Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Report On "Complications", by Atul Gawande
Caricato da
hatedhero100%(1)Il 100% ha trovato utile questo documento (1 voto)
2K visualizzazioni3 pagineA bit of a change of pace. This is a report I did for school on Atul Gawande's "Complications". I got full marks on it. What do you guys think? It's a great book, I recommend it 100%.
Titolo originale
Report on "Complications", by Atul Gawande
Copyright
© © All Rights Reserved
Formati disponibili
RTF, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoA bit of a change of pace. This is a report I did for school on Atul Gawande's "Complications". I got full marks on it. What do you guys think? It's a great book, I recommend it 100%.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato RTF, PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
2K visualizzazioni3 pagineReport On "Complications", by Atul Gawande
Caricato da
hatedheroA bit of a change of pace. This is a report I did for school on Atul Gawande's "Complications". I got full marks on it. What do you guys think? It's a great book, I recommend it 100%.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato RTF, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 3
Complications
Atul Gawande's Complications is a book that is set during Gawande's
residency. It deals with some of the ethical issues in the medical/surgical
practice. Each of these fourteen stories is true, and every new story makes you
realize in a different way the one main message Gawande set out to convey, the
one that ties all of the stories together: That doctors are only human.
Part One -- Fallibility
Fallibility includes titles "Education of a Knife", "The Computer and the
Hernia Factory", "When Doctors Make Mistakes", "Nine Thousand Surgeons",
and "When Good Doctors Go Bad." This part of the book deals with ethical
issues surrounding the education of doctors and the extent to which residents
should be allowed to perform surgery on people. It also acknowledges "the gap
between what we know and what we aim for."
"Education of a Knife" is about Gawande's initial failure at inserting central
lines into patients. As he tells patients that there are very few risks involved when
the procedure is in experienced hands, he feels conflicted for withholding from
the patient the fact that he does not have experienced hands, being only a
resident. He sees his mentor perform it many times, but has never gotten it right,
and he becomes more discouraged and frustrated and scared each time. A
woman had died of massive bleeding when a resident sliced through her vena
cava; a man had to have surgery because a resident lost control of the central
line being put in; a man had a heart attack when the wire caused ventricular
fibrillation. These were some of the disasters that occurred when residents tried
to put in central lines, and when Gawande is asking the patient's permission to
perform the procedure, he does not mention any of this. He wonders, to what
extent should residents be allowed to practice on people? He goes over in his
head the numerous surgical disasters that have taken place because a resident
did something wrong.
Does the need to educate surgeons warrant practicing on people during
residency, greatly increasing the risk of something going wrong? And, he writes,
should patients be given this choice? He recalls the time when his infant son had
to have heart surgery, and a resident approached him and asked if he could
assist. Gawande adamantly refused, wanting his child's life in the most
experienced and sure of hands. It is quite easy for people to say that patients
should let residents practice upon them, that these people need their education,
that there will always be a surgeon leading the operation. But, as Gawande
discovered, the decision is much more difficult when it is your own life, or that of
someone you love.
"When Good Doctors Go Bad" is the story of Hank Goodman (his name
has been altered for confidentiality), a man who started his career by being
brilliant in residency and coasting steadily to the top of his field. He was, for a
while, the most sought-after orthopedic surgeon around. And one of the things
that set him apart from other doctors was his compassion and dedication to his
practice. When a small boy needed his hip tapped late at night, Goodman rushed
in for him, even though he wasn't on call and he had no need to be there. He
went above and beyond, especially, he says, in residency. Goodman describes
the experience as "the four best years of my life". His unwillingness to turn
people down soon made him one of the busiest orthopedic surgeons in his state.
But somewhere along the way, he started to slip. He cut corners,
sometimes with dire consequences. His patients were hurt. Colleagues who once
looked to him for inspiration became horrified with the mistakes he was making,
and that he did not make efforts to right his wrongs. This was evident in cases
like Mrs. D's (patient's real name is confidential), a mother of two who came to
Goodman with fluid swelling in her knee. The week before, she'd had surgery to
remove similar fluid, but this time she said she was quite ill and that her knee
was unbearably painful. The flesh was red-hot, and there was discharge when he
inserted a needle into the joint. It was obvious that she was suffering from a
serious infection, but Goodman was busy and didn't bring her into the hospital, or
even refer her to someone else. He waved her away, calling her a whiner, and
within the week the infection had destroyed the cartilage in her knee, wrecking
the joint for good. With the cartilage gone, she had to have her knee fused,
making her unable to bend to pick up her child or run. Any doctor can make a
mistake like this when consumed with work and not fully paying attention, but
Goodman continued to make errors like this over and over again, refusing to
admit he was wrong when he inserted the wrong size screws into joints or put
pins into the hip of an eldery man whose X-rays showed that the problem was so
serious he needed an entire hip replacement. The thing that appalled his
colleagues was not the mistakes themselves, but that Goodman refused to admit
them or correct them.
Eventually, Goodman lost his license and took a much-needed break from
medicine. When asked what lead to the downfall of his career, he could only
shake his head and say, "I don't know what happened."
Part Two -- Mystery
Mystery includes titles "Full Moon Friday the Thirteenth", "The Pain
Perplex", "A Queasy Feeling", "Crimson Tide", and "The Man Who Couldn't Stop
Eating". These stories are about the unpredictable things in medicine that can't
be accounted for.
"The Pain Perplex" is about a man named Robert Scott Quinlan, who, after
fracturing his shoulder, developed severe pain spasms in his back. His CT scans,
X-rays, and other tests all came back clean, and no one could find any reason to
operate on his back. Gawande and the other doctors were skeptical, because his
entire workup was clean. Many chronic pain patients fake it for narcotic
prescriptions, and for many it is psychosomatic instead of merely physical. But
Quinlan was not on narcotics, claiming they didn't help, and his moods had been
the same as usual, with no added stress. The doctors had no idea what was
going on and couldn't think of a reason for him to be faking it. He wasn't
interested in drugs or trying to get a card for a handicap parking space because
he was lazy. But the disturbing thing about his case is that it is very typical.
Chronic patients are extremely common, and a dilemma doctors face is how to
know if they're faking it, and when to turn them away. Over time, Quinlan's back
pain worsened and he wanted an operation, but his tests showed no signs of a
ruptured or slipped disk, which is a common cause of chronic back pain in the
elderly and the most likely to be afflicting him, or any other problem. Studies point
to mundane things as a cause of chronic pain, "inorganic" factors such as
loneliness or job dissatisfaction. Quinlan's wife reported to the doctors that he
had been having mood swings and periods of depression, but no one was ever
sure if that was the cause or the result of his debilitating pain.
Part Three -- Uncertainty
Uncertainty includes titles "Final Cut", "The Dead Baby Mystery", "Whose
Body is it, Anyway?", and "The Case of the Red Leg". Part Three explores the
types of outside influences that can make or break the correctness of a medical
decision, and how they can complicate confirming or treating the diagnosis.
In "The Dead Baby Mystery", Marie Noe had lost all ten of her children as
infants. One was stillborn and one expired at the hospital shortly after birth, but
the other eight died at her home, where Noe said she found them all dead in their
cribs. Each year, thousands of infants die inexplicably in bed each year, a
circumstance dubbed Sudden Infant Death Syndrome, or SIDS. In 1998, when
Noe was seventy, new medical evidence was found that determined that she had
smothered her children with a pillow. Gawande writes that this puzzles him,
because the bodies of the infants were now just bone, making it seemingly
difficult to determine that the babies had been suffocated. So what was their
actual basis for charging Marie Noe with eight counts of first degree murder?
Under promise of anonymity, an official admitted that there was, in fact, no direct
evidence that proved Noe guilty of murder. She was charged under speculation.
A medical examiner working on the case said, "One SIDS death is a tragedy.
Two is a mystery. Three is murder." When it all comes down to it, sometimes
science isn't the deciding factor in decisions, but rather what people have to say.
Potrebbero piacerti anche
- Silvester, W The Age - 20-3-11Documento5 pagineSilvester, W The Age - 20-3-11Dying with Dignity NSWNessuna valutazione finora
- How Doctors DieDocumento8 pagineHow Doctors DieFeat GasNessuna valutazione finora
- Origin - A YA Superhero Short Story: The Hero of Heartland, #0Da EverandOrigin - A YA Superhero Short Story: The Hero of Heartland, #0Nessuna valutazione finora
- Killer Care: How Medical Error Became America's Third Largest Cause of Death, and What Can Be Done About ItDa EverandKiller Care: How Medical Error Became America's Third Largest Cause of Death, and What Can Be Done About ItValutazione: 4.5 su 5 stelle4.5/5 (2)
- Referat EticaDocumento5 pagineReferat EticaCarp Petru-CosminNessuna valutazione finora
- The Unexpected Patient: True Kiwi stories of life, death and unforgettable clinical casesDa EverandThe Unexpected Patient: True Kiwi stories of life, death and unforgettable clinical casesNessuna valutazione finora
- Shortcake: Impulse Reborn: The Shortcake Trilogy, #2Da EverandShortcake: Impulse Reborn: The Shortcake Trilogy, #2Nessuna valutazione finora
- Summary of Outlive by Peter Attia MD : The Science and Art of LongevityDa EverandSummary of Outlive by Peter Attia MD : The Science and Art of LongevityNessuna valutazione finora
- March 12, 2012, 2:56 PM, Things Adult Medicine Could Learn From Pediatrics, by PERRI KLASS, M.D., ColumnistDocumento4 pagineMarch 12, 2012, 2:56 PM, Things Adult Medicine Could Learn From Pediatrics, by PERRI KLASS, M.D., ColumnistSSSS123JNessuna valutazione finora
- Assignment 2Documento3 pagineAssignment 2api-725270319Nessuna valutazione finora
- Being MortalDocumento5 pagineBeing Mortalapi-391829073Nessuna valutazione finora
- 6.1.22 DisabilityDocumento2 pagine6.1.22 DisabilityTim BrownNessuna valutazione finora
- Medical Malpractice CasesDocumento5 pagineMedical Malpractice Casesankitjakhar35Nessuna valutazione finora
- An Excerpt From "Crooked: Outwitting The Back Pain Industry and Getting On The Road To Recovery"Documento4 pagineAn Excerpt From "Crooked: Outwitting The Back Pain Industry and Getting On The Road To Recovery"OnPointRadioNessuna valutazione finora
- The $1,000 Genome: The Revolution in DNA Sequencing and the New Era of Personalized MedicineDa EverandThe $1,000 Genome: The Revolution in DNA Sequencing and the New Era of Personalized MedicineValutazione: 3.5 su 5 stelle3.5/5 (4)
- Saving Grace: What Patients Teach Their Doctors about Life, Death, and the Balance in BetweenDa EverandSaving Grace: What Patients Teach Their Doctors about Life, Death, and the Balance in BetweenNessuna valutazione finora
- Better A Surgeons Notes On PerformanceDocumento2 pagineBetter A Surgeons Notes On PerformanceDivyesh DholariyaNessuna valutazione finora
- Robin Cook - Medico Interno (Year of The Intern) InglesDocumento133 pagineRobin Cook - Medico Interno (Year of The Intern) InglesIver Snney Vega Junieles50% (4)
- Chapter 10 of 10 - ConclusionDocumento3 pagineChapter 10 of 10 - ConclusionspiritualbeingNessuna valutazione finora
- Being Mortal: Medicine and What Matters in The EndDocumento15 pagineBeing Mortal: Medicine and What Matters in The EndEsteban0% (19)
- Cured: Strengthen Your Immune System and Heal Your LifeDa EverandCured: Strengthen Your Immune System and Heal Your LifeValutazione: 4 su 5 stelle4/5 (4)
- Box of Birds: What New Zealand taught me about life and the practice of medicineDa EverandBox of Birds: What New Zealand taught me about life and the practice of medicineNessuna valutazione finora
- Courtroom Speeches HandoutDocumento4 pagineCourtroom Speeches Handouthumaira.khanum01Nessuna valutazione finora
- Ejercicios de InglésDocumento9 pagineEjercicios de Inglésnatalia mendozaNessuna valutazione finora
- Profile Ahmad AyyadDocumento3 pagineProfile Ahmad Ayyadapi-537678695Nessuna valutazione finora
- Getting BetterDocumento18 pagineGetting BetterSonia AceresNessuna valutazione finora
- Argument PaperDocumento5 pagineArgument Paperapi-236956945Nessuna valutazione finora
- Robin Cook - Year of The InternDocumento140 pagineRobin Cook - Year of The Internmonktheop1155Nessuna valutazione finora
- Thesis Statement Pro EuthanasiaDocumento6 pagineThesis Statement Pro Euthanasiamizhesternewark100% (1)
- Healing Healthcare: How Doctors and Patients Can Heal Our Sick SystemDa EverandHealing Healthcare: How Doctors and Patients Can Heal Our Sick SystemNessuna valutazione finora
- Why Doctors Get It Wrong About When You Will Die - Life and Style - The GuardianDocumento6 pagineWhy Doctors Get It Wrong About When You Will Die - Life and Style - The GuardianlamacarolineNessuna valutazione finora
- 1 3 - Cómo Este Médico Está Cambiando El Campo de La Ortopedia - TRADUCIDO Oct2022Documento7 pagine1 3 - Cómo Este Médico Está Cambiando El Campo de La Ortopedia - TRADUCIDO Oct2022Choco LalaNessuna valutazione finora
- After the Error: Speaking Out About Patient Safety to Save LivesDa EverandAfter the Error: Speaking Out About Patient Safety to Save LivesNessuna valutazione finora
- NHS Accused of Involuntary Euthanasia of Tens of Thousands in UKDocumento8 pagineNHS Accused of Involuntary Euthanasia of Tens of Thousands in UKSheree GeoNessuna valutazione finora
- Medical Malpractice COMPLETEDocumento9 pagineMedical Malpractice COMPLETEAlexis Von TeNessuna valutazione finora
- Gloria Costa Blanca News 17 Feb 2012Documento3 pagineGloria Costa Blanca News 17 Feb 2012Geoffrey JaveaNessuna valutazione finora
- Our Stroke of Luck: New Technology Enables Stroke Victims to Make a Full RecoveryDa EverandOur Stroke of Luck: New Technology Enables Stroke Victims to Make a Full RecoveryNessuna valutazione finora
- Cure of All DiseasesDocumento327 pagineCure of All DiseasesJorge BarataNessuna valutazione finora
- DNRDocumento10 pagineDNRJoel SantosNessuna valutazione finora
- EthicalDocumento15 pagineEthicaljodNessuna valutazione finora
- Being Mortal GDocumento1 paginaBeing Mortal Gapi-295079231Nessuna valutazione finora
- Before The Light DiesDocumento14 pagineBefore The Light DiesStephen RalphNessuna valutazione finora
- That One Patient: Doctors and Nurses’ Stories of the Patients Who Changed Their Lives ForeverDa EverandThat One Patient: Doctors and Nurses’ Stories of the Patients Who Changed Their Lives ForeverNessuna valutazione finora
- Group Case StudyDocumento5 pagineGroup Case StudySiti SurayaNessuna valutazione finora
- Surgeon's Story: Inside OR-1 with One of America’s Top Pediatric Heart SurgeonsDa EverandSurgeon's Story: Inside OR-1 with One of America’s Top Pediatric Heart SurgeonsValutazione: 4.5 su 5 stelle4.5/5 (3)
- Is It Dangerous To Believe in CAM?Documento2 pagineIs It Dangerous To Believe in CAM?Michael SmithNessuna valutazione finora
- Dr. Kevorkian Research PaperDocumento6 pagineDr. Kevorkian Research Papervstxevplg100% (1)
- HarvardDocumento5 pagineHarvardsyed umairNessuna valutazione finora
- I'm Good With NamesDocumento1 paginaI'm Good With NameshatedheroNessuna valutazione finora
- Things I HateDocumento1 paginaThings I HatehatedheroNessuna valutazione finora
- Lucid DreamsDocumento1 paginaLucid DreamshatedheroNessuna valutazione finora
- Care - Day 29Documento1 paginaCare - Day 29hatedheroNessuna valutazione finora
- A Conscious Stream of Thought - Day 26Documento1 paginaA Conscious Stream of Thought - Day 26hatedheroNessuna valutazione finora
- Untitled PoemDocumento1 paginaUntitled Poemhatedhero100% (1)
- Quiet A MomentDocumento1 paginaQuiet A MomenthatedheroNessuna valutazione finora
- The Painting - Day 30Documento3 pagineThe Painting - Day 30hatedhero100% (1)
- Time To SleepDocumento1 paginaTime To SleephatedheroNessuna valutazione finora
- The Artist (Part 1)Documento8 pagineThe Artist (Part 1)hatedhero100% (1)
- The Rapture - Day 31Documento1 paginaThe Rapture - Day 31hatedheroNessuna valutazione finora
- I Say Okay - Day 28Documento1 paginaI Say Okay - Day 28hatedheroNessuna valutazione finora
- Putting On Clothes - Day 19Documento1 paginaPutting On Clothes - Day 19hatedheroNessuna valutazione finora
- Promise - Day 24Documento1 paginaPromise - Day 24hatedhero100% (1)
- A Lifetime - Day 27Documento2 pagineA Lifetime - Day 27hatedheroNessuna valutazione finora
- This Kind of Morning - Day 9Documento1 paginaThis Kind of Morning - Day 9hatedheroNessuna valutazione finora
- Shame - Day 25Documento1 paginaShame - Day 25hatedheroNessuna valutazione finora
- Reality Exists - Day 23Documento1 paginaReality Exists - Day 23hatedhero100% (1)
- Solid Light - Day 13Documento1 paginaSolid Light - Day 13hatedheroNessuna valutazione finora
- Dichotomy - Day 21Documento1 paginaDichotomy - Day 21hatedheroNessuna valutazione finora
- A Real Artist - Day 17Documento1 paginaA Real Artist - Day 17hatedheroNessuna valutazione finora
- SHH - Day 22Documento1 paginaSHH - Day 22hatedhero100% (1)
- Say Something - Day 16Documento1 paginaSay Something - Day 16hatedhero100% (1)
- Scared - Day 10Documento1 paginaScared - Day 10hatedheroNessuna valutazione finora
- Wash Away Face - Day 15Documento1 paginaWash Away Face - Day 15hatedhero100% (2)
- When I Open My Mouth - Day 4Documento1 paginaWhen I Open My Mouth - Day 4hatedhero100% (2)
- Wandering Son - Day 14Documento1 paginaWandering Son - Day 14hatedheroNessuna valutazione finora
- I See Not Wrong - Day 3Documento1 paginaI See Not Wrong - Day 3hatedheroNessuna valutazione finora
- Birdcage - Day 5Documento1 paginaBirdcage - Day 5hatedhero100% (1)
- Corruption - Day 2Documento4 pagineCorruption - Day 2hatedheroNessuna valutazione finora
- Mouse Deer and TigerDocumento2 pagineMouse Deer and Tigeralan.nevgan100% (1)
- 5.case Study: Effects of Homeopathic Medicines in AdultsDocumento2 pagine5.case Study: Effects of Homeopathic Medicines in AdultsAMEEN ARTSNessuna valutazione finora
- CDI-500 Specialized Crime Investigation and Legal MedicineDocumento20 pagineCDI-500 Specialized Crime Investigation and Legal MedicineCherry Len FaroniloNessuna valutazione finora
- Introducing Inspira's: Managed Noc & Itoc ServicesDocumento2 pagineIntroducing Inspira's: Managed Noc & Itoc ServicesmahimaNessuna valutazione finora
- Mill Test Certificate: Jindal Stainless (Hisar) LimitedDocumento1 paginaMill Test Certificate: Jindal Stainless (Hisar) Limitedhemantmech09920050% (2)
- Unit 3 Assignment - CompletedDocumento7 pagineUnit 3 Assignment - CompletedSu GarrawayNessuna valutazione finora
- Kelas 1 AlphabetTITLE Kelas 1 Numbers ConversationTITLE Kelas 2 Feelings Body PartsDocumento54 pagineKelas 1 AlphabetTITLE Kelas 1 Numbers ConversationTITLE Kelas 2 Feelings Body PartsArti Hikmatullah Perbawana Sakti BuanaNessuna valutazione finora
- Diff Types of Transmission Lines Used in CommsDocumento9 pagineDiff Types of Transmission Lines Used in CommsLe AndroNessuna valutazione finora
- Mahindra Powertrain - Market StrategyDocumento4 pagineMahindra Powertrain - Market StrategyEshan KapoorNessuna valutazione finora
- Makalah Bahasa Inggris - Narrative TextDocumento21 pagineMakalah Bahasa Inggris - Narrative TextFenny KartikaNessuna valutazione finora
- Turbine Stress EvaluatorDocumento14 pagineTurbine Stress EvaluatorsumitNessuna valutazione finora
- Hart Fuller Debate: Hart Fuller Debate Is One of The Most Interesting Academic Debates of All Times That Took Place inDocumento1 paginaHart Fuller Debate: Hart Fuller Debate Is One of The Most Interesting Academic Debates of All Times That Took Place inAmishaNessuna valutazione finora
- S10 Electric Power PackDocumento12 pagineS10 Electric Power PackrolandNessuna valutazione finora
- Shariff NDocumento4 pagineShariff NKruu ChinnuNessuna valutazione finora
- Eng ThreePDocumento192 pagineEng ThreePMr Ahmed AbdallahNessuna valutazione finora
- Rotary Gear Pump Manufacturers in India, Pulp Valve Manufacturers IndiaDocumento3 pagineRotary Gear Pump Manufacturers in India, Pulp Valve Manufacturers IndiaKirit IndustriesNessuna valutazione finora
- Manual of Curatorship: A Guide To Museum PracticeDocumento7 pagineManual of Curatorship: A Guide To Museum PracticeLuísa MenezesNessuna valutazione finora
- Practice: Circles and ArcsDocumento2 paginePractice: Circles and ArcsTIANA ARILENessuna valutazione finora
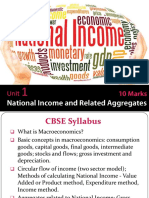
- MACRO XII Subhash Dey All Chapters PPTs (Teaching Made Easier)Documento2.231 pagineMACRO XII Subhash Dey All Chapters PPTs (Teaching Made Easier)Vatsal HarkarNessuna valutazione finora
- NTE56004 Thru NTE56010 TRIAC, 15 Amp: FeaturesDocumento2 pagineNTE56004 Thru NTE56010 TRIAC, 15 Amp: FeaturesFreddy SarabiaNessuna valutazione finora
- Tramadol Drug StudyDocumento1 paginaTramadol Drug Studymilkv82% (11)
- Secretary Birds: Fascinating Hunters of the African SavannahDocumento32 pagineSecretary Birds: Fascinating Hunters of the African Savannahpwint phyu kyawNessuna valutazione finora
- Ex Ophtalmo Eng 1Documento4 pagineEx Ophtalmo Eng 1Roxana PascalNessuna valutazione finora
- LirikDocumento537 pagineLirikMuhamad Iqbal FahmiNessuna valutazione finora
- Refraction Through Lenses & Optical Instruments5Documento144 pagineRefraction Through Lenses & Optical Instruments5geniusamahNessuna valutazione finora
- Mar For M: I MMQ SeriesDocumento28 pagineMar For M: I MMQ SeriesIpal Febri NartaNessuna valutazione finora
- 1 s2.0 S2210803316300781 MainDocumento8 pagine1 s2.0 S2210803316300781 MainGilang Aji P. EmonNessuna valutazione finora
- Grammarism Ed Ing Adjectives Test 4 1189424Documento2 pagineGrammarism Ed Ing Adjectives Test 4 1189424Royal Stars Drama AcademyNessuna valutazione finora
- Pre Test and Post TestDocumento27 paginePre Test and Post TestMATALANG GRACENessuna valutazione finora
- 322439480MVR Single Page Single Page Booklet - OPTDocumento12 pagine322439480MVR Single Page Single Page Booklet - OPTlarry vargas bautistaNessuna valutazione finora