushed home
within couple hours of giving birth,
distressed and in pain, probably still in
shock, which contributed to my PND.
increased instrumental and caesarean deliveries
which requires more intensive postnatal care.
NICE recommends that: Length of stay in a
maternity unit should be discussed between
the individual woman and her healthcare
professional, taking into account the health and
well-being of the woman and her baby and the
level of support available following discharge.
mother - Definitely feel
that staff are under huge
stress and the quality of
care is affected. After I
had my first baby I felt
awful and wanted to stay
overnight but was told no
that it was not a hotel!
midwife - The women are
discharged inadequately prepared
from the ward because the
hospital is grossly understaffed.
midwife - The management
told me that I had to discharge
this woman who was struggling
with breast feeding as we
needed the bed. There is little
support for the women due to
our early discharge policy.
15
Postnatal care planning
mother - A midwife never came to
me; I had to go to the maternity unit.
We asked midwives
and MSWs - Where is
postnatal care provided
in your area?
Midwives
midwife - Since re-structuring delivery of care continuity has
disintegrated. Lack of staff and money has led to a fragmented service.
We asked
mothers - Where
did your postnatal
care take place?
MSWs
100%
95%
80%
84%
66%
60%
88%
At home
7%
At the hospital
2%
At the GP surgery
3%
At a postnatal clinic
58%
48%
40%
43%
38%
28%
20%
19%
35%
32%
30%
28%
25%
20%
17%
15%
11%
0%
Home
Stand alone Alongside
midwifery midwifery
led unit
led unit
mother - I had to
go all over for it even
having a new baby,
a C-section scar and
being a single mum.
16
Labour
ward
Postnatal
ward
GP
surgery
Postnatal
clinic
Children's
centre
On the
phone
mother - I think parents should have a few
visits at home; I had to travel on a bus with
my baby to a clinic that isnt even near my
house. Nobody came to my house either
a day or a few days after to help with
breastfeeding I had to ask a neighbour. I
felt pretty let down after the birth of my
daughter, luckily I had my mum.
These findings demonstrate that a considerable
number of women still receive at least some of
their postnatal care at home. Good postnatal care
planning should enable women to take part in the
decision about where it takes place. There should
be genuine choice about whether the woman
gets home visits or accesses postnatal care via
community setting i.e. childrens centres. The RCM
believes it is important that the first postnatal
meeting with a midwife should be offered as a
home visit where possible and where appropriate,
according to the womans home environment.
43% of the midwives reported the use of postnatal
clinics and 35% the use of the phone. The use of
both these facilities has increased dramatically in
recent years. The increased use of these less personal
contacts might offer useful flexibility and potential
access to peer support for some women, but it can
also limit the potential for valuable information
sharing between the woman and the midwife, and
can result in women being less likely to voice concerns
about their emotional or mental wellbeing.
Recommendation
Postnatal care planning should enable women to take part in the decision and to make genuinely informed
choices about where it takes place.
17
Postnatal care planning
mother - I had trouble feeding
so my midwife visited me a lot.
Individualised care
Reasons for extra visits
We asked midwives
and MSWs - Did the
last woman you looked
after have more visits
than would be usual in
your practice?
25%
midwife - Women are all
different and their needs
cannot be treated by dictate.
Yes
Extra
Visits
Yes
18%
Feeding
34%
Emotional well-being / mental health
12%
Clinical concern about baby
19%
Clinical concern about mother
25%
Safeguarding issue
3%
Support of vulnerable family
6%
When asked to explain the reasons for extra visits the
most common reasons given by midwives were to
provide support with feeding (34%) and in response
to a clinical concern about the mother (25%).
mother - My community
midwife was very good
and I did receive good
care but they are very
stretched in terms of the
time they can give you.
18
midwife - I feel lucky that as a homebirth
midwife, my caseload allows me to give
extra time to my women, however, our
community midwives dont have that
luxury and we are always helping them
with their visits and clinics, which then
impacts on the care we provide.
Members of the maternity team are clearly
attempting to paper over the cracks of a creaking
postnatal care system by offering more visits
whenever they are able to. Corners being cut to
make cost savings, such as rushing to discharge
women, inevitably lead to maternity teams
stretching themselves to offer care later in the
postnatal care cycle.
Recommendation
Midwives should be entrusted to make clinical decisions about the number of postnatal contacts in line with
womens and babies needs and staffing levels should be established which enable this to happen.
19
Postnatal care planning
Continuity of care
mother - I never saw the
same midwife twice before
or afterwards, I felt like an
item for them to tick off and
got no real sense of care.
mother - I saw so many different
midwives, both before and after
the birth of my baby they had
not a hope of offering the kind of
care that I wanted. I never had a
chance to get to know and trust
any of them, and they never had
a chance to get to know me.
Despite the significant body of evidence
demonstrating the value continuity of care in the
provision of maternity services, it is disturbing that
only 4% of the women in this survey had had full
continuity of care that included antenatal, labour and
postnatal care.
We asked
midwives - How
would you describe
the relationship with
the last woman you
looked after?
27% of the women did have some care from the
same midwife antentally and postnatally but nearly
half of these women had only met the midwife during
the postnatal period.
Main carer antenatal, labour and postnatal
4%
Main carer antenatal and postnatal
27%
Main carer labour and postnatal
9%
Some care antenatal, labour and postnatal
4%
Some care labour and postnatal
7%
Postnatal care only
49%
Recommendation
Midwives and MSWs must be enabled to prioritise
continuity of care, through the intelligent
commissioning of maternity services. Models of care
20
must be implemented that have adequate provision
for home births and births in free standing maternity
units, which are more able to provide this continuity.
21
Postnatal care planning
Use of NICE postnatal quality standard
We asked student
midwives (who were
approaching qualification)
- Are you familiar with the
NICE quality standard
regarding the individualised
postnatal care plan?
82%
22
Yes
79%
Yes
student midwife - Never
came across this in practice.
No
18%
care plan. In addition 18% of those asked were
concerned that they did not feel adequately prepared
to discuss the plan with women.
student midwife - I
wasnt even aware that
such a plan existed.
21%
We asked student
midwives (who were
approaching qualification) Could you adequately discuss
with women their personal
individualised postnatal
care plan (IPPCP)?
No
One in five of the student midwives who were near
qualification were not aware of what the NICE
quality standard was saying about the postnatal
student midwife - Despite NICE
guidelines I have not yet observed
or been involved in developing a
care plan. Women are told what
visits they will be given and vary
rarely asked what they feel they
need for postnatal care.
student midwife - No placement
on postnatal since beginning of 1st
year. Now a 3rd year... Hope I can
remember what Im meant to do!
student midwife - There is
simply not enough time when
out in the community to make
individualised care planning.
23
Postnatal care planning
We asked midwives Are you aware of the
recently pubished NICE
quality standard on
postnatal care?
midwife - It has not been
promoted/acknowledged by out
trust and it wont make the slightest
bit of difference to the managers
who try to control my practice.
Yes but I havent
had an opportunity
to look at it in detail
50%
18%
No, I have not
received any
information
about it
32%
24
Our findings, that the majority of midwives (68%)
are not fully aware of relevant NICE guidance,
demonstrates that this information is not being
readily disseminated to front line staff, that they do
not have time to engage with it in any detail and
the content does not appear to be a policy driver.
midwife - Too busy to
remember what is in it.
Student midwives are more aware of what NICE
guidance recommends, but it is alarming that 18%
of those near qualification do not feel adequately
prepared to have the discussion with women. Their
comments tell us that they do not see also tell a
story that they do not see it as having any impact
on practice.
Recommendation
Yes and I
know what it
recommends
Organisations providing maternity care must ensure
that they adequately disseminate relevant NICE
guidance and that midwives are absorbing the key
recommendations so they are clear on what they
are meant to be providing. Comprehensive postnatal
care planning should be able to adequately respond
to the clinical needs of mothers and babies, and to
allow for support where it is needed most, be that
maternal mental health issues, support with infant
feeding or time spent educating parents.
The Pressure Points outlined here make clear that the
majority of midwives and maternity support workers
are not able to provide this care to a standard they
are pleased with. They are being constrained by a
system which doesnt allow them enough time to
discuss, and respond to, womens individual needs.
Midwives and MSWs want to offer individualised
postnatal care planning for the sake of women and
their babies, we need a system of commissioning
which enables them to do this.
25
Postnatal care planning
How do we fix this?
Despite the existence of NICE recommendations,
our surveys have identified significant gaps between
what women should be getting in terms of postnatal
care planning and what they are actually receiving.
The RCM believes there are a number of practical steps that can be taken to ensure that all women
receive the care that they need and is appropriate to them. These measures could include:
Postnatal services should be commissioned and provided in a way that is consistent
with NICE quality standard recommendations. In particular they should comply with the
recommendations that women are provided with an individualised postnatal care plan and that
there are enough midwives to ensure women receive the number of postnatal visits that are
appropriate to their needs.
Implementation of a maternity care pathway that reflects postnatal planning from pregnancy.
Adequate numbers of midwives and MSWs with time to develop and review the care plan in
response to womens needs.
Postnatal care planning that enables women to take part in the decision about where it takes place.
Underpinning all this is the need for more midwives,
particularly in England. A lack of resources is the key
reason standards of postnatal care are not as good
as they could be. Attempts at improving care will
always fall down in a service struggling to deliver
many of the basic aspects of maternity care.
Progress must be made on this if we are to get
anywhere in delivering the improvements in
postnatal care that the RCM wants to see, midwives
believe are necessary, the evidence shows are
important and which mothers deserve.
Get involved with our campaign online at
www.rcm.org.uk/pressurepoints
Midwifery staffing that reflects policy demands and can offer continuity of care.
Midwives empowered and entrusted to make clinical decisions about number of postnatal
contacts in line with womens and babies needs.
26
27
Postnatal care planning
The Royal College of Midwives
Published August 2014
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Physiology of Normal Spontaneous DeliveryDocumento2 paginePhysiology of Normal Spontaneous DeliverySummer Rain100% (2)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Injections SiteDocumento10 pagineInjections SiteNora100% (2)
- Indian Wife Taken byDocumento10 pagineIndian Wife Taken byRahul Jat100% (1)
- Stress Urinary Incontinence in Relation To Pelvic Floor Muscle StrengthDocumento10 pagineStress Urinary Incontinence in Relation To Pelvic Floor Muscle StrengthNoraNessuna valutazione finora
- Antenatal Care and Its Effect On Risk of PihDocumento11 pagineAntenatal Care and Its Effect On Risk of PihNoraNessuna valutazione finora
- Thyroid Hormonal Changes Among Women With Polycystic Ovarian SyndromeDocumento14 pagineThyroid Hormonal Changes Among Women With Polycystic Ovarian SyndromeNoraNessuna valutazione finora
- Female Circumcision: Limiting The Harm (Version 2 Peer Review: 2 Approved, 1 Approved With Reservations)Documento8 pagineFemale Circumcision: Limiting The Harm (Version 2 Peer Review: 2 Approved, 1 Approved With Reservations)NoraNessuna valutazione finora
- Pregnancy in A Patient With Recurrent GlioblastomaDocumento6 paginePregnancy in A Patient With Recurrent GlioblastomaNoraNessuna valutazione finora
- Abdul Halim, Abu Sayeed Md. Abdullah, Fazlur Rahman, Animesh BiswasDocumento11 pagineAbdul Halim, Abu Sayeed Md. Abdullah, Fazlur Rahman, Animesh BiswasNoraNessuna valutazione finora
- Anaemia On First Trimester PregnancyDocumento11 pagineAnaemia On First Trimester PregnancyNoraNessuna valutazione finora
- Bakri Balloon PDFDocumento5 pagineBakri Balloon PDFNoraNessuna valutazione finora
- Preterm DeliveryDocumento12 paginePreterm DeliveryNoraNessuna valutazione finora
- Active Management of Pregnant Cancer PatientDocumento9 pagineActive Management of Pregnant Cancer PatientNoraNessuna valutazione finora
- Menu Makanan Untuk Pesakit Hospital: IsninDocumento2 pagineMenu Makanan Untuk Pesakit Hospital: IsninNoraNessuna valutazione finora
- A Randomized Trial of Coached Versus Uncoached Maternal Pushing During The Second Stage of Labor 2006 American Journal of Obstetrics and GynecologyDocumento4 pagineA Randomized Trial of Coached Versus Uncoached Maternal Pushing During The Second Stage of Labor 2006 American Journal of Obstetrics and GynecologyNoraNessuna valutazione finora
- Pressure Points - Postnatal Care Planning PDFDocumento15 paginePressure Points - Postnatal Care Planning PDFNoraNessuna valutazione finora
- Nursing ManagerDocumento30 pagineNursing ManagerNoraNessuna valutazione finora
- Orientation ListDocumento1 paginaOrientation ListNoraNessuna valutazione finora
- End of Life Care BrochureDocumento2 pagineEnd of Life Care BrochureNoraNessuna valutazione finora
- BSSDocumento4 pagineBSSNoraNessuna valutazione finora
- Kwawu Foster Kwesi - Breast Cancer, Knowledge, Attitudes and Perception Amongs Female Soldiers of The Ghana Armed Forces in The Greater Accra Region - 2009 PDFDocumento93 pagineKwawu Foster Kwesi - Breast Cancer, Knowledge, Attitudes and Perception Amongs Female Soldiers of The Ghana Armed Forces in The Greater Accra Region - 2009 PDFNoraNessuna valutazione finora
- Didik UPSR 2017 TARIKH 9.1.2017 - 1079367617 PDFDocumento15 pagineDidik UPSR 2017 TARIKH 9.1.2017 - 1079367617 PDFPencil Box100% (2)
- Vaccination in Pregnancy PDFDocumento7 pagineVaccination in Pregnancy PDFNoraNessuna valutazione finora
- Active Labor Duration and Dilation Rates Among Low Risk Nulliparous Women With Spontaneous Labor Onset A Systematic Review 2010 Journal of MidwiferyDocumento11 pagineActive Labor Duration and Dilation Rates Among Low Risk Nulliparous Women With Spontaneous Labor Onset A Systematic Review 2010 Journal of MidwiferyNoraNessuna valutazione finora
- Prenatal Care by Connie Sussan AustenDocumento31 paginePrenatal Care by Connie Sussan AustenNoraNessuna valutazione finora
- The Effect of A Training Program During Pregnancy On The Attitude and Intention of NulliparousDocumento8 pagineThe Effect of A Training Program During Pregnancy On The Attitude and Intention of NulliparousNoraNessuna valutazione finora
- Hydatidiform MoleDocumento2 pagineHydatidiform MoleIrfan HardiNessuna valutazione finora
- IUGRDocumento10 pagineIUGRAiman ArifinNessuna valutazione finora
- Childbirth TechniquesDocumento9 pagineChildbirth TechniquesMajoy Bodollo100% (1)
- The Role of Arbudahara Taila Uttarbasti in Tubal Blockage InfertilityDocumento4 pagineThe Role of Arbudahara Taila Uttarbasti in Tubal Blockage InfertilityResearch ParkNessuna valutazione finora
- Ectopic PregDocumento6 pagineEctopic PregYwagar Ywagar0% (1)
- Pelvic Inflammatory Disease-SCIENCEDocumento7 paginePelvic Inflammatory Disease-SCIENCELeanne Marie Paredes TanNessuna valutazione finora
- A Journal Report of Receipt of Mrna Covid-19 Vaccines and Risk of Spontaneous AbortionDocumento11 pagineA Journal Report of Receipt of Mrna Covid-19 Vaccines and Risk of Spontaneous AbortionNica Joy DesquitadoNessuna valutazione finora
- Related Teenshealth Links: Health Problems SeriesDocumento13 pagineRelated Teenshealth Links: Health Problems SeriesMario BadayosNessuna valutazione finora
- Allarey v. Dela Cruz20220504-11-Xjvae6Documento21 pagineAllarey v. Dela Cruz20220504-11-Xjvae6Trea CheryNessuna valutazione finora
- Introduction About SelfDocumento27 pagineIntroduction About SelfsimonjosanNessuna valutazione finora
- Davis v. Sharp ComplaintDocumento30 pagineDavis v. Sharp ComplaintWashington Free BeaconNessuna valutazione finora
- Ultrasound-Why, When, What Is FoundDocumento15 pagineUltrasound-Why, When, What Is FoundDyAnna Williams GordonNessuna valutazione finora
- Gynecological Exam: Preparation For Your ExamDocumento2 pagineGynecological Exam: Preparation For Your ExamLotfyAdelNessuna valutazione finora
- Anatomy For Beginners - Reproduction WorksheetDocumento4 pagineAnatomy For Beginners - Reproduction WorksheetJames Dauray100% (1)
- Late Preterm InfantsDocumento26 pagineLate Preterm InfantsThaíssa CasagrandeNessuna valutazione finora
- Review Questions On MCHNDocumento42 pagineReview Questions On MCHNprokuno100% (30)
- 5 - Care of The Mother and The FetusDocumento36 pagine5 - Care of The Mother and The FetusMa Nelia P MagsinoNessuna valutazione finora
- Script Roleplay KonselingDocumento4 pagineScript Roleplay KonselingVella MerytaNessuna valutazione finora
- National Aids Control ProgrammeDocumento25 pagineNational Aids Control ProgrammeSanket TelangNessuna valutazione finora
- Teaching Sex Education in Schools in Bangladesh A Perception Study.Documento19 pagineTeaching Sex Education in Schools in Bangladesh A Perception Study.Ezharul Islam UdoyNessuna valutazione finora
- Low Amniotic Fluid LevelsDocumento2 pagineLow Amniotic Fluid LevelspramaNessuna valutazione finora
- Finalized Estrogens and Anti-Estrogens 2023 Duhs DMC 4th Yr ReproDocumento30 pagineFinalized Estrogens and Anti-Estrogens 2023 Duhs DMC 4th Yr ReprosyedsuhailalishahNessuna valutazione finora
- NCM 237-Course-OutlineDocumento2 pagineNCM 237-Course-OutlineKhibul LimNessuna valutazione finora
- Department of Education: Learning Activity Sheet in Science 6Documento4 pagineDepartment of Education: Learning Activity Sheet in Science 6Tampok ES (Region III - Bulacan)Nessuna valutazione finora
- Back Massage Menggunakan Clary Sage (Salvia Sclarea) Esensial Oil Dan Senam Nifas Terhadap Percepatan Involusi Uteri Post PartumDocumento7 pagineBack Massage Menggunakan Clary Sage (Salvia Sclarea) Esensial Oil Dan Senam Nifas Terhadap Percepatan Involusi Uteri Post PartumDina AryaniNessuna valutazione finora
- Abortion: Ina S. Irabon, MD, Fpogs, FPSRM, Fpsge Obstetrics and Gynecology Reproductive Endocrinology and InfertilityDocumento25 pagineAbortion: Ina S. Irabon, MD, Fpogs, FPSRM, Fpsge Obstetrics and Gynecology Reproductive Endocrinology and InfertilityBrainy GamerARNessuna valutazione finora
- Sexual Reproduction in Humans CLASS 10Documento5 pagineSexual Reproduction in Humans CLASS 10shallowNessuna valutazione finora
- Obstetric History Taking OSCE GuideDocumento17 pagineObstetric History Taking OSCE GuideSYDNIKA AIRA CARBONILLANessuna valutazione finora