Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Middle East Respiratory Syndrome
Caricato da
Anonymous IsKLcXFv1WCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Middle East Respiratory Syndrome
Caricato da
Anonymous IsKLcXFv1WCopyright:
Formati disponibili
Collin Sanderson
Middle East Respiratory Syndrome
Overview
Middle East Respiratory Syndrome (MERS) is a recently discovered virus from the
Betacoronaviral genus. It is an enveloped virus with a nucelocapsid-encased genome of singlestranded, positive RNA. The non-segmented genome is slightly above the average size of a viral
genome, with 32,000 base pairs. The virus was first discovered in connection with the
phylogenetically similar virus Severe Acute Respiratory Syndrome (SARS), and the first cases
emerged in 2012 in Saudi Arabia (Chan, Lau and Woo). It is believed that MERS originated
from bat populations, where it developed in coordination with bat evolution. MERS makes use
of the DPP4 (also known as CD-26) protein as a cell-entry receptor. The DPP4 gene evolutionary
footprint shows that the gene evolved as a result of natural selection in favor of bats that were
less susceptible to MERS. However, the receptor-binding domain of the MERS virus evolved in
harmony with bat DPP4, permitting continued infection among the bat populations (Cui, Eden
and Holmes). Thus, when the MERS virus came into contact with human individuals, it was
already highly developed for mammalian DPP4.
The connection between MERS and bats is clear, but the reservoir more closely
associated with human infection is camels. Contact with camels in the Middle East is frequent,
and camels milk and meat are lightly consumed as well. A recent study shows that a coronavirus
isolated from dromedary camels is 99.9% genomically identical to human MERS, significantly
more similar than to the MERS strain found in bats (Raj, Farag and Reusken). Evidently, MERS
Middle East Respiratory Syndrome
continued to evolve beyond its infection of bats and happened to grow an affinity for humans. Its
strong human affinity contributes to its great ability to establish an infection in a host patient.
MERS is an extremely deadly disease, and has been shown to be somewhat transmissible
between humans. As of June 2015, 483 deaths have occurred out of 1180 confirmed cases of
MERS (40% mortality) (Zumla, Hui and Perlman).
Pathogenesis/Disease Mechanism
The clinical signs of MERS infection include acute severe community-acquired
pneumonia in almost all cases, acute renal failure, cough, difficulty breathing, and gastrointestinal symptoms, including diarrhea. Complete respiratory failure also occurred in a majority
of cases, requiring ventilator support (Chan, Lau and Woo). Tropism of MERS is linked to
several cell-surface proteins, including previously mentioned DPP4 (CD-26). Many of these
proteins are common to respiratory epithelia as well as renal and enteric epithelial cells.
Additionally, DPP4 is involved in the regulation of several key cellular and systemic processes,
namely chemokine regulation, T-cell activation, and apoptosis (Matteucci and Giampietro).
More about DPP4 is discussed later on.
Many of the common symptoms of MERS can be traced to the cellular effect of infection.
More about the cytopathology of MERS is discussed later, but the most notable effect is that cell
detachment from the tissue eventually occurs. Detachment causes damage, or more specifically,
thinning of infected tissues (van den Brand, Smits and Haagmans). No literature directly
addresses the mechanisms whereby MERS causes its disease, so I will present inferences based
on the research observations of the cellular effect of MERS infection and the related
pathophysiology.
Middle East Respiratory Syndrome
The majority of the cells in MERS cellular tropism spectrum are epithelial cells. The
several respiratory symptoms (pneumonia, cough, difficulty breathing, and complete respiratory
failure) are all results of thinning of bronchial and alveolar epithelia. Alveolar epithelia are
responsible for respiratory gas exchange, as well as the production of pulmonary surfactants that
keep alveoli from collapsing during expiration (Ward and Nicholas). Bronchial epithelia have
cilia that move mucus, fluids, and foreign particles up the bronchi and out of the lungs (Jacquot,
Spilmont and de Bentzmann). Damage to these two tissues leads to fluid and particulate matter in
the lungs (pneumonia), poor pulmonary gas exchange, mucosal build-up which can cause
blockage of bronchi leading to coughing and difficulty breathing, and collapse of alveoli all
resulting in complete respiratory failure (Ketai and Godwin).
Renal epithelia are involved in the transport of blood filtrates into and out of the nephron
tubules for concentrating urine. Damage to this tissue can lead to decreased production of urine,
also known as kidney failure (Clark, Kirby and Baker). Enteric epithelia make up intestinal villi,
which are responsible for fluid and nutrient absorption. Damage to this tissue interferes with the
absorption of water, leading to diarrhea (Berkes, Viswanatha and Savkovic).
Avoiding the Immune System & Hypothesis
A goal of current research is to explain the mechanisms that MERS uses to avoid the
immune system. MERS has been found to inhibit antigen-presentation in infected cells, inhibit
cell death, and cause cells to eventually detach from tissue. I also present the hypothesis that
MERS inhibits/avoids an interferon response, and that this is key to the propagation of the
infection. I will provide evidences of my hypothesis, some of which are highly connected to
other immune avoidance mechanisms.
Middle East Respiratory Syndrome
Many viruses cause death of the cells they infect. Macrophages clean up dead cell
remains, and release inflammatory cytokines to bring additional blood flow to the area,
catalyzing an immune system response. Macrophages also release interferon during cleanup.
However, MERS causes cell detachment from tissues instead of cell death, preventing
macrophage involvement. In one article, the research team involved studied the effects of MERS
infection on cells over time. They infected an immortalized Vero cell line derived from kidney
epithelial cells (expressing the necessary DPP4 protein) with MERS and found that they
displayed only mild cytopathic effects up to six days after infection. Thereafter the infected cells
began to detach from the culture container surface, without cell death occurring. This matches
the common MERS incubation period of 5-7 days. This observation contrasted with the infection
progression of various non-MERS coronaviruses, all of which induced severe cytopathic effects
quickly after infection and observable cell death (de Wilde, Raj and Oudshoorn). Detachment of
cells instead of cell death agrees with the recorded observation that inflammation is very limited
in MERS infection (Lau, Lau and Chan). This illustrates the MERS infection strategy to avoid
an interferon and inflammatory response to cell death, supporting my hypothesis.
A few possible explanations of MERS inhibition of cell death exist. One explanation is in
its replication mechanism. The nucleocapsid-encased genome acquires its envelope by budding
from the organelle-membranes surrounding the cellular endoplasmic reticulum and Golgi
apparatus as an intracellular vesicle. The virions then exocytose from the cell, leaving the
cellular membrane intact (Stadler, Masignani and Eickmann). This mechanism prevents cell
death early in the infection process, preventing an immediate interferon response until the
infection is more pervasive. Additionally, the DPP4 gene is linked with regulation of apoptosis
in the cells where it is expressed, as mentioned previously. MERS strong connection to DPP4
Middle East Respiratory Syndrome
may give MERS some control over other ways that infected cells can induce apoptosis in
response to the virus, but this has not been researched thus far.
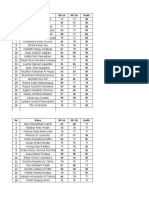
In a previously discussed article, the team studied the effects of interferon induction on
MERS infection, and compared it to the phylogenetically similar SARS virus. The data recorded
shows that SARS virus was unaffected by interferon until higher concentrations were present.
MERS, however, showed dramatic decrease in its cytopathic effects by even the smallest
concentrations of interferon that were tested (data below). This data provides evidence to my
hypothesis that inhibition of interferon is key to MERS infection progression (de Wilde, Raj and
Oudshoorn).
One of the strongest triggers of an interferon response is double-stranded RNA.
According to a recent review of MERS research, the positive sense MERS genome is replicated
in its full length into a negative sense copy (J. F. Chan, S. K. Lau and K. K. To). The coexistence of positive and negative sense RNA causes a strong presence of dsRNA in the infected
cell, which would be guaranteed to trigger interferon production. Therefore, MERS must have
Middle East Respiratory Syndrome
some interferon-inhibition mechanism to compensate for the volume of dsRNA it creates. A
recently discovered protein in the MERS transcriptome displays this ability. In the study, MERS
protein 4a bound to dsRNA created during viral replication (Siu, Yeung and Kok). We can then
infer that protein 4a would compete with PACT for binding in an infected cell. PACT is a
cellular protein that stimulates interferon production when bound to dsRNA (Patel and Sen).
This discovery hints at a highly specialized mechanism whereby MERS avoids an interferon
response. I believe that these several evidences provide strong support for my hypothesis that
MERS avoids and inhibits interferon in order to successfully propagate.
As a final immune-avoidance method, MERS substantially down-regulates the expression
of nine genes that are vital to the cells antigen-presentation---the means of activating the
adaptive immune system in response to an infection. Among these are genes from the
proteasome (PSMB8/9) and peptide-loading complex (PDIA3 and TAPBP), which are necessary
for the MHC class I pathway, and CD74 in the MHC class II pathway (data below) (Josset,
Menachery and Gralinski). The exact method whereby MERS causes this down-regulation is
unknown, but it is likely through proteins in MERS transcriptome, or a side effect of viral
replication.
Middle East Respiratory Syndrome
All of these mechanisms contribute to the high mortality of Middle East Respiratory
Syndrome. As such a newly emerging disease, there are no specialized medical treatments or
vaccines against it. Research is limited but ongoing in the search for a counterattack to this
deadly virus.
Scholarly Sources
Berkes, J., et al. "Intestinal epithelial responses to enteric pathogens: effects on the tights junction barrier, ion
transport, and inflammation." Gut 52.3 (2003): 439-451.
Chan, Jasper F.W., et al. "Middle East Respiratory Syndrome Coronavirus: Another Zoonotic Betacoronavirus
Causing SARS-Like Disease." Clinical Microbiology Reviews 28.2 (2015): 465-522.
Chan, Jasper Fuk-Woo, Susanna Kar-Pui Lau and Patrick Chiu-Yat Woo. "The emerging novel Middle East
respiratory syndrome coronavirus: The "knowns" and "unknowns"." Journal of the Formosan Medical
Association 112 (2013): 372-381.
Clark, K.R., et al. "Renal epithelium: reversal of cytotoxic damage by addition of anti-ththymocyte globulin."
Transplant International 4.4 (1991): 210-214.
Cui, Jie, et al. "Adaptive evolution of bat dipeptidyl peptidase 4 (dpp4): implications for the origin and emergence
of Middle East respiratory syndrome coronavirus." Virology Journal 304 (2013).
de Wilde, Adriaan H., et al. "MERS-coronavirus replication induces severe in vitro cytopathology and is strongly
inhibited by cyclosporin A or interferon-alpha treatment." Journal of General Virology 94 (2013): 17491760.
Jacquot, J., et al. "Structure and secretory functions of the respiratory epithelium." Archives internationales de
physiologie, de biochimie et de biophysique 100.4 (1992): A41-46.
Josset, Laurence, et al. "Cell Host Response to Infection with Novel Human Coronavirus EMC Predicts Potential
Antivirals and Important Differences with SARS Coronavirus." mBio 4.3 (2013).
Ketai, L.H. and J.D. Godwin. "A new view of pulmonary edema and acute respiratory distress syndrome." Journal of
Thoracic Imaging 13.3 (1998): 147-171.
Lau, S.K., et al. "Delayed induction of proinflammatory cytokines and suppression of innate antiviral response by
the novel Middle East respiratory syndrome coronavirus: implication for pathogenesis and treatment."
Journal of General Virology 94 (2013): 2679-2690.
Matteucci, E. and O. Giampietro. "Dipeptidyl Peptidase-4 (CD26): Knowing the Function before Inhibiting the
Enzyme." Current Medicinal Chemistry 16.23 (2009): 2943-2951.
Patel, Rekha C. and Ganes C. Sen. "PACT, a protein activator of the interferon-induced protein kinase, PKR." The
EMBO Journal 17 (1998): 4379-4390.
Raj, VS, EABA Farag and CBEM Reusken. "Isolation of MERS Coronavirus from a Dromedary Camel." Emerging
Infectious Diseases (2014): 1339-1342.
Middle East Respiratory Syndrome
Siu, Kam-Leung, et al. "Middle East Respiratory Syndrome Coronavirus 4a Protein Is a Double-Stranded DNABinding Protein That Suppresses PACT-Induced Activation of RIG-I and MDA5 in the Innate Antiviral
Response." Journal of Virology 88.9 (2014): 4866-4876.
Stadler, K, et al. "SARS--beginning to understand a new virus." Nature Reviews Microbiology 1 (2003): 209-218.
van den Brand, Judith M.A., Saskia L. Smits and Bart L. Haagmans. "Pathogenesis of Middle East respiratory
syndrome coronavirus." Journal of Pathology 235 (2015): 175-184.
Ward, HE and TE Nicholas. "Alveolar type I and type II cells." Australian & New Zealand Journal of Medicine 5.3
(1984): 731-734.
Zumla, Alimuddin, David S. Hui and Stanley Perlman. "Middle East respiratory syndrome." The Lancet 386.9997
(2015): 995-1007.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- BIOCHEM REPORT - OdtDocumento16 pagineBIOCHEM REPORT - OdtLingeshwarry JewarethnamNessuna valutazione finora
- Psc720-Comparative Politics 005 Political CultureDocumento19 paginePsc720-Comparative Politics 005 Political CultureGeorge ForcoșNessuna valutazione finora
- Global Marketing & R&D CH 15Documento16 pagineGlobal Marketing & R&D CH 15Quazi Aritra ReyanNessuna valutazione finora
- Personal Philosophy of Education-Exemplar 1Documento2 paginePersonal Philosophy of Education-Exemplar 1api-247024656Nessuna valutazione finora
- Guide To U.S. Colleges For DummiesDocumento12 pagineGuide To U.S. Colleges For DummiesArhaan SiddiqueeNessuna valutazione finora
- Hydrogen Peroxide DripDocumento13 pagineHydrogen Peroxide DripAya100% (1)
- Faith-Based Organisational Development (OD) With Churches in MalawiDocumento10 pagineFaith-Based Organisational Development (OD) With Churches in MalawiTransbugoyNessuna valutazione finora
- Communication and Globalization Lesson 2Documento13 pagineCommunication and Globalization Lesson 2Zetrick Orate0% (1)
- Eet 223 (1) Analog Electronics JagjeetDocumento79 pagineEet 223 (1) Analog Electronics JagjeetMahima ArrawatiaNessuna valutazione finora
- D5 PROF. ED in Mastery Learning The DefinitionDocumento12 pagineD5 PROF. ED in Mastery Learning The DefinitionMarrah TenorioNessuna valutazione finora
- Graphic Organizers As A Reading Strategy: Research FindDocumento9 pagineGraphic Organizers As A Reading Strategy: Research Findzwn zwnNessuna valutazione finora
- Traps - 2008 12 30Documento15 pagineTraps - 2008 12 30smoothkat5Nessuna valutazione finora
- Cognitive ApprenticeshipDocumento5 pagineCognitive ApprenticeshipRandall RobertsNessuna valutazione finora
- DBA Daily StatusDocumento9 pagineDBA Daily StatuspankajNessuna valutazione finora
- Life&WorksofrizalDocumento5 pagineLife&WorksofrizalPatriciaNessuna valutazione finora
- Acfrogb0i3jalza4d2cm33ab0kjvfqevdmmcia - Kifkmf7zqew8tpk3ef Iav8r9j0ys0ekwrl4a8k7yqd0pqdr9qk1cpmjq Xx5x6kxzc8uq9it Zno Fwdrmyo98jelpvjb-9ahfdekf3cqptDocumento1 paginaAcfrogb0i3jalza4d2cm33ab0kjvfqevdmmcia - Kifkmf7zqew8tpk3ef Iav8r9j0ys0ekwrl4a8k7yqd0pqdr9qk1cpmjq Xx5x6kxzc8uq9it Zno Fwdrmyo98jelpvjb-9ahfdekf3cqptbbNessuna valutazione finora
- Speech by His Excellency The Governor of Vihiga County (Rev) Moses Akaranga During The Closing Ceremony of The Induction Course For The Sub-County and Ward Administrators.Documento3 pagineSpeech by His Excellency The Governor of Vihiga County (Rev) Moses Akaranga During The Closing Ceremony of The Induction Course For The Sub-County and Ward Administrators.Moses AkarangaNessuna valutazione finora
- Accountancy Department: Preliminary Examination in MANACO 1Documento3 pagineAccountancy Department: Preliminary Examination in MANACO 1Gracelle Mae Oraller0% (1)
- Leisure TimeDocumento242 pagineLeisure TimeArdelean AndradaNessuna valutazione finora
- The Idea of Multiple IntelligencesDocumento2 pagineThe Idea of Multiple IntelligencesSiti AisyahNessuna valutazione finora
- Motivational Speech About Our Dreams and AmbitionsDocumento2 pagineMotivational Speech About Our Dreams and AmbitionsÇhärlöttë Çhrístíñë Dë ÇöldëNessuna valutazione finora
- Multiple Linear RegressionDocumento26 pagineMultiple Linear RegressionMarlene G Padigos100% (2)
- Ielts Reading Whale CultureDocumento4 pagineIelts Reading Whale CultureTreesa VarugheseNessuna valutazione finora
- Rosenberg Et Al - Through Interpreters' Eyes, Comparing Roles of Professional and Family InterpretersDocumento7 pagineRosenberg Et Al - Through Interpreters' Eyes, Comparing Roles of Professional and Family InterpretersMaria AguilarNessuna valutazione finora
- CN and OS Lab ManualDocumento53 pagineCN and OS Lab Manualsudheer mangalampalliNessuna valutazione finora
- WHAT - IS - SOCIOLOGY (1) (Repaired)Documento23 pagineWHAT - IS - SOCIOLOGY (1) (Repaired)Sarthika Singhal Sarthika SinghalNessuna valutazione finora
- Anclas Placas Base para Columnas Thomas MurrayDocumento89 pagineAnclas Placas Base para Columnas Thomas MurrayMariano DiazNessuna valutazione finora
- AdvacDocumento13 pagineAdvacAmie Jane MirandaNessuna valutazione finora
- 2,3,5 Aqidah Dan QHDocumento5 pagine2,3,5 Aqidah Dan QHBang PaingNessuna valutazione finora
- Chapter 019Documento28 pagineChapter 019Esteban Tabares GonzalezNessuna valutazione finora