Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Reading 2 and 3
Caricato da
RosSimbulanCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Reading 2 and 3
Caricato da
RosSimbulanCopyright:
Formati disponibili
Reading 2
1. What were the most common sources of non-prescription antibiotics?
Non-prescription use of antimicrobials occurs worldwide
Most of the non-prescription use of antibiotics are outside North
America and Northern Europe
The most common source of non-prescription antibiotics is the
Pharmacy. Other sources includes, friends, family and home.
2. What safety concerns were associated with nonprescription use of
antimicrobials?
An additional safety concern was substandard quality of antimicrobials available without
prescription.
Expired drugs or those that, as a result of degradation, have decreased bioavailability
might both predispose a patient to treatment failure and promote antimicrobial resistance.
Outright counterfeit antimicrobials are available in developing countries and can lead to
treatment failure or direct harm
Non-prescription use of substandard antimicrobials is probably more common, although
low-quality antimicrobials have also been identified through official prescription sources.
3. Were the adverse effects of nonprescription antimicrobials regularly
reported? What health governance problem does it imply?
Definite adverse effects of non-prescription antimicrobials were rarely reported, probably
due in part to the decentralized health-care systems in most areas with non-prescription
sale of antimicrobials.
Adverse effects of non-prescription antimicrobials are rarely reported, but they are likely
at least as common as adverse effects of prescription antimicrobials.
Of adverse events requiring emergency room attendance, 79% were allergic reactions.
4. What practices of nonprescription use of antimicrobials were probably
related to emerging resistance? Cite specific examples.
Bartoloni and colleagues studied non-pathogenic E coli isolates from children under age
5 years in Bolivia. Overall, 40% of children harboured nonpathogenic E. coli resistant to
ampicillin, co-trimoxazole, tetracycline, and chloramphenicol (which were the
antimicrobials most commonly used in the communities studied). In this population,
antimicrobials were available without a prescription and were frequently used.
At a population level, clinically important bacterial resistance including penicillinresistant and erythromycin- resistant S pneumoniae and ciprofloxacin-resistant nontyphi salmonella has been associated with increasing non-prescription use of these
antimicrobials in a Thai community.
Frequency of resistance has been examined in respiratory pathogens in Vietnamese
children and Senegalese adults with urinary tract infections. In all studies, high rates of
community resistance were reported and were associated with patients receiving
antimicrobials 6 months before each study, in communities with high non-prescription
antimicrobial use.
5. Under what circumstances were patients exposed to the risks of an antimicrobial without
benefit? Cite specific examples.
Pharmacists dispensing non-prescription antimicrobials without knowledge of patients
allergies.
Poor regulation of antimicrobials due to inefficient enforcement of policies.
lnadequate guidance regarding appropriate antimicrobial selection for individual
syndromes.
inadequate health education regarding safe practices to minimise adverse drug effects.
Financial concerns of the patient often guide antimicrobial selection resulting in short
duration of treatment.
Reading 3
1. What is meant by antibiotic stewardship?
It is an emerging field in medicine currently defined by a series of strategies and
interventions aimed toward improving appropriate prescription of antibiotics in humans
in all healthcare settings.
2. In what ways does antibiotic stewardship improve the quality of patient care and patient
safety?
Antibiotic stewardship contributes to the improvement of quality of patient care and
patient safety by minimizing toxicity and frequency of adverse drug events, reducing the
costs of healthcare for infections, and limiting the selection for drug - resistant strains.
3. As a future Bedan physician, how will you uphold and practice EVERY core element of
antibiotic stewardship? Identify these core elements then cite concrete examples.
Leadership Commitment: Dedicating necessary human, financial and information
technology resources.
Accountability: Appointing a single leader responsible for program outcomes. Experience
with successful programs show that a physician leader is effective.
Drug Expertise: Appointing a single pharmacist leader responsible for working to
improve antibiotic use.
Action: Implementing at least one recommended action, such as systemic evaluation of
ongoing treatment need after a set period of initial treatment (i.e. antibiotic time out
after 48 hours).
Tracking: Monitoring antibiotic prescribing and resistance patterns.
Reporting: Regular reporting information on antibiotic use and resistance to doctors,
nurses and relevant staff.
Education: Educating clinicians about resistance and optimal prescribing.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Daftar Obat - Obat Lasa (Look Alike Sound Alike)Documento2 pagineDaftar Obat - Obat Lasa (Look Alike Sound Alike)RonyChanya94% (18)
- Antimicrobial Stewardship Manual of Procedures For Hospitals 2016 v2Documento82 pagineAntimicrobial Stewardship Manual of Procedures For Hospitals 2016 v2kNessuna valutazione finora
- ABC TableDocumento2 pagineABC TableRosSimbulanNessuna valutazione finora
- Hepatitis Chart: The Texas Guide To School Health ProgramsDocumento2 pagineHepatitis Chart: The Texas Guide To School Health ProgramsRosSimbulanNessuna valutazione finora
- Price Elasticity of Supply and DemandDocumento4 paginePrice Elasticity of Supply and DemandRosSimbulanNessuna valutazione finora
- Hepatitis Chart: The Texas Guide To School Health ProgramsDocumento2 pagineHepatitis Chart: The Texas Guide To School Health ProgramsRosSimbulanNessuna valutazione finora
- Patients RightsDocumento31 paginePatients RightsRosSimbulanNessuna valutazione finora
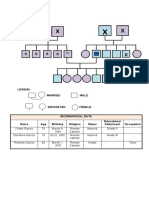
- GENOGRAMDocumento1 paginaGENOGRAMRosSimbulanNessuna valutazione finora
- GENOGRAMDocumento1 paginaGENOGRAMRosSimbulanNessuna valutazione finora
- Antibiotics-An Investigatory ProjectDocumento20 pagineAntibiotics-An Investigatory ProjectAdiJaijan100% (2)
- 10 5923 S Microbiology 201401 01Documento9 pagine10 5923 S Microbiology 201401 01Aksan IpeyNessuna valutazione finora
- The Risk For Endocarditis in Dental PracticeDocumento9 pagineThe Risk For Endocarditis in Dental PracticeisanreryNessuna valutazione finora
- Antibiotic PK PD (RASPRO Indonesia)Documento26 pagineAntibiotic PK PD (RASPRO Indonesia)Persi lampungNessuna valutazione finora
- Infection Control Policy5967286291Documento41 pagineInfection Control Policy5967286291Shyam PrasadNessuna valutazione finora
- Manual de Micologia IndustrialDocumento785 pagineManual de Micologia IndustrialJulio César Chacón HernándezNessuna valutazione finora
- Seiffert Et Al 2013Documento24 pagineSeiffert Et Al 2013Zubair Ibrahim100% (1)
- Plastic Surgery SummaryDocumento30 paginePlastic Surgery SummaryLailaAliNessuna valutazione finora
- Product Aiocd PDFDocumento10 pagineProduct Aiocd PDFJames PerianayagamNessuna valutazione finora
- Pharmacology Antibiotics: Fluoroquinolone - Chloramphenicol - TetracycllineDocumento40 paginePharmacology Antibiotics: Fluoroquinolone - Chloramphenicol - TetracycllinemluthfidunandNessuna valutazione finora
- Extended Spectrum BetalactamasesDocumento63 pagineExtended Spectrum Betalactamasestummalapalli venkateswara raoNessuna valutazione finora
- Antibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHDocumento5 pagineAntibiotic Susceptibility Patterns of Methicillin Resistant Staphyl - PDF NIHzia ul RahmanNessuna valutazione finora
- Germ Vs Cellular Theory PDFDocumento37 pagineGerm Vs Cellular Theory PDFpaulxe100% (3)
- Pakistan Kidney and Liver Institute & Research Centre (PKLI)Documento2 paginePakistan Kidney and Liver Institute & Research Centre (PKLI)Waqas SaleemNessuna valutazione finora
- AcaciaDocumento88 pagineAcaciaalmagloNessuna valutazione finora
- Food Poisoning - Outbreaks, Bacterial Sources and Adverse Health Effects (2015) PDFDocumento294 pagineFood Poisoning - Outbreaks, Bacterial Sources and Adverse Health Effects (2015) PDFAndré Campelo100% (1)
- 1 PBDocumento12 pagine1 PBAndy SetiawanNessuna valutazione finora
- The Antibacterial Activity of Borreria VerticillataDocumento5 pagineThe Antibacterial Activity of Borreria VerticillatathallyssoncostaNessuna valutazione finora
- Stok 03052019Documento141 pagineStok 03052019Renold EnoNessuna valutazione finora
- Quantum + Apl Jakarta 07-04-2021Documento1 paginaQuantum + Apl Jakarta 07-04-2021Apoteker depokNessuna valutazione finora
- And Antibacterial Resistance: Pseudomonas Aeruginosa: Burn Infection, TreatmentDocumento10 pagineAnd Antibacterial Resistance: Pseudomonas Aeruginosa: Burn Infection, TreatmentnurelisabayuNessuna valutazione finora
- ART Action and Resistance Mechanisms of Antibiotics A Guide For CliniciansDocumento16 pagineART Action and Resistance Mechanisms of Antibiotics A Guide For CliniciansHECTORIBZAN ACERO SANDOVALNessuna valutazione finora
- Jurnal AntibiotikDocumento5 pagineJurnal AntibiotikSela PutrianaNessuna valutazione finora
- CLSI M100 32e 2022 - Central Labs SummaryDocumento9 pagineCLSI M100 32e 2022 - Central Labs Summaryshimaa khaterNessuna valutazione finora
- Major Catalogue Complet PDFDocumento237 pagineMajor Catalogue Complet PDFHervis FantiniNessuna valutazione finora
- tmp7092 TMPDocumento8 paginetmp7092 TMPFrontiersNessuna valutazione finora
- Quiz Pharmacology Part 2 of 2Documento54 pagineQuiz Pharmacology Part 2 of 2MedShare92% (25)
- Antibióticos Intratecales en Pacientes Adultos: Intrathecal Administration of Antibiotics in Adult PatientsDocumento10 pagineAntibióticos Intratecales en Pacientes Adultos: Intrathecal Administration of Antibiotics in Adult PatientsNathaly Velasteguí PeraltaNessuna valutazione finora