Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Healthy Gingiva Guide
Caricato da
velangniTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Healthy Gingiva Guide
Caricato da
velangniCopyright:
Formati disponibili
Page 1 of 31
Chapter 12
The Gingiva
P.213
The true test of successful treatment, the real evaluation of the effects of scaling and related
instrumentation, is the health of the periodontal tissues. The objective of all treatment is to bring
the diseased periodontal tissues to a state of health that can be maintained by the patient. To do
this, the first objective is to learn to recognize normal healthy tissue; to observe certain
characteristics of color, texture, and form; to test for bleeding; and to apply this knowledge to the
treatment and supervision of the patient's gingiva until health is attained.
An outline of the clinical features of the periodontal tissues in health and disease is included in this
chapter. Key words are defined in Box 12-1.
Box 12-1 Key Words
Key Words: Gingiva and Periodontium
Attachme nt appa ratus: the c ementu m, peri odonta l liga ment, and t he alv eolar bone.
Clinica l atta chment level: the p robin g dept h meas ured f rom a f ixed point, such as th e
cemento enamel junc tion.
Desmosom e: cel l junc tion; consi sts of a de nse pl ate n ear th e cell surfa ce th at rel ates t o a
similar struc ture o n an a djace nt cel l, bet ween which are th in lay ers of extra cellu lar
materia l.
Diaste ma: a s pace betwee n two natur al adj acent teeth . Plur al, di astema ta. Se e also
Primate space , pag e 287 .
Epithel ium
O ral: t he ti ssue s erving as a liner for t he int raoral mucosa l surf aces.
S quamous: compo sed of a la yer of flat, scale like c ells; or may be st ratifi ed.
Fibrobla st: fi ber-pro ducin g cell of th e con nectiv e tis sue; a flatt ened, irreg ularly branc hed
cell wi th a large oval n ucleu s that is re spons ible i n part for t he pro ducti on and remod eling
of the extra cellu lar mat rix.
Fibrosi s: a f ibrous chang e of the mu cous me mbrane , espe cially the gingiv a, as a res ult of
chroni c infl ammatio n; fib rotic gingiv a may appear outwa rdly h ealth y, thu s mask ing
underl ying d iseas e.
Hemides mosome: half of a d esmoso me that forms a sit e of a ttach ment be tween junct ional
epithe lial c ells a nd th e toot h sur face.
Hyperk eratos is: ab normal thicke ning of the kerat in la yer (st ratum corneu m) of t he
epithe lium.
Hyperpl asia: abnor mal inc rease in vol ume of a tis sue o r orga n caus ed by format ion an d
growth of ne w norma l cell s.
Hypertr ophy: i ncreas e in s ize o f tiss ue or organ cause d by a n inc rease in siz e of i ts
consti tuent cells .
Kerati nizatio n: deve lopmen t of a horn y laye r of f latten ed ep itheli al cel ls con taini ng
kerati n.
Marker : iden tifier ; sympt oms or signs by wh ich a partic ular c ondit ion ca n be r ecogn ized;
for ex ample, clinic al an d micro biolog ic mark ers a re use d to i dentif y gin gival and
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 2 of 31
p eriod ontal infect ions.
Ma stica tion: ac t of chewin g.
N onkera tinized mucosa : linin g muco sa in which the s tratif ied sq uamous epith elial cells
r etain their nucle i and cytop lasm.
P eriodon tium: ti ssues surrou nding and suppor ting t he te eth; i n two sectio ns ar e the
g ingiv al uni t, comp osed of the free and a ttach ed gin giva a nd th e alve olar mucosa, and the
a ttach ment ap parat us, wh ich in clude s the cement um, per iodon tal lig ament, and alveol ar
p roces s.
P robing d epth: t he dis tance from t he gin gival margin to th e loca tion of the perio donta l
p robe tip in serted for g entle probi ng at the a ttachme nt.
P us: a fluid produc t of inflamma tion t hat c ontain s leu kocyte s, de genera ted ti ssue
e lement s, tis sue fl uids, and mi croorg anisms .
S harpey 's fi bers: penet rating conn ective tissu e fibe rs by which the t ooth i s att ached to
t he ad jacent alve olar b one; t he fi ber bu ndles penet rate c ementu m on o ne sid e and alveo lar
b one o n the other .
S tippling : the pitted , ora nge-pe el app earan ce fre quent ly see n on the su rface of th e
a ttach ed gin giva.
S uppurati on: for mation of pu s.
T aste bu d: rece ptor o f tas te on tongu e and oroph arynx; gobl et-sha ped ce lls o riente d at
r ight a ngles to th e surf ace o f the epith elium.
Objectives
The ultimate objective is to apply knowledge and skill in examination and assessment of the
periodontal tissues to patient care so that each patient attains and maintains optimum oral health.
The dental hygienist must know when the treatment provided by dental hygiene services is definitive
in restoring health and when additional treatment is needed. The patient can be properly informed so
that complete treatment can be provided.
Specific objectives are to be able to
Recognize normal periodontal tissues.
Know the clinical features of the periodontal tissues that must be examined for a complete
assessment.
P.214
Recognize the markers that are the basic signs of periodontal infections and classify them by
type and degree of severity.
Identify the dental hygiene treatment and instruction needed.
Outline the patient's preventive program.
The Treatment Area
The treatment procedures are applied directly to the teeth, the gingiva, and the gingival sulcus.
Detailed knowledge and understanding of the anatomy and normal clinical appearance of the hard
and soft oral tissues are prerequisite to meaningful examination and treatment.
I. The Teeth
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 3 of 31
A. Clinical Crown
The part of the tooth above the attached periodontal tissues. It can be considered the part of the
tooth where clinical treatment procedures are applied (Figure 12-1).
B. Clinical Root
The part of the tooth below the base of the gingival sulcus or periodontal pocket. It is the part of the
root to which periodontal fibers are attached.
C. Anatomic Crown
The part of the tooth covered by enamel.
D. Anatomic Root
The part of the tooth covered by cementum.
FIGURE 12-1 Clinical Crown. The part of the tooth that is above the attached
periodontal tissue. Left, When the periodontal pocket depth is increased, the clinical
crown extends to a position at which the clinical crown length is greater than the clinical
root length. The clinical root is that part of the tooth with attached periodontal tissues.
Right, When the clinical attachment level is at the cementoenamel junction, the clinical
crown and the anatomic crown are the same.
II. Oral Mucosa
The lining of the oral cavity, the oral mucosa, is a mucous membrane composed of connective tissue
covered with stratified squamous epithelium. There are three divisions or categories of oral mucosa.
A. Masticatory Mucosa
1.
Covers the gingiva and the hard palate, the areas used most during the mastication of food.
2.
Except for the free margin of the gingiva, the masticatory mucosa is firmly attached to
underlying tissues.
3.
The epithelial covering is generally keratinized.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 4 of 31
B. Lining Mucosa
1.
Covers the inner surfaces of the lips and cheeks, the floor of the mouth, the under side of the
tongue, the soft palate, and the alveolar mucosa.
2.
These tissues are not firmly attached to underlying tissue.
3.
The epithelial covering is not generally keratinized.
C. Specialized Mucosa
1.
Covers the dorsum (upper surface) of the tongue. It is composed of many papillae; some
contain taste buds.
2.
The distribution of the four types of papillae is shown in Figure 12-2.
a.
Filiform. Threadlike keratinized elevations that cover the dorsal surface of the tongue;
they are the most numerous of the papillae.
b.
Fungiform. Mushroom-shaped papillae interspersed among the filiform papillae on the
t i p a n d s i d e s o f t h e t o n g u e . O n c l i n i c a l e x a mi n a t i o n t h e y a p p e a r r e d d e r t h a n t h e f i l i f o r m
papillae and contain
P.215
variable numbers of taste buds. The inset enlargement in Figure 12-2 shows the
comparative shape and size of the filiform and fungiform papillae.
FIGURE 12-2 Papillae of the Tongue. Dorsal surface of a human tongue
shows the four types of papillae. Inset enlargement shows the shape of
filiform and fungiform papillae.
c.
Circumvallate (vallate). The 10 to 14 large round papillae arranged in a V between the
body of the tongue and the base. Taste buds line the walls.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 5 of 31
d.
Foliate. Vertical grooves on the lateral posterior sides of the tongue; also contain taste
buds.
III. The Periodontium
The periodontium is the functional unit of tissues that surrounds and supports the tooth. The four
parts are the gingiva, periodontal ligament, cementum, and bone; the last three make up the
attachment apparatus.
A. Periodontal Ligament
The periodontal ligament is the fibrous connective tissue that surrounds and attaches the
roots of teeth to the alveolar bone.
The ligament is located in the periodontal space between the cementum and the alveolar
bone.
It is composed of connective tissue cells and intracellular substance.
The fibers that are inserted into the cementum on one side and the alveolar bone on the other
are called Sharpey's fibers.
B. Periodontal Ligament Fiber Groups
The two general groups of fibers are the gingival groups (around the cervical area within the
gingival tissues) and the principal fiber groups (surrounding the root).1
1.
Gingival Fiber Groups (Figure 12-3)
Dentogingival fibers (free gingival). From the cementum in the cervical region into the
free gingiva to give support to the gingival.
Alveologingival fibers (attached gingival). From the alveolar crest into the free and
attached gingiva to provide support.
Circumferential fibers (circular). Continuous around the neck of the tooth to help to
maintain the tooth in position.
Dentoperiosteal fibers (alveolar crest). From the cervical cementum over the alveolar
crest to blend with fibers of the periosteum of the bone.
Transseptal fibers. From the cervical area of one tooth across to an adjacent tooth (on
the mesial or distal only) to provide resistance to separation of teeth (Figure 12-4).
2.
Principal Fiber Groups (Figure 12-4)
The five principal groups of collagen fibers are named for their location on the root and for their
direction. They are also called the dentoalveolar fiber groups.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 6 of 31
FIGURE 12-3 Gingival Fiber Groups. Cross section of the gingiva shows the relation of
the gingival fiber groups to the gingival sulcus, the free gingiva, the cementum, and the
alveolar bone.
Apical fibers. From the root apex to adjacent surrounding bone to resist vertical forces.
Oblique fibers. From the root above the apical fibers obliquely toward the occlusal to resist
vertical and unexpected strong forces.
Horizontal fibers. From the cementum in the middle of each root to adjacent alveolar bone to
resist tipping of the tooth.
Alveolar crest fibers. From the alveolar crest to the cementum just below the cementoenamel
junction to resist intrusive forces.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 7 of 31
FIGURE 12-4 Principal Fiber Groups of the Periodontium. The five principal
groups (apical, oblique, horizontal, alveolar crest, and interradicular) are shown.
The transseptal fibers of the gingival fiber groups are also shown as they span
across from the cervical area of one tooth to the neighboring tooth.
P.216
Interradicular fibers. From cementum between the roots of multirooted teeth to the adjacent
bone to resist vertical and lateral forces.
C. Cementum
The cementum is a thin layer of calcified connective tissue that covers the tooth from the
cementoenamel junction to, and around, the apical foramen.
1.
2.
Functions
To seal the tubules of the root dentin.
To provide attachment for the periodontal fiber groups.
Characteristics
Thickness is 50 to 200 m about the apex; 30 to 60 m about the cervical area.
Vascular and nerve connections are missing; therefore, cementum is insensitive.
Relationship of enamel and cementum at the cervical area is shown in Figure 14-2 (page 257).
D. Alveolar Bone
The alveolar bone consists of the lamina dura, which surrounds the tooth socket, and the
supporting bone.
When teeth are lost, the alveolar bone is resorbed.
The bone functions to support the teeth and provide attachment for the periodontal ligament
fibers.
E. Gingiva
The part of the masticatory mucosa that surrounds the necks of the teeth and is attached to the
teeth and the alveolar bone.
The Gingiva and Related Structures
The gingiva is made up of the free gingiva, the attached gingiva, and the interdental gingiva or
interdental papilla.
I. Free Gingiva (Marginal Gingiva)
In health, the free gingiva is closely adapted around each tooth. It connects with the attached
gingiva at the free gingival groove and attaches to the tooth at the coronal portion of the junctional
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 8 of 31
epithelium (Figure 12-5).
A. Free Gingival Groove
The free gingival groove is a shallow linear groove that demarcates the free from the attached
gingiva. Generally, about one-third of the teeth show a visible gingival groove when the
gingiva is healthy.2
FIGURE 12-5 Parts of the Gingiva. Cross-sectional diagram shows the parts of the
gingiva and adjacent tissues of a partially erupted tooth. Note that the junctional
epithelium is on the enamel.
In the absence of inflammation and pocket formation, the gingival groove runs somewhat
parallel with and about 0.5 to 1.5 mm from the gingival margin,3 and it is approximately at the
level of the bottom of the gingival sulcus.
B. Oral Epithelium (outer gingival epithelium, Figure 12-6)
Covers the free gingiva from the gingival groove over the gingival margin.
Composed of keratinized stratified squamous epithelium.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 9 of 31
FIGURE 12-6 The Gingival Tissues. Cross-sectional diagram shows the histologic
relationships of the oral, sulcular, and junctional epithelia and the connective
tissue.
P.217
C. Gingival Margin (gingival crest, margin of the gingiva, or free
margin, Figure 12-5)
This is the edge of the gingiva nearest the incisal or occlusal surface.
Marks the opening of the gingival sulcus.
II. Gingival Sulcus (Crevice)
A. Location
The crevice or groove between the free gingiva and the tooth.
B. Boundaries (Figure 12-6)
1.
Inner. Tooth surface. May be the enamel, cementum, or part of each, depending on the
position of the junctional epithelium.
2.
Outer. Sulcular epithelium.
3.
Base. Coronal margin of the attached tissues. The base of the sulcus or pocket is also called
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 10 of 31
the probing depth, the depth of the sulcus, or the bottom of the pocket.
C. Sulcular Epithelium
The continuation of the oral epithelium covering the free gingiva. Sulcular epithelium is not
keratinized.
D. Depth of Sulcus
Healthy sulci are shallow and may be only 0.5 mm.
The average depth of the healthy sulcus is about 1.8 mm.4
E. Gingival Sulcus Fluid (sulcular fluid, crevicular fluid)
A serum-like fluid that seeps from the connective tissue through the epithelial lining of the
sulcus or pocket.
FIGURE 12-7 Tooth Eruption and the Gingiva. (A) Before eruption, the oral
epithelium covers the tooth. (B) As the tooth emerges, the reduced epithelium
joins the oral epithelium as the gingival sulcus is formed. (C) Partial eruption with
the junctional epithelium along the enamel. (D) Eruption complete, with junctional
epithelium at the cementoenamel junction. (E) From disease or other cause, the
attachment migrates along the root surface, exposing the cementum.
Occurrence is slight to none in a normal sulcus; increases with inflammation. It is part of the
local defense mechanism and is able to transport many substances, including endotoxins,
enzymes, antibodies, and certain systemically administered drugs.
III. Junctional Epithelium (Attachment Epithelium)
A. Description
The junctional epithelium is a cuff-like band of stratified squamous epithelium that is
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 11 of 31
continuous with the sulcular epithelium and completely encircles the tooth.
It is triangular in cross section, is widest at the junction with the sulcular epithelium, and
narrows down to the width of a few cells at the apical end.
The junctional epithelium is not keratinized. It has two basement membranes: one adjacent to
the connective tissue and one adjacent to the tooth surface.
B. Size
The junctional epithelium may be up to 15 or 20 cells in thickness where it joins the sulcular
epithelium and tapers down to 1 or 2 cells in thickness at the apical end.
The length ranges from 0.25 to 1.35 mm.
C. Position
As the tooth erupts, the attachment is on the enamel; during eruption, the epithelium migrates
toward the cementoenamel junction (Figure 12-7).
At full eruption, the attachment is usually on the cementum, where it becomes firmly attached
(Figure 12-7D).
With wear of the tooth on the incisal or occlusal surface and with periodontal infections, the
attachment migrates along the root surface (Figure 12-7E).
P.218
D. Relation of Crest of Alveolar Bone to the Attached Gingival Tissue
The distance between the base of the attachment and the crest of the alveolar bone is
approximately 1.0 to 1.5 mm.
This distance is maintained in disease when the epithelium moves along the root surface and
bone loss occurs.
E. Attachment of the Epithelium to the Tooth Surface
The junctional epithelium or attachment epithelium provides a seal at the base of the sulcus.
The attachment, or connecting interface between the tooth and the tissue, is accomplished by
hemidesmosomes and the basal lamina of the junctional epithelium.
IV. Interdental Gingiva (Interdental Papilla)
A. Location
In health, the interdental gingiva occupies the interproximal area between two adjacent teeth.
The tip and lateral borders are continuous with the free gingiva, whereas other parts are
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 12 of 31
attached gingiva.
An interproximal area is also called an embrasure. In Type 1 embrasure the gingival tissue
fills the area; in Type 2 embrasure there is slight to moderate recession of the interdental
gingiva; in Type 3 embrasure there is extensive recession or complete loss of the of the
papilla as shown in Figure 26-1 (page 431).
B. Shape
1.
Varies With Spacing or Overlapping of the Teeth. The interdental gingiva may be flat or
saddle-shaped when wide spaces are between the teeth, or it may be tapered and narrow
when the teeth are crowded or overlapped.
2.
Between Anterior Teeth. Pointed, pyramidal.
3.
Between Posterior Teeth
Flatter than anterior papillae because of wider teeth, wider contact areas, and flattened
interdental bone.
Two papillae, one facial and one lingual, connected by a col, are found when teeth are
in contact.
C. Col
1.
A col is the depression between the lingual or palatal and facial papillae that conforms to the
proximal contact area (Figure 12-8).
2.
The center of the col area is not usually keratinized and thus is more susceptible to infection.
Most periodontal infection begins in the col area.
FIGURE 12-8 Col. A col is the depression between the lingual or palatal and the facial
papillae under the contact area. The contact area is represented by the striped lines. (A)
Mesial of mandibular molar to show wide col area. (B) Mesial of mandibular incisor to
show a narrow col. The col deepens when gingival enlargement occurs.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 13 of 31
V. Attached Gingiva
A. Extent
The attached gingiva is continuous with the oral epithelium of the free gingiva and is covered
with keratinized stratified squamous epithelium.
Maxillary palatal gingiva is continuous with the palatal mucosa.
The attached gingiva of the mandibular facial and lingual gingiva and maxillary facial gingiva
is demarcated from the alveolar mucosa by the mucogingival junction.
B. Attachment
Firmly bound to the underlying cementum and alveolar bone.
C. Shape
Follows the depressions between the eminences of the roots of the teeth.
VI. Mucogingival Junction
A. Appearance
The mucogingival junction appears as a line that marks the connection between the attached
gingiva and the alveolar mucosa.
The anterior line is scalloped, but it is fairly straight posterior to the premolars.
A contrast can be seen between the pink of the keratinized, stippled, attached gingiva and the
darker alveolar mucosa.
B. Location
A mucogingival line is found on the facial surface of all quadrants and on the lingual surface
of the mandibular arch.
P.219
There is no alveolar mucosa on the palate. The palatal tissue is firmly attached to the bone of
the roof of the mouth.
The three mucogingival lines are facial mandibular, lingual mandibular, and facial maxillary.
I n F i g u r e 1 2 - 9 , t h e f a c i a l m a x i l l a r y a n d m a n d i b u l a r m u c o g i n gi v a l j u n c t i o n s a r e s h o w n i n
relation to the attached gingiva and the alveolar mucosa.
VII. Alveolar Mucosa
A. Description
Movable tissue loosely attached to the underlying bone.
It has a smooth, shiny surface with nonkeratinized, thin epithelium. Underlying vessels may be
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 14 of 31
seen through the epithelium.
B. Frena (singular: frenum or frenulum)
Description. A frenum is a narrow fold of mucous membrane that passes from a more fixed to
a movable part, for example, from the attached gingiva at the mucogingival junction to the lip,
cheek, or undersurface of the tongue. A frenum serves to check undue movement.
Locations
a.
Maxillary and mandibular anterior frena. At midlines between central incisors. Figure
12-9 shows diagrammatically the location of the anterior frena.
b.
Lingual frenum. From undersurface of the tongue.
c.
Buccal frena. In the caninepremolar areas, both maxillary and mandibular.
Attachment of Frena in Relation to the Attached Gingiva
a.
b.
Closely associated with the mucogingival junction.
When the attached gingiva is narrow or missing, the frena may pull on the free gingiva
and displace it laterally. A tension test is used to locate frenal attachments and check
the adequacy of the attached gingiva (page 239).
FIGURE 12-9 Parts of the Gingiva. The mucogingival junction for each arch
is shown in relation to the attached gingiva, alveolar mucosa, and labial
anterior frena.
The Recognition of Gingival and Periodontal Infections
I. The Clinical Examination
The recognition of normal gingiva, gingival infections, and deeper periodontal involvement depends
on a disciplined, step-by-step examination.
It is necessary to know the extent of the disease. Gingival infections are confined to the gingiva,
whereas periodontal infections include all parts of the periodontium, namely, the gingiva,
periodontal ligament, bone, and cementum.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 15 of 31
A basic examination performed to recognize the signs and effects of inflammation includes
information about at least the following markers:
Gingival tissue changes (color, size, shape, surface texture, position).
Bleeding and exudates.
Mucogingival involvement (adequate width of attached gingiva).
Probing depths; pocket formation (attachment levels).
Furcation involvement.
Dental biofilm (and calculus) present.
Mobility of teeth.
Radiographic evidence.
II. Signs and Symptoms
Patients may or may not have specific symptoms to report because periodontal infections are
insidious in development.
Symptoms the patient notices or feels may include bleeding gingiva, sometimes only while
brushing, sometimes with drooling at night, or sometimes spontaneously.
Other possible symptoms are sensitivity to hot and cold, tenderness or discomfort while eating
or pain after eating, food retained between the teeth, unpleasant mouth odors, chronic bad
taste, or a feeling that the teeth are loose. Most of these are symptoms of advanced disease.
III. Clinically Normal
The terms clinically normal or clinically healthy may be used to designate gingival tissue that is
characterized by the following:
A shade of pale or coral pink varied by complexion and pigmentation.
A knife-edged gingival margin that adapts closely around the tooth.
Stippling; firmness; and minimal sulcus depth with no bleeding when probed.
Although normal varies with anatomic, physiologic, and other factors, general characteristics form
a baseline for a contrast in the recognition of inflammation.
P.220
IV. Causes of Tissue Changes
Disease changes produce alterations in color, size, position, shape, consistency, surface
texture, bleeding readiness, and exudate production.
To understand the changes that take place in the gingival tissues during the transition from
health to disease, it is necessary to have a clear picture of what dental biofilm is, the role of
biofilm microorganisms in the development of disease, and the inflammatory response by the
body.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 16 of 31
When the products of the biofilm microorganisms cause breakdown of the intercellular
substances of the sulcular epithelium, injurious agents can pass into the connective tissue,
where an inflammatory response is initiated.
An inflammatory response means that there is increased blood flow, increased permeability of
capillaries, and increased collection of defense cells and tissue fluid.
The changes produce the tissue alterations, such as in color, size, shape, and consistency,
that are described in the next section.
V. Descriptive Terminology
The degree of severity and distribution of a change should be noted when examining the gingiva.
When a deviation from normal affects a single area, it can be designated by the number of the
adjacent tooth and the surface of the tissue involved, namely, facial, lingual, mesial, or distal.
A. Severity
Severity is expressed as slight, moderate, or severe.
B. Distribution
Terms used for describing distribution are as follows:
1.
Localized: The gingiva is involved only about a single tooth or a specific group of teeth.
2.
Generalized: The gingiva is involved about all or nearly all of the teeth throughout the mouth.
A condition may also be generalized throughout a single arch, the maxillary or mandibular.
3.
Marginal: A change that is confined to the free or marginal gingiva. This is specified as either
localized or generalized.
4.
Papillary: A change that involves a papilla but not the rest of the free gingiva around a tooth.
A papillary change may be localized or generalized.
5.
Diffuse: Spread out, dispersed; affects gingival margin, attached gingiva, and interdental
papillae; may extend into alveolar mucosa. A diffuse condition is more frequently localized,
rarely generalized.
VI. Early Recognition of Tissue Changes
Marked changes, such as moderate to severe generalized redness, enlargement, sponginess,
deep pockets, and definite mobility, are relatively easy to detect even with limited experience,
provided there is good light and accessibility for vision.
In contrast, when changes are subtle, localized about one or a few teeth, and of a lesser
degree of severity, more skillful application of knowledge is needed.
Early recognition and treatment of gingival and periodontal infections prevents neglect of
conditions that can develop into severe disease. Treatment is less complicated, and the
success of treatment and recovery to healthy tissue is predictable when early recognition
makes early treatment possible.
The Gingival Examination
The examination of the gingiva includes evaluation of color, size, shape, consistency, surface
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 17 of 31
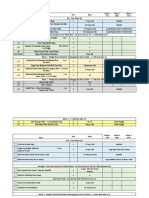
texture, position, mucogingival junctions, bleeding, and exudate. These are summarized in Table 121, which is a clinical reference chart.
I. Color
A. Signs of Health
1.
Pale Pink. Darker in people with darker complexions.
2.
Factors Influencing Color
a.
Vascular supply.
b.
Thickness of epithelium.
c.
Degree of keratinization.
d.
Physiologic pigmentation: melanin pigmentation occurs frequently in African Americans,
Asians, Indians, and Caucasians of Mediterranean countries.
B. Changes in Disease
1.
In Chronic Inflammation. Dark red, bluish red, magenta, or deep blue.
2.
In Acute Inflammation. Bright red.
3.
Extent. Deep involvement can be expected when diffuse color changes extend into the
attached gingiva, or from the marginal gingiva to the mucogingival junction, or through into
alveolar mucosa.
II. Size
A. Signs of Health
1.
Free Gingiva. Flat, not enlarged; fits snugly around the tooth.
2.
Attached Gingiva
a.
Width of attached gingiva varies among patients and among teeth for an individual, from
1 to 9 mm.5
Table 12-1 Examination of the Gingival Clinical Markers
CHANGES IN
DISEASE
APPEARANCE IN CLINICAL
HEALTH
APPEARANCE
Color
Uniformly pale
pink or coral
pink
Acute: bright
red
CAUSES FOR
CHANGES
Inflammation
Capillary
dilation
Increased
blood flow
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 18 of 31
Variations in
pigmentation
related to
complexion,
race
Chronic:
bluish pink,
bluish red
Vessels
engorged
Blood flow
sluggish
Venous return
impaired
Anoxemia
Increased
fibrosis
Attached
gingiva: color
change may
extend to the
mucogingival
line
Deepening of
pocket,
mucogingival
involvement
Size
Not enlarged
Fits snugly
around the
tooth
Enlarged
Edematous:
inflammatory
fluid, cellular
exudate,
vascular
engorgement,
hemorrhage
Fibrotic: new
collagen
fibers
Shape
(contour)
Marginal
gingiva: knifeedged, flat,
follows a curved
line about the
tooth
Marginal
gingiva:
rounded
rolled
Inflammatory
changes:
edematous or
fibrous
Papillae:
(1)normal
contact: papilla
is pointed and
pyramidal; fills
the
interproximal
area
Papillae:
bulbous
flattened
blunted
cratered
Bulbous with
gingival
enlargement
(see
edematous
and fibrotic,
above)
(2)space
(diastema)
between teeth;
gingiva is flat or
saddle shaped
Cratered in
necrotizing
ulcerative
gingivitis
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 19 of 31
Consistency
Surface
Texture
Position of
Gingival
Margin
Firm
Attached
gingiva firmly
bound down
Soft, spongy:
dents readily
when
pressed with
probe
Associated
with red
color, smooth
shiny
surface, loss
of stippling,
bleeding on
probing
Edematous:
fluid between
cells in
connective
tissue
Firm, hard:
resists probe
pressure
Associated
with pink
color,
stippling,
bleeding only
in depth of
pocket
Fibrotic:
collagen
fibers
Free gingiva:
smooth
Acute
condition:
smooth,
shiny gingiva
Inflammatory
changes in
the
connective
tissue;
edema,
cellular
infiltration
Attached
gingiva: stippled
Chronic:
hard, firm,
with stippling,
sometimes
heavier than
normal
Fibrosis
Fully erupted
tooth: margin is
12 mm above
cementoenamel
junction, at or
slightly below
the enamel
contour
Enlarged
gingiva:
margin is
higher on the
tooth, above
normal,
pocket
deepened
Recession:
Edematous or
fibrotic
Junctional
epithelium
has migrated
along the
root; gingival
margin
follows
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 20 of 31
margin is
more apical;
root surface
is exposed
Position of
Junctional
Epithelium
During eruption
along the
enamel surface
(Figure 12-7)
Fully erupted
tooth: the
junctional
epithelium is at
the
cementoenamel
junction
Position
determined
by use of
probe, is on
the root
surface
Apical
migration of
the epithelium
along the root
Mucogingival
Junctions
Make clear
demarcation
between the
pink, stippled,
attached
gingiva and the
darker alveolar
mucosa with
smooth shiny
surface
No attached
gingiva:
(1) Color
changes may
extend full
height of the
gingiva;
mucogingival
line
obliterated
(2) Probing
reveals that
the bottom of
the pocket
extends into
the alveolar
mucosa
(3) Frenal
pull may
displace the
gingival
margin from
the tooth
Apical
migration of
the junctional
epithelium
Attached
gingiva
decreases
with pocket
deepening
Inflammation
extends into
alveolar
mucosa
Bleeding
No
spontaneous
bleeding or
upon probing
Spontaneous
bleeding
Bleeding on
probing:
bleeding
near margin
in acute
condition;
bleeding
deep in
Degeneration
of the sulcular
epithelium
with the
formation of
pocket
epithelium
Blood vessels
engorged
Tissue
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 21 of 31
Exudate
No exudate
expressed on
pressure
pocket in
chronic
condition
edematous
White fluid,
pus, visible
on digital
pressure
Amount not
related to
pocket depth
Inflammation
in the
connective
tissue
Excessive
accumulation
of white blood
cells with
serum and
tissue makes
up the
exudate (pus)
P.221
P.222
b.
W i d e r i n m a x i l l a t h a n m a n d i b le ; b r o a d e s t z o n e r e l a t e d t o i n c i s o r s , n a r r o w e s t a t t h e
canine and premolar regions.
B. Changes in Disease
1.
Free Gingiva and Papillae. Become enlarged. May be localized or limited to specific areas or
generalized throughout the gingiva. The col deepens as the papillae increase in size.
2.
Attached Gingiva. Decreases in amount as the pocket deepens.
C. Enlargement From Drug Therapy
Certain drugs used for specific systemic therapy cause gingival enlargement as a side effect.
Examples of such drugs are phenytoin, cyclosporine, and nifedipine.
III. Shape (Form or Contour)
A. Signs of Health
1.
Free Gingiva
a.
Follows a curved line around each tooth; may be straighter along wide molar surfaces.
b.
The margin is knife-edged or slightly rounded on facial and lingual gingiva; closely
adapted to the tooth surface.
2.
Papillae
a.
Teeth with contact area. Facial and lingual gingiva are pointed or slightly rounded
papillae with a col area under the contact (Figure 12-8).
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 22 of 31
b.
Spaced teeth (with diastemata). Interdental gingiva is flat or saddle shaped.
B. Changes in Disease
1.
Free Gingiva. Rounded or rolled.
2.
Papillae. Blunted, flattened, bulbous, cratered (Figure 12-10).
3.
Festoon (McCall's festoon). An enlargement of the marginal gingiva with the formation of a
lifesaver-like gingival prominence. Frequently, the total gingiva is very narrow, with
associated apparent recession, as shown in Figure 12-10D.
4.
Clefts
a.
Stillman's cleft (Figure 12-11). A localized recession may be V-shaped, apostropheshaped, or form a slitlike indentation. It may extend several millimeters toward the
mucogingival junction or even to or through the junction.
P.223
b.
Floss cleft. A cleft created by incorrect floss positioning appears as a vertical linear or
V-shaped fissure in the marginal gingiva.6 It usually occurs at one side of an interdental
papilla. The injury can develop when dental floss is curved repeatedly in an incomplete
C around the line angle so the floss is pressed across the gingiva.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 23 of 31
FIGURE 12-10 Gingival Shape or Contour. (A) Blunted papillae. (B) Bulbous papillae.
(C) Cratered papillae. (D) Rolled, lifesaver-shaped McCall's festoons.
IV. Consistency
A. Signs of Health
1.
Firm when palpated with the side of a blunt instrument (probe).
2.
Attached gingiva is bound down firmly to the underlying bone.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 24 of 31
B. Changes in Disease
1.
To Determine Consistency. Gently press side of probe on free gingiva. Soft, spongy gingiva
dents readily; firm, hard tissue resists.
2.
Soft, Spongy Gingiva. Related to acute stages of inflammation with increased infiltration of
fluid and inflammatory elements. The tissue appears red, may be smooth and shiny with loss
of stippling, has marginal enlargement, and bleeds readily on probing.
3.
Firm, Hard Gingiva. Related to chronic inflammation with increased fibrosis. The tissue may
appear pink and well stippled. Bleeding, when probed, usually occurs only in the deeper part
of a pocket, not near the margin.
4.
Retraction of the Margin Away From the Tooth. Normally, the free gingiva fits snugly about the
tooth. When the margin tends to hang slightly away or is readily displaced with a light air
blast, the gingival fibers that support the margin have been destroyed (Figure 12-3).
V. Surface Texture
A. Signs of Health
1.
Free Gingiva. Smooth.
2.
Attached Gingiva. Stippled (minutely pebbled or orange peel surface).
3.
Interdental Gingiva. The free gingiva is smooth; the center portion of each papilla is stippled.
B. Changes in Disease
1.
Inflammatory Changes. May be loss of stippling, with smooth, shiny surface.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 25 of 31
FIGURE 12-11 Gingival Clefts. (A) V-shaped Stillman's cleft. (B) Slit-like Stillman's
clefts of varying degrees of severity in relation to the mucogingival junction.
P.224
2.
Hyperkeratosis. May result in a leathery, hard, or nodular surface.
FIGURE 12-12 Gingival Recession. Left, Clinically visible recession of the gingival
margin with root surface apparent to the eye. Right, The actual recession exposes
the root surface as the periodontal attachment migrates along the root surface.
3.
Chronic Disease. Tissue may be hard and fibrotic, with a normal pink color and normal or
deep stippling.
VI. Position
The actual position of the gingiva is the level of the attached periodontal tissue. It is not directly
visible but can be determined by probing.
The apparent position of the gingiva is the level of the gingival margin or crest of the free gingiva
that is seen by direct observation.
A. Signs of Health
For the fully erupted tooth in an adult, the apparent position of the gingival margin is normally at the
level of, or slightly below, the enamel contour or prominence of the cervical third of a tooth.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 26 of 31
FIGURE 12-13 Localized Recession. A single tooth may show narrow or wide, deep or
shallow recession. (A) Wide, shallow. (B) Wide, deep, with narrow attached gingiva. (C)
Narrow, deep, with missing attached gingiva.
B. Changes in Disease
1.
Effect of Gingival Enlargement. When the gingiva enlarges, the gingival margin may be high
on the enamel, partly or nearly covering the anatomic crown.
2.
Effect of Gingival Recession
a.
Definition. Recession is the exposure of root surface that results from the apical
migration of the junctional epithelium (Figure 12-12).
b.
Actual recession. The actual recession is shown by the position of the attachment level.
The receded area is from the cementoenamel junction to the attachment.
c.
Visible recession. The visible recession is the exposed root surface that is visible on
clinical examination. It is seen from the gingival margin to the cementoenamel junction.
d.
Localized recession (Figure 12-13). A localized recession may be narrow or wide, deep
or shallow. The root surface is denuded, and the visible recession may extend to or
through the mucogingival junction.
e.
Measurement. Both actual and visible recession can be measured with a probe from the
cementoenamel junction. Total recession is the actual and visible positions added
together.
VII. Bleeding
A. Signs of Health
1.
No bleeding spontaneously or on probing.
2.
Healthy tissue does not bleed.
B. Changes in Disease
1.
Bleeding occurs spontaneously or when probed.
2.
Sulcular epithelium becomes diseased pocket epithelium. The ulcerated pocket wall bleeds
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 27 of 31
readily on gentle probing.
P.225
VIII. Exudate
A. Signs of Health
There is no exudate except slight gingival sulcus fluid. Gingival sulcus fluid cannot be seen by
direct observation.
B. Changes in Disease
1.
Increased gingival sulcus fluid.
2.
Amount of exudate is not an indicator of the extent of disease or the depth of the periodontal
pockets.
The Gingiva of Young Children7 , 8
I. Signs of Health
A. Primary Dentition
1.
Color. Pink or slightly red.
2.
Shape. Thick, rounded, or rolled.
3.
Consistency. Less fibrous than adult gingiva; not tightly adapted to the teeth; may be easily
displaced with a light air jet.
4.
Surface Texture. May or may not have stippling; high percentage of patients has shiny
gingiva.
5.
Attached Gingiva. Width of attached gingiva in children aged 3 to 5 years: between 1 and 6
mm.5
6.
Interdental Gingiva
a.
b.
Anterior: diastemata are frequently present and the papillae are flat or saddle shaped.
Posterior: col between facial and lingual papillae when teeth are in contact (Figure 128).
E veryda y Ethi cs
Britain and Nicholas were first-year dental hygiene students just beginning to practice on each
other as student partners in the preclinic program. During the oral examination, Britain noticed
that Nicholas had some areas of bleeding and changes in the contour of the marginal gingiva. In
general, the soft tissue seemed more sponge-like and loose, but Britain was not sure she clearly
understood what is considered normal, remembering that the clinical instructor often referred
to a range of normal.
Britain decided to focus on and document the areas that were pale pink, firm, and pointed in the
interproximal areas. She carefully recorded this information with great detail and then signaled
for her instructor to verify the findings. When the instructor sat down and reviewed the
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 28 of 31
examination she was pleased with Britain's thoroughness. The instructor provided positive
feedback and quickly moved on to the next pair of students. Britain began to feel uneasy that
she hadn't pointed out the gingival tissues that she thought were possibly inflamed.
Q uestion s for C onsider ation
1.
Explain how the ethical principles of autonomy, beneficence, and veracity apply to this
situation.
2.
Indicate how Nicholas is the center of this dilemma both from the perspective of Britain, a
student, and the clinical instructor who finds out from another faculty member that he or
she thinks Nicholas has definite signs of periodontal disease.
3.
Ethically, what alternatives or actions can Britain take at this time to address the uneasy
feeling she has about Nicholas' gingival status?
B. Mixed Dentition
Constant state of change related to exfoliation and eruption.
Free gingiva may appear rolled or rounded, slightly reddened, shiny, and with a lack of
firmness.
The gingiva covers a varying portion of the anatomic crown, depending on the stage of
eruption (Figure 12-7).
II. Changes in Disease
Examination of the periodontal tissues of a child is not different from that of an adult. A complete
examination is necessary, including probing around each tooth.
Gingivitis occurs frequently in children but is usually reversible without leaving permanent damage.
Although relatively rare, periodontitis can occur in primary dentition.
Mucogingival problems occur in children.9,10 The recognition of deficiencies of attached gingiva has
particular significance for the child who will need orthodontic treatment.
The Gingiva after Periodontal Surgery
The characteristics of normal healthy gingiva take on different dimensions for the patient who has
completed treatment for pockets, bone loss, and other signs of a periodontal infection. The
junctional epithelium is apical to the cementoenamel junction. After healing, the sulcus
P.226
depths may be within normal range and no bleeding occurs when probed.
Depending on the exact treatment performed, examination shows changes from the initial
evaluation. For example, where the initial examination showed a deficiency of attached gingiva with
frenal pull, mucogingival surgery may have been designed and treatment satisfactorily completed to
create new attached gingiva. With each maintenance appointment, a thorough, careful examination
is necessary to control factors that may permit recurrence of disease.
Factors To Teach The Patient
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 29 of 31
C haract eristi cs of normal healt hy gin giva.
Th e sig nifica nce o f blee ding; healt hy tis sue d oes no t ble ed.
R elatio nship of fi ndings durin g a g ingiva l exam inatio n to t he pe rsonal daily care
p rocedu res f or inf ection contr ol.
Th e spe cial a ttent ion ne eded for an area of gi ngival reces sion t o pre vent a brasio n,
i nflamma tion, and fu rther involv ement.
H ow the metho d of b rushin g, sti ffnes s of t oothb rush f ilament s, ab rasive ness o f a
d entifr ice, a nd pr essure appli ed du ring b rushin g can be fa ctors in gin gival reces sion.
References
1. Avery, J.K. and Steele, P.F.: Essentials of Oral Histology and Embryology: A Clinical
Approach. St. Louis, Mosby, 1992, pp. 131134.
2. Ainamo, J. and Le, H.: Anatomical Characteristics of Gingiva: A Clinical and Microscopic
Study of the Free and Attached Gingiva, J. Periodontol., 37, 5, JanuaryFebruary, 1966.
3. Orban, B.: Clinical and Histologic Study of the Surface Characteristics of the Gingiva, Oral
Surg. Oral Med. Oral Pathol., 1, 827, September, 1948.
4. Bhaskar, S.N., ed.: Orban's Oral Histology and Embryology, 11th ed. St. Louis, Mosby, 1991,
pp. 323325.
5 . B o w e r s , G . M .: A S t u d y o f t h e W i d t h o f A t t a c h e d G i n g i v a , J . P e r i o d o n t o l . , 3 4 , 2 0 1 , M a y , 1 9 6 3 .
6. Hallman, W.W., Waldrop, T.C., Houston, G.D., and Hawkins, B.F.: Flossing Clefts: Clinical
and Histologic Observations, J. Periodontol., 57, 501, August, 1986.
7. Duperon, D. and Takei, H.H.: Gingival Diseases in Childhood, in Newman, M.G., Takei, H.H.,
Klokkevold, P.R., and Carranza, F.A.: Carranza's Clinical Periodontics, 10th ed. St Louis,
Saunders/Elsevier, 2006, pp. 404410.
8. Casamassimo, P.S.: Periodontal Conditions, in Pinkham, J.R., ed.: Pediatric Dentistry:
Infancy Through Adolescence, 2nd ed. Philadelphia, W.B. Saunders Co., 1994, pp. 353357,
607615.
9. Maynard, J.G. and Ochsenbein, C.: Mucogingival Problems, Prevalence and Therapy in
Children, J. Periodontol., 46, 543, September, 1975.
10. Andlin-Sobocki, A., Marcusson, A., and Persson, M.: 3-Year Observations on Gingival
Recession in Mandibular Incisors in Children, J. Clin. Periodontol., 18, 155, March, 1991.
Suggested Readings
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 30 of 31
Ainamo, A., Ainamo, J., and Poikkeus, R.: Continuous Widening of the Band of Attached
Gingiva From 23 to 65 Years of Age, J. Periodont. Res., 16, 595, November, 1981.
Fedi, P.F., Vernino, A.R., and Gray, J.L.: The Periodontic Syllabus, 4th ed. Baltimore,
Lippincott Williams & Wilkins, 2000, pp. 113.
G r a n t , D . A ., S t e r n , I . B . , a n d L i s t g a r t e n , M . A . , e d s . : P e r i o d o n t i c s , 6 t h e d . S t . L o u i s , M o s b y ,
1988, pp. 375.
Hassell, T.M.: Tissues and Cells of the Periodontium, Periodontol. 2000, 3, 9, 1993.
Hempton, T.J., Wilkins, E., and Lancaster, D.: Evaluation of Attached Tissue Aids in Treatment
of Recession, RDH, 16, 34, June, 1996.
Mariotti, A.: The Extracellular Matrix of the Periodontium: Dynamic and Interactive Tissues,
Periodontol. 2000, 3, 39, 1993.
Melfi, R.C. and Alley, K.E.: Permar's Oral Embryology and Microscopic Anatomy, 10th ed.
Philadelphia, Lippincott Williams & Wilkins, 2000, pp. 237251.
Serino, G., Wennstrm, J.L., Lindhe, J., and Eneroth, L.: The Prevalence and Distribution of
G i n g i v a l R e c e s s i o n i n S u b j e c t s W i t h a H i g h S t a n d a r d o f O r a l H y g i e n e , J . C l i n . P e r i o d o n t o l ., 2 1 ,
57, January, 1994.
Vacek, J.S., Gher, M.E., Assad, D.A., Richardson, A.C., and Giambarresi, L.I.: The Dimensions
of the Human Dentogingival Junction, Int. J. Periodont. Restorative Dent., 14, 155, Number 2,
1994.
Gingiva of Children
American Academy of Periodontology, Committee on Research, Science and Therapy:
Position Paper: Periodontal Diseases of Children and Adolescents, J. Periodontol., 67, 57,
January, 1996.
Andlin-Sobocki, A.: Changes of Facial Gingival Dimensions in Children: A 2-year Longitudinal
Study, J. Clin. Periodontol., 20, 212, March, 1993.
Andlin-Sobocki, A. and Bodin, L.: Dimensional Alterations of the Gingiva Related to Changes
of Facial/Lingual Tooth Position in Permanent Anterior Teeth of Children: A 2-year Longitudinal
Study. J. Clin. Periodontol., 20, 218, March, 1993.
Bimstein, E. and Eidelman, E.: Longitudinal Changes in the Width of Attached Gingiva in
Children, Pediatr. Dent., 10, 22, March, 1988.
Bimstein, E., Machtei, E., and Eidelman, E.: Dimensional Differences in the Attached and
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Page 31 of 31
Keratinized Gingiva and Gingival Sulcus in the Early Permanent Dentition: A Longitudinal
Study, J. Pedod., 10, 247, Spring, 1986.
Bimstein, E., Matsson, L., Soskolne, A.W., and Lustman, J.: Histologic Characteristics of the
Gingiva Associated With the Primary and Permanent Teeth of Children, Pediatr. Dent., 16, 206,
May/June, 1994.
Keszthelyi, G.: The Width of Plaque-Free Zones on Primary Molars With Attachment Loss, J.
Clin. Periodontol., 18, 94, February, 1991.
Saario, M., Ainamo, A., Mattila, K., and Ainamo, J.: The Width of Radiologically Defined
Attached Gingiva Over Permanent Teeth in Children, J. Clin. Periodontol., 21, 666, November,
1994.
Saario, M., Ainamo, A., Mattila, K., Suomalainen, K., and Ainamo, J.: The Width of
Radiologically Defined Attached Gingiva Over Deciduous Teeth, J. Clin. Periodontol., 22, 895,
December, 1995.
Tenenbaum, H. and Tenenbaum, M.: A Clinical Study of the Width of the Attached Gingiva in
the Deciduous, Transitional and Permanent Dentitions, J. Clin. Periodontol., 13, 270, April,
1986.
http://pt.wkhealth.com/pt/re/9780781763226/bookContentPane_frame.htm;jsessionid=MQ... 11/2/2010
Potrebbero piacerti anche
- The Periodontal Pocket PDFDocumento9 pagineThe Periodontal Pocket PDFIgnacio PulleyNessuna valutazione finora
- Oral Wound Healing: Cell Biology and Clinical ManagementDa EverandOral Wound Healing: Cell Biology and Clinical ManagementHannu LarjavaNessuna valutazione finora
- Basic TxPlanning-Prognosis and Treatment Planning-Revised 9 September 2014Documento54 pagineBasic TxPlanning-Prognosis and Treatment Planning-Revised 9 September 2014DraspiNessuna valutazione finora
- Gingival EnlargementDocumento74 pagineGingival EnlargementSarita Diwakar100% (2)
- Perio Endo LesionsDocumento39 paginePerio Endo Lesionsthanhchon100% (17)
- Gingival Diseases - Their Aetiology, Prevention and Treatment PDFDocumento246 pagineGingival Diseases - Their Aetiology, Prevention and Treatment PDFnaresh sharma0% (1)
- Ultrasonic Scaling: Associated Risks.: Review ArticleDocumento5 pagineUltrasonic Scaling: Associated Risks.: Review Articlevivi alfiyani noorNessuna valutazione finora
- Review Article: Diagnostic Features of Common Oral Ulcerative Lesions: An Updated Decision TreeDocumento15 pagineReview Article: Diagnostic Features of Common Oral Ulcerative Lesions: An Updated Decision TreemutiaNessuna valutazione finora
- PERIODONTAL POCKET DEFINITION AND CLASSIFICATIONDocumento6 paginePERIODONTAL POCKET DEFINITION AND CLASSIFICATIONManoj Kn100% (1)
- Perio-Prog Class 2012Documento80 paginePerio-Prog Class 2012moorenNessuna valutazione finora
- Dentin Hypersensitivity2 PDFDocumento5 pagineDentin Hypersensitivity2 PDFIvan TerresNessuna valutazione finora
- Bone Loss &Documento30 pagineBone Loss &AME DENTAL COLLEGE RAICHUR, KARNATAKANessuna valutazione finora
- Nonsurgical Periodontal Therapy DCNADocumento12 pagineNonsurgical Periodontal Therapy DCNAdhwanit31Nessuna valutazione finora
- Desquamative GingivitisDocumento6 pagineDesquamative Gingivitissidra malikNessuna valutazione finora
- 4 - The Periodontium (Mahmoud Bakr)Documento128 pagine4 - The Periodontium (Mahmoud Bakr)MobarobberNessuna valutazione finora
- Cementum EhtishamDocumento102 pagineCementum EhtishamHannasa R JNessuna valutazione finora
- Laser Periodontitis Therapy Reduces BacteriaDocumento7 pagineLaser Periodontitis Therapy Reduces BacteriarindaNessuna valutazione finora
- 08 - Salivary Biomarkers A Periodontal OverviewDocumento6 pagine08 - Salivary Biomarkers A Periodontal OverviewFisaNessuna valutazione finora
- Cementum PDFDocumento12 pagineCementum PDFHafra AminiNessuna valutazione finora
- Bone Loss and Patterns of Bone DestructionDocumento75 pagineBone Loss and Patterns of Bone DestructionmunnabjujjiNessuna valutazione finora
- Immunology of Periodontal DiseasesDocumento9 pagineImmunology of Periodontal DiseasesoladunniNessuna valutazione finora
- Advanced Microbial Diagnostic TechniquesDocumento38 pagineAdvanced Microbial Diagnostic TechniquesPiyusha SharmaNessuna valutazione finora
- Effect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisDocumento5 pagineEffect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisKanagavalli VijayakumarNessuna valutazione finora
- Dentin Hypersensitivity: Understanding the Mechanism and ManagementDocumento4 pagineDentin Hypersensitivity: Understanding the Mechanism and Managementmohamed saadNessuna valutazione finora
- Time To Shift - From Scaling and Root Planing To Root Surface DebridementDocumento5 pagineTime To Shift - From Scaling and Root Planing To Root Surface DebridementYing Yi TeoNessuna valutazione finora
- Gingival Biotype Determines Periodontal Disease and Treatment OutcomesDocumento6 pagineGingival Biotype Determines Periodontal Disease and Treatment Outcomesilich sevillaNessuna valutazione finora
- 118raspadores Ultrasonicos2 PDFDocumento11 pagine118raspadores Ultrasonicos2 PDFYaneth Cristina Morales BlasNessuna valutazione finora
- Folic Acid and Periodontal Disease PDFDocumento8 pagineFolic Acid and Periodontal Disease PDFAnonymous 8raPGW1tLNessuna valutazione finora
- Dentogingival UnitDocumento53 pagineDentogingival Unitperiodontics0780% (5)
- Role of Antimcrobial Agents in Periodontal TherapyA Review On Prevailing TreatmentModalitiesDocumento5 pagineRole of Antimcrobial Agents in Periodontal TherapyA Review On Prevailing TreatmentModalitiesInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Indices PerioDocumento15 pagineIndices PerioJunaid100% (2)
- Dry Mouth (Xerostomia)Documento18 pagineDry Mouth (Xerostomia)dr_jamal1983Nessuna valutazione finora
- Random Control TrialDocumento6 pagineRandom Control TrialKarabaugilaEntertainmenTNessuna valutazione finora
- Shalu Bathla - Chronic PeriodontitisDocumento6 pagineShalu Bathla - Chronic PeriodontitisFerdinan PasaribuNessuna valutazione finora
- GINGIVA (2) / Orthodontic Courses by Indian Dental AcademyDocumento21 pagineGINGIVA (2) / Orthodontic Courses by Indian Dental Academyindian dental academyNessuna valutazione finora
- #1 Rationale ImplantDocumento5 pagine#1 Rationale Implantsohaib197Nessuna valutazione finora
- Role of Occlusion in Periodontal Disease Etiology and TreatmentDocumento6 pagineRole of Occlusion in Periodontal Disease Etiology and TreatmentKyoko CPNessuna valutazione finora
- Gingival Enlargement: Drg. Ade Ismail A. K.,MDSCDocumento31 pagineGingival Enlargement: Drg. Ade Ismail A. K.,MDSCFina AkmaliaNessuna valutazione finora
- Maxillary Odontogenic Tumor IdentificationDocumento17 pagineMaxillary Odontogenic Tumor Identificationsamhita100% (1)
- AggressiveDocumento55 pagineAggressiveSaima KhanNessuna valutazione finora
- 4phase II Periodontal TherapyDocumento76 pagine4phase II Periodontal TherapyKaraz StudiosNessuna valutazione finora
- Biologic WidthDocumento26 pagineBiologic Widthbhasalepooja67% (3)
- The Biologic Width: - A Concept in Periodontics and Restorative DentistryDocumento8 pagineThe Biologic Width: - A Concept in Periodontics and Restorative DentistryDrKrishna DasNessuna valutazione finora
- Anatomy and Microstructure of PeriodontiumDocumento9 pagineAnatomy and Microstructure of PeriodontiumAnonymous k8rDEsJsU1100% (1)
- Dental Plaque PresentationDocumento10 pagineDental Plaque PresentationHeshamNessuna valutazione finora
- Vitamin CDocumento8 pagineVitamin CArjuna BuduhNessuna valutazione finora
- Gingival EpitheliumDocumento20 pagineGingival EpitheliumPoojan ThakoreNessuna valutazione finora
- Perio Case HistoryDocumento90 paginePerio Case HistoryMoola Bharath ReddyNessuna valutazione finora
- Dental Plaque: By:-Raina J. P. Khanam Post Graduate 2 Year Dept. of Periodontics and ImplantologyDocumento69 pagineDental Plaque: By:-Raina J. P. Khanam Post Graduate 2 Year Dept. of Periodontics and ImplantologyAtul KoundelNessuna valutazione finora
- Development of PeriodontiumDocumento24 pagineDevelopment of Periodontiumpalak sharma100% (1)
- The TongueDocumento21 pagineThe Tonguemanojchouhan2014Nessuna valutazione finora
- E-1-Osteoporosis and Periodontitis 2016Documento14 pagineE-1-Osteoporosis and Periodontitis 2016Yessid Baltazar Arango100% (1)
- DENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideDa EverandDENTAL AUXILIARY EDUCATION EXAMINATION IN DENTAL MATERIALS: Passbooks Study GuideNessuna valutazione finora
- Interpretation Basics of Cone Beam Computed TomographyDa EverandInterpretation Basics of Cone Beam Computed TomographyValutazione: 4 su 5 stelle4/5 (1)
- Atlas of Topographical and Pathotopographical Anatomy of the Head and NeckDa EverandAtlas of Topographical and Pathotopographical Anatomy of the Head and NeckNessuna valutazione finora
- Diabetes Mellitus: Impact on Bone, Dental and Musculoskeletal HealthDa EverandDiabetes Mellitus: Impact on Bone, Dental and Musculoskeletal HealthMeng Hee TanNessuna valutazione finora
- Non-Subsidised Programmes Singapore Citizen $ Singapore PR $ International Student $Documento1 paginaNon-Subsidised Programmes Singapore Citizen $ Singapore PR $ International Student $velangniNessuna valutazione finora
- Academic Calendar 2021Documento1 paginaAcademic Calendar 2021velangniNessuna valutazione finora
- 2021 Non-Tuition Fees For Igcse Prep Courses: Relevant Fees Singapore-Based Students International StudentsDocumento4 pagine2021 Non-Tuition Fees For Igcse Prep Courses: Relevant Fees Singapore-Based Students International StudentsvelangniNessuna valutazione finora
- Visual Business AnalyticsDocumento9 pagineVisual Business AnalyticsvelangniNessuna valutazione finora
- Sentosa Islander Membership FAQsDocumento10 pagineSentosa Islander Membership FAQsvelangniNessuna valutazione finora
- Art - 253A10.1007 - 252Fs00595 015 1236 XDocumento18 pagineArt - 253A10.1007 - 252Fs00595 015 1236 XvelangniNessuna valutazione finora
- Year 2022 Programme Fees: Programme Singapore Citizen/ Permanent Residents Other ResidentsDocumento4 pagineYear 2022 Programme Fees: Programme Singapore Citizen/ Permanent Residents Other ResidentsvelangniNessuna valutazione finora
- SAS VA 7.5/8.3 Analysis and Design Practice QuestionsDocumento9 pagineSAS VA 7.5/8.3 Analysis and Design Practice QuestionsvelangniNessuna valutazione finora
- Family Fun For The Holidays Parent KitDocumento5 pagineFamily Fun For The Holidays Parent KitvelangniNessuna valutazione finora
- Computer Science Prospectus 2021Documento16 pagineComputer Science Prospectus 2021velangniNessuna valutazione finora
- 2020 P1 Orientation Combined SlideDocumento103 pagine2020 P1 Orientation Combined SlidevelangniNessuna valutazione finora
- Medical Claims Authorisation FormDocumento11 pagineMedical Claims Authorisation FormvelangniNessuna valutazione finora
- Data Science and Analytics in Healthcare and Public Health: FacultyDocumento1 paginaData Science and Analytics in Healthcare and Public Health: FacultyvelangniNessuna valutazione finora
- P1 2021 Booklist DistributedDocumento2 pagineP1 2021 Booklist DistributedvelangniNessuna valutazione finora
- FAQs OCI RegistrationDocumento9 pagineFAQs OCI RegistrationGagan KashyapNessuna valutazione finora
- GeriatryDocumento5 pagineGeriatryvelangniNessuna valutazione finora
- Top cyber security risks facing healthcare industryDocumento5 pagineTop cyber security risks facing healthcare industryvelangniNessuna valutazione finora
- Mikhy Brochez Found Guilty of Trying To Extort Singapore Government in HIV Registry Leak TrialDocumento4 pagineMikhy Brochez Found Guilty of Trying To Extort Singapore Government in HIV Registry Leak TrialvelangniNessuna valutazione finora
- Covishield Information Fact SheetDocumento5 pagineCovishield Information Fact SheetvelangniNessuna valutazione finora
- Flyer The Queens Commonwealth Essay Competition 2021Documento2 pagineFlyer The Queens Commonwealth Essay Competition 2021velangniNessuna valutazione finora
- Parkway Shenton Ehs Packages-2020-English-1Documento12 pagineParkway Shenton Ehs Packages-2020-English-1velangniNessuna valutazione finora
- IT Brochure 05 2021view OnlyDocumento20 pagineIT Brochure 05 2021view OnlyvelangniNessuna valutazione finora
- Personal Information of More Than 800,000 Blood Donors Exposed Online by Tech Vendor: HSADocumento4 paginePersonal Information of More Than 800,000 Blood Donors Exposed Online by Tech Vendor: HSAvelangniNessuna valutazione finora
- 2008 Y Older Teeth, Gums and Other Oral Bits 20may MGussyDocumento10 pagine2008 Y Older Teeth, Gums and Other Oral Bits 20may MGussyvelangniNessuna valutazione finora
- SSHSPH PhD/MSc Online AppDocumento14 pagineSSHSPH PhD/MSc Online AppvelangniNessuna valutazione finora
- Lanai Medical Centre Success StoryDocumento10 pagineLanai Medical Centre Success StoryvelangniNessuna valutazione finora
- AIC CHAS Brochure English - DN4 - NCDocumento2 pagineAIC CHAS Brochure English - DN4 - NCvelangniNessuna valutazione finora
- Humanitrian CrisisDocumento4 pagineHumanitrian CrisisvelangniNessuna valutazione finora
- SRFAC BCLS+AED and CPR (MTM) +AED Manual (2018) PDFDocumento97 pagineSRFAC BCLS+AED and CPR (MTM) +AED Manual (2018) PDFmadworld26Nessuna valutazione finora
- Engage TB TMslides PDFDocumento188 pagineEngage TB TMslides PDFvelangniNessuna valutazione finora
- Explorace GamesDocumento2 pagineExplorace GamesDexi Chen100% (1)
- Thyroid Function TestingDocumento12 pagineThyroid Function TestingDewi Paramita YuniarahmiNessuna valutazione finora
- Acsm Personal Trainer Exam Study GuideDocumento18 pagineAcsm Personal Trainer Exam Study GuideHong Ye100% (1)
- Endotracheal Intubation: Angel Ann G. Talento Bsn-IvDocumento39 pagineEndotracheal Intubation: Angel Ann G. Talento Bsn-IvKaren Kate AblesNessuna valutazione finora
- Physiology Lecture 9 Q-Bank (Smooth Muscle Structure, Contraction, and Relationships)Documento5 paginePhysiology Lecture 9 Q-Bank (Smooth Muscle Structure, Contraction, and Relationships)ChrisOrtNessuna valutazione finora
- Nerve Fiber Classification and Regeneration GuideDocumento15 pagineNerve Fiber Classification and Regeneration GuidehemnikilNessuna valutazione finora
- The Skeletal System HDocumento23 pagineThe Skeletal System HRajorshi MishraNessuna valutazione finora
- Nerve and Spinal Cord BiomechanicsDocumento65 pagineNerve and Spinal Cord BiomechanicsZinneRah RahManNessuna valutazione finora
- Active Anti Shear Device For Knee RehabiDocumento94 pagineActive Anti Shear Device For Knee Rehabiаримотома аримотомаNessuna valutazione finora
- The AbdomenDocumento30 pagineThe AbdomenMaxamed Faarax XaashiNessuna valutazione finora
- Trauma Tulang Belakang-Ppgd - Dr. YoyosDocumento57 pagineTrauma Tulang Belakang-Ppgd - Dr. YoyoszaroziNessuna valutazione finora
- (11.10) Imaging of The Endocrine System (TG1-CG14) Final VersionDocumento12 pagine(11.10) Imaging of The Endocrine System (TG1-CG14) Final VersionLANCE GILL TolentinoNessuna valutazione finora
- Anatomy and Types of Orofacial CleftsDocumento19 pagineAnatomy and Types of Orofacial CleftsTj AngelaNessuna valutazione finora
- ECG Project ReportDocumento22 pagineECG Project ReportEr Sunil Kumar82% (11)
- Bowflex Xtreme 2 SE Home Gym ManualDocumento92 pagineBowflex Xtreme 2 SE Home Gym ManualBest Home Gym100% (1)
- Trauma-Trauma Medula SpinalisDocumento33 pagineTrauma-Trauma Medula SpinalisHendricNessuna valutazione finora
- Diploma Lab manual-HB-IIDocumento103 pagineDiploma Lab manual-HB-IIvanshNessuna valutazione finora
- Anatomy Lower Limb by DR AzamDocumento19 pagineAnatomy Lower Limb by DR AzamroulprayashNessuna valutazione finora
- Cervical Disc ProlapseDocumento27 pagineCervical Disc ProlapseMaroofAliNessuna valutazione finora
- CDDocumento3 pagineCDMeireza AdityaNessuna valutazione finora
- Program Forta 3 Saptamani 3 ZileDocumento5 pagineProgram Forta 3 Saptamani 3 ZileIoan-Alexandru CodarceaNessuna valutazione finora
- Ex - Neuro LLDocumento3 pagineEx - Neuro LLssNessuna valutazione finora
- Anatomy 7 Lecture NotesDocumento12 pagineAnatomy 7 Lecture NotesarunNessuna valutazione finora
- Thyroiditis: What Is The Thyroid Gland?Documento3 pagineThyroiditis: What Is The Thyroid Gland?Angga M RahmanNessuna valutazione finora
- C9apstudy GuideDocumento37 pagineC9apstudy GuidejqtdNessuna valutazione finora
- MCQ DentalDocumento20 pagineMCQ DentalKovoor LedchumananNessuna valutazione finora
- Pranayama - The Ancient Science of Breath ControlDocumento34 paginePranayama - The Ancient Science of Breath ControlSkucan KsasaNessuna valutazione finora
- Surgical Anatomy of The LarynxDocumento39 pagineSurgical Anatomy of The LarynxSabyasachi PatiNessuna valutazione finora
- LE Muscles OINADocumento5 pagineLE Muscles OINAUshuaia Chely FilomenoNessuna valutazione finora
- PHR 121 Anatomy & Physiology: Diploma in PharmacyDocumento51 paginePHR 121 Anatomy & Physiology: Diploma in PharmacyAzmi ArifinNessuna valutazione finora