Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
276 Infantile Hypertrophic Pyloric Stenosis
Caricato da
Susi Muharni RismaCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
276 Infantile Hypertrophic Pyloric Stenosis
Caricato da
Susi Muharni RismaCopyright:
Formati disponibili
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.
com
INFANTILE HYPERTROPHIC PYLORIC STENOSIS
ANAESTHESIA TUTORIAL OF THE WEEK 276
26TH NOVEMBER 2012
Dr Ian Davies
University Hospitals Bristol
Correspondence to ian.davies2@nhs.net
QUESTIONS
Before reading this tutorial, please answer the following question (true or false). The answers and an
explanation are at the end of the tutorial.
1.
The following fluids have a role in infantile hypertrophic pyloric stenosis (true or false)
a. 0.9% saline
b. Hartmanns solution
c. Isotonic bicarbonate
d. 0.45% saline with 5% glucose
2.
Which one of the following statements is false?
a. The usual biochemical picture is that of hypochloraemic metabolic alkalosis
b. Potassium chloride may be added to intravenous fluid once urine output is
established
c. Upper GI imaging and barium studies are the gold-standard for diagnosis
d. Up to 80% of infants continue to regurgitate following corrective surgery
3.
Regarding pyloromyotomy, which of the following statements is true or false?
a. Pyloromyotomy is always an emergency procedure
b. Pyloromyotomy is associated with severe postoperative pain
c. Babies should be nil by mouth for a minimum of 12 hours following surgery
d. Pyloromyotomy is curative and is associated with low mortality
INTRODUCTION
Pyloric stenosis, or infantile hypertrophic pyloric stenosis (IHPS), is a condition characterised by
hypertrophy of the two muscle layers of the pylorus. The pyloric canal lengthens, the whole pylorus
thickens, and the mucosa becomes oedematous causing functional obstruction of the gastric outlet.
EPIDEMIOLOGY
Incidence varies between regions, but ranges from 2-4 per 1000 live births. The condition is more
commonly seen in males (4:1). Presentation is usually early in life, between 3 and 5 weeks of age, and
approximately 95% of cases are identified in those aged 3-12 weeks.
Mortality is low. An eight-year cohort study of 350 patients admitted to hospital in the Republic of
Ireland with IHPS identified only one death, which was attributed to an underlying myopathy.
ATOTW 276 Infantile Hypertrophic Pyloric Stenosis, 26th November 2012
Page 1 of 5
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
AETIOLOGY
Whilst the exact causative mechanisms of IHPS are unknown, there are several established
associations.
A Danish study identified a nearly 200-fold increase in incidence of IHPS among monozygotic twins,
suggesting familial factors are significant. Several genetic loci have been implicated, including IHPS1,
where a deficient production of neuronal nitric oxide synthase causes impaired relaxation of pyloric
smooth muscle.
It has been suggested that a high gastric parietal cell mass may result in impaired gastrin control and
hence, duodenal hyperacidity. This hyperacidity may produce IHPS as a result of repeated contraction
of the pylorus.
The use of macrolide antibiotics such as erythromycin in the first two weeks of life appears to convey a
risk of IHPS, and an association has also been shown between macrolide antibiotic use by pregnant or
breast-feeding mothers and the development of IHPS in their offspring.
PRESENTATION
The classical presentation is that of a 3-5 week old infant with non-bilious projectile vomiting
immediately after feeding, and where the infant is hungry soon after vomiting. An olive-like mass can
be felt at the lateral edge of the rectus abdominis muscle in the right upper quadrant of the abdomen.
The best time to feel this is immediately after a test feed, after the child has vomited.
The child may present with clinical signs of dehydration if the diagnosis if delayed and vomiting
prolonged for a number of weeks. Signs of dehydration include a sunken fontanelle, dry mucous
membranes, poor skin turgor and lethargy. Signs of malnutrition and poor weight gain may also be
apparent.
Laboratory Investigations
The classical picture is hypochloraemic metabolic alkalosis due to loss of hydrochloric acid in vomited
gastric fluid. This may be associated with hypokalaemia as the kidneys compensate for the underlying
alkalosis by preferentially excreting potassium in order to retain hydrogen ions. This is usually seen as
a result of persistent vomiting (often more than three weeks). Persistent vomiting and dehydration may
also result in either hyper- or hyponatraemia. Pre-renal failure can occur.
DIAGNOSIS
Diagnosis is usually made on the basis of a typical history and palpation of the olive-like mass. In the
early stages, IHPS can be difficult to distinguish from gastro-oesophageal reflux disease or even sepsis.
In such situations, diagnosis may be confirmed radiologically.
Ultrasound
This is the diagnostic test of choice, although the accuracy is operator-dependent. The size of the
pylorus is measured and compared to standard values. Pyloric muscle thickness >4mm, pyloric muscle
length >14 20mm and pyloric diameter >10-14mm is diagnostic in term infants, with both a high
sensitivity (90-99%) and high specificity (97-100%). Ultrasound is less accurate in premature infants.
ATOTW 276 Infantile Hypertrophic Pyloric Stenosis, 26th November 2012
Page 2 of 5
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
Upper GI Imaging
Barium studies show classical signs of an elongated pyloric canal (string sign) or thickened pyloric
mucosa (double-track sign). Due to concerns about radiation exposure, upper GI imaging is only used
when ultrasound is inconclusive.
MANAGEMENT
Resuscitation
Initial management should follow an ABC approach, and fluid management should focus on
correction of underlying dehydration, as well as electrolyte and acid-base abnormalities. An initial
bolus of 20ml/kg 0.9% saline should be used if the infant is dehydrated. Thereafter, maintenance fluid
should be started, the purpose of which is to maintain adequate hydration whilst protecting against
hypernatraemia and hypoglycaemia. An appropriate maintenance fluid is 5% glucose/0.45% saline,
provided the plasma sodium is not low; 5% glucose/0.9% saline should be used in this situation.
Potassium chloride should be added to the fluid as required once urine output has been established. An
accurate fluid balance chart should be kept and urinary catheterisation should be considered if the child
is dehydrated. Serial electrolyte, acid-base and blood glucose measurements must be performed. A
nasogastric tube should be passed to decompress the stomach.
Conservative Management
IHPS can be managed conservatively by naso-duodenal feeding. This has to be continued over several
months to allow the obstructive process resolve and the infant to gain weight. Treatment with atropine
has also been described. The safety and effectiveness of surgery means that conservative management
is reserved for those in whom surgery is contra-indicated.
Surgery
This is not an emergency procedure, and surgery may proceed only when fluid balance, acid-base
status and electrolyte levels have been restored to normal. The baby is at risk of postoperative apnoeas
if the metabolic alkalosis is not corrected prior to surgery. The classical operation is a Ramstedt
pyloromyotomy; a longitudinal incision of the pylorus with blunt dissection to the level of the submucosa, thus relieving the gastric outlet obstruction. This operation is considered curative with
minimal associated mortality.
Pyloromyotomy may also be performed laparoscopically. Prospective randomised controlled trials
comparing open and laparoscopic techniques have suggested that laparoscopic surgery results in
reduced post-operative emesis, reduced analgesia requirements, a more rapid return to enteral feeding
and shorter hospital stay.
Endoscopic balloon dilatation has been used, but is not as successful as surgical pyloromyotomy. This
technique is reserved for those in whom surgery poses a significant risk.
ANAESTHESIA
The nasogastric tube should be aspirated before induction of anaesthesia to minimise the risk of
pulmonary aspiration of gastric contents. A 4 quadrant aspiration (turning the infant through a full
rotation and aspirating the stomach at each quarter turn) has been suggested as being effective.
Anaesthesia may be induced by inhalation with sevoflurane (or halothane), or rapid sequence induction
with either thiopentone or propofol. This depends on personal preference and whether the stomach can
be safely considered empty following suctioning, or if the child should still be considered at a high risk
of aspirating on induction. Good intubating conditions are obtained with 1-2mg/kg of suxamethonium,
ATOTW 276 Infantile Hypertrophic Pyloric Stenosis, 26th November 2012
Page 3 of 5
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
and prolonged paralysis using non-depolarising neuromuscular blocking drugs. Classic RSI with
application of cricoid pressure is not possible in infants as the child will desaturate rapidly whilst
apnoeic; a modified RSI with gentle positive pressure ventilation is commonly used.
Anaesthesia should be maintained with volatile agents with or without nitrous oxide (avoid nitrous in
laparoscopic surgery). Full intra-operative monitoring as per AAGBI guidelines is strongly advised.
Patient temperature should be monitored and the child should be maintained in a warm environment to
avoid cooling. Antibiotic prophylaxis (e.g. co-amoxiclav 30 mg/kg IV or cefuroxime 50mg/kg IV)
should be given prior to skin incision to reduce postoperative wound infection.
Boluses of an isotonic fluid (saline 0.9% or hartmanns solution) 10ml/kg may be given intraoperatively to correct circulating volume if required. Glucose containing maintenance solutions may be
continued in theatre, but must NOT be used for bolus fluid replacement. If glucose containing
maintenance fluids are discontinued intra-operatively, the blood glucose should be checked regularly to
ensure normoglycaemia throughout the perioperative period.
It used to be common practice to inject air via the nasogastric tube at the end of the procedure to ensure
pyloric patency, but this is no longer recommended.
Postoperative pain is not usually severe, and good analgesia may be achieved intra-operatively with an
intravenous opioid such as fentanyl 1 mcg/kg and paracetamol (7.5 mg/kg IV or 30-40mg/kg PR). The
wound should be infiltrated with bupivacaine 0.25% 2 mg/kg (0.8 ml/kg) where possible.
At the end of surgery, extubation should be performed in the left lateral position once neuromuscular
blockade is fully reversed, and the infant is awake.
POSTOPERATIVE CONSIDERATIONS
Analgesia should be provided with paracetamol as required and non-steroidal anti-inflammatory drugs
(NSAIDs) such as ibuprofen 5mg/kg if pain is worse than anticipated. The nasogastric tube may be
removed at the conclusion of the procedure, and maintenance intravenous fluids should continue until
feeding is re-established. Modern strategies focus on early implementation of feeding from four hours
after surgery. Up to 80% patients continue to regurgitate after surgery, but this almost always
improves in the ensuing days.
The infant can be considered fit for discharge when well hydrated and tolerating feeds. Prognosis
following surgery is good and complete recovery and catch-up growth is the norm.
SUMMARY
Infantile hypertrophic pyloric stenosis is a common condition, occurring in
2 4 per 1000 live births
Presentation is usually early, between 3 5 weeks of age
Initial management is aimed at resuscitation, correcting of dehydration,
alkalosis and electrolyte disturbances before corrective surgery can occur
A variety of anaesthetic techniques have been used successfully, although
rapid sequence intravenous induction, endotracheal intubation and
maintenance with an inhalational agent is common and safe.
ATOTW 276 Infantile Hypertrophic Pyloric Stenosis, 26th November 2012
Page 4 of 5
Sign up to receive ATOTW weekly - email worldanaesthesia@mac.com
ANSWERS TO QUESTIONS
1.
a.
b.
c.
d.
T the resuscitation fluid of choice
T may be used if monitoring blood glucose regularly
F may worsen alkalosis
T maintenance fluid of choice, provided the child is not hyponatraemic
a.
b.
c.
d.
T
T
F on the occasions the disorder cannot be diagnosed clinically, ultrasound is
the choice
T
a.
b.
c.
d.
F should be delayed until fluid balance and acid-base status are corrected
F although adequate analgesia should still be ensured
F early feeding, from 4 hours post-op, has been shown to be of benefit
T
2.
3.
REFERENCES AND FURTHER READING
Medscape Reference. Drugs, Diseases & Procedures. Paediatric Pyloric Stenosis [Online]. 2012 [cited
19th August 2012]. Available from: http://emedicine.medscape.com/article/803489-overview (accessed
25th November 2012).
MacDonald NJ, Fitzpatrick GJ, Moore KP, Wren WS and Keenan M. Anaesthesia for congenital
hypertrophic pyloric stenosis. A review of 350 patients. Br. J. Anaesth. 1987;59:672-677.
Panteli C. New insights into the pathogenesis of infantile pyloric stenosis. Pediatr Surg Int.
2009:25(12);1043-1052.
Perger L, Fuchs JR, Komidar L, Mooney DP. Impact of surgical approach on outcome in 622
consecutive pyloromyotomies at a paediatric teaching institution. J Pediatr Surg. 2009;44:2119-25.
Miozzari HH, Tnz M, von Vigier RO, Bianchetti MG. Fluid resuscitation in infantile hypertrophic
pyloric stenosis. Acta Paediatr. 2001;90(5):511-4.
ATOTW 276 Infantile Hypertrophic Pyloric Stenosis, 26th November 2012
Page 5 of 5
Potrebbero piacerti anche
- 5 Acute Heart Failure Drcindyboom PDFDocumento20 pagine5 Acute Heart Failure Drcindyboom PDFSusi Muharni RismaNessuna valutazione finora
- Genogram Template 11Documento1 paginaGenogram Template 11Susi Muharni RismaNessuna valutazione finora
- Genogram Template 04Documento4 pagineGenogram Template 04Susi Muharni RismaNessuna valutazione finora
- My Family Tree: Great-Grandfather: Great-Grandmother: Great-Grandfather: Great-GrandmotherDocumento1 paginaMy Family Tree: Great-Grandfather: Great-Grandmother: Great-Grandfather: Great-GrandmotherSusi Muharni RismaNessuna valutazione finora
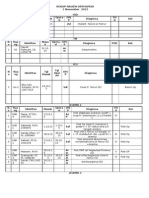
- Rekap Pasien Orthopaedi 1 November 2015Documento4 pagineRekap Pasien Orthopaedi 1 November 2015Susi Muharni RismaNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Chapter 3 - the-WPS OfficeDocumento15 pagineChapter 3 - the-WPS Officekyoshiro RyotaNessuna valutazione finora
- CH Folk Media and HeatlhDocumento6 pagineCH Folk Media and HeatlhRaghavendr KoreNessuna valutazione finora
- Binary SearchDocumento13 pagineBinary SearchASasSNessuna valutazione finora
- 67-Article Text-118-1-10-20181206Documento12 pagine67-Article Text-118-1-10-20181206MadelNessuna valutazione finora
- Discussion #3: The Concept of Culture Learning ObjectivesDocumento4 pagineDiscussion #3: The Concept of Culture Learning ObjectivesJohn Lery SurellNessuna valutazione finora
- The Handmaid's Tale - Chapter 2.2Documento1 paginaThe Handmaid's Tale - Chapter 2.2amber_straussNessuna valutazione finora
- 2022 Drik Panchang Hindu FestivalsDocumento11 pagine2022 Drik Panchang Hindu FestivalsBikash KumarNessuna valutazione finora
- August Strindberg's ''A Dream Play'', inDocumento11 pagineAugust Strindberg's ''A Dream Play'', inİlker NicholasNessuna valutazione finora
- Jurnal Politik Dan Cinta Tanah Air Dalam Perspektif IslamDocumento9 pagineJurnal Politik Dan Cinta Tanah Air Dalam Perspektif Islamalpiantoutina12Nessuna valutazione finora
- TypeFinderReport ENFPDocumento10 pagineTypeFinderReport ENFPBassant AdelNessuna valutazione finora
- Department of Education: Republic of The PhilippinesDocumento2 pagineDepartment of Education: Republic of The PhilippinesShailac RodelasNessuna valutazione finora
- Sucesos de Las Islas Filipinas PPT Content - Carlos 1Documento2 pagineSucesos de Las Islas Filipinas PPT Content - Carlos 1A Mi YaNessuna valutazione finora
- Psc720-Comparative Politics 005 Political CultureDocumento19 paginePsc720-Comparative Politics 005 Political CultureGeorge ForcoșNessuna valutazione finora
- Zimbabwe Mag Court Rules Commentary Si 11 of 2019Documento6 pagineZimbabwe Mag Court Rules Commentary Si 11 of 2019Vusi BhebheNessuna valutazione finora
- The Personal Law of The Mahommedans, According To All The Schools (1880) Ali, Syed Ameer, 1849-1928Documento454 pagineThe Personal Law of The Mahommedans, According To All The Schools (1880) Ali, Syed Ameer, 1849-1928David BaileyNessuna valutazione finora
- MSDS PetrolDocumento13 pagineMSDS PetrolazlanNessuna valutazione finora
- German Monograph For CannabisDocumento7 pagineGerman Monograph For CannabisAngel Cvetanov100% (1)
- Education Law OutlineDocumento53 pagineEducation Law Outlinemischa29100% (1)
- Calcined Clays For Sustainable Concrete Karen Scrivener, AurÇlie Favier, 2015Documento552 pagineCalcined Clays For Sustainable Concrete Karen Scrivener, AurÇlie Favier, 2015Débora BretasNessuna valutazione finora
- University of Dar Es Salaam MT 261 Tutorial 1Documento4 pagineUniversity of Dar Es Salaam MT 261 Tutorial 1Gilbert FuriaNessuna valutazione finora
- Marcelo H Del PilarDocumento8 pagineMarcelo H Del PilarLee Antonino AtienzaNessuna valutazione finora
- Form No. 10-I: Certificate of Prescribed Authority For The Purposes of Section 80DDBDocumento1 paginaForm No. 10-I: Certificate of Prescribed Authority For The Purposes of Section 80DDBIam KarthikeyanNessuna valutazione finora
- Promising Anti Convulsant Effect of A Herbal Drug in Wistar Albino RatsDocumento6 paginePromising Anti Convulsant Effect of A Herbal Drug in Wistar Albino RatsIJAR JOURNALNessuna valutazione finora
- CopacabanaDocumento2 pagineCopacabanaNereus Sanaani CAñeda Jr.Nessuna valutazione finora
- Payment Billing System DocumentDocumento65 paginePayment Billing System Documentshankar_718571% (7)
- Memoire On Edgar Allan PoeDocumento16 pagineMemoire On Edgar Allan PoeFarhaa AbdiNessuna valutazione finora
- Kodak Case StudyDocumento8 pagineKodak Case StudyRavi MishraNessuna valutazione finora
- DELA CRUZ - LAC 1 - 002 - Individual Learning Monitoring Plan - Bugtongnapulo INHSDocumento2 pagineDELA CRUZ - LAC 1 - 002 - Individual Learning Monitoring Plan - Bugtongnapulo INHSGilbert Dela CruzNessuna valutazione finora
- 4 Major Advantages of Japanese Education SystemDocumento3 pagine4 Major Advantages of Japanese Education SystemIsa HafizaNessuna valutazione finora
- LittorinidaeDocumento358 pagineLittorinidaeSyarif Prasetyo AdyutaNessuna valutazione finora