Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Aust Triage Scale
Caricato da
mutiaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Aust Triage Scale
Caricato da
mutiaCopyright:
Formati disponibili
POLICY ON
THE AUSTRALASIAN TRIAGE SCALE
1.
INTRODUCTION
The Australasian Triage Scale (ATS) is designed for use in hospital-based emergency services
throughout Australia and New Zealand. It is a scale for rating clinical urgency. Although
primarily a clinical tool for ensuring that patients are seen in a timely manner, commensurate
with their clinical urgency, the ATS is also a useful casemix measure. The scale directly relates
triage code with a range of outcome measures (inpatient length of stay, ICU admission,
mortality rate) and resource consumption (staff time, cost). It provides an opportunity for
analysis of a number of performance parameters in the Emergency Department (casemix,
operational efficiency, utilisation review, outcome effectiveness and cost).
2.
PRACTICALITY AND REPRODUCIBILITY
As the ATS is a primarily clinical tool, the practicalities of patient flow must be balanced with
attempts to maximise inter-rater reproducibility. It is recognised that no casemix measure
reaches perfect reproducibility. Reproducibility within and between emergency departments can
be maximised by application of the Guidelines for Implementation and widespread use of the
training package.
Triage accuracy and system evaluation can be assessed by comparison against guidelines.
Patterns of triage category distribution, ICU admission and mortality by triage category should
be comparable between peer hospitals of similar role delineation. Admission rate by triage
category is also a useful comparison between peer hospitals for the higher urgency categories.
These benchmarks for Emergency Departments of different role delineation should be reviewed
from time to time as disposition practices change.
Standards of consistency should also be regularly checked with studies of inter-rater reliability.
An acceptable standard of inter-rater agreement is represented by a weighted Kappa Statistic of
at least 0.6.
3.
APPLICATION
3.1 Procedure
All patients presenting to an Emergency Department should be triaged on arrival by a
specifically trained and experienced registered nurse. The triage assessment and ATS code
allocated must be recorded. The triage nurse should ensure continuous reassessment of patients
who remain waiting, and, if the clinical features change, re-triage the patient accordingly. The
triage nurse may also initiate appropriate investigations or initial management according to
organisational guidelines.
The triage nurse applies an ATS category in response to the question: This patient should wait
for medical assessment and treatment no longer than.
34 Jeffcott Street y West Melbourne y Victoria 3003 y Australia y Telephone: (03) 9320 0444 y Fax: (03) 9320 0400
P06 Policy on The Australasian Triage Scale
Page 2
____________________________________________________________________________________________________
3.2 Environmental and Equipment Requirements
The triage area must be immediately accessible and clearly sign-posted. Its size and design must
allow for patient examination, privacy and visual access to the entrance and waiting areas, as
well as for staff security.
The area should be equipped with emergency equipment, facilities for standard precautions
(hand-washing facilities, gloves), security measures (duress alarms or ready access to security
assistance), adequate communications devices (telephone and/or intercom etc) and facilities for
recording triage information.
4.
5.
DESCRIPTION OF SCALE
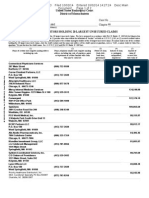
ATS CATEGORY
TREATMENT ACUITY
(Maximum waiting time)
PERFORMANCE
INDICATOR
THRESHOLD
ATS 1
Immediate
100%
ATS 2
10 minutes
80%
ATS 3
30 minutes
75%
ATS 4
60 minutes
70%
ATS 5
120 minutes
70%
PERFORMANCE INDICATOR THRESHOLDS
The indicator threshold represents the percentage of patients assigned Triage Code 1 through to
5 who commence medical assessment and treatment within the relevant waiting time from their
time of arrival. Staff and other resources should be deployed so that thresholds are achieved
progressively from ATS Categories 1 through to 5. The performance indicator thresholds shown
are appropriate for the period 1998 2002 inclusive1, and should be achievable in all
Emergency Departments. Performance indicator thresholds must be kept under regular review.
Where Emergency Department resources are chronically restricted, or during periods of
transient patient overload, staff should be deployed so that performance is maintained in the
more urgent categories.
It is neither clinically nor ethically acceptable to routinely expect any patient or group of
patients to wait longer than two (2) hours for medical attention. Prolonged waiting times for
undifferentiated patients presenting for emergency care is viewed as a failure of both access and
quality.
6.
QUALITY ASSURANCE
Triage accuracy and system evaluation may be undertaken in part by reviewing the triage
allocation against guidelines, triage category footprint of example diagnoses, average waiting
time, admission rates and mortality rates in each triage category with peer hospitals. As practices
such as disposition change over time, these benchmarks should be periodically reviewed.
P06 Policy on The Australasian Triage Scale
Page 3
____________________________________________________________________________________________________
7.
REFERENCE
Commonwealth Department of Health and Family Services, Coopers and Lybrand Consultants.
Development of Agreed Set of National Access Performance Indicators for: Elective Surgery,
Emergency Departments and Outpatient Services. Canberra, July 1997, p106.
P06
Reviewed March 2006 (no changes made)
Revised November 2000
Adopted by Council November 1993
This document is Copyright and cannot be reproduced in whole or in part without prior permission
Potrebbero piacerti anche
- The Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayDa EverandThe Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayNessuna valutazione finora
- Introduction to Clinical Effectiveness and Audit in HealthcareDa EverandIntroduction to Clinical Effectiveness and Audit in HealthcareNessuna valutazione finora
- Australian Model Triage ScaleDocumento3 pagineAustralian Model Triage ScaleHendraDarmawanNessuna valutazione finora
- Triage ATS PDFDocumento7 pagineTriage ATS PDFkalembrowNessuna valutazione finora
- G24 Guidelines On Implementation of ATSDocumento10 pagineG24 Guidelines On Implementation of ATSsestia dia alifahNessuna valutazione finora
- Australasian Triage Scale Ats PDFDocumento4 pagineAustralasian Triage Scale Ats PDFIwan SetiawanNessuna valutazione finora
- AustralianTriageScales Guidelines PDFDocumento10 pagineAustralianTriageScales Guidelines PDFMaryantiNessuna valutazione finora
- Critical Care Environment: BOX 2.1 Business Case: Sample HeadingsDocumento8 pagineCritical Care Environment: BOX 2.1 Business Case: Sample HeadingsIqbal Yusuf AshariNessuna valutazione finora
- Initial Assessment of Emergency Department PatientsDocumento11 pagineInitial Assessment of Emergency Department PatientsDen Sinyo0% (1)
- Triage in The HospitalDocumento15 pagineTriage in The HospitalCarie Manarondong100% (1)
- Research 1Documento3 pagineResearch 1Doaa AwadNessuna valutazione finora
- Canadian Triage Acuity Scale (CTAS)Documento32 pagineCanadian Triage Acuity Scale (CTAS)Ciecilia Stefanny Sistandria Mahesta100% (3)
- Patient Identification ProcedureDocumento3 paginePatient Identification ProcedureEva JaworskiNessuna valutazione finora
- New Rich Text DocumentDocumento3 pagineNew Rich Text DocumentDoaa AwadNessuna valutazione finora
- Canadian Triage PDFDocumento3 pagineCanadian Triage PDFJany UllauriNessuna valutazione finora
- Safe HandoversDocumento7 pagineSafe HandoversRobMarvinNessuna valutazione finora
- Guidelines For Nurses Performing TriageDocumento4 pagineGuidelines For Nurses Performing TriagedroenNessuna valutazione finora
- Committee Opinion: Preparing For Clinical Emergencies in Obstetrics and GynecologyDocumento3 pagineCommittee Opinion: Preparing For Clinical Emergencies in Obstetrics and GynecologyMochammad Rizal AttamimiNessuna valutazione finora
- Case2 Individual Submission Vibhuty Tulika 991725526Documento13 pagineCase2 Individual Submission Vibhuty Tulika 991725526Tulika Anand GuptaNessuna valutazione finora
- Patients' Waiting Time: Indices For Measuring Hospital EffectivenessDocumento18 paginePatients' Waiting Time: Indices For Measuring Hospital Effectivenessmr kevinNessuna valutazione finora
- Case2 Individual Submission Vibhuty Tulika 991725526Documento13 pagineCase2 Individual Submission Vibhuty Tulika 991725526Tulika Anand GuptaNessuna valutazione finora
- Sact Passport Final Aug 2020Documento68 pagineSact Passport Final Aug 2020ryze.ahmedNessuna valutazione finora
- StaffingDocumento11 pagineStaffingAnezka Valine Santos Tanguio100% (3)
- 259-MED824447RLHNS - Job Description and Person Specification - Generic Non Specialist ACCU Clin Fellow JD 2016Documento8 pagine259-MED824447RLHNS - Job Description and Person Specification - Generic Non Specialist ACCU Clin Fellow JD 2016Daniyal AzmatNessuna valutazione finora
- Dr. Kshanti Adhitya, SpEm - Perencanaan Sistem Triage IGD (KSA)Documento35 pagineDr. Kshanti Adhitya, SpEm - Perencanaan Sistem Triage IGD (KSA)bio rizkimaulanaNessuna valutazione finora
- WEEK 3. Quality and Safe Management in The ERDocumento19 pagineWEEK 3. Quality and Safe Management in The ERAira Espleguira100% (1)
- Practice Standards For Obstetric and Gynaecological UnitDocumento27 paginePractice Standards For Obstetric and Gynaecological UnitRDi J100% (1)
- Safety PaperDocumento4 pagineSafety Paperapi-336793554Nessuna valutazione finora
- 2011 - Application of Queuing Theory in Health CareDocumento11 pagine2011 - Application of Queuing Theory in Health CareAneri JainNessuna valutazione finora
- Quality Improvement Opportunity - HealthDocumento8 pagineQuality Improvement Opportunity - HealthSam kNessuna valutazione finora
- IC 1 Minimum Standards For Intensive Care UnitsDocumento15 pagineIC 1 Minimum Standards For Intensive Care UnitsRositaadlNessuna valutazione finora
- Waiting Line ModelsDocumento15 pagineWaiting Line ModelsHussam MubashirNessuna valutazione finora
- Waiting Time ManagementDocumento11 pagineWaiting Time ManagementRiaz AhmedNessuna valutazione finora
- BI&DV Cia1Documento13 pagineBI&DV Cia1ATHIRA DENNY 2127958Nessuna valutazione finora
- ICU Nurse PrivilegesDocumento35 pagineICU Nurse PrivilegesSarah Alberto100% (4)
- DR Raya Ezat Lec 4Documento16 pagineDR Raya Ezat Lec 4Djdjjd SiisusNessuna valutazione finora
- Guidelines For ICU Admission, Discharge, and Triage (Crit Care Med 1999)Documento11 pagineGuidelines For ICU Admission, Discharge, and Triage (Crit Care Med 1999)Kary VelazquezNessuna valutazione finora
- Final ACC 2021Documento67 pagineFinal ACC 2021Karien UysNessuna valutazione finora
- Hand Off CommunicationDocumento6 pagineHand Off CommunicationALELAW100% (1)
- Good Practice 12 Patient HandoverDocumento4 pagineGood Practice 12 Patient HandoverDewi Ratna SariNessuna valutazione finora
- Surgical Self-Assessment ChecklistDocumento8 pagineSurgical Self-Assessment ChecklistJyoti KumarNessuna valutazione finora
- Leadership Analysis PaperDocumento8 pagineLeadership Analysis Paperapi-238680155Nessuna valutazione finora
- IMRT - ACR - ASTRO GuidelinesDocumento11 pagineIMRT - ACR - ASTRO GuidelinesSayan DasNessuna valutazione finora
- TJEM - Factors Affecting The Accuracy of Nurse Triage in Tertiary Care E.RDocumento5 pagineTJEM - Factors Affecting The Accuracy of Nurse Triage in Tertiary Care E.RIntanPermataSyariNessuna valutazione finora
- Clinical Practice in AmbulanceDocumento4 pagineClinical Practice in Ambulancengurah_wardanaNessuna valutazione finora
- Standardised Handover Protocol 2014 PDFDocumento7 pagineStandardised Handover Protocol 2014 PDFNikkae AngobNessuna valutazione finora
- Acr Practice Parameter For The Performance of Fluoroscopic Contrast Enema Examination in AdultsDocumento8 pagineAcr Practice Parameter For The Performance of Fluoroscopic Contrast Enema Examination in AdultsHercules RianiNessuna valutazione finora
- Draft 3Documento3 pagineDraft 3michealNessuna valutazione finora
- Hospital-Based Triage of Obstetric Patients ACOGDocumento4 pagineHospital-Based Triage of Obstetric Patients ACOGponekNessuna valutazione finora
- Allocation of Extra Surgical Staff in Surgical Assessment Unit SAU An Effective Strategy For ImprovementDocumento8 pagineAllocation of Extra Surgical Staff in Surgical Assessment Unit SAU An Effective Strategy For ImprovementAthenaeum Scientific PublishersNessuna valutazione finora
- Optimization of An Appointment Scheduling ProblemDocumento20 pagineOptimization of An Appointment Scheduling ProblemKumar palNessuna valutazione finora
- s41598 021 98851 7Documento19 pagines41598 021 98851 7Kumar palNessuna valutazione finora
- Us ObDocumento16 pagineUs ObWahyu RianiNessuna valutazione finora
- Examples of Triage ConditionsDocumento9 pagineExamples of Triage ConditionsDevi Christina Damanik (Papua medical School)Nessuna valutazione finora
- Acr Practice Parameter For Breast UltrasoundDocumento7 pagineAcr Practice Parameter For Breast UltrasoundBereanNessuna valutazione finora
- Acute Care Toolkit 1 - HandoverDocumento4 pagineAcute Care Toolkit 1 - Handoveranurag katiyarNessuna valutazione finora
- Patient Tracer Methodology - RadiologyDocumento5 paginePatient Tracer Methodology - RadiologyRicardo Espinoza LipaNessuna valutazione finora
- Roils ReportDocumento5 pagineRoils Reportapi-632526087Nessuna valutazione finora
- TÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANODa EverandTÉCNICAS DEL AUXILIAR DE ENFERMERÍA EN EL ÁREA DE QUIRÓFANONessuna valutazione finora
- Textbook of Urgent Care Management: Chapter 16, Urgent Care Duties, Staffing Mix and RatiosDa EverandTextbook of Urgent Care Management: Chapter 16, Urgent Care Duties, Staffing Mix and RatiosNessuna valutazione finora
- Analisis Dan Perancangan Sistem Informas PDFDocumento19 pagineAnalisis Dan Perancangan Sistem Informas PDFmutiaNessuna valutazione finora
- 2012-1-00995-IF Ringkasan001Documento10 pagine2012-1-00995-IF Ringkasan001mutiaNessuna valutazione finora
- Publikasi 08.11.1965Documento18 paginePublikasi 08.11.1965tblues41Nessuna valutazione finora
- Medical Reconciliation Form: Name: Source of InformationDocumento1 paginaMedical Reconciliation Form: Name: Source of InformationmutiaNessuna valutazione finora
- A Triage Scale PDFDocumento13 pagineA Triage Scale PDFQueeiin NeeshaNessuna valutazione finora
- Pedoman Clinical PrivilegeDocumento13 paginePedoman Clinical PrivilegemutiaNessuna valutazione finora
- Applicant Declaration Form - 1 Jul 2013Documento3 pagineApplicant Declaration Form - 1 Jul 2013Vo Minh KhoiNessuna valutazione finora
- MR XXX Original CVDocumento6 pagineMR XXX Original CVEpan SaputraNessuna valutazione finora
- People Vs Yam-IdDocumento9 paginePeople Vs Yam-Idautumn moonNessuna valutazione finora
- Richard Stitely v. Carolyn Colvin, 4th Cir. (2015)Documento6 pagineRichard Stitely v. Carolyn Colvin, 4th Cir. (2015)Scribd Government DocsNessuna valutazione finora
- Filing Complaint To Consumer CourtDocumento1 paginaFiling Complaint To Consumer CourtksheetalkumarNessuna valutazione finora
- Deployment Program/ Project Application FormDocumento1 paginaDeployment Program/ Project Application FormCrystal Ann Monsale TadiamonNessuna valutazione finora
- List of Important Days - National & International: JanuaryDocumento3 pagineList of Important Days - National & International: JanuarybalaNessuna valutazione finora
- RA 11058 IRR MelDocumento48 pagineRA 11058 IRR MelNick Latumbo100% (1)
- LNP: Still Keeping Secrets, Feb. 4, 2016Documento44 pagineLNP: Still Keeping Secrets, Feb. 4, 2016LNP MEDIA GROUP, Inc.Nessuna valutazione finora
- Adelson-Weinberg Article On CIRMDocumento6 pagineAdelson-Weinberg Article On CIRMCalifornia Stem Cell ReportNessuna valutazione finora
- National Social Protection Strategy GhanaDocumento95 pagineNational Social Protection Strategy GhanaSisiraPinnawalaNessuna valutazione finora
- Unit V Pharmacy and ControlDocumento10 pagineUnit V Pharmacy and ControlJenesis Cairo CuaresmaNessuna valutazione finora
- Health Care Domain (US)Documento28 pagineHealth Care Domain (US)nimeshbrNessuna valutazione finora
- Hampden County Physican Associates CreditorsDocumento2 pagineHampden County Physican Associates CreditorsJim KinneyNessuna valutazione finora
- Combined Chapters 1 and 2Documento36 pagineCombined Chapters 1 and 2Alysia Gearty100% (1)
- TURNBUCKLEDocumento2 pagineTURNBUCKLEAnonymous cljdRqO8Nessuna valutazione finora
- Duflo - The Economist As PlumberDocumento39 pagineDuflo - The Economist As PlumberhsdNessuna valutazione finora
- Organizational Goals and Environment: Goal-Setting As An Interaction ProcessDocumento10 pagineOrganizational Goals and Environment: Goal-Setting As An Interaction Processtempduc177Nessuna valutazione finora
- Role of Insurance Companies in The Economic Development of BangladeshDocumento4 pagineRole of Insurance Companies in The Economic Development of BangladeshAsim Mandal60% (5)
- Mental HealthCare Acts Rules Compendium India As On 20181112Documento86 pagineMental HealthCare Acts Rules Compendium India As On 20181112Disability Rights AllianceNessuna valutazione finora
- 40 HR Training Guide For Fire Safety Inspector and Practitioner PDFDocumento659 pagine40 HR Training Guide For Fire Safety Inspector and Practitioner PDFAramis89% (9)
- The Settings, Processes, Methods, and Tools in Social WorkDocumento5 pagineThe Settings, Processes, Methods, and Tools in Social WorkJaymar Kasan KamidNessuna valutazione finora
- Flowable Wound Matrix Outpatient Reimbursement Summary 2019Documento4 pagineFlowable Wound Matrix Outpatient Reimbursement Summary 2019Bob RiouxNessuna valutazione finora
- IMC ACT 1956 OriginalDocumento20 pagineIMC ACT 1956 OriginalMahesh KumarNessuna valutazione finora
- Regatta 2012 Team 1 - CompaniesDocumento1 paginaRegatta 2012 Team 1 - Companiesapi-160838686Nessuna valutazione finora
- Batas Reptlblika: (Republic Act)Documento9 pagineBatas Reptlblika: (Republic Act)Que BeneviceNessuna valutazione finora
- Anti-Noise and Public Nuisance OrdDocumento3 pagineAnti-Noise and Public Nuisance OrdRenz CarloNessuna valutazione finora
- D43 PDFDocumento2 pagineD43 PDFArnold RojasNessuna valutazione finora
- Cadet Activities Consent FormDocumento1 paginaCadet Activities Consent Formrobby_dicksonNessuna valutazione finora
- Annual Report Full 2015 16 PDFDocumento340 pagineAnnual Report Full 2015 16 PDFAkhil SoniNessuna valutazione finora