Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
A Case of Sodium Chlorite Toxicity Managed With Concurrent Renal Replacement Therapy and Red Cell Exchange
Caricato da
the fifth estateTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
A Case of Sodium Chlorite Toxicity Managed With Concurrent Renal Replacement Therapy and Red Cell Exchange
Caricato da
the fifth estateCopyright:
Formati disponibili
J. Med. Toxicol.
(2013) 9:6770
DOI 10.1007/s13181-012-0256-9
TOXICOLOGY OBSERVATION
A Case of Sodium Chlorite Toxicity Managed with Concurrent
Renal Replacement Therapy and Red Cell Exchange
Adam Romanovsky & Dennis Djogovic & Dat Chin
Published online: 21 September 2012
# The Author(s) 2012. This article is published with open access at Springerlink.com
Abstract
Introduction Sodium chlorite is a powerful oxidizing agent
with multiple commercial applications. We report the presentation and management of a single case of human toxicity of sodium chlorite.
Case report A 65-year-old man presented to hospital after
accidentally ingesting a small amount of a sodium chlorite
solution. His principal manifestations were mild methemoglobinemia, severe oxidative hemolysis, disseminated intravascular coagulation, and anuric acute kidney injury. He was
managed with intermittent hemodialysis, followed by continuous venovenous hemofiltration for management of acute
kidney injury and in an effort to remove free plasma chlorite.
Concurrently, he underwent two red cell exchanges, as well as
a plasma exchange, to reduce the burden of red cells affected
by chlorite. These interventions resulted in the cessation of
hemolysis with stabilization of serum hemoglobin and platelets. The patient survived and subsequently recovered normal
renal function.
Discussion This is only the second case of sodium chlorite
intoxication reported in the medical literature and the first to
A. Romanovsky : D. Djogovic : D. Chin
Division of Critical Care Medicine, University of Alberta,
Edmonton, AB, Canada
A. Romanovsky
Division of Nephrology, University of Alberta,
Edmonton, AB, Canada
D. Djogovic
Department of Emergency Medicine, University of Alberta,
Edmonton, AB, Canada
A. Romanovsky (*)
General Systems Intensive Care Unit,
University of Alberta Hospital,
3C1.12 WMC, 8440 112 Street,
Edmonton, AB T6G 2B7, Canada
e-mail: asr1@ualberta.ca
report the use of renal replacement therapy in combination
with red cell exchange in its management.
Keywords Sodium chlorite . Renal replacement therapy .
Red cell exchange . Plasma exchange . Oxidative hemolysis .
Acute kidney injury
Introduction
Sodium chlorite is a powerful oxidizing agent used to generate chlorine dioxide, which has several applications, including bleaching of pulp, paper, and textiles. When
ingested, oxidizing agents can lead to methemoglobinemia,
and intravascular hemolysis may ensue. Only one case of
sodium chlorite ingestion has been reported in the literature
[1]. We report the only known case of accidental sodium
chlorite ingestion leading to mild methemoglobinemia, severe hemolysis, and acute kidney injury (AKI) successfully
treated with hemodialysis, followed by hemofiltration and
concurrent red cell and plasma exchange.
Case
A 65-year-old man presented to his local hospital with
nausea, vomiting, diarrhea, and dark urine after ingesting a
small amount of a 28 % sodium chlorite solution. He had
diluted the sodium chlorite in a cup with an unmeasured
amount of water and was using this solution to clean his
fruit. He then accidentally drank a mouthful of the solution
after confusing this cup with another that contained only
water. Upon ingestion, he immediately self-induced vomiting, and only after 4 h when he noticed dusky finger tips and
lips, did he present to the hospital. He was transferred to our
institution and, upon arrival, was hemodynamically stable,
mildly confused, and anuric. Initial pertinent laboratory
68
results revealed hemoglobin 184 g/L, white blood cell count
22.1109/L, normal platelet count, creatinine 144 mol/L,
sodium 141 mmol/L, potassium 5.5 mmol/L, bicarbonate
19 mmol/L, chloride 114 mmol/L, calculated anion gap 14,
ionized calcium 1.13 mmol/L, phosphate 1.37 mmol/L, and
haptoglobin of <0.08 g/L. Bilirubin and lactate dehydrogenase
were unable to be processed by the laboratory, but the serum
was described as being brownish in color. Urine was brown,
and examination showed 3+ hemoglobin, with few red blood
cells and many hemegranular casts. Initial arterial blood gas
showed pH 7.35, paCO2 35 mmHg, paO2 256 mmHg, methemoglobin (MetHb) 6.7 %, and lactate 1.8 mmol/L.
He was admitted to the intensive care unit and treated
with an 8-h session of hemodialysis to manage hyperkalemia and to attempt removal of sodium chlorite. We used a
high-flux dialysis filter (Toray TS-1.6SL polysulfone filter)
and prescribed a blood flow of 400 mL/min with a dialysate
flow of 500 mL/min to maximize clearance. The dialysate
contained electrolytes in the following concentrations: bicarbonate 35 mmol/L, sodium 140 mmol/L, potassium
2 mmol/L, magnesium 0.75 mmol/L, calcium 1.5 mmol/L,
and glucose 8 mmol/L.
He was not treated with methylene blue or ascorbic acid but
was started on a high-dose N-acetylcysteine infusion. We used
the 21-h intravenous N-acetylcysteine regimen recommended
in acetaminophen toxicity (150 mg/kg over 1 h, followed by
50 mg/kg over 4 h then 100 mg/kg over 16 h). While on
dialysis, his MetHb levels decreased to normal, but upon its
completion, he developed an increasing lactate (8.2 mmol/L),
a drop in hemoglobin to 87 g/L, and hemodynamic instability
requiring intravenous fluid resuscitation and vasopressor support with norepinephrine (10 mcg/min). A serum glucose-6phosphate dehydrogenase (G6PD) screen revealed deficiency,
and plasma-free hemoglobin was markedly elevated at
1,783 mg/L. A peripheral blood film showed blister and bite
cells consistent with oxidative hemolysis, with no evidence of
microangiopathic hemolysis. It also showed marked thrombocytopenia due to peripheral consumption with platelets of 28
106/L. In addition to thrombocytopenia, elevated PT INR
(1.4) and D-dimer (15.43 mg/L) were consistent with the
diagnosis of disseminated intravascular coagulation (DIC).
Peak fibrinogen and creatine kinase were 2.2 g/L and
2,926 U/L, respectively.
High FiO2 was delivered via a non-rebreather mask, and
continuous venovenous hemofiltration (CVVH) with a total
effluent of 50 mL/kg was initiated. The filter used was
Gambro ST100 AN69 membrane, and replacement fluid
was Gambro PrismaSol with electrolyte concentrations as
follows: bicarbonate 32 mmol/L, sodium 140 mmol/L, potassium 3 mmol/L, chloride 108 mmol/L, magnesium
0.5 mmol/L, and lactate 3.0 mmol/L. Concurrently, red cell
exchange was initiated via a separate 12 French dual lumen
central venous catheter. Upon completion of the 2-h long red
J. Med. Toxicol. (2013) 9:6770
cell exchange (total of 3.3 L exchanged), his symptoms
improved, and the lactate and plasma-free hemoglobin
decreased to 4.8 mmol/L and 967 mg/L, respectively,
(Fig. 1). After an initial several hours of stability, his
hemoglobin again dropped to 83 g/L. This was accompanied by worsening nausea and back pain, as well as
an increase in lactate to 9.5 mmol/L and a recurrence of
hemodynamic instability. He underwent a second session
of red cell exchange (2 h with total exchange of 2 L),
which was followed by plasma exchange (3.5 h with
5.2 L exchanged). With this exchange, his symptoms
again abated, and his lactate normalized. Plasma-free
hemoglobin decreased to 125 mg/L.
He subsequently remained stable with no further drops in
hemoglobin or rises in lactate. He underwent esophagogastroduodenoscopy which revealed only superficial gastric
ulcers. Repeat screens for G6PD deficiency at 4 days and
12 months were negative. He was continued on continuous
renal replacement for 96 h in total at which time he was
transitioned to intermittent hemodialysis as he remained
anuric; 17 days after admission to hospital, he was no longer
dialysis-dependent and was discharged home. Over the following 2 months, his serum creatinine returned to its premorbid level of 94 mol/L.
Discussion
Sodium chlorite is a white crystal that is readily dissolvable in water. Its primary commercial application is that of
a bleaching agent in the pulp and paper and textile industries. Outside of its commercial uses, it has numerous
unfounded claims as a natural health cure for a multitude of health issues.
Fig. 1 Serum hemoglobin, lactate, and plasma-free hemoglobin (PFH)
over time
J. Med. Toxicol. (2013) 9:6770
Although there is not an abundance of data regarding the
physiologic effects of sodium chlorite, several animal and
human studies have documented its ability to cause methemoglobinemia, hemolysis, and glutathione depletion [2].
More physiologic data exist for the related compound, sodium chlorate [3, 4]. A study by Singelmann et al. examined
the effect of incubating human red cells with varying concentrations of chlorate, showing that these red cells develop
glutathione depletion and methemoglobinemia. In addition,
chlorate led to inhibition of G6PD and increased membrane
rigidity. This drug-induced G6PD deficiency, in addition to
glutathione depletion and membrane rigidity, leads to oxidative hemolysis and explains the lack of efficacy of methylene blue in these patients [3, 4]. Importantly, Steffen et al.
noted that the presence of methemoglobin was necessary for
inhibition of G6PD and cross-linking of membrane proteins.
If, however, hypochlorite was used instead of chlorate;
oxidation of hemoglobin and oxidative hemolysis occurred
independent of methemoglobin. This feature may explain
the severity of hemolysis in our case, despite the presence of
only mild methemoglobinemia.
Only one previous case of acute sodium chlorite toxicity
has been reported in the literature [1]. Lin et al. described a
case of intentional ingestion of sodium chlorite leading to
severe methemoglobinemia, hemolysis, DIC, and renal failure. The patient presented with a MetHb level of 59 %,
which did not respond to administration of multiple doses
of methylene blue. He subsequently developed hemolysis
and DIC and was treated with continuous arteriovenous
hemofiltration. He survived and eventually recovered renal
function.
Our patient presented with similar gastric upset, likely as
a result of chlorite-induced irritation of the gastric mucosa.
Unlike the previous case, our patient presented with only
mild methemoglobinemia. Despite this, he developed inhibition of G6PD and went on to suffer life-threatening oxidative hemolysis. This suggests that methemoglobinemia is
not a prerequisite for chlorite-induced enzyme inhibition
and membrane protein cross-linking. Due to the low levels
of MetHb, acute G6PD deficiency, and previous lack of
efficacy reported for chlorate and chlorite ingestions, we
chose not to administer methylene blue or ascorbic acid.
We did, however, employ high-dose N-acetylcysteine in an
attempt to replenish depleted glutathione stores. Although
we had no data to suggest its use, we felt that there was a
theoretical benefit with minimal risk of adverse consequences. It is unclear what factors contributed to the discrepancy
between MetHb levels and hemolysis in the two cases. It
may be that a smaller ingested amount of chlorite resulted in
less MetHb, although this leaves unexplained the similar
degree of hemolysis in the two cases. It is plausible, as
explained above, that oxidative hemolysis with chlorite
may occur independently of methemoglobinemia.
69
In the absence of severe methemoglobinemia, we believe
that the intermittent lactic acidosis resulted from a combination of decreased oxygen-carrying capacity and reduced
tissue perfusion. The patient had hemolyzed more than half
of his red cells, thereby reducing oxygen-carrying capacity
of more than 50 %. In addition, massive hemolysis can lead
to hypotension due to peripheral vasodilation, thereby leading to reduced tissue perfusion and lactic acidosis [5]. This
explains the simultaneous occurrence of hemolysis, hypotension, and increasing serum lactate levels.
The exact cause of the acute kidney injury is unclear but
is likely multifactorial. Lin et al. reported a diagnosis of
acute interstitial nephritis in a patient with sodium chlorite
toxicity [1]. Findings on renal biopsy included acute tubulointerstitial changes, lymphocytic infiltration, and severe
interstitial edema. They also described moderate tubule
damage with hemorrhage and necrosis along with focally
collapsed loops. However, several of these findings, such as
necrosis, are not usual findings of interstitial nephritis. In
addition, the extremely rapid progression to anuria is not
consistent with interstitial nephritis.
Several studies of chlorate, a chemically similar compound to chlorite, suggest that renal toxicity is due to a
combination of methemoglobinuria, direct proximal tubular
toxicity, and possibly lesions similar to those seen with the
hemolytic uremic syndrome [4, 6]. In the absence of severe
methemoglobinemia, it is likely that the patients AKI is
accounted for by a combination of tubular toxicity from
hemoglobin and renal ischemia due to poor oxygen delivery.
The renal medulla has a very low oxygen tension in normal
conditions and is, therefore, extremely sensitive to reduced
systemic oxygen delivery. Cases of renal failure with other
forms of oxidative hemolysis support this theory [7].
With a molecular weight of 67.45 daltons, unbound chlorite should be effectively removed by hemodialysis with a
standard or high-flux dialysis membrane. Our patients hemoglobin and hemodynamics remained stable while receiving IHD, which we theorize may be related to removal of
free chlorite. It is important to note that the amount of free
versus bound chlorite in serum is unknown, and that hemodialysis was undertaken both to manage AKI and in an
attempt to remove any free chlorite. It is difficult to know
whether or not extracorporeal removal of chlorite played a
significant role in improving the patients outcome, and it
remains possible that it was of little benefit.
In trying to remove small toxins, such as chlorite, high
efficiency clearance achieved with intermittent hemodialysis
dictates that this be the modality of choice. The volume of
distribution of chlorite is unknown; therefore, a prolonged
session of intermittent dialysis, similar to that used in a
lithium overdose, is prudent.
Our patient developed worsening hemolysis after completion of a session of intermittent hemodialysis, which we
70
suspected was due to a rebound increase in serum chlorite
levels secondary to redistribution from the extravascular
space. Due to intermittent hemodynamic instability and in
an attempt to avoid rebound increases in serum chlorite
levels, continuous renal replacement therapy was initiated.
We prescribed a relatively high dose of CVVH (50 mL/kg)
to maximize clearance of chlorite. Pure hemofiltration was
chosen over dialysis in an effort to enhance clearance of free
hemoglobin and limit renal tubular damage. It is, however,
unlikely that removal of free hemoglobin altered the course
of AKI as the patient was already anuric.
Although not previously used in chlorite intoxication, red
cell exchange has been used in numerous chlorate ingestions,
with variable success [6, 8]. We undertook red cell exchange
to reduce the burden of red cells affected by chlorite. Indeed,
the patient did significantly improve with this intervention. It
is unclear if his subsequent deterioration was due to residual
abnormal red cells, serum chlorite affecting transfused red
cells, or progressive DIC from the persistent presence of
hemolytic waste products in the plasma [6]. A second red cell
exchange was therefore performed together with a plasma
exchange, resulting in cessation of hemolysis and continued
physiologic stability.
In conclusion, it is important to consider sodium chlorite
ingestion when encountered by a patient with hemolysis, with
or without methemoglobinemia. Methylene blue is ineffective
for reducing MetHb. Although no clinical evidence exists for
its use, high-dose N-acetylcysteine may be considered for its
theoretical benefit along with minimal risk.
This is the first reported case of sodium chlorite toxicity
managed with hemodialysis, hemofiltration, and concurrent
red cell and plasma exchange. Without larger case series or
J. Med. Toxicol. (2013) 9:6770
prospective studies, it is difficult to suggest this as standard
of care; but with physiologic reasoning, our successful patient outcome, and minimal risk, it should be strongly considered in the critically ill patient with related exposure.
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution,
and reproduction in any medium, provided the original author(s) and
the source are credited.
References
1. Lin JL, Lim PS (1993) Acute sodium chlorite poisoning associated
with renal failure. Ren Fail 15(5):645648
2. Couri D, Abdel-Rahman MS, Bull RJ (1982) Toxicological effects
of chlorine dioxide, chlorite and chlorate. Environ Health Perspect
46:1317
3. Singelmann E, Wetzel E, Adler G, Steffen C (1984) Erythrocyte
membrane alterations as the basis of chlorate toxicity. Toxicology
30(2):135147
4. Steffen C, Wetzel E (1993) Chlorate poisoning: mechanism of
toxicity. Toxicology 84(1-3):217231
5. Dzik WH (2002) Cardinal signs of reactions: hypotension following
blood transfusion. Vox Sang 83(Suppl 1):145146
6. Steffen C, Seitz R (1981) Severe chlorate poisoning: report of a
case. Arch Toxicol 48(4):281288
7. Schuurman M, van Waardenburg D, Da Costa J, Niemarkt H, Leroy
P (2009) Severe hemolysis and methemoglobinemia following fava
beans ingestion in glucose-6-phosphatase dehydrogenase deficiency: case report and literature review. Eur J Pediatr 168(7):779782
8. Eysseric H, Vincent F, Peoch M, Marka C, Aitken Y, Barret L
(2000) A fatal case of chlorate poisoning: confirmation by ion
chromatography of body fluids. J Forensic Sci 45(2):474477
Potrebbero piacerti anche
- Rubin Lab Methodology For Shrimp ProjectDocumento9 pagineRubin Lab Methodology For Shrimp Projectthe fifth estateNessuna valutazione finora
- Marketplace Plastic Waste March 2019Documento7 pagineMarketplace Plastic Waste March 2019the fifth estate0% (1)
- Marketplace Plastic Waste March 2019Documento8 pagineMarketplace Plastic Waste March 2019the fifth estateNessuna valutazione finora
- What The Yale Team StudiedDocumento5 pagineWhat The Yale Team Studiedthe fifth estateNessuna valutazione finora
- CBC Marketplace Statement - November 12, 2018Documento1 paginaCBC Marketplace Statement - November 12, 2018the fifth estateNessuna valutazione finora
- Rice Test ResultsDocumento2 pagineRice Test Resultsthe fifth estate0% (1)
- Studies Provided by LifeLabs and DynacareDocumento48 pagineStudies Provided by LifeLabs and Dynacarethe fifth estateNessuna valutazione finora
- Gray - Media Release July 21 2016Documento3 pagineGray - Media Release July 21 2016the fifth estateNessuna valutazione finora
- Response - ShroffDocumento12 pagineResponse - Shroffthe fifth estateNessuna valutazione finora
- Read The Waivers From The Parks Marketplace VisitedDocumento45 pagineRead The Waivers From The Parks Marketplace Visitedthe fifth estateNessuna valutazione finora
- Axact RespondsDocumento3 pagineAxact Respondsthe fifth estateNessuna valutazione finora
- DeBungee OIPRD Investigative Report - February 15 2018Documento126 pagineDeBungee OIPRD Investigative Report - February 15 2018the fifth estateNessuna valutazione finora
- Full Results For Cosmetic Samples Lab TestDocumento3 pagineFull Results For Cosmetic Samples Lab Testthe fifth estateNessuna valutazione finora
- Statement From The Law Society of Upper CanadaDocumento2 pagineStatement From The Law Society of Upper Canadathe fifth estate100% (1)
- Dismissal MotionDocumento24 pagineDismissal Motionthe fifth estateNessuna valutazione finora
- Leaked Documents From Panama PapersDocumento2 pagineLeaked Documents From Panama Papersthe fifth estateNessuna valutazione finora
- Shroff Notice of Civil Claim May 6 2015Documento20 pagineShroff Notice of Civil Claim May 6 2015the fifth estateNessuna valutazione finora
- Amended and Supplemental Summons.Documento252 pagineAmended and Supplemental Summons.the fifth estateNessuna valutazione finora
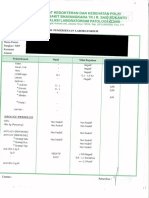
- Bhayangkara Police Hospital, Jakarta, Indonesia // July 16, 2014Documento1 paginaBhayangkara Police Hospital, Jakarta, Indonesia // July 16, 2014the fifth estateNessuna valutazione finora
- Mistry Notice of Civil Claim May 6 2015Documento17 pagineMistry Notice of Civil Claim May 6 2015the fifth estateNessuna valutazione finora
- Daniel Smith Trial Closing ArgumentsDocumento23 pagineDaniel Smith Trial Closing Argumentsthe fifth estateNessuna valutazione finora
- Response - MistryDocumento10 pagineResponse - Mistrythe fifth estateNessuna valutazione finora
- Dennis Oland's AppealDocumento6 pagineDennis Oland's Appealthe fifth estate100% (1)
- Notice of Civil Claim Against NevsunDocumento27 pagineNotice of Civil Claim Against Nevsunthe fifth estateNessuna valutazione finora
- Pondok Indah Hospital, Jakarta, Indonesia // May 2, 2014Documento1 paginaPondok Indah Hospital, Jakarta, Indonesia // May 2, 2014the fifth estateNessuna valutazione finora
- SOS Medika Clinic, Jakarta, Indonesia // March 22, 2014Documento1 paginaSOS Medika Clinic, Jakarta, Indonesia // March 22, 2014the fifth estateNessuna valutazione finora
- Institute of Tropical Medicine, Antwerp, Belgium // 19 Nov 2015Documento1 paginaInstitute of Tropical Medicine, Antwerp, Belgium // 19 Nov 2015the fifth estateNessuna valutazione finora
- Response To Civil Claim Against NevsunDocumento17 pagineResponse To Civil Claim Against Nevsunthe fifth estateNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- COVID19 Pandemic: Problems and Reflection in Indonesia: Lecturer: Nina Fatriana, S.PD.,M.PDDocumento20 pagineCOVID19 Pandemic: Problems and Reflection in Indonesia: Lecturer: Nina Fatriana, S.PD.,M.PDGisca Syanitia IINessuna valutazione finora
- Dr. Ilham - AFLP - ISSHP 2017 BandungDocumento40 pagineDr. Ilham - AFLP - ISSHP 2017 BandungMegaSariDewiNessuna valutazione finora
- ICMR AbstractDocumento2 pagineICMR AbstractKanthimathinathan KrishnanNessuna valutazione finora
- CA A Cancer J Clinicians - 2018 - Bray - Global Cancer Statistics 2018 GLOBOCAN Estimates of Incidence and MortalityDocumento31 pagineCA A Cancer J Clinicians - 2018 - Bray - Global Cancer Statistics 2018 GLOBOCAN Estimates of Incidence and MortalityAngelia Adinda AnggonoNessuna valutazione finora
- Assignment 3Documento6 pagineAssignment 3ticticNessuna valutazione finora
- Evaluation of The R One Robotic System For Percutaneous Coronary Intervention THDocumento11 pagineEvaluation of The R One Robotic System For Percutaneous Coronary Intervention THNeranga SamaratungeNessuna valutazione finora
- Theroleofpain Classificationsystemsin Painmanagement: Patty Montgomery Orr,, Bettina Cobb Shank,, Amy Conner BlackDocumento12 pagineTheroleofpain Classificationsystemsin Painmanagement: Patty Montgomery Orr,, Bettina Cobb Shank,, Amy Conner Blackneurologi standart4Nessuna valutazione finora
- Record Below The Total Number of Cases and Deaths For Each Disease/condition For The Current WeekDocumento2 pagineRecord Below The Total Number of Cases and Deaths For Each Disease/condition For The Current WeekYohannes MengistNessuna valutazione finora
- Fetal Alcohol Syndrome Brochure For Nursing SchoolDocumento2 pagineFetal Alcohol Syndrome Brochure For Nursing SchoolKrystal Cowley Miller100% (1)
- Alcohol and PancreatitisDocumento2 pagineAlcohol and Pancreatitishrpwmv83Nessuna valutazione finora
- The Poppelreuter Figure Visual PerceptualDocumento4 pagineThe Poppelreuter Figure Visual PerceptualIcaroNessuna valutazione finora
- PhysioEx9,1: Exercise 7 Activity 2: PEX-07-02Documento8 paginePhysioEx9,1: Exercise 7 Activity 2: PEX-07-02mishael_baig100% (11)
- Org Chart 122007Documento1 paginaOrg Chart 122007d40sithuiNessuna valutazione finora
- Company ProfileDocumento6 pagineCompany ProfileAhmed Eljenan100% (1)
- Claudia Dorsey-Resume2Documento1 paginaClaudia Dorsey-Resume2api-454149310Nessuna valutazione finora
- DrugDocumento4 pagineDrugAugene ToribioNessuna valutazione finora
- Obat Klinik 2022-2023Documento96 pagineObat Klinik 2022-2023jeane rahmanNessuna valutazione finora
- Patheon Dosage CapabilitiesDocumento6 paginePatheon Dosage CapabilitiesHariharan90Nessuna valutazione finora
- Health Hazards of Chemicals Commonly Used On Military BasesDocumento35 pagineHealth Hazards of Chemicals Commonly Used On Military Basesmale nurseNessuna valutazione finora
- Pfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)Documento13 paginePfeiffer 5 Ppts Chapter05 - The Psychology of Injury (Student Copy)api-287615830Nessuna valutazione finora
- Discharge PlanDocumento1 paginaDischarge PlanGail GenturalezNessuna valutazione finora
- Chapter37 Assessment and Management of Patients With Allergic DisordersDocumento40 pagineChapter37 Assessment and Management of Patients With Allergic Disordersjericho dinglasanNessuna valutazione finora
- Communicable Disease Nursing Part II Diseases (1) 2Documento21 pagineCommunicable Disease Nursing Part II Diseases (1) 2MK LiNessuna valutazione finora
- (AIA) Hospital DESIGN GuidelinesDocumento100 pagine(AIA) Hospital DESIGN Guidelinespolyplop100% (1)
- Stewardship White PaperDocumento21 pagineStewardship White PaperHosam GomaaNessuna valutazione finora
- DESIGN AND DEVELOPMENT OF C-ARM MACHINE - Pptx.feem - Backup - 265248Documento11 pagineDESIGN AND DEVELOPMENT OF C-ARM MACHINE - Pptx.feem - Backup - 265248TamilandaNessuna valutazione finora
- Intensive & Critical Care NursingDocumento7 pagineIntensive & Critical Care NursingFernando PintoNessuna valutazione finora
- Peds Exam 2 Review QuestionsDocumento11 paginePeds Exam 2 Review Questionschristalh7460% (5)
- Radiology and HoneyCombDocumento12 pagineRadiology and HoneyCombmuhhasanalbolkiah saidNessuna valutazione finora
- Past Psychiatric History ExamplesDocumento11 paginePast Psychiatric History ExamplesEzra Denise Lubong RamelNessuna valutazione finora