Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Epidemiology Consequences of FOAD
Caricato da
Muljadi HartonoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Epidemiology Consequences of FOAD
Caricato da
Muljadi HartonoCopyright:
Formati disponibili
294_N01-162 8/4/2002 3:35 pm Page 294
(Black plate)
International Epidemiological Association 2002
Printed in Great Britain
International Journal of Epidemiology 2002;31:294299
REVIEWS
Epidemiological challenges in studying the
fetal origins of adult chronic disease
Matthew W Gillman
Keywords
Fetal origins of adult disease, lifecourse, socioeconomic status, fetal growth, geneenvironment interaction, nutrition, epidemiological study design, fetal programming
Accepted
23 October 2001
The relatively new research field of the fetal origins of adult
disease has matured greatly in the past decade. Recent systematic overviews provide strong evidence that robust inverse
epidemiological associations exist between birthweight and later
blood pressure/hypertension1 and glucose intolerance/type 2
diabetes.2 Consistent associations are also evident for the inverse associations of birthweight with coronary heart disease
incidence and mortality.3,4 Studies with high follow-up rates
and adjustment for social and economic variables have to a large
extent mitigated earlier criticisms that observed associations
were highly subject to confounding and selection bias.5 Many
questions remain, however, about the contributing roles of
postnatal growth and development, underlying biological mechanisms, and the importance of the epidemiological findings to
public health. This review outlines current challengesstated
in the form of propositionsthat epidemiologists in this field
currently face.
1. The Lifecourse Approach Helps Put
Fetal Influences into Perspective
The lifecourse approach to chronic disease posits that fetal life
is one important period of development, but not the only one,
in determining susceptibility to adult chronic disease.6 Many
studies have now shown that associations of birth size with later
cardiovascular outcomes are modified by body mass index in
adulthood or, indeed, in childhood.7,8 The highest risk is typically among adults who were born small and become overweight
during childhood or adulthood. Examples of outcomes that fit
this profile include insulin resistance in Indian 8-year-old boys
and girls,9 blood pressure levels among 50-year-old Swedish
men,10 and incidence of coronary heart disease among middle
to older age Welsh men.4 In another example, body mass index
at age 11 appeared to modify the association of ponderal index
at birth with adult coronary disease risk in Finnish males.7
From this observed phenomenon some have inferred that
that postnatal catch up growth modifies intrauterine influences.
There are two problems with this inference. First, most studies
Department of Ambulatory Care and Prevention, Harvard Medical School and
Harvard Pilgrim Health Care, and the Department of Nutrition, Harvard
School of Public Health, Boston, MA, USA.
to date include only two weight pointsone at birth and one
later in life. Without a third, intermediate, point, it is difficult to
distinguish whether the findings represent an interaction
between fetal and postnatal exposures or merely some facets of
postnatal growth itself.11 Some recent studies, however, have
had multiple postnatal measures of height and weight. Overall
they have suggested that both intrauterine and postnatal
growth are important, but it is not clear exactly which periods
are important or even whether increased or decreased postnatal
growth is harmful. For example, in a Finnish cohort, adult
hypertension was associated with both lower birthweight and
accelerated growth in the first 7 years of life.12 In contrast, in a
small group of Chinese adults, both lower ponderal index
at birth and a decrease in ponderal index from 6 to 18 months of
life were related to increased systolic blood pressure level at age
30 years.13 Moreover, in two recently reported studies from the
UK, catch up growth in the first 6 months of life was not clearly
related to young adult blood pressure at all, although birthweight was.14,15 In another study, growth patterns exemplified
by lower birthweight followed by reduced growth until age 1
seemed to confer the highest risk for ischaemic heart disease
later in life, but the analysis was confined to men.16 These disparate results call for additional serial growth data to determine
which periods of growth contribute most to the observed interactions between fetal and postnatal size in determining health
outcomes.
A second issue is that catch up growth traditionally refers to
the first 612 months after birth, not later growth. The standard
interpretation is that catch up growth represents realignment of
ones genetic growth potential after intrauterine growth restriction. One advantage of this interpretation is that it allows for
fetal growth restriction at any birthweighteven large fetuses
can be growth restricted relative to their genetic potentialthus
obviating the need for arbitrary definitions such as small for
gestational age. This distinction is important in the fetal origins
of adult disease, since observed associations of birthweight with
later outcomes generally span the entire birthweight spectrum,
not just at the low birthweight end. The major problems,
however, are in the measurement of catch up growth. Some
investigators resort to a post hoc, empirical definition, using the
observed infant growth patterns relative to birthweight.17 A
second possibility is that mid-parental height gives a good
294
294_N01-162 8/4/2002 3:35 pm Page 295
(Black plate)
CHALLENGES RELATING TO FETAL PROGRAMMING
estimate of the childs growth potential, but usually for height,
not relative weight, and the estimation is better after 2 years of
age than in infancy. Third, while needing confirmation, recent
data raise the possibility that levels of maternal insulin-like
growth factor I during pregnancy may reflect fetal growth restriction.18 A final issue with measuring catch up growth is that even
in the first 6 months of life, postnatal environmental factors can
also influence growth. For example, while having been breastfed
seems to protect against obesity later in childhood,19 breastfed
infants in developed countries generally exhibit higher body mass
during the first year of life that formula-fed infants.20
In sum, there are three possible general inferences from
observations that the highest risk for cardiovascular outcomes
lies among individuals both born small and achieving high body
size later in life. The first is that fast postnatal growth itself
increases risk. The second is that factors related to fetal growth
restriction increase risk and the third involves an interaction
between the two. Thus studies of the fetal origins of adult
disease will benefit from having multiple measures of height
and weight through the lifecourse, to distinguish prenatal influences from influences occurring at various points in infancy,
childhood, and later. They will also benefit from a clear definition
of catch up growth and a non-circular method of measuring it.
In the meantime, authors should clarify what periods of life
their measurements cover, preferably reserving the term catch
up growth for its traditional meaning of realignment to genetic
potential during infancy.
2. Adjustment for Achieved Body Mass
Index, Despite Being Controversial,
Is Often Helpful
While the points above concern effect modification by achieved
body size, this section addresses adjustment for it. Some epidemiological associations, for example the inverse relationship
of birthweight with blood pressure, appear strongeror in some
studies, appear onlyafter statistical adjustment for adult (or
childhood) body mass index.21,22 How, or even whether, to
make such adjustments is controversial. Some of the controversy seems to emanate from the fact that epidemiologists from
a variety of fieldsperinatal, cardiovascular, paediatricwith
different lexicons, are converging on the same research topics.
Also, perinatal epidemiologists have traditionally been concerned
with avoiding low birthweight. In fact, increasing birthweight
at this end of the spectrum, primarily by avoiding preterm
births,23 would reduce neonatal and infant adverse outcomes.
From this perspective, birthweight is an entity in and of itself,
with aetiological significance. In contrast, in the field of fetal
origins of adult disease, birthweight is not a monolith. Not all
determinants of birthweight are salient, so increasing birthweight is not necessarily helpful. Further, this new paradigm is
concerned with the entire spectrum of birthweight, rather than
just the lower parts of the distribution. Adjusting for later body
size is therefore appropriate; it can elucidate underlying aetiological pathways.
Figure 1 demonstrates this argument, using the example of
blood pressure as an outcome. If it is true that (1) birthweight is
positively related to later body mass index,24 (2) birthweight
is inversely related to later blood pressurethe association of
295
Figure 1 Why adjustment for attained body mass index is warranted.
See text (Challenge No. 2) for explanation. BMI = body mass index;
BP = blood pressure; + indicates direct association; indicates inverse
association
primary interest, and (3) body mass index is positively related
to contemporaneous blood pressure (a well-known relationship), then the prenatal factors explaining pathways #1 and #2
(labelled Factors A and Factors B, respectively) are almost
surely different. Adjusting for body mass index could elucidate
some of the factors underlying the inverse birthweight-blood
pressure association, and is thus potentially useful.
One empirical example that serves to illustrate this point is
the relationship between birthweight and development of type
2 diabetes. Unadjusted for attained body mass index, the shape
of the relationship is a U or reverse J, with increased risk at
both ends of the birthweight spectrum.25 But this observation
obscures the fact that there are probably two underlying mechanisms. At high birthweights, maternal gestational diabetes is
causing obesity and excess diabetes risk in the offspring. Adjustment for attained body mass, however, reveals an inverse and
linear association across the birthweight spectrum, reflecting
a second pathway with reduced risk at higher birthweights,
a pattern sometimes attributed to the influence of a thrifty
phenotype.26
3. Social and Economic Factors Are Not
Just Confounders
Many decades span the time from birth until cardiovascular
diseases declare themselves. Most of these diseases are related
to both lower birthweight and poorer socioeconomic circumstances in adulthood. Thus controlling for these circumstances
seems necessary to isolate prenatal influences. On the other
hand, for some social class is stable across generations. Under
these conditions, the same socioeconomic factors that affect
postnatal life may affect prenatal life as well, and could thus
determine the putative exposures under study. In this view, the
social and economic factors are part of the causal pathway, both
before and after birth.
For others, social circumstances change over time. Depending
on the disorder, the place, and the era, societal factors can have
impact in different points in the lifespan. In the UK in the
294_N01-162 8/4/2002 3:35 pm Page 296
296
(Black plate)
INTERNATIONAL JOURNAL OF EPIDEMIOLOGY
late 20th century, for example, low childhood social class is
more strongly associated with risk of stroke than is adult social
class. For coronary heart disease, however, childhood and adulthood social factors appear to play equal roles.27
The challenges for future analyses are to consider the explanatory as well as confounding effects of social and economic
factors; and to take into account changes in these factors across
the lifespan. As these effects are being clarified, it will be
important to assess how such societal factors affect physiological
mechanisms underlying the epidemiological phenomena. Some
factors may operate through their associations with behavioural
factors. For example, maternal diet may differ by social class.
In contrast, other societal factors may directly affect biological
responses; for example, accumulated stress may influence the
hypothalamic-pituitary-adrenal axis independent of lifestyle
choices. Alternatively, the two kinds of pathways may actually
work in concert with each other. In rodent models, stress during
gestation causes reduced levels of maternal licking/grooming of
her offspring, which are in turn related to levels of offspring
stress reactivity through effects on systems that regulate activity
of corticotropin-releasing hormone.28
4. Fetal Growth and Size at Birth Are Not
Synonymous
In studies that can separate length of gestation from overall
birthweight, most observed associations between birthweight
and later cardiovascular outcomes are not due to length of
gestation.29 Epidemiologists have called the remaining factor in
birthweight fetal growth. However, fetal size at birth, adjusted
for length of gestation, is only a snapshot of the trajectory of
fetal growth throughout gestation.
Some, but clearly not all, epidemiological studies have found
stronger associations with later outcomes for thinness or shortness at birth, or even abdominal or other body circumferences,
rather than birthweight itself. Authors have hypothesized
trimester-specific perturbations of growth of the fetus or
particular organs to explain these phenomena.30 Whether such
hypotheses have merit cannot be fully addressed with crude
measures of fetal size at birth, considering not only the measurement error inherent in length and circumference measures,
but also the non-specificity of even accurate measures at birth
for determining fetal growth trajectories.31,32
Ongoing animal studies of fetal growth will continue to inform the epidemiology. In addition, one way studies of humans
can be refined is to take advantage of serial ultrasound measures
to measure fetal growth parameters throughout pregnancy. For
example, preliminary data from one study suggested that femur
length at 24 weeks was more strongly inversely associated
with blood pressure at age 6 years than were either head or
abdominal circumferences.33 In that study, however, changes in
ultrasound measurements from 18 to 38 weeks were not clearly
related to the outcome.
In addition, the dearth of data linking reduced gestational
age at birth with adult health outcomes is chiefly a function of
the historical data available to date, not necessarily because the
link is absent. When most of the participants in the currently
published long-term studies were born, relatively few preterm
infants survived. To what extent gestational age predicts adult
outcomes is an unresolved question, but an important one. In
general, determinants of preterm birth and fetal growth are not
the same.34
5. Some Determinants of Fetal Growth
Will Be Red Herrings
While the observed epidemiological associations appear to implicate fetal growth as a major factor, overall fetal size at birth is
an amalgam of many determinants. Some of these determinants
may be related to susceptibility to adult disease, and others may
not. Conversely, some prenatal determinants of adult outcomes
may not be related to fetal growth. While investigations of
fetal growth are likely to reveal some underlying processes, the
need exists to investigate more directly prenatal determinants of
postnatal outcomes, irrespective of effects on birthweight.
One example of size at birth potentially being a good proxy
for an underlying causal pathway derives from the hypothesis
that a congenital nephron deficit underlies predisposition to
hypertension in adult life.35 A recent study shows that kidney
volume is smaller in adults who were thinner at birth, even
after adjustment for current body size.36 In contrast, a potential
example of a prenatal exposure causing postnatal disease without effects on birthweight is the newly described association of
paracetamol use by mothers in late pregnancy and risk of asthma
in their preschool age offspring.37 Maternal smoking during
pregnancy is a good example of a prenatal exposure whose
deleterious effect on fetal growth is well-known but whose
influence on long-term offspring health is uncertain. Perhaps
investigation of the seemingly paradoxical protective effect of
smoking against the development of pre-eclampsia38 will offer
insights.
6. Both Genes and Environment Are
Important. Even Distinction Between
the Two Is Difficult
Many critics of the fetal origins hypothesis have taken to task
the epidemiological studies for not accounting for possible genetic
explanations. Although rare genetic mutations do not explain
the findings of population-based studies, they may provide a
paradigm for understanding. For example, a rare mutation in
the glucokinase gene causes drastically reduced birthweight and
offspring insulin resistance.39 No analogous common allelic
variation has yet been discovered, but it is possible that some
exist to help explain the observed phenomena.
In addition, maternal, paternal, and fetal genes may all play
roles. While inherited fetal gene expression can underlie susceptibility to disease, it is also likely that the maternal genome
codes for substances that affect the fetal environment. As such,
what is genetic for the mother is environmental for the fetus.
One example of this principle is that it appears that the
maternal thermolabile variant of methylenetetrahydrofolate
reductase may be associated with the risk of neural tube defects
in the offspring, even in the face of a normal fetal genotype.40
This consideration also highlights the close relationship
between genes and environment and the need to examine interactions between them. Not only can maternal gene expression
alter the fetal environment, but it is also possible that the
maternal gestational environment can affect fetal gene expression.
294_N01-162 8/4/2002 3:35 pm Page 297
(Black plate)
CHALLENGES RELATING TO FETAL PROGRAMMING
For example, in a mouse model, feeding the mother foods with
different quantities of methyl donors can alter offspring coat
colour through modification of gene expression.41,42 More
substantial progress in humans will occur when investigators
can assess interactions among environmental factors and
candidate genes as their identities become available. Ultimately,
there will be probably be less distinction between genes and
environment than most researchers currently consider.
7. Maternal Nutrition Does Not Equal
Fetal Nutrition
Scientists and the public have been confused by statements
about undernutrition explaining the observed epidemiological
phenomena. Except at the extremes of intake, maternal energy
and macronutrient intake have relatively little impact on
birthweight. In addition, little or no firm evidence suggests that
maternal intake of total energy or macronutrients during pregnancy, or maternal body composition, have substantial impact
on offspring risk of chronic disease. In fact, some empirical
results seem diametrically opposed to each other. For example,
results of one abstract presented at the 2001 World Congress on
the fetal origins of adult disease suggested that a high dietary
protein/carbohydrate ratio in the third trimester was associated
with lower offspring blood pressure, whereas the authors of the
next presentation observed higher blood pressures among
offspring of mothers consuming a relatively high protein, low
carbohydrate diet in late pregnancy.43,44
In contrast, what is often termed fetal nutrition is likely to
be vital. The oxygen and nutrients that support fetal growth and
development rely on the entire nutrient supply line, beginning
with maternal consumption and body size, but extending to
uterine perfusion, placental function, and fetal metabolism.
Interruptions of the supply line at any point could result in programming the fetus for future risk of cardiovascular disease.31
Some of the confusion arises because a common animal model
for interrupting the supply line is to alter maternal gestational
intake.45 Interrupting the supply line at other points, say by
underperfusing the placenta, can have analogous effects. One
should use the animal experimental data only as models, as
they are intended.
The placenta is likely to be a key to understanding associations
of fetal growth with adult health, owing to its inherent endocrine function as well as its metabolic and transfer capacities.31
The lack of good animal models for placentation has hampered
understanding of the pathways by which the fetus receives
nutrients and oxygen from the mother, and what processes alter
these pathways. Possible ways to study placental function
in population-based studies include placental morphological
pathology, as well as using specimens of placenta, maternal
prenatal blood or other biological specimens, and umbilical cord
blood to measure markers of altered blood flow, endocrine and
transport characteristics, or activity of specific enzymes. These
biological specimens can also be used to investigate other mechanisms underlying the observed epidemiological findings, including maternal and fetal endocrine pathways,46 inflammatory
and immune function,47 and changes in the central and peripheral nervous system,48,49 among others.
Still, researchers should not dismiss the possibility that
maternal dietary intake could be an important supply line
297
component in humans. In investigating maternal dietary
impact, investigators should concentrate on pathways that could
involve specific foods and micronutrients in addition to energy
and macronutrient intake, which appear to be relatively
unimportant on their own. For example, recent data from 27
pregnant women suggest that while overall gestational protein
intake is unimportant, relative partitioning from protein
oxidation to deposition, perhaps related to micronutrient
factors, is associated with birthweight.50 Relevant examples
from perinatal epidemiology include that fatty acids of the
n-3 family prolong gestation and reduce the incidence of preterm birth, and inadequate folic acid intake causes neural
tube defects.51,52 Future research may reveal that fatty acids,
folate, or other nutrients may also be involved in programming
of chronic disease risk.
8. New Epidemiological Study Designs
Will Help
Many of the extant epidemiological findings have emanated from
historical cohort studies, taking great advantage of serendipitous
clinically recorded perinatal variables. The next generation of
studies, however, should overcome the limitations of the earlier
studies. These limitations include lack of research quality measures, limited information on covarying factors, and absence of
biological specimens. Although no one study can address all
methodological issues, three types of studies will be especially
valuable in the coming years:
1. New prospective studies of pregnant women (including ones
that even start pre-conceptionally) that follow their offspring
over time, collecting biological samples to explore mechanisms,
as well as research quality epidemiological data.53 These have
the advantage of collecting detailed prospective data and examining childhood cardiovascular risk factors and diseases such as
asthma, but must wait decades for adult disease outcomes to
occur.
2. Follow-up of adult cohorts in which biological samples and
prospectively collected epidemiological data are available from
the past.54 These have the advantage of research quality data
and emerging disease outcomes, but may lack important exposure or covariate information, such as maternal diet during
pregnancy.
3. Follow-up into childhood or adulthood of randomized controlled trials conducted during pregnancy.55 These have the
advantage of isolating an environmental insult during pregnancy and so can come close to proving that programming
occurs. However, this type of study is limited to examining a
single or limited number of exposures.
9. To Make Policy Recommendations
Now Regarding Fetal Programming Is
Dangerous
Strong evidence exists for programming in humans. First is the
robust epidemiological findings of associations between size
at birth and later health outcomes. Second is the experimental
animal evidence that in utero environmental insults produce
lifelong alterations in metabolism, physiology, and pathology,
294_N01-162 8/4/2002 3:35 pm Page 298
298
(Black plate)
INTERNATIONAL JOURNAL OF EPIDEMIOLOGY
whether or not the exact perturbations have analogy in human
systems.
One area of great importance is implications for developing
countries undergoing the epidemiological transition from infectious disease to chronic disease, chiefly cardiovascular disease,
as well as the nutrition transition from an active, low-calorie
lifestyle to a sedentary, high-calorie lifestyle.56 Available data
indicate that a lower birthweight combined with higher attained
body mass confers the highest risk for cardiovascular disease.
Successive generations of individuals in developing countries
are likely to have ever larger proportions with that high-risk
profile. Efforts to prevent development of obesity in areas
undergoing the epidemiological and nutritional transitions are
paramount.
It is premature to make policy recommendations regarding
fetal programming. Since birthweight is only a marker for underlying aetiological pathways, the true aetiological factors are
unknown. Until they are identified, it is impossible to calculate
attributable risks or design interventions to modify them. Interventions to increase birthweight per se would be at best inefficient, probably ineffective, and potentially harmful. Ultimately,
the promise of the fetal origins paradigm is that attending to the
health of women of reproductive age will have profound impact
on the well-being of their progeny.
4 Frankel S, Elwood P, Sweetnam P, Yarnell J, Davey Smith G.
Birthweight, body-mass index in middle age, and incident coronary
heart disease. Lancet 1996;348:147880.
5 Gillman MW, Rich-Edwards J. The fetal origins of adult disease: from
sceptic to convert. Pediatr Perinat Epidemiol 2000;14:19293.
6 Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease
Epidemiology. New York: Oxford University Press, 1997.
7 Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker
DJP. Catch-up growth in childhood and death from coronary heart
disease: a longitudinal study. BMJ 1999;318:42731.
8 Whincup PH, Bredow M, Payne F, Sadler S, Golding J. Size at birth
and blood pressure at 3 years of age. The Avon Longitudinal Study
of Pregnancy and Childhood (ALSPAC). Am J Epidemiol 1999;149:
73039.
9 Bavdekar A, Yajnik CS, Fall CHD et al. The insulin resistance
syndrome in eight-year-old Indian children; small at birth, big at eight
years or both? Diabetes 1999;48:242229.
10 Leon DA, Koupilova I, Lithell HO et al. Failure to realise growth
potential in utero and adult obesity in relation to blood pressure in 50
year old Swedish men. BMJ 1996;312:40106.
11 Lucas A, Fewtrell MS, Cole TJ. Fetal origins of adult diseasethe
hypothesis revisited. BMJ 1999;319:24549.
12 Eriksson J, Forsen T, Tuomilehto J, Osmond C, Barker D. Fetal and
childhood growth and hypertension in adult life. Hypertension 2000;
36:79094.
13 Cheung YB, Low L, Osmond C, Barker D, Karlberg J. Fetal growth
Acknowledgements
Many of the ideas expressed here grew out of a Harvard Medical
School conference, Fetal Origins of Adult Cardiovascular
Disease: New Directions, which I chaired in November 1999.
The contributions of the 48 attendees of that conference, which
included epidemiologists, biomedical scientists, and health policy
researchers, were instrumental in the genesis of this paper. The
list of attendees and the conference agenda are available upon
request. I also acknowledge the helpful comments of Janet
Rich-Edwards, conference co-chair, on a draft of this manuscript. Conference funding was supplied by Maternal and Child
Health Bureau of Health Resources and Services Administration
(6-MCJ-000102451), Department of Ambulatory Care and
Prevention at Harvard Medical School/Harvard Pilgrim Health
Care, SmithKline Beecham Consumer Healthcare, Harvard Center
for Childrens Health, Department of Nutrition at Harvard School
of Public Health, Council on Epidemiology and Prevention of
the American Heart Association, Mead Johnson Nutritionals,
The Procter and Gamble Co. This work was also supported by
grants from the US National Institutes of Health (HD 34568,
HL 64925, HL 68041) and by Harvard Medical School and the
Harvard Pilgrim Health Care Foundation.
References
and early postnatal growth are related to blood pressure in adults.
Hypertension 2000;36:795800.
14 McCarthy A, Ben-Schlomo Y, Elwood P, Davies D, Davey Smith G.
The relationship between birth weight, catch up growth in infancy
and blood pressure in young adulthood. Pediatr Res 2001;50:45A.
15 Law CM, Shiell AW, Syddall HE. Growth in utero, infancy and
childhood: which influences adult blood pressure? Pediatr Res
2001;50:11A.
16 Eriksson JG, Forsen T, Tuomilehto J, Osmond C, Barker DJP. Early
growth and coronary heart disease in later life: longitudinal study.
BMJ 2001;322:94953.
17 Dunger DB, Ong KKL, Huxtable SJ et al. Association of the INS VNTR
with size at birth. Circulation 1998;96:223338.
18 Holmes RP, Holly JM, Soothill PW. A prospective study of maternal
serum insulin-like growth factor-I in pregnancies with appropriately
grown or growth restricted fetuses. Br J Obstet Gynaecol 1998;105:
127378.
19 Gillman MW, Rifas-Shiman SL, Camargo CA Jr et al. Risk of
overweight among adolescents who had been breast fed as infants.
JAMA 2001;285:246167.
20 Dewey KG, Peerson JM, Brown KB et al. Growth of breast-fed infants
deviates from current reference data: a pooled analysis of US,
Canadian, and European data sets. Pediatrics 1995;96:495503.
21 Leon DA. Fetal growth and later disease: epidemiological evidence
from Swedish cohorts. In: OBrien PMS, Wheeler T, Barker DJP (eds).
Fetal Programming. Influences on Development and Disease in Later Life.
London: RCOG Press, 1999, pp.1229.
1 Huxley RR, Shiell AW, Law CM. The role of size at birth and postnatal
22 Whincup PH. Fetal origins of cardiovascular risk: evidence from
catch-up growth in determining systolic blood pressure: a systematic
review of the literature. J Hypertens 2000;18:81531.
studies in children. In: OBrien PMS, Wheeler T, Barker DJP (eds).
Fetal Programming. Influences on Development and Disease in Later Life.
London: RCOG Press, 1999, pp.3040.
2 Law CM, Fall CHD, Newsome CA, Shiell AW, Phillips DIW, Shier R. Is
birthweight related to glucose and insulin metabolism?a systematic
review. Pediatr Res 2001;50:60A.
23 Wilcox AJ. On the importanceand the unimportanceof birth
3 Rich-Edwards JW, Stampfer MJ, Manson JE et al. Birthweight and
24 Parsons TJ, Powers C, Logan S, Summerbell CD. Childhood predictors
the risk of cardiovascular disease in adult women. BMJ 1997;
315:396400.
of adult obesity: a systematic review. Int J Obes Relat Metab Disord
1999;23:S1107.
weight. Int J Epidemiol 2001;30:123341.
294_N01-162 8/4/2002 3:35 pm Page 299
(Black plate)
CHALLENGES RELATING TO FETAL PROGRAMMING
25 Rich-Edwards JW, Colditz GA, Stampfer MJ et al. Birthweight and the
risk for type 2 diabetes mellitus in adult women. Ann Intern Med
1999;130:27884.
299
42 Wolff GL, Kodell RL, Moore SR, Cooney CA. Maternal epigenetics and
methyl supplements affect agouti gene expression in Avy/a mice.
FASEB J 1998;12:94957.
26 Hales CN, Barker DJP. Type 2 (non-insulin-depedent) diabetes
43 Haselden S, Shiell AW, Campbell-Brown M, Robinson S, Godfrey KM,
mellitus: the thrifty phenotype hypothesis. Diabetologia 1992;35:
595601.
Barker DJP. A high meat, low carbohydrate diet in pregnancy; relation
to the offsprings blood pressure and glucose-insulin metabolism at
age 30. Pediatr Res 2001;50:24A.
27 Davey Smith G, Hart C, Blane D, Hole D. Adverse socioeconomic
conditions in childhood and cause specific adult mortality: prospective
observational study. BMJ 1998;316:163135.
28 Francis D, Diorio J, Liu D, Meaney MJ. Nongenomic transmission
across generations in maternal behavior and stress responses in the
rat. Science 1999;286:115558.
29 Leon DA, Lithell HO, Vagero D et al. Reduced fetal growth rate and
increased risk of death from ischemic heart disease: cohort study of
15 000 Swedish men and women born 191529. BMJ 1998;317:
24145.
30 Barker DJP. Mothers, Babies, and Disease in Later Life. 2nd Edn. London:
Harcourt Brace & Co. Ltd, 1998.
31 Harding JE. The nutritional basis of the fetal origins of adult disease.
Int J Epidemiol 2001;30:1523.
32 Kramer MS, McLean FH, Olivier M, Willis DM, Usher RH. Body
proportionality and head and length sparing in growth-retarded
neonates: a critical appraisal. Pediatrics 1989;84:71723.
33 Blake KV, Gurrin LC, Stanley FJ, Landau LI, Beilin LJ, Newnham JP.
Intrauterine growth and subsequent blood pressure in childhood.
Pediatr Res 2001;50:42A.
34 Kramer MS. Determinants of low birth weight: methodological assess-
ment and meta-analysis. Bull World Health Organ 1987;65:
663737.
44 Roseboom TJ, van der Meulen JH, van Montfrans GA et al. Maternal
nutrition during gestation and blood pressure in later life. J Hypertens
2001;19:2934.
45 Jackson AA. Maternal and fetal demands for nutrients: significance of
protein restriction. In: OBrien PMS, Wheeler T, Barker DJP (eds).
Fetal Programming. Influences on Development and Disease in Later Life.
London: RCOG Press, 1999, pp.24670.
46 Welberg LA, Seckl JR. Prenatal stress, glucocorticoids and the
programming of the brain. J Neuroendocrinol 2001;13:11328.
47 Prescott SL, Macaubas C, Smallacombe T, Holt BJ, Sly PD, Holt PG.
Development of allergen-specific T-cell memory in atopic and normal
children. Lancet 1999;353:118788.
48 Plagemann A, Harder T, Melchior K, Rake A, Rohde W, Dorner G.
Elevation of hypothalamic neuropeptide Y-neurons in adult offspring
of diabetic mother rats. NeuroReport 1999;10:321116.
49 Young JB, Morrison SF. Effects of fetal and neonatal environment
on sympathetic nervous system development. Diabetes Care 1998;21:
B15660.
50 Duggleby SL, Jackson AA. Maternal amino acid oxidation during
pregnancy and birth weight. Pediatr Res 2001;50:3A.
51 Olsen SF, Secher NJ, Tabor A, Weber T, Walker JJ, Gluud C.
cause of adult hypertension and progressive renal injury? Curr Opin
Nephrol Hypertens 1993;2:69195.
Randomised clinical trials of fish oil supplementation in high risk
pregnancies. Fish Oil Trials in Pregnancy (FOTIP) Team. Br J Obstet
Gynaecol 2000;107:38295.
36 Singh GR, White AV, Spencer J, Hoy WE. Intrauterine growth
52 MRC Vitamin Study Research Group. Prevention of neural tube
influences kidney size and function: the renal dimension of the fetal
origins hypothesis. Pediatr Res 2001;50:30A.
defects: results of the Medical Research Council Vitamin Study. Lancet
1991;338:13137.
37 Shaheen SO, Newson RB, Sherriff AM et al. Analgesic use in
53 Rich-Edwards J, Krieger N, Majzoub J, Zierler S, Lieberman E,
pregnancy and atopic disease in early childhood. Pediatr Res 2001;
50:5A.
Gillman M. Maternal experiences of racism and violence as predictors
of preterm birth: rationale and study design. Paediatr Perinat Epidemiol
2001;15:12435.
35 Brenner BM, Chertow GM. Congenital oligonephropathy: an inborn
38 Xiong X, Wang FL, Davidge ST et al. Maternal smoking and
preeclampsia. J Reprod Med 2000;45:72732.
39 Hattersley AT, Tooke JE. The fetal insulin hypothesis: an alternative
explanation of the association of low birthweight with diabetes and
vascular disease. Lancet 1999;353:178992.
40 Wenstrom KD, Johanning GL, Owen J, Johnston KE, Acton S,
Tamura T. Role of amniotic fluid homocysteine level and of fetal 5,
10-methylenetetrahydrafolate reductase genotype in the etiology of
neural tube defects. Am J Med Genet 2000;90:1216.
54 Seidman LJ, Buka SL, Goldstein JM, Horton NJ, Rieder RO, Tsuang
MT. The relationship of prenatal and perinatal complications to
cognitive functioning at age 7 in the New England Cohorts of the
National Collaborative Perinatal Project. Schizophr Bull 2000;26:
30921.
55 Belizan JM, Villar J, Bergel E et al. Long term effect of calcium
supplementation during pregnancy on the blood pressure of offspring:
follow up of a randomised controlled trial. BMJ 1997;315:28185.
41 Morgan HD, Sutherland HGE, Martin DIK, Whitelaw E. Epigenetic
56 Murray CJL, Lopez AD. Alternative projections of mortality and
inheritance at the agouti locus in the mouse. Nat Genet 1999;23:
31418.
disability by cause 19902020: Global Burden of Disease Study. Lancet
1997;349:1498504.
Potrebbero piacerti anche
- Kamus Operasional KompetensiDocumento8 pagineKamus Operasional KompetensiMuljadi HartonoNessuna valutazione finora
- Hungry in A Hurry: Food For Fast Times: FALL 2012Documento4 pagineHungry in A Hurry: Food For Fast Times: FALL 2012Muljadi HartonoNessuna valutazione finora
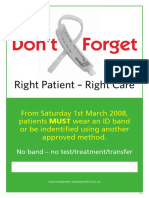
- Don't Forget: Right Patient - Right CareDocumento1 paginaDon't Forget: Right Patient - Right CareMuljadi HartonoNessuna valutazione finora
- Soal 42 Sampe 50 Bahasa InggrisDocumento2 pagineSoal 42 Sampe 50 Bahasa InggrisMuljadi HartonoNessuna valutazione finora
- Bedah Soal Grup 1Documento7 pagineBedah Soal Grup 1Muljadi HartonoNessuna valutazione finora
- Healthliteracy PDFDocumento367 pagineHealthliteracy PDFMuljadi HartonoNessuna valutazione finora
- Patient Centered Care Improvement Guide 10.10.08Documento247 paginePatient Centered Care Improvement Guide 10.10.08Muljadi HartonoNessuna valutazione finora
- Empat Pilar ServiceDocumento20 pagineEmpat Pilar ServiceMuljadi HartonoNessuna valutazione finora
- BJ Upacara AdatDocumento2 pagineBJ Upacara AdatMuljadi HartonoNessuna valutazione finora
- Fetal Origins of Adult DiseaseDocumento9 pagineFetal Origins of Adult DiseaseMuljadi HartonoNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- University of Engineering & Management, Jaipur: (A) Production (B) Quality (C) Product Planning (D) All of The AboveDocumento4 pagineUniversity of Engineering & Management, Jaipur: (A) Production (B) Quality (C) Product Planning (D) All of The AboveSupriyo BiswasNessuna valutazione finora
- A Brief History of LinuxDocumento4 pagineA Brief History of LinuxAhmedNessuna valutazione finora
- Surat Textile MillsDocumento3 pagineSurat Textile MillsShyam J VyasNessuna valutazione finora
- Cui Et Al. 2017Documento10 pagineCui Et Al. 2017Manaswini VadlamaniNessuna valutazione finora
- Fireware EssentialsDocumento499 pagineFireware EssentialsEmmanuel RodríguezNessuna valutazione finora
- Soul Winners' SecretsDocumento98 pagineSoul Winners' Secretsmichael olajideNessuna valutazione finora
- Saln 1994 FormDocumento3 pagineSaln 1994 FormJulius RarioNessuna valutazione finora
- Sycip v. CA (Sufficient Funds With The Drawee Bank)Documento15 pagineSycip v. CA (Sufficient Funds With The Drawee Bank)Arnold BagalanteNessuna valutazione finora
- Compare Visual Studio 2013 EditionsDocumento3 pagineCompare Visual Studio 2013 EditionsankurbhatiaNessuna valutazione finora
- What Can Tesla Learn From Better Place's FailureDocumento54 pagineWhat Can Tesla Learn From Better Place's Failuremail2jose_alex4293Nessuna valutazione finora
- Vocabulary Words - 20.11Documento2 pagineVocabulary Words - 20.11ravindra kumar AhirwarNessuna valutazione finora
- EMP Step 2 6 Week CalendarDocumento3 pagineEMP Step 2 6 Week CalendarN VNessuna valutazione finora
- Laws and Policies of Fertilizers SectorDocumento12 pagineLaws and Policies of Fertilizers Sectorqry01327Nessuna valutazione finora
- Effect of Innovative Leadership On Teacher's Job Satisfaction Mediated of A Supportive EnvironmentDocumento10 pagineEffect of Innovative Leadership On Teacher's Job Satisfaction Mediated of A Supportive EnvironmentAPJAET JournalNessuna valutazione finora
- Why The American Ruling Class Betrays Its Race and CivilizationDocumento39 pagineWhy The American Ruling Class Betrays Its Race and CivilizationNinthCircleOfHellNessuna valutazione finora
- AX Series Advanced Traffic Manager: Installation Guide For The AX 1030 / AX 3030Documento18 pagineAX Series Advanced Traffic Manager: Installation Guide For The AX 1030 / AX 3030stephen virmwareNessuna valutazione finora
- Contoh Rancangan Pengajaran Harian (RPH)Documento7 pagineContoh Rancangan Pengajaran Harian (RPH)Farees Ashraf Bin ZahriNessuna valutazione finora
- A Comparison of Practitioner and Student WritingDocumento28 pagineA Comparison of Practitioner and Student WritingMichael Sniper WuNessuna valutazione finora
- Complete Cocker Spaniel Guide 009 PDFDocumento119 pagineComplete Cocker Spaniel Guide 009 PDFElmo RNessuna valutazione finora
- Safe Britannia PDFDocumento2 pagineSafe Britannia PDFeden4872Nessuna valutazione finora
- ZultaniteDocumento4 pagineZultaniteAcharya BalwantNessuna valutazione finora
- Danese and Romano (2011) ModerationDocumento14 pagineDanese and Romano (2011) ModerationUmer NaseemNessuna valutazione finora
- Civil Engineering Interview QuestionsDocumento19 pagineCivil Engineering Interview QuestionsSrivardhanSrbNessuna valutazione finora
- Construction Agreement SimpleDocumento3 pagineConstruction Agreement Simpleben_23100% (4)
- Baixar Livro Draw With Jazza Creating Characters de Josiah Broo PDFDocumento5 pagineBaixar Livro Draw With Jazza Creating Characters de Josiah Broo PDFCarlos Mendoza25% (4)
- Pre-Boarding Announcement Skill Focus: ListeningDocumento5 paginePre-Boarding Announcement Skill Focus: ListeningJony SPdNessuna valutazione finora
- The Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersDocumento11 pagineThe Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersDM YazdaniNessuna valutazione finora
- Design and Experimental Performance Assessment of An Outer Rotor PM Assisted SynRM For The Electric Bike PropulsionDocumento11 pagineDesign and Experimental Performance Assessment of An Outer Rotor PM Assisted SynRM For The Electric Bike PropulsionTejas PanchalNessuna valutazione finora
- New Count The DotsDocumento1 paginaNew Count The Dotslin ee100% (1)
- The Trial of Jesus ChristDocumento10 pagineThe Trial of Jesus ChristTomaso Vialardi di Sandigliano100% (2)