Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ero Diabetes Type II
Caricato da
NocReyes100%(1)Il 100% ha trovato utile questo documento (1 voto)
63 visualizzazioni4 pagineThere are an estimated 23. Million people in the u.s. (7.8% of the population) with diabetes. 90% of those diagnosed are type 2 diabetes. Insulin resistance is a problem with the cells that respond to insulin.
Descrizione originale:
Copyright
© Attribution Non-Commercial (BY-NC)
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoThere are an estimated 23. Million people in the u.s. (7.8% of the population) with diabetes. 90% of those diagnosed are type 2 diabetes. Insulin resistance is a problem with the cells that respond to insulin.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
63 visualizzazioni4 pagineEro Diabetes Type II
Caricato da
NocReyesThere are an estimated 23. Million people in the u.s. (7.8% of the population) with diabetes. 90% of those diagnosed are type 2 diabetes. Insulin resistance is a problem with the cells that respond to insulin.
Copyright:
Attribution Non-Commercial (BY-NC)
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 4
DIABETES TYPE II
NON INSULIN DEPENDENT
Diabetes mellitus type 2 or type 2 diabetes (formerly called
non-insulin-dependent diabetes mellitus (NIDDM), or adult-
onset diabetes) is a disorder that is characterized by high
blood glucose in the context of insulin resistance and
relative insulin deficiency. While it is often initially managed
by increasing exercise and dietary modification, medications
are typically needed as the disease progresses. There are an
estimated 23.6 million people in the U.S. (7.8% of the
population) with diabetes with 17.9 million being diagnosed,
90% of whom are type 2. With prevalence rates doubling
between 1990 and 2005, CDC has characterized the increase
as an epidemic.
Traditionally considered a disease of adults, type 2 diabetes
is increasingly diagnosed in children in parallel to rising
obesity rates, due to alterations in dietary patterns as well
as in life styles during childhood.
Unlike type 1 diabetes, there is very little tendency toward
ketoacidosis in type 2 diabetes, though it is not unknown.
One effect that can occur is nonketonic hyperglycemia which
also is quite dangerous, though it must be treated very
differently. Complex and multifactorial metabolic changes
very often lead to damage and function impairment of many
organs, most importantly the cardiovascular system in both
types. This leads to substantially increased morbidity and
mortality in both type 1 and type 2 patients, but the two
have quite different origins and treatments despite the
similarity in complications.
PATHOPHYSIOLOGY
Insulin resistance means that body cells do not respond
appropriately when insulin is present. Unlike type 1 diabetes mellitus,
insulin resistance is generally "post-receptor", meaning it is a problem
with the cells that respond to insulin rather than a problem with the
production of insulin.
Other important contributing factors: increased hepatic glucose
production (e.g., from glycogen -> glucose conversion), especially at
inappropriate times (typical cause is deranged insulin levels, as those
levels control this function in liver cells)
• decreased insulin-mediated glucose transport in (primarily)
muscle and adipose tissues (receptor and post-receptor defects)
• impaired beta-cell function—loss of early phase of insulin release
in response to hyperglycemic stimuli
This is a more complex problem than type 1, but is sometimes easier
to treat, especially in the early years when insulin is often still being
produced internally. Type 2 may go unnoticed for years before
diagnosis, since symptoms are typically milder (eg, no ketoacidosis,
coma, etc) and can be sporadic. However, severe complications can
result from improperly managed type 2 diabetes, including renal
failure, erectile dysfunction, blindness, slow healing wounds (including
surgical incisions), and arterial disease, including coronary artery
disease. The onset of type 2 has been most common in middle age and
later life, although it is being more frequently seen in adolescents and
young adults due to an increase in child obesity and inactivity. A type
of diabetes called MODY is increasingly seen in adolescents, but this is
classified as a diabetes due to a specific cause and not as type 2
diabetes.
Diabetes mellitus type 2 is presently of unknown etiology (i.e., origin).
Diabetes mellitus with a known etiology, such as secondary to other
diseases, known gene defects, trauma or surgery, or the effects of
drugs, is more appropriately called secondary diabetes mellitus or
diabetes due to a specific cause. Examples include diabetes mellitus
such as MODY or those caused by hemochromatosis, pancreatic
insufficiencies, or certain types of medications (e.g., long-term steroid
use).
Diabetes mellitus type 2 is often associated with obesity, hypertension,
elevated cholesterol (combined hyperlipidemia), and with the condition
often termed Metabolic syndrome (it is also known as Syndrome X,
Reavan's syndrome, or CHAOS). Secondary causes of Diabetes mellitus
type 2 are: acromegaly, Cushing's syndrome, thyrotoxicosis,
pheochromocytoma, chronic pancreatitis, cancer and drugs.
Drug induced hyperglycemia:
• Atypical Antipsychotics - Alter receptor binding characteristics,
leading to increased insulin resistance.
• Beta-blockers - Inhibit insulin secretion.
• Calcium Channel Blockers - Inhibits secretion of insulin by
interfering with cytosolic calcium release.
• Corticosteroids - Cause peripheral insulin resistance and
gluconeogensis.
• Fluoroquinolones - Inhibits insulin secretion by blocking ATP
sensitive potassium channels.
• Naicin - They cause increased insulin resistance due to increased
free fatty acid mobilization.
• Phenothiazines - Inhibit insulin secretion.
• Protease Inhibitors - Inhibit the conversion of proinsulin to insulin.
• Thiazide Diuretics - Inhibit insulin secretion due to hypokalemia.
They also cause increased insulin resistance due to increased
free fatty acid mobilization.
Additional factors found to increase risk of type 2 diabetes include
aging, high-fat diets and a less active lifestyle..
PATIENT PROFILE
Name: Palomera Carolino
Age: 62
Gender: male
Birth date: January 15, 1947
Educational attainment: Commerce graduate
Religion: Catholic
Occupation: Retired custom representative
Patient history: He has no maintenance of meds. Only self
discipline on terms of diet and exercise but because of his
depression on his job early retirement he stopped his healthy
lifestyle that lead to below the knee amputation.
Present condition: Right leg amputated last Nov. 23, 2009
Past illnesses: none
Family history of illness: Diabetes and hypertension on father
side.
Past hospitalization: Last Oct. because of unhealed wound on the
dorsum on the right foot.
Diet: Before, he is very conscious about his diet but when he
retired on his job he become depressed and did not care about
what he eat. He always drinks coke zero because he believes
that it is zero sugar.
Exercise: before, he does a lot of exercises but when he become
depressed because of his retirement he stopped.
Sleep pattern: Mr. Palomera sleeps at around 8-9pm and woke
up as early as 3am.
Voiding pattern: he voids 3x a day.
Vices: None. Because they know that it can induced high blood
sugar.
Potrebbero piacerti anche
- Breaking the Chains of Diabetes. A Comprehensive Guide to Understanding and Managing Diabetes NaturallyDa EverandBreaking the Chains of Diabetes. A Comprehensive Guide to Understanding and Managing Diabetes NaturallyNessuna valutazione finora
- Ultimate Diet Plan for Diabetic Patients: Revolutionizing Diabetic NutritionDa EverandUltimate Diet Plan for Diabetic Patients: Revolutionizing Diabetic NutritionNessuna valutazione finora
- Diabetes MellitusDocumento13 pagineDiabetes Mellitusdreneavalentinstefan100% (1)
- IntroductionDocumento22 pagineIntroductionjayrana40Nessuna valutazione finora
- Pathophysiology and Pathogenesis of Type 2 DiabetesDocumento8 paginePathophysiology and Pathogenesis of Type 2 DiabetesGladys SorianoNessuna valutazione finora
- Diabetes MellitusDocumento5 pagineDiabetes MellitussujithasNessuna valutazione finora
- Diabeties NewDocumento54 pagineDiabeties NewDipti SharmaNessuna valutazione finora
- Dad ADocumento107 pagineDad Abammu21Nessuna valutazione finora
- Type 1 vs Type 2 Diabetes: Causes and TreatmentsDocumento3 pagineType 1 vs Type 2 Diabetes: Causes and TreatmentsTvisha PatelNessuna valutazione finora
- Controlling Blood Glucose 2 (AutoRecovered)Documento3 pagineControlling Blood Glucose 2 (AutoRecovered)Tvisha PatelNessuna valutazione finora
- Controlling Blood Glucose 2 (AutoRecovered)Documento3 pagineControlling Blood Glucose 2 (AutoRecovered)Tvisha PatelNessuna valutazione finora
- Type 1 vs Type 2 Diabetes: Causes and TreatmentsDocumento3 pagineType 1 vs Type 2 Diabetes: Causes and TreatmentsTvisha PatelNessuna valutazione finora
- How EXERCISE Helps Control DiabetesDocumento23 pagineHow EXERCISE Helps Control DiabetesApurba MukherjeeNessuna valutazione finora
- Bka Case FinalDocumento26 pagineBka Case FinalJayson SorianoNessuna valutazione finora
- Diabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inDocumento3 pagineDiabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inGanesh BalaNessuna valutazione finora
- Diabetes MellitusDocumento19 pagineDiabetes MellitusHaleelu Abdul JaleelNessuna valutazione finora
- Diabetes MellitusDocumento6 pagineDiabetes MellitusChristian YuNessuna valutazione finora
- Diabetes Mellitus 1Documento16 pagineDiabetes Mellitus 1Ajet AsaniNessuna valutazione finora
- Case Study - Diabetes Mellitus (Nutrition&Dietetics)Documento10 pagineCase Study - Diabetes Mellitus (Nutrition&Dietetics)Summer Suarez100% (1)
- Presentation On Diabetes Mellitus in Pharmacology LabDocumento35 paginePresentation On Diabetes Mellitus in Pharmacology Labpurwo yuhantoNessuna valutazione finora
- Type 2 Diabetes MellitusDocumento19 pagineType 2 Diabetes MellitusFelipe Senn Guerrero100% (2)
- Introduction To DiabetesDocumento9 pagineIntroduction To DiabetesSameer Saurabh100% (1)
- DM ThyroidDocumento184 pagineDM ThyroidtentenNessuna valutazione finora
- Pathophysiology of Type II Diabetes MellitusDocumento7 paginePathophysiology of Type II Diabetes Mellituschinthaka18389021Nessuna valutazione finora
- Diabetes MellitusDocumento12 pagineDiabetes MellitusAli Khan pashtoonNessuna valutazione finora
- Pathophysiology of Type 2 DiabetesDocumento5 paginePathophysiology of Type 2 DiabetesLouella Mae CoraldeNessuna valutazione finora
- Diabetes Types ExplainedDocumento11 pagineDiabetes Types ExplainedHasan AlomariNessuna valutazione finora
- Diabetes Mellitus Is A Group of Metabolic Diseases Characterized byDocumento67 pagineDiabetes Mellitus Is A Group of Metabolic Diseases Characterized byBivek TimalsinaNessuna valutazione finora
- Physiology and Causes of DiabatesDocumento7 paginePhysiology and Causes of DiabatesasaadsarfrazNessuna valutazione finora
- Diabetes Type 2 and How It ArisesDocumento9 pagineDiabetes Type 2 and How It Arisesayankotlai099Nessuna valutazione finora
- Type 1 Diabetes Mellitus: PathoDocumento6 pagineType 1 Diabetes Mellitus: PathoMary JoyceNessuna valutazione finora
- Non-communicable Disease Types and CausesDocumento18 pagineNon-communicable Disease Types and CausestomailjoNessuna valutazione finora
- Diabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inDocumento9 pagineDiabetes Mellitus, Often Simply Referred To As Diabetes, Is A Group of Metabolic Diseases inShAm BuenacosaNessuna valutazione finora
- Definition and Diagnostic Criteria For Diabetes Mellitus and Other Categories of Glucose IntoleranceDocumento4 pagineDefinition and Diagnostic Criteria For Diabetes Mellitus and Other Categories of Glucose Intolerancevai2Nessuna valutazione finora
- DM1-DM2 OdtDocumento5 pagineDM1-DM2 OdtCarlaLuisaVillalunaNessuna valutazione finora
- Diabetes MellitusDocumento8 pagineDiabetes MellitusJaja RamosNessuna valutazione finora
- Diabetes MellitusDocumento8 pagineDiabetes MellitusJaja RamosNessuna valutazione finora
- Diabetes MellitusDocumento8 pagineDiabetes MellitusJaja RamosNessuna valutazione finora
- Diabetes MellitusDocumento21 pagineDiabetes MellitusJuri GallosNessuna valutazione finora
- DiabatesDocumento10 pagineDiabatesMuhammad touseefNessuna valutazione finora
- DM Report1Documento16 pagineDM Report1Wendy EscalanteNessuna valutazione finora
- Diabetes Mellitus Type 2Documento3 pagineDiabetes Mellitus Type 2Licio LentimoNessuna valutazione finora
- Diabetes Mellitus 1Documento19 pagineDiabetes Mellitus 1shamma shahulhameedNessuna valutazione finora
- Jaya's BiochemistryDocumento13 pagineJaya's BiochemistryJKKP HPJBNessuna valutazione finora
- DiabetesDocumento3 pagineDiabetesruqqyNessuna valutazione finora
- DM Presentation (3)Documento28 pagineDM Presentation (3)mymommywowNessuna valutazione finora
- Pathophysiology of Diabetes MellitusDocumento2 paginePathophysiology of Diabetes MellitusShelly_Ann_Del_9959Nessuna valutazione finora
- DM Grand Case PresDocumento24 pagineDM Grand Case PresBing Howell de GuzmanNessuna valutazione finora
- Diabetes Facts: Types, Causes and Symptoms ExplainedDocumento13 pagineDiabetes Facts: Types, Causes and Symptoms ExplainedShelly_Ann_Del_9959Nessuna valutazione finora
- Clinical PathologyDocumento10 pagineClinical PathologyAnas AshrafNessuna valutazione finora
- IntroductionDocumento13 pagineIntroductionSaadNessuna valutazione finora
- Nursing Care Plans For Diabetes MellitusDocumento12 pagineNursing Care Plans For Diabetes MellitusPuteri AzmanNessuna valutazione finora
- Definition of Diabtes MellitusDocumento10 pagineDefinition of Diabtes MellitusJeremy Edbert JinggaNessuna valutazione finora
- 222 Diabetes FinalDocumento61 pagine222 Diabetes Finalrajatsgr100% (1)
- DM ReportDocumento16 pagineDM ReportWendy EscalanteNessuna valutazione finora
- Case Presentation EndocrineDocumento42 pagineCase Presentation EndocrineLéojAfallaNessuna valutazione finora
- Management of Diabetes Mellitus 11Documento25 pagineManagement of Diabetes Mellitus 11khalid.zainabNessuna valutazione finora
- Diabetes OverviewDocumento38 pagineDiabetes OverviewKye GarciaNessuna valutazione finora
- DiabetesDocumento34 pagineDiabetesqurat-ul-ain.sonNessuna valutazione finora
- Nursing Care Plans For Diabetes MellitusDocumento12 pagineNursing Care Plans For Diabetes MellitusRaveen mayi85% (59)
- Operating Systems Software in The BackgroundDocumento58 pagineOperating Systems Software in The BackgroundNocReyesNessuna valutazione finora
- NCP EbuenDocumento3 pagineNCP EbuenNocReyesNessuna valutazione finora
- Lyn's Drug StudyDocumento2 pagineLyn's Drug StudyNocReyesNessuna valutazione finora
- Broncho Pneumonia 1Documento28 pagineBroncho Pneumonia 1NocReyesNessuna valutazione finora
- Coronary Artery Disease Congestive Heart Failure HypertensionDocumento28 pagineCoronary Artery Disease Congestive Heart Failure HypertensionNocReyesNessuna valutazione finora
- Prepared By: Jose Chino O. Reyes, BSN III - DiureticsDocumento6 paginePrepared By: Jose Chino O. Reyes, BSN III - DiureticsNocReyesNessuna valutazione finora
- Increasing Muscle Mass To CDocumento8 pagineIncreasing Muscle Mass To CCarlos MosqueraNessuna valutazione finora
- Concept of Fat Balance in Human Obesity Revisited With Particular Reference To de Novo LipogenesisDocumento9 pagineConcept of Fat Balance in Human Obesity Revisited With Particular Reference To de Novo LipogenesisEduardo de SouzaNessuna valutazione finora
- JURNAL - Jaringan AdiposaDocumento10 pagineJURNAL - Jaringan AdiposaPramesvara NaoriNessuna valutazione finora
- Diabetes Management in GP 09 PDFDocumento47 pagineDiabetes Management in GP 09 PDFRizka ArianiNessuna valutazione finora
- A Review of The Ef Ficacy and Safety of Banaba (Lagerstroemia Speciosa L.) and Corosolic AcidDocumento8 pagineA Review of The Ef Ficacy and Safety of Banaba (Lagerstroemia Speciosa L.) and Corosolic AcidLyka MahrNessuna valutazione finora
- Summary On Sugar-Sweetened Beverage But Not Diet Soda Consumption Is Positively Associated With Progression of Insulin Resistance and Prediabetes'Documento2 pagineSummary On Sugar-Sweetened Beverage But Not Diet Soda Consumption Is Positively Associated With Progression of Insulin Resistance and Prediabetes'amrit khatriNessuna valutazione finora
- Nursing Care Plans For Diabetes MellitusDocumento12 pagineNursing Care Plans For Diabetes MellitusPuteri AzmanNessuna valutazione finora
- Nutrition Exam Multiple ChoiceDocumento8 pagineNutrition Exam Multiple ChoiceSofia Spears Elma100% (6)
- Perspective: Plant-Based Eating Pattern For Type 2 Diabetes Prevention and Treatment: Efficacy, Mechanisms, and Practical ConsiderationsDocumento11 paginePerspective: Plant-Based Eating Pattern For Type 2 Diabetes Prevention and Treatment: Efficacy, Mechanisms, and Practical ConsiderationsdgmtfmNessuna valutazione finora
- VerbalDocumento7 pagineVerbalKirsten Evidente100% (1)
- Association Between Cortisol, Insulin Resistance and ZincDocumento8 pagineAssociation Between Cortisol, Insulin Resistance and ZincEzard DavidNessuna valutazione finora
- Ginger ArticleDocumento17 pagineGinger ArticleDr-Aftab Ahmed KhanNessuna valutazione finora
- Diabetic Retinopathy-An Underdiagnosed and Undertreated Inflammatory, Neuro-Vascular Complication of DiabetesDocumento14 pagineDiabetic Retinopathy-An Underdiagnosed and Undertreated Inflammatory, Neuro-Vascular Complication of DiabetesVivi DeviyanaNessuna valutazione finora
- Current Trends in The Diagnosis and Management ofDocumento42 pagineCurrent Trends in The Diagnosis and Management ofseun williamsNessuna valutazione finora
- Surgical Techniques For Pancreas Transplantation: Ugo Boggi, Gabriella Amorese and Piero MarchettiDocumento10 pagineSurgical Techniques For Pancreas Transplantation: Ugo Boggi, Gabriella Amorese and Piero MarchettiNatalindah Jokiem Woecandra T. D.Nessuna valutazione finora
- The Effect of Ginger PowderDocumento8 pagineThe Effect of Ginger PowdermplennaNessuna valutazione finora
- Diabetes Classification UpdateDocumento241 pagineDiabetes Classification UpdateAlex MarinNessuna valutazione finora
- Medication-Induced Diabetes MellitusDocumento6 pagineMedication-Induced Diabetes MellitusAmjadNessuna valutazione finora
- Hormonal Secretion of PancreasDocumento17 pagineHormonal Secretion of PancreasNazia WasimNessuna valutazione finora
- Jurnal New 3 PDFDocumento134 pagineJurnal New 3 PDFMahda LNNessuna valutazione finora
- Diabetes Chapter 1 IntroductionDocumento23 pagineDiabetes Chapter 1 IntroductionHannah CaldinoNessuna valutazione finora
- Lifestyle and Nutritional ImbalancesDocumento19 pagineLifestyle and Nutritional Imbalanceskiko arrojasNessuna valutazione finora
- Diabetes Mellitus Complte LONG 2Documento56 pagineDiabetes Mellitus Complte LONG 2John Vincent Dy OcampoNessuna valutazione finora
- DANTAS 2020 Exercise-Induced Increases in Insulin Sensitivity After Bariatric Surgery Are Mediated by Muscle Extracellular Matrix RemodelingDocumento17 pagineDANTAS 2020 Exercise-Induced Increases in Insulin Sensitivity After Bariatric Surgery Are Mediated by Muscle Extracellular Matrix RemodelingCris AquinoNessuna valutazione finora
- 7 Food Timing Hacks For Rapid Fat LossDocumento20 pagine7 Food Timing Hacks For Rapid Fat LossLennart BjurstromNessuna valutazione finora
- Targeted Weight Reduction Using Sibutramine.Documento4 pagineTargeted Weight Reduction Using Sibutramine.International Medical PublisherNessuna valutazione finora
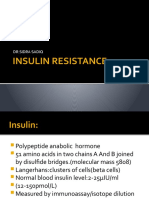
- Insulin Resistance by DR Sidra SadiqDocumento34 pagineInsulin Resistance by DR Sidra Sadiqdr. SheryarOrakzaiNessuna valutazione finora
- Physiologic Changes PregnancyDocumento53 paginePhysiologic Changes PregnancyDeedong Zydee100% (1)
- (Nutrition and Health) Giamila Fantuzzi, Carol Braunschweig (Eds.) - Adipose Tissue and Adipokines in Health and Disease-Humana Press (2014) PDFDocumento388 pagine(Nutrition and Health) Giamila Fantuzzi, Carol Braunschweig (Eds.) - Adipose Tissue and Adipokines in Health and Disease-Humana Press (2014) PDFjoao manoelNessuna valutazione finora
- Periodontal Disease and Its Impact On Health FromDocumento9 paginePeriodontal Disease and Its Impact On Health FromLisbethNessuna valutazione finora