Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Terrorism and Eduaction
Caricato da
esat936Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Terrorism and Eduaction
Caricato da
esat936Copyright:
Formati disponibili
JGIM
HE ALTH POLIC Y
Terrorisms Psychologic Effects and Their Implications for Primary Care Policy,
Research, and Education
David P. Eisenman, MD, MSHS,1,2 Bradley D. Stein, MD, PhD,3,4 Terri L. Tanielian, MA,3
Harold Alan Pincus, MD5,6
1
Division of General Internal Medicine and Health Services Research, Department of Medicine, UCLA, Los Angeles, Calif, USA; 2RAND
Corporation, Health Sciences Program, Santa Monica, Calif, USA; 3Mental and Behavioral Health, Center for Domestic and International
Health Security, RAND Corporation, Health Sciences Program, Santa Monica, Calif, USA; 4University of Southern California, Los Angeles,
Calif, USA; 5Department of Psychiatry, University of Pittsburgh Medical Center Senior Natural Scientist; 6RAND Corporation, Health
Sciences Program, Pittsburgh, Pa, USA.
This paper examines primary care physicians (PCP) roles in helping the
nation prepare for, respond to, and recover from the psychologic consequences of chemical, biologic, radiologic, or nuclear (CBRN) terrorism. First, we discuss the psychologic consequences of a CBRN attack
and PCPs roles in responding to these consequences. Second, we analyze these roles in light of the known barriers to delivering high-quality,
primary carebased, mental health care. Third, we offer recommendations for mitigating these barriers and preparing PCPs to respond to the
psychosocial consequences of a CBRN weapon. Importantly, our recommendations provide dual-use benefits to PCPs faced with the daily
concerns of primary care mental health, including improved linkages
and electronic connectivity with mental health, information technology,
and decision support for providers, and needed education and
research.
KEY WORDS: terrorism; bioterrorism; mental health; primary care.
DOI: 10.1111/j.1525-1497.2005.0192.x
J GEN INTERN MED 2005; 20:772776.
Q2
ince the September 11, 2001, and subsequent anthrax
attacks, substantial federal funds have been devoted to
improving the health care systems capacity to detect and respond to a chemical, biologic, radiologic, or nuclear (CBRN)
weapon attack. These events highlighted primary care physicians (PCPs) contributions to addressing the psychologic consequences of terrorism.15 After the attacks, PCPs reported a
willingness to deliver CBRN-related mental health care, especially if education, links with mental health care, and improved
reimbursement were available.5,6
PCPs should ensure that their interests are represented in
the mental health care planning for a CBRN event. Mental
health experts and disaster planners recognize that primary
care, already the major component of the de facto mental
health care system,7 will have to respond to the emotional and
behavioral consequences of the event.5,8,9 Estimates of psychologic to physical casualties range from 5 to 1 to 50 to 1 and
will likely be widespread and enduring.911 Primary care may
be a central location for triaging patients into primary care
based mental health interventions.12 Appropriate preparation
and planning by administrators, PCPs (and PCPs families) will
The authors have no conflicts of interest to declare, for this article or
this research.
Address correspondence and requests for reprints to Eisenman: The
RAND Corporation, 1776 Main Street, Santa Monica, CA 90407 (e-mail:
(David_Eisenman@rand.org).
772
likely reduce their work burden13 and the risk of stress, trauma, and burnout.14,15 Importantly, such planning for primary
mental health care after a CBRN event serves a dual-use
function as an opportunity for improving the quality of mental
health care for routine mental health problems that occur in
daily clinical care.6 A similar dual-use revamping of the public
health system is occurring with federal funds for bioterrorism
preparedness.16
The quality of primary mental health care, already hampered by barriers at the conceptual, patient, provider, and system levels,17 will face new additions to these barriers after an
attack. After discussing the psychologic consequences of a
CBRN attack and PCPs anticipated roles in response, we examine what these barriers imply for primary mental health
care. Next, we offer recommendations for mitigating these barriers and preparing PCPs to respond to the psychosocial consequences of a CBRN weapon.
PSYCHOLOGIC CONSEQUENCES AND
PCPS ROLES
A CBRN attack may lead to or exacerbate depression,18 anxiety
disorders,19 posttraumatic stress disorder (PTSD),20 somatization disorders, and substance use21 even among persons
distant from the attack.2,2228 The triaging of distressed patients29 may allow PCPs to counsel patients to help them manage their anxieties about exposure, infection, contagion,
illness severity, and access to therapeutic and prophylactic
measures. Grief counseling, already variably performed by
PCPs,30 may also be needed for individuals who have lost
friends or loved ones.31
Nonspecific symptoms, coupled with the absence of rapid,
definitive diagnostic testing, and uncertainty about how to assess exposure and the optimal prophylaxis regimen (as occurred in the 2001 anthrax event), may exacerbate anxieties
and lead to noncompliance with public health recommendations.32 Common physical complaints may stimulate demands
for medical intervention in the absence of evidence of exposure. For example, over 30,000 individuals were offered prophylactic antibiotics during the relatively small 2001 anthrax
attack33 in which only 22 people were infected,34 and many
more individuals, some far from the attack, sought antibiotics
Received for publication February 3, 2005
and in revised form April 27, 2005
Accepted for publication April 27, 2005
Q1
JGIM
Eisenman et al., Terrorisms Psychologic Effects
outside of official channels.35 Unexposed patients may present
with somatic symptoms mimicking exposure symptoms.36 For
example, when a radioactive substance in Brazil contaminated
250 persons in 1987, 5,000 of the first 60,000 persons
screened had symptoms of acute radiation sickness (e.g., vomiting, diarrhea, and neck/facial rash), but none were contaminated. Disaster Somatization Reaction (DSR), a disaster
psychiatry term for unexposed individuals who interpret their
anxiety symptoms as evidence of exposure or infection or exhibit symptoms similar to the disease, replaces the stigmatized
terms hysteria and psychogenic illness,37 which have little
triage value.
Some agents can linger in the environment for weeks to
years (e.g., anthrax38 and radiologic isotopes), sustaining exposure risk and prolonging stress. Unexplained, persistent neuropsychologic problems can be an effect of CBRN agents.21,39
One year after the anthrax attacks, survivors reported memory
difficulties, poor concentration,40,41 and psychological distress.42 PCPs with patients experiencing multiple unexplained physical symptoms (MUPS)12,43 may have difficulty
in determining whether such symptoms are because of a medical condition or are psychological in origin.40
Managing PCPs own emotional and behavioral responses
will also be important. In the aftermath of the Toronto SARS
epidemic where 40% of the 20,000 quarantined persons were
health care workers, high rates of PTSD and depression symptoms among surviving health care workers were described44,45
and the value of psychosocial support for quarantined workers
was demonstrated.14,15 In a CBRN event, demands for unnecessary testing and prescriptions may further stress already
strained PCPs whose fears and angers may be exacerbated by
those of their patients.46 These providers will be at risk for
burnout, stress disorders, anxiety, and depression.47,48
BARRIERS TO PCP DELIVERY OF MENTAL HEALTH
CARE IN A CBRN EVENT
Existing barriers to delivering high-quality primary mental
health care are relevant to PCPs abilities to deliver psychosocial care after a CBRN event.
Conceptual Barriers
Mental health providers linked to different systems from PCPs
(e.g., social workers in social service systems) may have scant
understanding of primary care. Conversely, PCPs view the
DSM-IV-R as too complex and specialty focused.49,50 Existing
treatment guidelines for primary care focus on major disorders
and little guidance is provided about sub-threshold forms of
PTSD,51,52 panic,53 somatization,54,55 and substance abuse,56
although all may affect functioning. The burgeoning field
of disaster mental health57 and its evolving terminology may
add an additional communication barrier in the event of a
CBRN event.
Provider- and Patient-Level Barriers
Most Americans will likely turn first to their physicians for information about a bioterrorist event,58 but studies performed
before September 11 reported that physicians are reluctant to
inquire about personal traumas.5961 Risk communication
with patients may reduce their emotional distress62 but this
is not a skill mastered by all physicians,63 as demonstrated
773
during the anthrax attacks.32 In addition, labeling individuals
presenting with somatic symptoms without an apparent physical etiology as worried well will create an obstacle between
patient and provider.13,36 Somatic presentations of emotional
distress can act as a barrier to its detection and response.
Nonspecific symptoms coupled with providers reluctance to
repeatedly test for exposure or infection may exacerbate patients anxieties.
System Barriers
Mental health providers are isolated from PCPs in the health
care system and payment structures provide disincentives to
PCPs treating mental health problems.64 These barriers may
be exacerbated after a CBRN attack because of the confusing
array of organizations that will be involved and the lack of
clarity about payment mechanisms.29 Most primary care practices have little experience with the Substance Abuse and Mental Health Services Administration (SAMHSA), the lead federal
agency for disaster mental health response. Public mental
health systems charged with delivering disaster mental health
care usually do not incorporate PCPs into their postdisaster
treatment policies, trainings, and reimbursements.65 Differentiating long-term organic mental disorders from psychologic
distress and formulating an appropriate treatment plan will
require guidance in distinguishing and referring patients and
linkage between primary care and disaster response agencies.66 Existing collaborative care models do not incorporate
the public health and disaster experts so additional linkages
are needed if patients are to be triaged into proposed interventions12 for reducing development of chronic medically unexplained syndromes (e.g., Gulf War syndrome).9
RECOMMENDATIONS
Primary care physicians can play important roles in policy,
education, and research that will contribute to overcoming
these barriers and preparing them to respond to the psychosocial consequences of a CBRN weapon (see Table 1).
1. Leaders in primary care should improve linkages with local,
state, and federal mental health and public health agencies:
Medical associations should support federal legislation,
like the National Resilience Development Act, calling for
federal coordination and resources to improve the nations
response to the mental health consequences of terrorism.67
National organizations, including the Society for General
Internal Medicine, should meet with officials from the U.S.
Department of Health and Human Services (DHHS) and
SAMHSA to address system-level barriers to care, such as
lack of reimbursement and linkage with disaster mental
health services. SAMSHA could ensure that PCPs are prepared to address CBRN-related concerns in patients, including being able to provide relevant recommendations,
education, testing, and referrals.9 SGIM should suggest
that the Federal Disaster Response Plan, which guides
the coordinated delivery of federal assistance and resources in the event of a major disaster, should address the complex and ambiguous long-term mental health disorders
that do not fit traditional diagnostic categories but are
likely to be treated by PCPs.66 Such activities would likely
Q1
774
Eisenman et al., Terrorisms Psychologic Effects
benefit the public mental health system, as enhancing PCP
capacity to address these issues will reduce financial and
workforce strain among mental health providers.6568Administrators and primary care leaders of managed health
care organizations, health plans, and other health organizations should begin by meeting with state and local medical societies and bioterrorism coordinators to learn about
how existing disaster mental health plans incorporate primary care services, and to acquaint themselves with model
linkages that they can implement after a CBRN event. (The
job of bioterrorism coordinators, located in public health
agencies and often funded by CDC and DHHS grants, in69
cludes working with the private sector.) For example, the
Department of Defense implemented a novel program after
September 11 in which PCPs were assigned to a trained
care manager to help treat terrorism-related problems.70 A
proposed stepped system of evidence-based rehabilitative
care for military personnel that links primary care, mental
health, and public health and disaster experts in the prevention and treatment of disaster-related somatic symptoms could be adapted for civilian populations.71,72 Health
plans can develop 2-way communication systems between
primary care and behavioral health call centers and case
Q5
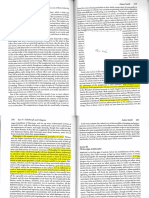
Table 1. How Primary Care Physicians Can Prepare for the Psychosocial Consequences of a CBRN Attack
Response planning (national level)
Leadership to meet with DHS, DHHS, SAMHSA
Leadership to address reimbursement issues
Support legislation
Partner with disaster agencies
Participation in disaster response exercises
Develop guidelines regarding management and referral of patients
with DSR, MUPS
Response planning (state/local level)
Meet with local/state bioterrorism coordinators and public mental
health
Partner with public health using Bioterrorism and Cooperative
Agreement Program funds
Support legislation
Participation in disaster response exercises
Develop guidelines regarding management and referral of patients
with DSR, MUPS
Response planning (institutional level)
Develop family, practice, and institution-level disaster plans
Develop psychosocial support plans for staff
Ensure representation in Incident Command Structure
Link information technologies and decision support programs to
mental health
Two-way communication systems with behavioral health call centers
Adapt best practices models to local environment (e.g., Operation
Solace, Engels, and Katon model)
Develop guidelines regarding management and referral of patients
with DSR, MUPS
Research and education
Test triage algorithms, screening tools, brief psychologic
interventions
Develop information technologies and decision support programs
Curriculum development (e.g., developing family and practice
disaster plans; psychologic impacts of isolation and quarantine;
formal skills in risk communication)
Develop guidelines regarding management and referral of patients
with DSR, MUPS
CBRN, chemical, biologic, radiologic, or nuclear; DHHS, Department of
Health and Human Services; SAMHSA, Substance Abuse and Mental
Health Services Administration; DSR, Disaster Somatization Reaction;
MUPS, multiple unexplained physical symptoms.
JGIM
managers,16 supported by funding from DHHSs Bioterrorism and Cooperative Agreement Program, which is intended
for improving communications.73 Information technologies
(e.g., telemedicine, electronic linkages) planned for frontline clinicians should include links to mental health services and decision support programs. Also, PCPs can have
input into disaster response plans by participating in local
municipal and hospital disaster management exercises.
Lastly, PCPs working in hospital-based practices and managed care organizations should ensure that they are represented in their hospitals or organizations incident
command structure, which is responsible for managing
and coordinating the response to a disaster.
2. Disaster planning should include training PCPs about the
emotional and behavioral responses: Standard educational
curriculums can do more to emphasize training in grief and
bereavement and the science-based approach to risk communication. They should include simple interventions
such as psychologic first aid, a set of skills believed to limit distress, and negative health behaviors.9,10 Training
should also address PCPs own responses to a CBRN attack by developing family and practice disaster plans,29
including prevention of PCPs adverse psychologic reactions.46,74 Training should address the psychologic impacts of isolation and quarantine and formal skills in risk
communication that will help them access and use risk information when it is disseminated. PCPs should learn
about DSR and MUPS and establish guidelines of care to
both inform that education and guide the management and
referral of these patients. Training modules and curriculum can build on existing ones (e.g., www.med.nyu.edu/
chip), be prepared and tested in advance, and disseminated as just-in-time packages with information on referrals.
3. PCPs should research critical knowledge gaps: PCPs need to
develop and study models of mental health linkages between primary care and the different service sectors that
will operate in a CBRN event. More information is needed
about PCPs roles in addressing sub-threshold mental
health disorders and somatization symptoms resulting
from a disaster. Research into the long-term psychologic
consequences of the anthrax attacks and SARS epidemic is
required to ameliorate any potential future public health
problems.36,72 Finally, additional research is needed on
what aspects of PCPs knowledge and skills in addressing
traumatic issues occurring in everyday practice (e.g., interpersonal violence) are most relevant for addressing psychologic issues in the aftermath of a CBRN event.
CONCLUSIONS
CBRN response planning could help spur improvements in the
daily management of routine mental health problems in primary care settings, similar to the way federal bioterrorism
funds are improving the public health infrastructure. Efforts
to address the primary carebased treatment of these mental
health consequences6 should be sustained and increased as
recommended.
REFERENCES
1. Barbera J, Macintrye AG. The reality of the modern bioterrorism response. Lancet. 2004;360(1 suppl):33.
Q1
Q3
Q4
JGIM
Eisenman et al., Terrorisms Psychologic Effects
2. Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Mental health
service and medication use in New York City after the September 11,
2001, terrorist attack. Psychiatr Serv. 2002;55:27483.
3. McCarter L, Goldman W. Use of psychotropics in two employee groups
directly affected by the events of September 11. Psychiatr Serv. 2002;
53:13668.
4. Adams ML, Ford JD, Dailey WF. Predictors of help seeking among Connecticut adults after September 11, 2001. Am J Public Health. 2004;94:
1596602.
5. Facing fear together: mental health and primary care in a time of terrorism. Blueprint Report, Americas Health Together; 2003.
6. Laraque D, Boscarino JA, Battista A, et al. Reactions and needs
of tristate-area pediatricians after the events of September 11th: implications for childrens mental health services. Pediatrics. 2004;113:
135766.
7. Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorder service system:
epidemiologic catchment area prospective one-year prevalence rates of
disorders and services. Arch Gen Psychiatry. 1993;50:8594.
8. Tanielian T, Stein B, Eisenman D, Keyser D, Olmstead S, Pincus H.
Understanding and Preparing for the Mental Health Consequences of
Bioterrorism. Report No. DRR-2919-RC. Santa Monica, Calif: The RAND
Corporation; 2003.
9. Institute of Medicine. Preparing for the Psychological Consequences of
Terrorism: A Public Health Strategy. Washington, DC: The National
Academies Press; 2003.
10. Hall MJ, Norwood AE, Ursano RJ, Fullerton CS. The psychological impacts of bioterrorism. Biosecurity Bioterrorism: Biodefense Strategy
Pract Sci. 2003;1:13944.
11. Demartino RM. Bioterrorism: what are we afraid of and what should we
do? Paper presented at Biosecurity 2002 Conference, November 2002,
Las Vegas, Nev.
12. Clauw D, Engel C, Aronowitz R, et al. Unexplained symptoms after
terrorism and war: an expert consensus statement. J Occup Environ
Med. 2003;45:10408.
13. Lacy TJ, Benedek DM. Terrorism and weapons of mass destruction:
managing the behavioral reaction in primary care. South Med J.
2003;96:3949.
14. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R.
SARS control and psychological effects of quarantine, Toronto, Canada.
Emerg Infect Dis. 2004;10:120612.
15. Maunder R, Hunter J, Vincent L, et al. The immediate psychological
and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:124551.
16. Burstin H. Bioterrorism and health system preparedness: emerging
tools, methods, and strategies. Web Conference, broadcast on April 29,
30, and May 1, 2002. Rockville, Md: Agency of Healthcare Research and
Quality. Available at: http://www.ahrq.gov/news/ulp/bioteleconf/.
17. Pincus HA, Pechura CM, Elinson L, Pettit AR. Depression in primary
care: linking clinical and systems strategies. Gen Hosp Psychiatry.
2001;23:3118.
18. Havenaar J, Rumyahtzeva G, Van Den Brink W, et al. Long-term mental health effects of the Chernobyl disaster: an epidemiologic survey in
two former Soviet regions. Am J Psychiatry. 1997;154:16057.
19. Bowler R, Mergler D, Huel G, Cone JE. Psychological, psychosocial,
and psychophysiological sequelae in a community affected by a railroad
chemical disaster. J Traumatic Stress. 1994;7:60124.
20. Kawana N, Ishimatsu S, Kanda K. Psycho-physiological effects of the
terrorist Sarin attack on the Tokyo subway system. Mil Med.
2001;166(12 suppl):236.
21. Kovalchick DF, Burgess JL, Kyes KB, et al. Psychological effects of
hazardous materials exposure. Psychosom Med. 2002;64:8416.
22. Schuster MA, Stein BD, Jaycox L, et al. A national survey of stress
reactions after the September 11, 2001, terrorist attacks. N Engl J Med.
2001;345:150712.
23. Boscarino JA, Galea S, Ahern J, Resnick H, Vlahov D. Psychiatric
medication use among Manhattan residents following the World. J
Traum Stress. 2003;16:3016.
24. Terr LC, Bloch DA, Michel BA, Shi H, Reinhardt JA, Metayer S. Childrens symptoms in the wake of Challenger: a field study of distant-traumatic effects and an outline of related conditions. Am J Psychiatry.
1999;156:153644.
25. Pfefferbaum B, Seale TW, McDonald NB, et al. Posttraumatic stress
two years after the Oklahoma City bombing in youths geographically
distant from the explosion. Psychiatry. 2000;63:35870.
775
26. Smith DW, Christiansen EH, Vincent R, Hann NE. Population effects of
the bombing of Oklahoma City. J Okla State Med Assoc. 1999;92:1938.
27. Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to
terrorist attacks: findings from the national study of Americans reactions to September 11. JAMA. 2002;288:5818.
28. Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11.
JAMA. 2002;288:123544.
29. Rippen HE, Gursky E, Stoto MA. Importance of bioterrorism preparedness for family physicians. Am Fam Physician. 2003;67:18778.
30. Lemkau JP, Mann B, Little D, Whitecar P, Hershberger P, Schumm
JA. A questionnaire survey of family practice physicians perceptions of
bereavement care. Arch Fam Med. 2000;9:8229.
31. Wunsch-Hitzig R, Plapinger J, Draper J, del Campo E. Calls for help
after September 11: a community mental health hot line. J Urban
Health. 2002;79:41728.
32. Stein BD, Tanielian TL, Ryan GW, Rhodes HJ, Young SD, Blanchard
JC. A bitter pill to swallow: nonadherence with prophylactic antibiotics
during the anthrax attacks and the role of private physicians. Biosecurity Bioterrorism. 2004;2:17585.
33. Gerberding JL, Hughes JM, Koplan JP. Bioterrorism preparedness and
response: clinicians and public health agencies as essential partners.
JAMA. 2002;287:898900.
34. Bioterrorism: Public Health Response to Anthrax Incidents of 2001. Washington, DC: US General Accounting Office October; 2003, GAO-04152.
35. Shaffer D, Armstrong G, Higgins K, et al. Increased US prescription
trends associated with the CDC Bacillus anthracis antimicrobial postexposure prophylaxis campaign. Pharmacoepidemiol Drug Saf. 2003;12:
17782.
36. Pastel RH. Collective behaviors: mass panic and outbreaks of multiple
unexplained symptoms. Mil Med. 2001;166(12 suppl):446.
37. Diamond D, Schreiber M. Terrorism Agent Information and Treatment
Guidelines for Clinicians and Hospitals. Los Angeles: County of Los Angeles Department of Health Services; 2003.
38. Inglesby TV, Henderson DA, Bartlett JG, et al. Anthrax as a biological
weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA. 1999;281:173545.
39. DiGiovanni C Jr. Domestic terrorism with chemical or biological agents:
psychiatric aspects. Am J Psychiatry. 1999;156:15005.
40. Cymet TC, Kerkvliet GJ. Inhalational anthrax: the natural history of a
treatable disease. J Am Osteopath Assoc. 2003;103:390.
41. Shane S. Anthrax survivors find life a struggle. Baltimore Sun; September 18, 2003.
42. Reissman DB, Whitney EA, Taylor TH Jr, et al. One-year health assessment of adult survivors of Bacillus anthracis infection. JAMA. 2004;
291:19948.
43. Hassett AL, Sigal LH. Unforeseen consequences of terrorism: medically
unexplained symptoms in a time of fear. Arch Intern Med. 2002;162:
180913.
44. Styra R, Gold W, Robinson S. Post-traumatic stress disorder and quality of life in patients diagnosed with SARS. Paper presented at 43rd Interscience Conference on Antimicrobial Agents and Chemotherapy,
Chicago, Ill; September 1417, 2003.
45. Caulford P. SARS: aftermath of an outbreak. Lancet. 2003;362(1 suppl):
23.
46. Fain RM, Schreier RA. Disaster, stress and the doctor. Med Educ.
1989;23:916.
47. Holtz TH, Salama P, Lopes Cardozo B, Gotway CA. Mental health status of human rights workers. Kosovo J Trauma Stress. 2002;15:3895.
48. Grieger TA, Fullerton CS, Ursano RJ. Posttraumatic stress disorder,
alcohol use, and perceived safety after the terrorist attack on the Pentagon. Psychiatr Serv. 2003;54:13802.
49. Coyne J, Thompson R, Klinkman M, Nease D. Emotional disorders in
primary care. J Consult Clin Psychol. 2002;70:798809.
50. Goldberg D. A classification of psychological distress for use in primary
care settings. Soc Sci Med. 1992;35:1893.
51. Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, Holmes T.
PTSD and utilization of medical treatment services among male Vietnam
veterans. J Nerv Ment Dis. 2000;188:496504.
52. Schnurr PP, Spiro A III, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans.
Health Psychol. 2000;19:917.
53. Klerman GLWM, Ouellette R, Johnson J, Greenwald S. Panic attacks
in the community. Social morbidity and health care utilization. JAMA.
1991;265:7426.
Q1
776
Eisenman et al., Terrorisms Psychologic Effects
54. Escobar JI, Canino G, Rubio Stipec M, Bravo M. Somatic symptoms
after a natural disaster: a prospective study. Am J Psychiatry. 1992;149:
9657.
55. Escobar J, Burnam MA, Karno M, Forsythe A, Golding JM.
Somatization in the community. Arch Gen Psychiatry. 1987;44:
7138.
56. Webb G, Hennrikus DJ, Kelman GR, Gibberd RW, Sanson-Fisher R.
The relationships between high-risk and problem drinking and the occurrence of work injuries and related absences. J Stud Alcohol.
1994;55:4346.
57. Becker SM. Meeting the threat of weapons of mass destruction terrorism: toward a broader conception of consequence management. Mil Med.
2001;166(12 suppl):136.
58. Blendon RJ, Benson JM, DesRoches CM, Pollard WE, Parvanta C,
Herrmann MJ. The impact of anthrax attacks on the American public.
Med Gen Med. 2002;4:1.
59. McCauley J, Yurk RA, Jenckes MW, Ford DE. Inside Pandoras box:
abused womens experiences with clinicians and health services. J Gen
Intern Med. 1998;13:54955.
60. Sugg N, Inui T. Primary care physicians response to domestic violence.
Opening Pandoras box. JAMA. 1992;315760.
61. Parsons LH, Zaccaro D, Wells B, Stovall TG. Methods of and attitudes
toward screening obstetrics and gynecology patients for domestic violence. Am J Obstet Gynecol. 1995;173:3817.
62. DiGiovanni C Jr, Reynolds B, Harwell R, Stonecipher EB, Burkle FM
Jr. Community reaction to bioterrorism: prospective study of simulated
outbreak. Emerg Infect Dis. 2003;9:70812.
63. Haq C, Steele DJ, Marchand L, Seibert C, Brody D. Integrating the art
and science of medical practice: innovations in teaching medical communication skills. Fam Med. 2004;36(suppl):S4350.
64. Olsen CG. Good grief. Arch Fam Med. 2000;9:8334.
JGIM
65. Jack K, Glied S. The public costs of mental health response: lessons
from the New York City post-9/11 needs assessment. J Urban Health.
2002;79:3329.
66. Becker SM. Are the psychosocial aspects of weapons of mass destruction incidents addressed in the Federal Response Plan: summary of an
expert panel. Mil Med. 2001;166(12 suppl):668.
67. National Resilience Development Act of 2003 H.R. 2370. 1st Session;
2003.
68. Siegel C, Wanderling J, Laska E. Coping with disasters: estimation of
additional capacity of the mental health sector to meet extended service
demands. J Ment Health Policy Econ. 2004;7:2935.
69. Beitsch L. Bioterrorism and health system preparedness: emerging
tools, methods, and strategies. Web Conference, Broadcast on April 29,
30, and May 1, 2002. Rockville, Md: Agency for Healthcare Research and
Quality. Available at: http://www.ahrq.gov/news/ulp/bioteleconf/.
70. Hoge CW, Orman DT, Robichaux RJ, et al. Operation solace: overview
of the mental health intervention following the September 11, 2001 Pentagon attack. Mil Med. 2002;167(9 suppl):447.
71. Engel CC, Katon W. Population and Need-Based Prevention of Unexplained Symptoms in the Community. Strategies to Protect the Health of
Deployed U.S. Forces: Medical Surveillance, Record Keeping, and Risk
Reduction. Washington, DC: National Academy Press; 1999:173212.
72. Engel CC Jr. Outbreaks of medically unexplained physical symptoms
after military action, terrorist threat, or technological disaster. Mil Med.
2001;166(12 suppl):478.
73. Meehan PJ. Bioterrorism and health system preparedness: emerging
tools, methods, and strategies. Web Conference, Broadcast on April 29,
30, and May 1, 2002. Rockville, Md: Agency for Healthcare Research and
Quality. Available at: http://www.ahrq.gov/news/ulp/bioteleconf/.
74. Bradford R, John AM. The psychological effects of disaster work: implications for disaster planning. J R Soc Health. 1991;111:10710.
Potrebbero piacerti anche
- Evidence Based Treatments for Trauma-Related Psychological Disorders: A Practical Guide for CliniciansDa EverandEvidence Based Treatments for Trauma-Related Psychological Disorders: A Practical Guide for CliniciansUlrich SchnyderNessuna valutazione finora
- Review of Psychological Trauma: Theory, Practice, Policy and ResearchDocumento10 pagineReview of Psychological Trauma: Theory, Practice, Policy and ResearchMohammad TahanNessuna valutazione finora
- Trastorno Depresivo en Edades TempranasDocumento15 pagineTrastorno Depresivo en Edades TempranasManuel Dacio Castañeda CabelloNessuna valutazione finora
- Shkrimi AkademikDocumento6 pagineShkrimi AkademikRita JakupiNessuna valutazione finora
- Anxiety Disorder Psychological Testing Research WorkDocumento7 pagineAnxiety Disorder Psychological Testing Research Workshaswat chaudharyNessuna valutazione finora
- 02-Tahan (64-73)Documento10 pagine02-Tahan (64-73)José Carlos Sánchez RamírezNessuna valutazione finora
- The Biology of Borderline (And A Diagnostic Tip)Documento7 pagineThe Biology of Borderline (And A Diagnostic Tip)JuanFelipeRamirezCNessuna valutazione finora
- Complex Ptsd Recovery Understanding and treating Complex Trauma Using Emdr and Concepts from Individual PsychologyDa EverandComplex Ptsd Recovery Understanding and treating Complex Trauma Using Emdr and Concepts from Individual PsychologyNessuna valutazione finora
- Manejo Depresion 1Documento10 pagineManejo Depresion 1Luis HaroNessuna valutazione finora
- Park, 2019 - NEJM - DepressionDocumento10 paginePark, 2019 - NEJM - DepressionFabian WelchNessuna valutazione finora
- Chochinov DistressDocumento11 pagineChochinov DistressThatiana GimenesNessuna valutazione finora
- The Effectiveness of Art Therapy Interventions in Reducing Post Traumatic Stress Disorder PTSD Symptoms in Pediatric Trauma PatientsDocumento6 pagineThe Effectiveness of Art Therapy Interventions in Reducing Post Traumatic Stress Disorder PTSD Symptoms in Pediatric Trauma PatientsJoan Choi0% (1)
- Journal NeurotraumaDocumento34 pagineJournal NeurotraumaCarolina MuñozNessuna valutazione finora
- Borderline Personality Disorder Otto F. Kernberg M.D.Robert Michels M.DDocumento5 pagineBorderline Personality Disorder Otto F. Kernberg M.D.Robert Michels M.DДанило ПисьменнийNessuna valutazione finora
- Early Psychosocial Intervention Following Traumatic EventsDocumento4 pagineEarly Psychosocial Intervention Following Traumatic EventsAdrian CantemirNessuna valutazione finora
- Biobehavioral Utility of Mindfulness-Based Art Therapy: Neurobiological Underpinnings and Mental Health ImpactsDocumento9 pagineBiobehavioral Utility of Mindfulness-Based Art Therapy: Neurobiological Underpinnings and Mental Health Impactsотец хентайNessuna valutazione finora
- Davydow 2010 Psychiatric MorbidityDocumento9 pagineDavydow 2010 Psychiatric MorbidityAndrew EdisonNessuna valutazione finora
- Bereavement Challenges and Their Relationship To Physical and Psychological Adjustment To LossDocumento10 pagineBereavement Challenges and Their Relationship To Physical and Psychological Adjustment To LossJeselle CaputolanNessuna valutazione finora
- The Moral Injury and Distress Scale: Psychometric Evaluation and Initial Validation in Three High-Risk PopulationsDocumento12 pagineThe Moral Injury and Distress Scale: Psychometric Evaluation and Initial Validation in Three High-Risk PopulationsJonathan MacFarlaneNessuna valutazione finora
- Borderline Personality Is A Serious Psychiatric DisorderDocumento13 pagineBorderline Personality Is A Serious Psychiatric DisorderYEA BOIIINessuna valutazione finora
- Mood Disorders After TBIDocumento17 pagineMood Disorders After TBIJaun CarrilloNessuna valutazione finora
- From Rage to Recovery: Navigating Intermittent Explosive DisorderDa EverandFrom Rage to Recovery: Navigating Intermittent Explosive DisorderNessuna valutazione finora
- Comorbid Chronic Illness and The Diagnosis and Treatment of Depression in Safety Net Primary Care Settings - AniDocumento19 pagineComorbid Chronic Illness and The Diagnosis and Treatment of Depression in Safety Net Primary Care Settings - AniestudiolascrechesNessuna valutazione finora
- A Cross-Sectional Study of Factors Predicting Relapse in People With SchizophreniaDocumento12 pagineA Cross-Sectional Study of Factors Predicting Relapse in People With SchizophreniaArif IrpanNessuna valutazione finora
- The Mental Mirror: Reflections on Psychiatry: Beyond the Looking Glass: The Enigmatic Odyssey of the MindDa EverandThe Mental Mirror: Reflections on Psychiatry: Beyond the Looking Glass: The Enigmatic Odyssey of the MindNessuna valutazione finora
- Your Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022Da EverandYour Examination for Stress & Trauma Questions You Should Ask Your 32nd Psychiatric Consultation William R. Yee M.D., J.D., Copyright Applied for May 31st, 2022Nessuna valutazione finora
- PTSD-Adults Protocol 20111220Documento25 paginePTSD-Adults Protocol 20111220black_alynaNessuna valutazione finora
- Los Efectos Biológicos Del Trauma InfantilDocumento39 pagineLos Efectos Biológicos Del Trauma InfantilFelipe Cáceres RiquelmeNessuna valutazione finora
- 2002, Vol.25, Issues 1, Psychiatry in The Medically IllDocumento239 pagine2002, Vol.25, Issues 1, Psychiatry in The Medically IllGonzalo Sepulveda EstayNessuna valutazione finora
- Ijerph 16 02537 PDFDocumento11 pagineIjerph 16 02537 PDFDaniela DiazNessuna valutazione finora
- Depression and Suicidality in First Episode PsychoDocumento9 pagineDepression and Suicidality in First Episode PsychoNatalia Martinez CastroNessuna valutazione finora
- Use of Cannabis in the Treatment of Post-Traumatic Stress DisorderDa EverandUse of Cannabis in the Treatment of Post-Traumatic Stress DisorderNessuna valutazione finora
- Posttraumatic Stress Disorder: Scientific and Professional DimensionsDa EverandPosttraumatic Stress Disorder: Scientific and Professional DimensionsNessuna valutazione finora
- Psychiatric I PDFDocumento10 paginePsychiatric I PDFDhino Armand Quispe SánchezNessuna valutazione finora
- Evaluation of Depression and Suicidal Patients in The Emergency RoomDocumento15 pagineEvaluation of Depression and Suicidal Patients in The Emergency RoomjuanpbagurNessuna valutazione finora
- Evidence-Basedcareofthe Patientwithborderline PersonalitydisorderDocumento10 pagineEvidence-Basedcareofthe Patientwithborderline PersonalitydisorderMoonyNessuna valutazione finora
- ALTERACIaN DEL LENGUAJE COMO PREDICTOR DEL INICIO DE LA PSICOSIS EN JaVENES CON RIESGO CL+NICO AUMENTADODocumento2 pagineALTERACIaN DEL LENGUAJE COMO PREDICTOR DEL INICIO DE LA PSICOSIS EN JaVENES CON RIESGO CL+NICO AUMENTADOAlí Amaroo Pellicer OchoaNessuna valutazione finora
- 2006 - Dementia Care - Lancet NeurologyDocumento13 pagine2006 - Dementia Care - Lancet NeurologycoconitaNessuna valutazione finora
- Borderline Personality Is A Serious Psychiatric DisorderDocumento14 pagineBorderline Personality Is A Serious Psychiatric DisorderYEA BOIIINessuna valutazione finora
- Narcissistic Personality DisorderDocumento3 pagineNarcissistic Personality DisorderJohnson JosephNessuna valutazione finora
- Torres-Reading On PTSDDocumento15 pagineTorres-Reading On PTSDbabiNessuna valutazione finora
- Cognitive Functioning Under StressDocumento13 pagineCognitive Functioning Under StressMladen PuljićNessuna valutazione finora
- Fpsyt 11 565239Documento16 pagineFpsyt 11 565239Moira LudwigNessuna valutazione finora
- BB Web TP Focus 2011 Diag y Tto Del TPanico Resistente. LydiardDocumento11 pagineBB Web TP Focus 2011 Diag y Tto Del TPanico Resistente. LydiardAdriana Rodriguez PalmeroNessuna valutazione finora
- Covi̇dde Tükenmi̇şli̇kDocumento8 pagineCovi̇dde Tükenmi̇şli̇kTalipNessuna valutazione finora
- H1P S A C: Sychological Ymptoms in Dvanced AncerDocumento11 pagineH1P S A C: Sychological Ymptoms in Dvanced AnceryuliaNessuna valutazione finora
- Ansiedade 04Documento9 pagineAnsiedade 04Karina BorgesNessuna valutazione finora
- Major Depressive Disorder (MDD) - From Causes to Control: Health MattersDa EverandMajor Depressive Disorder (MDD) - From Causes to Control: Health MattersNessuna valutazione finora
- Tugas Bahasa IngrisDocumento5 pagineTugas Bahasa Ingrislong bottomNessuna valutazione finora
- A Systematic Review of The Impact of Disaster On The Mental Health of Medical RespondersDocumento12 pagineA Systematic Review of The Impact of Disaster On The Mental Health of Medical RespondersGustavo LimachiNessuna valutazione finora
- Riesgo Criminogenico y Salud MentalDocumento8 pagineRiesgo Criminogenico y Salud MentalPSIQUIATRIA HEJENessuna valutazione finora
- Post-Traumatic Stress Disorders Among The COVID-19 Survivors: Impact On Mental HealthDocumento4 paginePost-Traumatic Stress Disorders Among The COVID-19 Survivors: Impact On Mental Healthnashwamy04Nessuna valutazione finora
- Post-Traumatic Stress Disorder: A Guide for Primary Care Clinicians and TherapistsDa EverandPost-Traumatic Stress Disorder: A Guide for Primary Care Clinicians and TherapistsNessuna valutazione finora
- Corona Virus and Its ImplicationDocumento9 pagineCorona Virus and Its ImplicationElly RupangNessuna valutazione finora
- Assessing and Managing Violence Risk in Outpatient Settings: Randy K. OttoDocumento28 pagineAssessing and Managing Violence Risk in Outpatient Settings: Randy K. OttoFetty Ign DimengerthiNessuna valutazione finora
- Depression and The Environment DR Vishal BhavsarDocumento11 pagineDepression and The Environment DR Vishal Bhavsarugudaa fsiiNessuna valutazione finora
- 1 s2.0 S1755599X18301149 MainDocumento6 pagine1 s2.0 S1755599X18301149 Mainהילה אביאליNessuna valutazione finora
- PDF 157105 89671Documento14 paginePDF 157105 89671Krikunov KaNessuna valutazione finora
- Article Revised Naeem, Ammar, QuratDocumento7 pagineArticle Revised Naeem, Ammar, QuratNoorulain HamidNessuna valutazione finora
- Preprint Moral Injury - 2021Documento18 paginePreprint Moral Injury - 2021Mihaela-AlexandraGhermanNessuna valutazione finora
- 2d Text Preset Pack For Animation Composer LicenseDocumento1 pagina2d Text Preset Pack For Animation Composer Licenseesat936Nessuna valutazione finora
- Odyssey Outline p.456Documento2 pagineOdyssey Outline p.456esat936Nessuna valutazione finora
- William Empson On Enabling Modernist AmbiguitiesDocumento1 paginaWilliam Empson On Enabling Modernist Ambiguitiesesat936Nessuna valutazione finora
- Critical Theory Notes On PhaedrusDocumento1 paginaCritical Theory Notes On Phaedrusesat936Nessuna valutazione finora
- Elements of Rhetorical Narratology in PlatoDocumento3 pagineElements of Rhetorical Narratology in Platoesat936Nessuna valutazione finora
- Homo Nationalis - An Anthropological Sketch of The Nation-FormDocumento2 pagineHomo Nationalis - An Anthropological Sketch of The Nation-Formesat936Nessuna valutazione finora
- Homo Nationalis - An Anthropological Sketch of The Nation-FormDocumento2 pagineHomo Nationalis - An Anthropological Sketch of The Nation-Formesat936Nessuna valutazione finora
- Odyssey Outline p.456Documento2 pagineOdyssey Outline p.456esat936Nessuna valutazione finora
- Higher Education and The Politics of Knowledge PDFDocumento15 pagineHigher Education and The Politics of Knowledge PDFesat936Nessuna valutazione finora
- Ambient Meaning PDFDocumento155 pagineAmbient Meaning PDFesat936Nessuna valutazione finora
- Adam Smith - The Origin of PhilosophyDocumento3 pagineAdam Smith - The Origin of Philosophyesat936Nessuna valutazione finora
- Critique of LatourDocumento20 pagineCritique of Latouresat936Nessuna valutazione finora
- Unit 1 Cheat SheetDocumento1 paginaUnit 1 Cheat Sheetesat936Nessuna valutazione finora
- Walking in The CityDocumento14 pagineWalking in The Cityesat936Nessuna valutazione finora
- The Fashion System PDFDocumento233 pagineThe Fashion System PDFesat936Nessuna valutazione finora
- Work HoursDocumento1 paginaWork Hoursesat936Nessuna valutazione finora
- Bolivian Climate JusticeDocumento18 pagineBolivian Climate Justiceesat936Nessuna valutazione finora
- CH 1 States of Denial (Cohen)Documento12 pagineCH 1 States of Denial (Cohen)esat936Nessuna valutazione finora
- Sebastio SalgadoDocumento7 pagineSebastio Salgadoesat936Nessuna valutazione finora
- Letter To A Japanese FriendDocumento4 pagineLetter To A Japanese FriendmbhajianiNessuna valutazione finora
- Bolivian Climate JusticeDocumento18 pagineBolivian Climate Justiceesat936Nessuna valutazione finora
- Popper - Knowledge Without AuthorityDocumento6 paginePopper - Knowledge Without Authorityesat936Nessuna valutazione finora
- Philadelphia and Urban Recovery: Chapter 13 - EpilogueDocumento6 paginePhiladelphia and Urban Recovery: Chapter 13 - Epilogueesat936Nessuna valutazione finora
- Raymond Williams Marxism and LiteratureDocumento113 pagineRaymond Williams Marxism and Literatureesat936100% (2)
- Hegel DictionaryDocumento281 pagineHegel DictionaryNusret Sarraf100% (22)
- Everything Is MineDocumento24 pagineEverything Is Mineesat936Nessuna valutazione finora
- DLL in MAPEH 6 - Health Week 10Documento4 pagineDLL in MAPEH 6 - Health Week 10Sara Jane C. Jose-TayaoNessuna valutazione finora
- CV UPDATE Agt, 2021Documento6 pagineCV UPDATE Agt, 2021nadita erischaNessuna valutazione finora
- The Andrea Bocelli ConcertDocumento2 pagineThe Andrea Bocelli Concertgastoast5Nessuna valutazione finora
- GB 20799-2016 Code of Hygienic Practice For Meat and Meat ProductsDocumento6 pagineGB 20799-2016 Code of Hygienic Practice For Meat and Meat Productsjose ManuelNessuna valutazione finora
- Critical Thinking Case Study #18:: Sickle-Cell AnemiaDocumento15 pagineCritical Thinking Case Study #18:: Sickle-Cell AnemiaHakima Hadji DaudNessuna valutazione finora
- OSH Manual Medium Risk EntitiesDocumento122 pagineOSH Manual Medium Risk EntitiesNitika SinhaNessuna valutazione finora
- Armor All Original Protectant (2015-01) SDS EnglishDocumento5 pagineArmor All Original Protectant (2015-01) SDS EnglishomarhereeraNessuna valutazione finora
- W E L L N E: Learning Activity Sheets in Health Education Mapeh 7 Quarter 1 Week 8Documento3 pagineW E L L N E: Learning Activity Sheets in Health Education Mapeh 7 Quarter 1 Week 8Joseph Eric NardoNessuna valutazione finora
- Career Map AssignmentDocumento9 pagineCareer Map Assignmentapi-301456362Nessuna valutazione finora
- How To Be A Business OwnerDocumento34 pagineHow To Be A Business Ownersimbarashe mukondo100% (2)
- CIF - Version 9 GENE XPERT POST MORTEMDocumento3 pagineCIF - Version 9 GENE XPERT POST MORTEMBALIUAG DISTRICT LABORATORYNessuna valutazione finora
- NursingDocumento9 pagineNursingIlie SmarandacheNessuna valutazione finora
- TLE 7 Health and Safety in The KItchenDocumento32 pagineTLE 7 Health and Safety in The KItchenChristine Mabelle AlmojuelaNessuna valutazione finora
- The Real Secret To BeautyDocumento3 pagineThe Real Secret To BeautySyafiq SaroniNessuna valutazione finora
- 500GR Triton TM Kaowool Epsilon Ceramic Fibre PureDocumento10 pagine500GR Triton TM Kaowool Epsilon Ceramic Fibre PureArief BudimanNessuna valutazione finora
- (Main Manuscript) Clinical Practice Guidelines For The Screening, Diagnosis, Treatment and Prevention of Neonatal SepsisDocumento69 pagine(Main Manuscript) Clinical Practice Guidelines For The Screening, Diagnosis, Treatment and Prevention of Neonatal Sepsiskaydee.arNessuna valutazione finora
- Fibromyalgia: Invisible Pain (Body Image and Depression)Documento8 pagineFibromyalgia: Invisible Pain (Body Image and Depression)4gen_3Nessuna valutazione finora
- Disaster Management at Site and at HospitalDocumento21 pagineDisaster Management at Site and at HospitalAlmasNessuna valutazione finora
- Current Trends and Issues in SpedDocumento2 pagineCurrent Trends and Issues in SpedRyan RV ViloriaNessuna valutazione finora
- HemivaginaDocumento3 pagineHemivaginafitriamarizkaNessuna valutazione finora
- Lost All HopeDocumento8 pagineLost All HopeRhemiel Castañeda100% (1)
- CIRCI Guidelines 2015Documento6 pagineCIRCI Guidelines 2015Wissam SleimanNessuna valutazione finora
- Epidemiology, Pathology, Clinical Features, and Diagnosis of Meningioma - UpToDateDocumento22 pagineEpidemiology, Pathology, Clinical Features, and Diagnosis of Meningioma - UpToDatewilson kores100% (1)
- Dme Qualification 02072023Documento2 pagineDme Qualification 02072023MLBB RangersNessuna valutazione finora
- BodyBallancer Lipo Brochure PDFDocumento2 pagineBodyBallancer Lipo Brochure PDFRoss Gale100% (1)
- Library - Uns.ac - Id Digilib - Uns.ac - Id: Daftar PustakaDocumento6 pagineLibrary - Uns.ac - Id Digilib - Uns.ac - Id: Daftar PustakaJulistin haiNessuna valutazione finora
- Management of Pneumonia in Intensive Care: Andrew Conway MorrisDocumento17 pagineManagement of Pneumonia in Intensive Care: Andrew Conway MorrisWillian Palma GómezNessuna valutazione finora
- Ro10 Bukidnon Provincial Medical Center Malaybalay CityDocumento37 pagineRo10 Bukidnon Provincial Medical Center Malaybalay Citycaleb castilloNessuna valutazione finora
- 8760 HoursDocumento18 pagine8760 HoursRubeel KhatibNessuna valutazione finora
- Risk For Unstable Blood Glucose Related To Unhealthy Lifestyle.Documento8 pagineRisk For Unstable Blood Glucose Related To Unhealthy Lifestyle.eleinsamNessuna valutazione finora