Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Fluids Electrolytes
Caricato da
1234chocoCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Fluids Electrolytes
Caricato da
1234chocoCopyright:
Formati disponibili
Cut out this Section
FLUIDS & ELECTROLYTES
GUIDELINES - ADULT
PRESCRIBING INTRAVENOUS FLUIDS and ELECTROLYTES for ADULT patients (4th Edition)
Reviewed by Queensland Health Safe Medication Management Unit, Fluid and Electrolyte Guidelines Working Party,
September 2010, Next review: end of 2012
1. Assess current fluid status
Is the patient dry, wet or just right?
Review fluid balance charts, urine output and daily weight
Review clinical symptoms and signs of fluid deficit or overload
Fluid deficit
Estimate degree from history and signs including: thirst, dry mucous membranes, tachycardia, and low urine output. Postural or
supine hypotension plus flat neck veins with or without other evidence of shock indicate intravascular hypovolaemia.
First correct intravascular hypovolaemia: Institute rapid replacement with fluids such as 0.9% sodium chloride or Compound
Sodium Lactate, or appropriate colloids such as Albumin 4% or succinylated Gelatin. Blood and blood products may be indicated.
Seek assistance from a Senior Medical Officer. It may be necessary to contact ICU or Emergency Department.
Replace estimated extracellular deficit: Correct with an appropriate replacement fluid, based on type of fluid lost and current
tonicity (plasma sodium concentration). Compound Sodium Lactate may be appropriate. If serum sodium is low, avoid 5% glucose
or glucose saline combinations. Administer half required volume over 8 hours and the second half over 16 hours. If poor cardiac
reserve reduce rate to half over 12 hours and second half over 24 hours. Frequently reassess during this process.
Fluid Overload
Signs include: increased daily weight, raised JVP, peripheral oedema (consider hypoalbuminaemia) and pulmonary oedema.
Management: Minimise sodium and fluid given. Consider diuretic.
2. Assess ongoing fluid losses
Estimate ongoing volume losses including vomiting, diarrhoea, nasogastric drainage and other losses (e.g. with ileus). These should
be added to the volume given daily. The type of fluid to use depends on the source of loss.
3. Assess maintenance requirements
Requirements in unstressed, well individuals differ from sick hospital patients. A well, unstressed 70 kg adult, who is NBM,
euvolaemic, not septic or post-surgical, with normal cardiac and renal function and no additional fluid losses would have needs met by
0.3% sodium chloride and 3.3% glucose containing 40 mmol/L of potassium at 80 mL/hr (1L 12hrly).
Typical daily healthy ADULT needs
Sodium
Potassium
Fluid
Weight based (lean body weight)
2 mmol/kg
1 mmol/kg
30-35mL/kg
For Average Adult
140 mmol
70 mmol
2L
Remember to consider all sources of fluid administration, including TPN, NG feeds, and drug infusions.
Post-operative or sick patients or those with co-morbidities, including neurosurgical patients, require a modifed regime.
4. Modify in the following situations
If you are not experienced with management of any of these patients, please seek advice
Conditions where ADH levels are elevated
Patients (especially young women) with nausea, emesis, pain and stress tend to retain water and develop hypotonicity. The postoperative period is high risk. Fluids with a higher sodium concentration administered in reduced volumes are indicated (for example
day 1 post-op: 0.9% sodium chloride with 20 mmol/L potassium at 40-50 mL/hr may be appropriate in a euvolaemic patient).
Smaller patients (weight less than 50kg)
Proportional reductions are indicated.
Reduced left ventricular function
Patients are at increased risk of fluid overload. Reduce volume given and monitor fluid status more frequently.
Reduced renal function
Patients may be at increased risk of fluid overload and hyperkalaemia.
If oliguric, do not use maintenance potassium. If hypovolaemic, correct any fluid deficit as above. If euvolaemic, limit the volume
given to approximately: urine vol + other losses + 500mL per day.
Medications that increase potassium (e.g. ACE inhibitors and Angiotensin II antagonists, spironolactone and eplerenone)
Patients are at increased risk of hyperkalaemia. Monitor potassium levels frequently.
Septic patients
Have variably increased fluid requirements. Vasopressor support in ICU may be required.
Obese
Estimate fluid requirements and electrolyte doses based on lean body weight (see medication dose calculators
http://medicationdosingcalculators.health.qld.gov.au). Adjustment of weight for morbid obesity is complex.
Malnourished patients and extended duration of therapy
Often experience complex and resistant electrolyte disturbances.
Specific fluid requirements
Patients on dialysis, with burns, transplants, acute neurological conditions (such as meningitis, encephalitis and stroke), diabetic
ketoacidosis or hyperosmolar hyperglycaemic state have very specific fluid requirements. Seek advice.
Some properties of common fluids (adapted from table 1 in the GIFTSUP guidelines)
Type of Fluid
Sodium mmol/L
Potassium mmol/L
Chloride mmol/L
Sodium chloride 0.9% *
154
0
154
Compound Sodium Lactate
129
5
109
0.3% sodium chloride & 3.3% glucose *
51
0
51
5% glucose
0
0
0
Glucose g/L
0
0
33
50
v4.00 - 04/2011
* Available as pre-mix with 20mmol or 40mmol/L of potassium.
5. When to review
Unstable patients need to be reviewed at least every 2-4 hours. All patients should be reassessed at least daily.
Consider slowing the rate of fluid infusion overnight in patients at risk of overload.
Switch to an enteral route (oral, NG, PEG etc) as soon as possible to minimise iatrogenic complications.
Please direct any feedback / comments on these guidelines to Safe Medication Management Unit (07) 31316525
See Prescribing Guidelines for Electrolytes over page
FLUIDS & ELECTROLYTES
GUIDELINES - ADULT
Cut out this Section
Electrolyte disturbances that are difficult to correct often indicate significant pathology please seek advice.
Unit specific protocols for electrolyte disturbances take precedence over these guidelines.
HYPOKALAEMIA (mild 3.1 - 3.5mmol/L, moderate 2.5 - 3.0mmol/L, severe less than 2.5mmol/L)
The total body deficit of potassium correlates poorly with plasma potassium because most potassium is intracellular.
Low plasma potassium is a serious problem: Plasma levels less than 3.5mmol/L may result in dysrhythmias.
Moderate and severe hypokalaemia should be treated with IV and (where possible) oral supplementation. These patients usually
require at least an extra 60-80mmol potassium above maintenance requirements in next 24 hours (i.e. 100 -140mmol in total);
repeat plasma levels 4-6 hours after commencing treatment.
All potassium containing infusions must be given via an infusion pump or burette.
Maximum CONCENTRATION = 40mmol/L in sodium chloride 0.9% peripherally to prevent phlebitis.
EXCEPTION: isotonic, premixed potassium chloride 10mmol/100mL minibags (commercially premade, ready to use) can
be given peripherally. Note: Minibags MUST be given via an infusion pump.
If maximum concentrations are exceeded administration through a large vein with high blood flow (e.g. CVC, venous access
port, PICC) is required.
Maximum RATE:
With burette = 10mmol/hr.
With infusion pump = 20mmol/hr.
If maximum rate (above) exceeded, cardiac monitoring and administration through a large vein is recommended.
Mild hypokalaemia may be treated with oral supplementation alone, provided the oral route is available. For example:
Potassium Chloride effervescent Tablets (e.g. Chlorvescent) - 12 tablets twice daily (14mmol potassium per tablet).
OR
Potassium Chloride slow release tablets 600mg (e.g. Span K or Slow K or Duro K) - 2 tablets twice daily (8mmol potassium
per tablet).
OR
Potassium chloride 10% oral solution - (20mmol potassium per 15mL).
If resistant to treatment, check magnesium and replace if necessary; check for medications which may decrease plasma
potassium, e.g. salbutamol, and ensure that potassium containing maintenance fluid is administered as necessary.
HYPOMAGNESAEMIA (less than 0.7mmol/L, severe less than 0.4mmol/L)
Severe or symptomatic hypomagnesaemia (tremors, weakness, cardiac arrhythmias, convulsions) should be corrected with
intravenous magnesium sulphate.
Magnesium sulphate 5mL ampoules contain 2.47g magnesium sulphate equivalent to 10mmol magnesium. 10-20mmol
magnesium, as magnesium sulphate, can be administered in 100mL 0.9% sodium chloride over 1-2 hours. NB: in emergency
situations, magnesium can be given more rapidly.
Mild or asymptomatic hypomagnesaemia can be treated with oral magnesium supplements, Magmin.
MagMin tablets contain 500mg magnesium aspartate equivalent to 1.54mmol magnesium. Begin with 1-2 magnesium
aspartate (MagMin) tablets twice daily and increase dose if tolerated; diarrhoea is a common side effect.
HYPONATRAEMIA (less than 135mmol/L, severe less than 120mmol/L)
Management of hyponatraemia requires careful assessment of fluid status and biochemical indices including plasma glucose and
osmolality, and urinary sodium and osmolality.
If hypovolaemic, correction of the intravascular deficit with 0.9% sodium chloride is appropriate.
If euvolaemic or hypervolaemic, consider drugs (e.g. SSRIs, diuretics, antiepileptics) or conditions associated with inappropriate
ADH secretion, or conditions with reduced effective circulating volume (e.g. cirrhosis, cardiac failure). Manage with fluid restriction.
Symptomatic hyponatraemia (e.g. drowsiness, headache, fitting) is an emergency and should be managed in an intensive care
setting. Hypertonic saline and airway access may be indicated.
Seek senior advice, especially in severe (less than 120 mmol/L) or symptomatic hyponatraemia.
In general, increase plasma sodium by no more than 10mmol/L/day, to prevent permanent neurological injury from osmotic
demyelination. 0.9% sodium chloride (not hypertonic saline) is the normal mainstay of IV therapy.
HYPOPHOSPHATAEMIA (less than 0.7mmol/L, severe less than 0.4mmol/L)
Phosphate does not normally need replacement until less than 0.6mmol/L except if: alcoholism, alcohol withdrawal, malnutrition, refeeding syndrome, receiving TPN, renal phosphate wasting, recovery from diabetic ketoacidosis or respiratory failure.
Consider IV replacement if plasma phosphate less than 0.4mmol/L.
Sodium phosphate and potassium phosphate (Low-K Phos) contains 13.4mmol of phosphate in a 20mL ampoule. If phosphate
is less than 0.3mmol/L then 2 ampoules of Low-K Phos are often needed in the first 24 hours. This can be added to 100250mL
0.9% sodium chloride and given over 6-8 hours.
Oral effervescent phosphate is available, Phosphate Sandoz, and contains 16.1mmol phosphate per 500mg tablet. May need to
divide daily dose throughout the day. Diarrhoea is a common side effect.
HYPOCALCAEMIA (less than 2.15mmol/L, severe less than 2mmol/L CORRECTED or less than 0.9mmol/L IONISED)
REMEMBER: Plasma calcium (even corrected for albumin) is an unreliable measure of functional (ionised) calcium.
Hypocalcaemia often reflects severe body fluid and electrolyte disturbances.
If the patient is symptomatic (e.g. seizures, tetany, positive Chvosteks / Trousseaus) or at high risk of developing symptomatic
hypocalcaemia (e.g. post-parathyroidectomy), use IV replacement.
Calcium gluconate 10% is the preferred form of IV replacement and contains 2.25mmol of calcium in 10mL. It can be added to
100mL of 0.9% sodium chloride and infused over 30 minutes, preferably into a large vein.
Calcium chloride 10% contains 6.8mmol calcium in 10mL. It is very irritating and should be given via a central line.
DO NOT co-infuse or mix calcium with phosphate containing preparations.
For oral replacement, use effervescent calcium tablets (Sandocal) or calcium carbonate tablets (Caltrate). Give away from food.
Active Ingredient per tablet:
Sandocal - 1g elemental calcium providing approx 25mmol calcium.
Caltrate - 600mg elemental calcium providing approx 15mmol calcium.
If resistant to treatment, exclude hypomagnesaemia.
Electrolyte solutions are incompatible with blood products, other medications and often each other.
Seek advice before mixing together in an infusion or giving simultaneously via the same IV line.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Code Geass - StoriesDocumento5 pagineCode Geass - Stories1234chocoNessuna valutazione finora
- Blue Veins Sub Theme TVBDocumento4 pagineBlue Veins Sub Theme TVB1234chocoNessuna valutazione finora
- Doctor Talk: Communication Practice Role PlaysDocumento6 pagineDoctor Talk: Communication Practice Role Plays1234chocoNessuna valutazione finora
- Osteo Infographic FinalDocumento1 paginaOsteo Infographic Final1234chocoNessuna valutazione finora
- QLD Rail Traim PDFDocumento1 paginaQLD Rail Traim PDF1234chocoNessuna valutazione finora
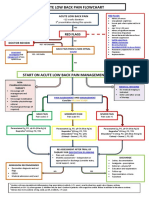
- Acute Low Back Pain Flowchart January 2017Documento1 paginaAcute Low Back Pain Flowchart January 20171234chocoNessuna valutazione finora
- Mbs Quick Guide: JULY 2020Documento2 pagineMbs Quick Guide: JULY 20201234chocoNessuna valutazione finora
- Pokemon Theme Song 22Documento4 paginePokemon Theme Song 221234chocoNessuna valutazione finora
- Fairy Tail - Main ThemeDocumento3 pagineFairy Tail - Main Theme1234chocoNessuna valutazione finora
- Blue BirdDocumento7 pagineBlue Bird1234chocoNessuna valutazione finora
- Topical Steroids (Sep 19) PDFDocumento7 pagineTopical Steroids (Sep 19) PDF1234chocoNessuna valutazione finora
- Topical Steroids (Sep 19) PDFDocumento7 pagineTopical Steroids (Sep 19) PDF1234chocoNessuna valutazione finora
- VTE GuidelinesDocumento11 pagineVTE Guidelines1234chocoNessuna valutazione finora
- Getting the Hospital Job: A Step-by-Step Guide to Applying for Your First PositionDocumento41 pagineGetting the Hospital Job: A Step-by-Step Guide to Applying for Your First Position1234chocoNessuna valutazione finora
- Metro South Intern Training Form (Logan)Documento3 pagineMetro South Intern Training Form (Logan)1234chocoNessuna valutazione finora
- USMLE Flashcards: Anatomy - Side by SideDocumento190 pagineUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- 2016 Applicant Guide Web V2Documento83 pagine2016 Applicant Guide Web V21234chocoNessuna valutazione finora
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDocumento7 pagine# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoNessuna valutazione finora
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDocumento1 paginaFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoNessuna valutazione finora
- PBM Module1 MTP Template 0Documento2 paginePBM Module1 MTP Template 01234chocoNessuna valutazione finora
- Herd Immunity'' A Rough Guide PDFDocumento6 pagineHerd Immunity'' A Rough Guide PDF1234chocoNessuna valutazione finora
- Taking a Social and Cultural History: A Biopsychosocial ApproachDocumento3 pagineTaking a Social and Cultural History: A Biopsychosocial Approach1234chocoNessuna valutazione finora
- ImprovingMedAdherenceOlderAdultslyer Final 508CDocumento2 pagineImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilNessuna valutazione finora
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDocumento5 pagineManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoNessuna valutazione finora
- The Effects of Social Networks On Disability in Older AustraliansDocumento22 pagineThe Effects of Social Networks On Disability in Older Australians1234chocoNessuna valutazione finora
- A Conceptual Framework For HealthDocumento1 paginaA Conceptual Framework For Health1234chocoNessuna valutazione finora
- Language of PreventionDocumento9 pagineLanguage of Prevention1234chocoNessuna valutazione finora
- Defining and Assessing Risks To Health PDFDocumento20 pagineDefining and Assessing Risks To Health PDF1234chocoNessuna valutazione finora
- Clinical Contributions To Addressing The Social Determinants of HealthDocumento5 pagineClinical Contributions To Addressing The Social Determinants of Health1234chocoNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- DLL - Mapeh 6 - Q4 - W6Documento4 pagineDLL - Mapeh 6 - Q4 - W6Bernard Martin100% (1)
- DOH Administrative Order No 2020 0043Documento11 pagineDOH Administrative Order No 2020 0043Marie AsyethNessuna valutazione finora
- Pharmacy Daily For Wed 25 Sep 2013 - Children/'s Panadol Is Back, Happy World Pharmacist Day, SHPA Pharmacy Honours, HealthDocumento3 paginePharmacy Daily For Wed 25 Sep 2013 - Children/'s Panadol Is Back, Happy World Pharmacist Day, SHPA Pharmacy Honours, HealthpharmacydailyNessuna valutazione finora
- Forecasting Pharma Ind Book BrochureDocumento2 pagineForecasting Pharma Ind Book BrochureAbhishek DixitNessuna valutazione finora
- Ethics in Pharmacy PracticeDocumento21 pagineEthics in Pharmacy PracticeLighto Ryusaki100% (1)
- Acetaminophen (Paracetamol)Documento2 pagineAcetaminophen (Paracetamol)Joshua KellyNessuna valutazione finora
- Zanthoxylum Fruit Extracts Boost Immune Activity in RatsDocumento1 paginaZanthoxylum Fruit Extracts Boost Immune Activity in RatsM Fzn LbsNessuna valutazione finora
- AIIMS June 2020 DR Siraj Ahmad PDFDocumento4 pagineAIIMS June 2020 DR Siraj Ahmad PDFadiNessuna valutazione finora
- Laporan Pemakaian Dan Lembar Permintaan Obat (Lplpo)Documento11 pagineLaporan Pemakaian Dan Lembar Permintaan Obat (Lplpo)HendriAnasPartIINessuna valutazione finora
- Advances in Analytical Techniques and Therapeutic Applications of PhytochemicalsDocumento11 pagineAdvances in Analytical Techniques and Therapeutic Applications of PhytochemicalsKIU PUBLICATION AND EXTENSIONNessuna valutazione finora
- Product Profiling and ManufacturingDocumento16 pagineProduct Profiling and ManufacturingPriyanka RawoolNessuna valutazione finora
- Pharmaceutics Chapter 7 Novel Drug Delivery System NotesDocumento10 paginePharmaceutics Chapter 7 Novel Drug Delivery System NotesBhuvnesh ChandraNessuna valutazione finora
- Sterile Product Package Integrity TestingDocumento104 pagineSterile Product Package Integrity TestingJihad Elias ChahlaNessuna valutazione finora
- Form Stock ObatDocumento7 pagineForm Stock ObatSyarifahUniqueNessuna valutazione finora
- Background of The StudyDocumento2 pagineBackground of The StudyAiza Mae RamosNessuna valutazione finora
- InventoryDocumento12 pagineInventoryMarko ParungoNessuna valutazione finora
- Insecticidal Activity of Castanospermum Australe Against Stored Grain Pest Callosobruchus AnalisDocumento3 pagineInsecticidal Activity of Castanospermum Australe Against Stored Grain Pest Callosobruchus AnalisIOSR Journal of PharmacyNessuna valutazione finora
- Propylane GlycolDocumento176 paginePropylane GlycolAgra AdiptaNessuna valutazione finora
- GMP Manual IvzDocumento36 pagineGMP Manual IvzLaith Abdul RahimNessuna valutazione finora
- M7 Post Task PharmaDocumento1 paginaM7 Post Task PharmaPanda JocyNessuna valutazione finora
- The Bacterial ChallengeDocumento54 pagineThe Bacterial Challengeepreda_1Nessuna valutazione finora
- Sun Pharma - Annual Report 2016-17Documento284 pagineSun Pharma - Annual Report 2016-17Kumar RajputNessuna valutazione finora
- List of Medicines and Stock in PharmacyDocumento74 pagineList of Medicines and Stock in PharmacyQblay AlbarnNessuna valutazione finora
- Clinical PharmacokineticsDocumento5 pagineClinical Pharmacokineticsfarha naazNessuna valutazione finora
- TABLE COMPLETION. Complete The Table by Supplying The Missing DataDocumento2 pagineTABLE COMPLETION. Complete The Table by Supplying The Missing DataShaira Dawn PlancoNessuna valutazione finora
- GMP Inspection Checklist - قائمة المراجعة (GMP)Documento24 pagineGMP Inspection Checklist - قائمة المراجعة (GMP)michael_payne353280% (5)
- GS1 Product Classification in Healthcare PDFDocumento18 pagineGS1 Product Classification in Healthcare PDFjgallegosNessuna valutazione finora
- Thesis English 4Documento21 pagineThesis English 4Hermiie Joii Galang MaglaquiiNessuna valutazione finora
- Monoclonal AntibodiesDocumento68 pagineMonoclonal AntibodiesvedabantiNessuna valutazione finora
- Rasaprakashasudhakar Chapter 1Documento42 pagineRasaprakashasudhakar Chapter 1NCSASTRO100% (1)